Abstract
In degenerative disc disease (DDD), increased loading in the posterior column increases facet joint subchondral bone density and may lead to facet joint degeneration. While spinal fusion is commonly used to treat patients with symptomatic DDD, increased stress at the levels adjacent to fusion may accelerate facet joint and adjacent segment degeneration. Artificial disc replacements have been developed as an alternative to fusion. In this prospective study, the effects of disc replacement with the CHARITÉ™ Artificial Disc on facet joint loading and integrity were evaluated. Thirteen patients aged <50 years with symptomatic DDD were recruited. Computed tomography (CT) osteoabsorptiometry was performed prior to the implantation of the CHARITÉ Artificial Disc and six months after. With this technique, increases or decreases in facet joint loading and integrity are indicated by corresponding changes in subchondral bone density. Changes in the distribution of load alter the distribution of the areas of maximum bone density. Clinical outcome was also assessed at pre-operative and 6 and 12 month post-operative visits using the Visual Analogue Scale back and leg pain scores, the Oswestry Disability Index and the Short Form-36 (SF-36) questionnaire. The height of the intervertebral space at the operated level was monitored by lateral X-ray. Subchondral bone density was evaluated in the facet joints of all 13 patients at the operated level, 12 patients at the level above the operated segment, and five patients at the level below the operated segment. Quantitative measurements revealed no significant increases (≥3%) in subchondral bone density of the facet joints at any level in any patient. Significant decreases (≥3%) in subchondral bone density were measured at the operated level in 10/13 patients, at the level above the operated segment in 6/12 patients, and at the level below the operated segment in 3/5 patients. There were no changes in the distribution of the areas of maximum bone density in any of the studied facet joints at 6 months compared with pre-operative measurements. Clinical outcome scores were improved at 6 and 12 months compared with baseline. The mean intervertebral space height at the operated level was increased following implantation of the CHARITÉ Artificial Disc and was 1.8 times greater than the pre-operative height at both 6 and 12 months. In this study, replacement of degenerated intervertebral discs with the CHARITÉ Artificial Disc was not associated with increased loading of the facet joints at the operated or adjacent levels. Decreases in subchondral bone density may indicate reduced loading in the posterior column following disc replacement compared with loading in the pre-operative degenerated spine. Further study is required to establish the baseline for healthy subchondral bone density and to compare this baseline with long-term measurements in patients undergoing disc replacement.
Keywords: Artificial disc replacement, Facet joints, Bone density, Disc height, Degenerative disc disease
Introduction
The kinematics of the lumbar spine are dependent on a precise interaction between the posterior and anterior structures of the spine. Facet joints are diarthrodial joints of the posterior spinal column that restrict vertebral motion and share stress and load with the intervertebral discs of the anterior column [1, 13, 19, 25]. Pathology of the facet joints is a major cause of lower back pain and segmental instability [4, 12].
Injury to the intervertebral discs disturbs segmental stability and produces asymmetric facet joint movement [17, 33, 41]. Reductions in intervertebral space height and intradiscal pressure that are associated with degenerative disc disease (DDD) increase loading on the facet joints [5, 13, 32, 39]. Facet joint degeneration is often preceded by disc injury and may be a consequence of the increased loading associated with DDD [6, 28, 35].
Bone morphology is known to adapt to mechanical load with additional loading of a joint causing appositional bone growth and in some cases bone sclerosis [10, 31, 34, 38]. Subchondral bone density is particularly affected by load and the ‘loading history’ of a joint can be determined from the distribution of bone density [3, 8, 30, 31]. The areas of the subchondral bone plate exposed to the greatest load correspond to the areas of maximum bone density [27]. Subchondral bone density can be accurately measured in living subjects by computed tomography (CT) osteoabsorptiometry [2, 3, 26, 30, 31].
Traditionally, most patients with symptomatic DDD who do not respond to non-operative intervention have been treated with spinal fusion. While fusion may restore segmental stability and halt degeneration at the operated level, increased stress at the adjacent levels may accelerate facet joint and adjacent segment degeneration [9, 16, 18, 21, 23]. Lee [23] reported hypertrophic degenerative osteoarthritis of the facet joints at levels adjacent to the fused vertebrae in 16 of 18 patients presenting with new symptoms ≥1 year after spinal fusion.
