Abstract
Two cases with a long-standing thoracolumbar kyphosis due to ankylosing spondylitis are presented with a symptomatic localized destructive kyphotic lesion of the spine. Clinical and radiographic findings demonstrated a progressive vertebral and discovertebral kyphotic pseudarthrosis, known as an Andersson lesion, at the L1 and L1-2 level, respectively. Surgical correction and stabilization was performed by an extending transpedicular wedge resection osteotomy to restore spinal stability, to facilitate fracture healing as well as to restore the sagittal balance of the ankylosed spine. To predict the effect of a surgical correction of the Andersson lesion on the sagittal balance, deformity planning was performed preoperatively. The indication for surgery, the surgical technique and the 2 years’ clinical results are described. In addition, the difficulties experienced with preoperative deformity planning are evaluated.
Keywords: Ankylosing spondylitis, Andersson lesion, Surgery, Deformity planning
Introduction
Ankylosing spondylitis (AS) may lead to a fixed thoracolumbar deformity of the spine [22]. A minor trauma may cause a transvertebral, discovertebral, or transdiscal fracture of the ankylosed spine [16]. As a result of persistent motion at the fracture site, the healing process stops and the bone fails to unite, which leads to pseudarthrosis [12]. Spinal pseudarthrosis-complicating AS is currently known as an Andersson lesion (AL) [4, 5, 7, 11]. In addition, an AL may result in a localized progressive painful kyphotic deformity that leads to considerable disturbances of posture and sagittal balance.
Surgical correction and stabilization of a painful kyphotic AL in AS by an extending osteotomy may be considered. The goals of such a surgical procedure are to restore spinal stability, facilitate fracture healing, and to restore the sagittal balance of the ankylosed spine. In order to prevent complications related to overcorrection [14] or undercorrection [18], and to predict the effect of an extending osteotomy on the ankylosed spine, adequate deformity planning is essential. Since the spine in AS is a rigid beam of bone, an extending osteotomy can be planned with elementary trigonometric equations. The optimum osteotomy angle to be performed is based on the correction of both: the patient’s capacity to see the horizon and the sagittal balance of the ankylosed spine. The relationship between the osteotomy angle, sagittal balance, and level of osteotomy in patients with a thoracolumbar deformity caused by AS has been described before [20]. However, deformity planning in patients suffering from a kyphotic AL-complicating AS, in which the level of osteotomy is defined by the lesion itself, has not been described before.
We present the clinical results of two cases that have kyphotic AL-complicating AS, treated by a transpedicular wedge resection osteotomy, with a follow-up of more than 2 years. The aim of the present case report is to describe the consequences of deformity planning in patients with a fixed AL in relation to the osteotomy angle and the postoperative sagittal balance. Our patients were informed that data concerning their case would be submitted for publication.
Case 1
A 59-year-old man with a 41-year history of AS was presented to a regional hospital with thoracolumbar back pain after a minor fall. At physical examination no neurological deficits were observed. Initial plain radiographs were not made. One month after trauma, he developed progressive thoracolumbar back pain. Radiographs showed a classical appearance of an ankylosed spine with a compression fracture of L1. The patient was treated with a thoracolumbar sacral orthosis (TLSO) for 6 months. During immobilization, however, the pain increased, and he experienced a more stooped position during the day.
At presentation in our centre 9 months after initial trauma, physical examination revealed a severe thoracolumbar kyphosis with no neurological signs. Radiographic examination of the lumbar spine demonstrated an intravertebral fracture line and the appearance of pseudarthrosis with marked sclerosis at L1. There was a wedge-shaped appearance to the vertebral body L1 with a 40° kyphotic deformity at the thoracolumbar junction according to Cobb (Fig. 1). The lesion was recognized as a kyphotic AL.
Fig. 1.