The limitations of spinal fusion have led to the development of several artificial disc replacement systems designed to mimic the function of intact intervertebral discs. By restoring disc height, segmental stability and normal kinematics, a fully effective disc replacement could prevent the degenerative cascade in adjacent levels. The CHARITÉ™ Artificial Disc is the most widely implanted disc replacement and has been used in the treatment of over 6,000 patients worldwide. In a recent study, which was the first to report Class I data comparing lumbar artificial disc replacement with fusion, equivalent or better outcomes were seen following disc replacement with the CHARITÉ Artificial Disc compared with BAK-assisted fusion [15].
The aims of this study were to determine the effects of disc replacement with the CHARITÉ Artificial Disc on facet joint loads and integrity by comparing pre- and post-operative subchondral bone density and the distribution of the areas of maximum subchondral bone density.
Materials and methods
Patients
Patients aged <50 years with symptomatic DDD were included in this prospective study. Using the CT and MRI criteria of Weishaupt and Fujiwara to judge facet joint integrity [14, 36] patients with no or minor facet joint degeneration (Class 0–II) were eligible for inclusion to ensure as near normal physiological kinematics as possible. Eligible patients presented with lower back pain as the predominate symptom and had been unsuccessfully treated by conservative methods for at least 6 months prior to surgery. Patients were excluded if there was evidence of osteoporosis, segmental instability, infection or tumour.
Pre-operative evaluation
All patients underwent a pre-operative examination during which baseline pain, function and quality of life were measured using the Visual Analogue Scale (VAS) back and leg pain scores, the Oswestry Disability Index (ODI) and the Short Form-36 (SF-36) questionnaire. Thin-slice CT scans of the affected and neighbouring spinal segments were performed for osteoabsorptiometry and to measure spinal canal width. Pre-operative facet joint integrity was determined by a three-phase skeleton scintigraphy and thin-slice CT scans [36]. The presence of disc degeneration and osteochondrosis of the vertebral endplates was investigated by a pre-operative magnetic resonance imaging scan.
Surgical technique
The CHARITÉ Artificial Disc was implanted via a ventral, retroperitoneal access. Angulated base plates and sliding cores of different heights were implanted for lordosis adjustment and individual adjustment of intervertebral height. Details of the surgical technique were as described by Hochschuler et al. [20].
Post-operative evaluation
Post-operative examinations were performed at 6 weeks, 3 months, 6 months and 12 months. Post-operative X-ray images were taken immediately following the operation and at 14 days, 6 months and 1 year post-operatively. Post-operative VAS, ODI and SF-36 scores were recorded and are reported for 6 and 12 months.
Determination of post-operative facet joint loading by CT osteoabsorptiometry
Thin-slice CT scans were performed 6 months post-operatively for osteoabsorptiometry. Both ventral (upper vertebra) and dorsal (lower vertebra) aspects of the left and right facet joints were evaluated in the operated level of all 13 patients (52 zones). The same aspects of the facet joints at the level above the operated segment were evaluated in 12/13 (92.3%) patients (48 zones) and at the level below the operated segment in 5/13 (38.5%) patients (20 zones). A total of 120 zones were examined. The areas of maximum subchondral bone density within each zone were determined pre-operatively for every patient and exactly the same areas were evaluated 6 months post-operatively.
Measurement of intervertebral space height and implant position
The intervertebral space at the operated level and the level above were measured by lateral X-ray. Normalised values were calculated by dividing the sum of the ventral and dorsal intervertebral space height (using the edges of the vertebral endplates as landmarks), by the sum of the ventral and dorsal height of the adjacent vertebral body (using the same landmarks), and shown as a percentage. This procedure enabled us to eliminate errors due to variability in magnification.
In order to track the progression of intervertebral space height at the operated level, X-rays were taken at the pre-operative examination, immediately after insertion of the CHARITÉ Artificial Disc, and at each post-operative examination. The intervertebral space height at the operated level was also compared with that at the level above.
The position of the CHARITÉ Artificial Disc was assessed by anteroposterior and lateral X-rays. The centre of an ideally positioned disc should appear in line with the spinous processes of the adjacent vertebra in anteroposterior X-rays. In lateral X-rays, the centre of the CHARITÉ Artificial Disc should be approximately 2 mm dorsal from the midline of the vertebral body. This is because the nucleus pulposus is shifted dorsally in physiological lumbar lordosis [37].
Determination of subchondral bone density by CT osteoabsorptiometry
Subchondral bone density and the distribution of the areas of maximum subchondral bone density were determined by CT osteoabsorptiometry. Slice images of the lumbar spine were produced at 1 mm intervals and reconstructed into a 3D map using a Somatom Plus 4 computed tomograph (Siemens AG Medical Solutions, Erlangen, Germany). Subchondral bone density was determined using Analyze maximum intensity projection software (Mayo Foundation, Rochester, USA) running on an IBM workstation (RISC System/6000; IBM, Germany).