Lateral radiographs of the lumbar spine demonstrating the Andersson lesion-complicating ankylosing spondylitis of the vertebral body of L1 in case 1 (a) before correction and (b) 32 months after correction of the kyphotic deformity by a transpedicular wedge resection osteotomy and transpedicular fixation
Given the history of the combination of progressive thoracolumbar back pain, no neurological deficit, and a progressive thoracolumbar kyphosis at the intravertebral pseudarthrosis of L1, we recommended both stabilization and correction of the deformity by an extending osteotomy at the level of the AL. The extent of correction needed to restore the sagittal deformity was determined by the principles of deformity planning described in [20]. In short, the correction of the chin-brow to vertical angle (CBVA) was measured clinically. In addition, on a standing full-length lateral radiograph, the sacral endplate angle (SEA) was measured. The radiographic deviation of the SEA from 40°, defined as the neutral SEA from the horizon, was calculated.
The sum of the corrected CBVA and the deviation of the SEA from 40° give the recommended osteotomy angle in the lumbar spine. From the relationship between the osteotomy angle and the level of osteotomy follows the postoperative sagittal balance expressed by the sagittal vertical axis (SVA) [20]. The SVA is defined by the horizontal distance between the posterior endplate of S1 and the plumb line from C7, measured with the SEA at 40°.
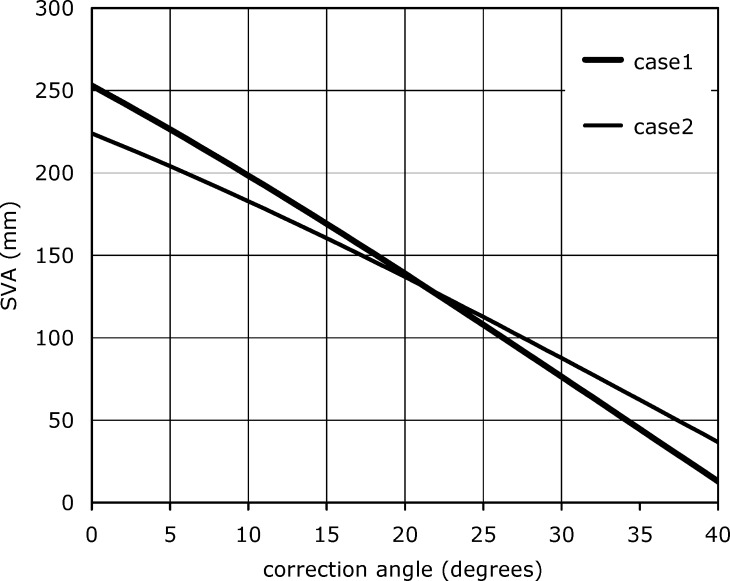
The correction of the CBVA was 0° because still some flexibility remained in the cervical spine. The SEA measured on a standing full-length lateral radiograph of the spine was 23°. As a result, the overall correction to be performed at the level of the AL was 17°. The hinge of the osteotomy was chosen at the centre of the anterior cortex of L1. The preoperative SVA was 253 mm. It was realized, however, that a 17° correction at L1 would not correct the imbalance of the patient. Rather, it would result in a postoperative SVA of 157 mm, which is more than the assumed optimal SVA in AS patients of 75 mm anterior to S1 [20]. To generate a SVA of 75 mm, a recommended correction angle of 30° was calculated at L1 (Fig. 2). However, a 30° correction at L1 would overcorrect the CBVA by 13°. Nevertheless, as there proved to be still some cervical mobility, this overcorrection was considered as not having clinical consequences.
Fig. 2.
The mathematical relation between the correction angle and the SVA for cases 1 and 2. The nomogram is constructed for the osteotomy of the AL at the L1 and L1–L2 level, respectively. The disparity between the mathematical SVA and the acquired postoperative SVA can be explained as a minor measurement error on the postoperative standing full-length radiograph
A transpedicular wedge resection osteotomy was performed at L1. Prior to the osteotomy, pedicle screws were inserted through the center of the pedicles of Th11, Th12, L2, and L3 (Xia spinal system, Stryker Spine, Cestas, France). A V-shaped wedge of bone including spinous processes, laminae, articular processes and part of the floor and roof of the intervertebral foramen was resected. The epidural space was entered, and the L1 nerve roots were identified. The pedicles of L1 were resected carefully and from both sides a posterior wedge of the vertebral body and the base of the pedicles, including the sclerotic margins surrounding the lytic fracture, were excised. The lateral walls were crushed and the transverse processes were excised. The anterior cortex of the vertebra and anterior longitudinal ligament were preserved and acted as a hinge for the closure of the gap. The planned amount of intravertebral correction was measured intraoperatively and controlled with the help of two osteotomes, a regular goniometer, and image intensification. Closure of the osteotomy was performed by hyperextending the hips and knees. After correction, the osteotomy was secured by fixing the rods in the pedicle screws. Postoperatively, a dorsal and ventral plaster shell was applied, and a circoelectric bed (Stryker, Uden, The Netherlands) was used. After 10 days, the patient was immobilized in a TLSO with one hip included for 3 months.
Radiographic examination immediately after the operation demonstrated a 24° correction of the kyphotic deformity at L1 (Fig. 1). Unfortunately, the patient showed a partial peroneal nerve palsy of his right lower leg postoperatively. The patient was evaluated at 6 weeks, 3 months, 6 months, 1 year, and 2 years postoperatively, over which time the back pain resolved and the peroneal function partially improved. At the 32-month follow-up examination, the patient had no back pain and was satisfied with the result. He was able to walk unlimited distances and the kickup foot brace that was used initially was not needed thereafter. The neurological examination demonstrated grade 4 of 5 strength of the extensor hallucis longus muscle and grade 4+ of 5 strength of the tibialis anterior muscle. The sensory examination demonstrated only a slight decrease in sensation to pinprick in the first dorsal web space. Radiographs at final follow-up demonstrated a complete consolidation of the osteotomy with no loss of correction, a SEA of 30°, and an SVA of 130 mm.
Case 2
A 45-year-old man with a 28-year history of AS presented with progressive intermittent thoracolumbar back pain. He was a professional gardener and did not have any history of spinal trauma in the past. At physical examination he showed a severe thoracic kyphotic deformity with no neurologic deficits. Radiography of the thoracolumbar spine showed fusion of the sacroiliac joints, as well as a complete ankylosing of the anterior and posterior spinal column. The lumbar spine showed opposing marginal destruction of L1 and L2 with sclerosis and osteophyte formation and a segmental kyphosis of 15°. Magnetic resonance imaging and CT imaging of the lumbar spine showed a discovertebral pseudarthrosis at L1-2 with canal narrowing without compression of the nerve roots. The lesion was recognized as a kyphotic AL.
Stabilization and pseudarthrosis repair of the AL was considered. In addition, an extending correction osteotomy was planned according to the mathematical method described before. The correction of the CBVA was 15° and the SEA measured on a standing full-length lateral radiograph of the spine was 22°. The rotation point or hinge of the osteotomy was chosen at the antero-inferior margin of L1. A recommended correction angle of 33 (18+15) degrees was calculated at L1-2.
A transpedicular wedge resection osteotomy was performed at L2, including resection of the opposing sclerotic marginal destruction of L1, with pedicle screw fixation from Th11 to L4, as described in case 1. Postoperatively, there were no complications (Fig. 3). Radiographic assessment immediately after the operation demonstrated a 31° correction of the kyphotic deformity at L1–L2. On a standing full-length lateral radiograph, a postoperative SEA of 34°, and an SVA of 55 mm were measured. At the 31-month follow-up, the radiographs showed an unaltered reduction with no loss of correction and complete consolidation of the osteotomy (Fig. 4).
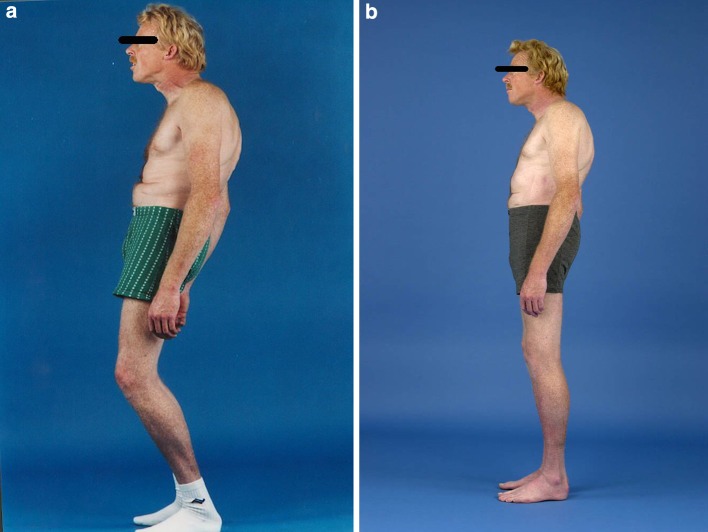
Fig. 3.
Clinical appearance (a) before and (b) after a transpedicular wedge resection osteotomy in case 2
Fig. 4.
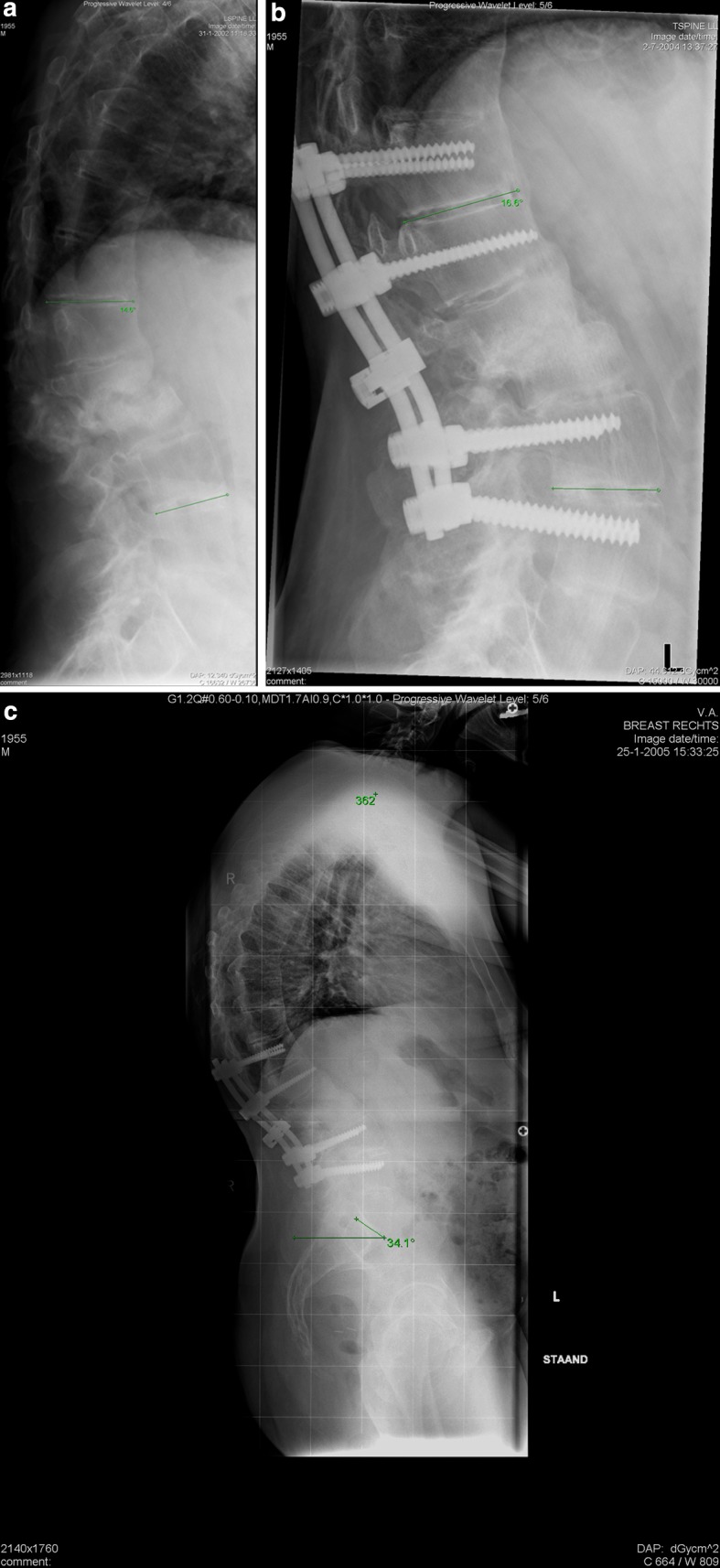
Lateral radiographs of the lumbar spine in case 2 (a) before and (b) after a transpedicular wedge resection osteotomy of L2 shows 31° correction. c Lateral radiographs of the full spine at final follow-up
Discussion
Andersson first described discovertebral destructive lesions of the spine related to AS in 1937 [1]. Currently, it has been recognized that these destructive lesions represent spinal pseudarthrosis that occur after failed fracture healing of the ankylosed spine in response to minor trauma or local stress [4, 6–9, 13, 23, 24]. Such lesions are referred to as AL of the spine complicating AS [5, 6, 11, 12, 15, and 17]. In addition, the combination of spinal pseudarthrosis and a pre-existing severe thoracolumbar kyphotic deformity caused by AS may result in a painful kyphotic AL
The history and radiographic findings after a minor trauma in AS are sometimes difficult to interpret and a spinal fracture can be missed easily when a patient is presented at the emergency department with back pain [10]. Patients are sometimes even not aware of a traumatic event in the past. This possibly was the reason for the delay in diagnosis and treatment in case 1. The second case, patient 2, was a hard working, self-employed gardener with no history of a traumatic event. He possible suffered from a stress fracture at the thoracolumbar region of the ankylosed spine.
Both patients presented here suffered from a painful progressive kyphotic AL and surgical stabilization was mandatory. Anterior spinal fusion may be advised in progressive kyphotic AL to heal the lesion [13]; however, this does not correct the kyphotic deformity. We therefore recommended a posterior, transpedicular wedge resection osteotomy to restore spinal stability, facilitate fracture healing and to restore the sagittal balance of the ankylosed spine [2, 3, 19, and 21]. To our knowledge, there are no reports describing a transpedicular wedge resection osteotomy for progressive thoracolumbar kyphotic deformity due to an AL-complicating AS.
A posterior transpedicular wedge resection osteotomy for the treatment of a kyphotic AL-complicating AS alters both the clinical view-angle (defined as the CBVA) and the sagittal balance of the spine. To predict the effect of a surgical correction of the AL on the CBVA and the sagittal balance, deformity planning is mandatory. Recently, a biomechanical and mathematical method for deformity planning for sagittal plane corrective osteotomies of the spine in AS has been developed to predict the effect of an osteotomy on the CBVA and sagittal balance of the spine [20]. Following the promoted mathematical equation, a nomogram subsequently shows the relationship between the level of osteotomy and the sagittal balance (expressed by the SVA).
This method of deformity planning was used in our two patients with a kyphotic AL-complicating AS. It was realized, however, that in these two cases the level of osteotomy was fixed by the AL. As was to be expected, the correction of the AL in the high lumbar region resulted in the inability to reach the optimal restoration of the sagittal balance in these patients. However, overcorrection at the level of the AL, in an attempt to achieve a better correction of the sagittal balance, may result in an extension deformity of the cervical spine forcing the visual field upward [14]. This dilemma is well demonstrated in the first case (patient 1): A correction angle of 17° was calculated at L1; however, this led to insufficient correction of the SVA. The osteotomy angle needed to reach an assumed optimal postoperative SVA of 75 mm [20] proved to be 30° at L1 (Fig. 2). It was realized, however, that a correction of 30° at L1 inevitably overcorrects the patient’s CBVA with 13°. Nevertheless, as a result of there remaining some movements in his cervical spine, this overcorrection was not considered to have clinical consequences. Unfortunately, a correction of 30° was not feasible during surgery. A maximal correction of 24° was achieved resulting in a postoperative SVA of 130 mm. The postoperative SEA was 30°, indicating that this patient continued to compensate sagittal spinal imbalance by rotating his pelvis posterior. This dilemma did not occur in the second case (patient 2). The reason may be that the level of osteotomy was at a lower level in the lumbar spine. In addition, the achieved osteotomy angle in the second patient correlated well with the planned correction needed at L2 to come close to the assumed optimal postoperative SVA of 75 mm.
To achieve the exact planned osteotomy angle during surgery, we used osteotomes and a regular goniometer in addition to the image intensifier. However, this measurement device obviously is not accurate. Therefore, a special measurement device for corrective osteotomies in AS should be developed.
In conclusion, we prospectively evaluated the biomechanical and clinical results of two patients suffering from a progressive kyphotic AL-complicating AS, treated by a posterior transpedicular wedge resection osteotomy at the level of the lesion. In the second case (patient 2), the transpedicular wedge resection osteotomy corrected the sagittal spinal balance with respect to the SEA and SVA. He is back to work as a gardener without any physical complaints. However, in the first case (patient 1), the SEA and SVA were not normalized postoperatively. Both patients, however, improved considerably with respect to posture and complaints. As a result, the benefit of preoperative deformity planning of a kyphotic AL-complicating AS in relation to the clinical outcome may be questioned. Consequently, further clinical research on the effect of deformity planning in transpedicular wedge resection osteotomy on the treatment of a kyphotic AL-complicating AS is necessary.
References
- 1.Andersson O. Röntgenbilden vid spondylarthritis ankylopoetica. Nord Med Tidskr. 1937;14:2000–2002. [Google Scholar]
- 2.Berven SH, Deviren V, Smith JA, Emami A, Hu SS, Bradford DS. Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine. 2001;26:2036–2043. doi: 10.1097/00007632-200109150-00020. [DOI] [PubMed] [Google Scholar]
- 3.Bridwell KH, Lewis SJ, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am. 2003;85-A:454–463. doi: 10.2106/00004623-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Cawley MI, Chalmers TM, Kellgren JH, Ball J. Destructive lesions of vertebral bodies in ankylosing spondylitis. Ann Rheum Dis. 1972;31:345–358. doi: 10.1136/ard.31.5.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dihlmann W, Delling G. Disco-vertebral destructive lesions (so-called Andersson lesions) associated with ankylosing spondylitis. Skeletal Radiol. 1978;3:10–16. doi: 10.1007/BF00365106. [DOI] [Google Scholar]
- 6.Dihlmann W, Lindenfelser R. Polysegmentäre Andersson Läsion bei ankylosierender spondylitis (röntgenologisch-histologische synopsis) Rofo. 1979;130:454–460. doi: 10.1055/s-0029-1231308. [DOI] [PubMed] [Google Scholar]
- 7.Fang D, Leong JC, Ho EK, Chan FL, Chow SP. Spinal pseudarthrosis in ankylosing spondylitis. Clinicopathological correlation and the results of anterior spinal fusion. J Bone Joint Surg Br. 1988;70:443–447. doi: 10.1302/0301-620X.70B3.3372569. [DOI] [PubMed] [Google Scholar]
- 8.Finkelstein JA, Chapman JR, Mirza S. Occult vertebral fractures in ankylosing spondylitis. Spinal Cord. 1999;37:444–447. doi: 10.1038/sj.sc.3100837. [DOI] [PubMed] [Google Scholar]
- 9.Gelman MI, Umber JS. Fractures of the thoracolumbar spine in ankylosing spondylitis. AJR Am J Roentgenol. 1978;130:485–491. doi: 10.2214/ajr.130.3.485. [DOI] [PubMed] [Google Scholar]
- 10.Hunter T, Dubo HI. Spinal fractures complicating ankylosing spondylitis. A long-term followup study. Arthritis Rheum. 1983;26:751–759. doi: 10.1002/art.1780260608. [DOI] [PubMed] [Google Scholar]
- 11.Obradov M, Schonfeld DH, Franssen MJ, Rooy DJ. Andersson lesion in ankylosing spondylitis. JBR–BTR. 2001;84:71. [PubMed] [Google Scholar]
- 12.Pettersson T, Laasonen L, Leirisalo-Repo M, Tervahartiala P. Spinal pseudoarthrosis complicating ankylosing spondylitis: a report of two patients. Br J Rheumatol. 1996;35:1319–1323. doi: 10.1093/rheumatology/35.12.1319. [DOI] [PubMed] [Google Scholar]
- 13.Rivelis M, Freiberger RH. Vertebral destruction at unfused segments in late ankylosing spondylitis. Radiology. 1969;93:251–256. doi: 10.1148/93.2.251. [DOI] [PubMed] [Google Scholar]
- 14.Sengupta DK, Khazim R, Grevitt MP, Webb JK. Flexion osteotomy of the cervical spine: a new technique for correction of iatrogenic extension deformity in ankylosing spondylitis. Spine. 2001;26:1068–1072. doi: 10.1097/00007632-200105010-00016. [DOI] [PubMed] [Google Scholar]
- 15.Sparenberg A, Hamm B, Wolf KJ. Ankylosierende spondylitis: Andersson-Läsion. Rofo. 1989;150:744–745. doi: 10.1055/s-2008-1047118. [DOI] [PubMed] [Google Scholar]
- 16.Thorngren KG, Liedberg E, Aspelin P. Fractures of the thoracic and lumbar spine in ankylosing spondylitis. Arch Orthop Trauma Surg. 1981;98:101–107. doi: 10.1007/BF00460796. [DOI] [PubMed] [Google Scholar]
- 17.Unsal E, Arici AM, Kavukcu S, Pirnar T. Andersson lesion: spondylitis erosiva in adolescents. Two cases and review of the literature. Pediatr Radiol. 2002;32:183–187. doi: 10.1007/s00247-001-0629-8. [DOI] [PubMed] [Google Scholar]
- 18.Van Royen BJ (1999) Lumbar osteotomy in ankylosing spondylitis, biomechanical and clinical aspects. Thesis, Vrije Universiteit, Amsterdam
- 19.Royen BJ, Gast A. Lumbar osteotomy for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. A structured review of three methods of treatment. Ann Rheum Dis. 1999;58:399–406. doi: 10.1136/ard.58.7.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Royen BJ, Gast A, Smit TH. Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis. Eur Spine J. 2000;9:492–498. doi: 10.1007/s005860000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Royen BJ, Slot GH. Closing-wedge posterior osteotomy for ankylosing spondylitis. Partial corporectomy and transpedicular fixation in 22 cases. J Bone Joint Surg Br. 1995;77:117–121. [PubMed] [Google Scholar]
- 22.Bechterew W. Steifigkeit der wirbelsäule und ihre Verkrümmung als besondere Erkrankungsform. Neurologisches Zentralbl. 1893;12:426–434. [Google Scholar]
- 23.Wu PC, Fang D, Ho EK, Leong JC. The pathogenesis of extensive discovertebral destruction in ankylosing spondylitis. Clin Orthop. 1988;230:154–161. [PubMed] [Google Scholar]
- 24.Yau AC, Chan RN. Stress fracture of the fused lumbo-dorsal spine in ankylosing spondylitis. A report of three cases. J Bone Joint Surg Br. 1974;56-B:681–687. doi: 10.1302/0301-620X.56B4.681. [DOI] [PubMed] [Google Scholar]