Bone density was visualised in the CT-slices and 3D maps as different colours with areas of high density appearing white or black, thus providing a qualitative assessment of areas of maximum density and pre- and post-operative levels of mineralisation. Quantitative analysis was performed using a calibrated colour scale of pixel density measured in Housefield Units (HU) with an arbitrary range of 200 (low) to 1,200 HU (high). Bone mineral density in mg/ml of calcium was then calculated from the HU levels. Using this method, any increase or decrease in bone density of ≥3% is considered significant [29, 31]. CT osteoabsorptiometry examinations were performed immediately prior to implantation of the CHARITÉ Artificial Disc and 6 months post-operatively.
Statistics
Pre- and post-operative ODI, VAS and SF-36 scores are presented as mean±SD values. These outcome measures were used to indicate levels of pain, function and quality of life. No statistical analyses of pre- and post-operative differences in outcome measures were performed because of the small patient population. Pre- and post-operative range of motion values are presented as mean±SD.
Results
Patients
Patient demographics and baseline characteristics are shown in Table 1. Thirteen patients (10 female and 3 male) with a mean age of 39 years (range 27–49 years) were recruited for the study. All 13 patients had severe disc degeneration; 10 patients had monosegmental osteochondritis and three patients had bisegmental osteochondritis. Pre-operative CT and MRI scans showed that facet degeneration did not exceed Class II in any patient. There were no cases of spinal stenosis or nerve root compression. Five patients had previously undergone nucleotomies at the same level as the CHARITÉ Artificial Disc implant.
Table 1.
Patient demography and baseline characteristics
| Characteristics | |
|---|---|
| Male/female (n) | 3/10 |
| Mean age (range) (years) | 39 (27–49) |
| Pre-operative disc pathology (n) | |
| L4/L5 | 9 |
| L5/S1 | 4 |
| Pre-operative vertebral endplate pathology (n) | |
| Monosegmental osteochondritis | 10 |
| Bisegmental osteochondritis | 3 |
| Pre-operative facet integrity (n) | |
| Class 0 | 1 |
| Class 0–I | 1 |
| Class I | 2 |
| Class I–II | 6 |
| Class II | 3 |
| Previous surgery (n) | |
| Nucleotomy at operating level | 5 |
Surgery
The CHARITÉ Artificial Disc was implanted at L4/L5 in nine patients and L5/S1 in four patients. The three patients with bisegmental osteochondritis underwent fusion at L5/S1 and disc replacement with the CHARITÉ Artificial Disc at L4/L5. There were post-operative complications in three patients. One patient experienced an ileus that was successfully treated with a gastrograph. In two patients, post-operative sympathicus lesions were detected; one of these patients fully recovered after 3 months. All three complications were related to the anterior approach and not the insertion of the CHARITÉ Artificial Disc.
Post-operative outcomes
Post-operative examinations showed a continually improving symptom profile. At the 12-month post-operative examination, nine patients were pain-free and pain was clearly reduced in the remaining four patients. Radicular leg pain persisted sporadically in one patient.
Pre-operative and 6- and 12-month post-operative ODI, VAS and SF-36 scores are presented in Table 2. Mean ODI scores improved by 27 points at 6 months compared with pre-operative scores and there were improvements in mean VAS back pain and leg pain scores of 41 and 15 points, respectively. There were improvements in all parameters of the SF-36 score at 6 months. SF-36 pain intensity scores were particularly improved (16 points vs. 50 points). At the 12-month follow-up, further improvements in mean ODI, VAS back pain and VAS leg pain scores of 16, 11 and 13 points, respectively, were noted. There was little change in all parameters of the SF-36 score at 12 months compared with the 6-month scores.
Table 2.
Pre-operative and 6- and 12-month post-operative ODI, VAS and SF-36 scores
| Mean score±SD | Pre-operative | 6 months | 12 months |
|---|---|---|---|
| ODI | 53.38 ± 18.30 | 26.15 ± 15.46 | 10.38 ± 8.01 |
| VAS back pain | 68.00 ± 22.55 | 26.54 ± 22.90 | 16.31 ± 13.38 |
| VAS leg pain | 48.31 ± 34.64 | 32.92 ± 25.81 | 19.62 ± 17.08 |
| SF-36 category | |||
| Physical | 36.54 ± 24.97 | 67.65 ± 14.51 | 64.23 ± 5.34 |
| Social | 47.39 ± 41.02 | 75.41 ± 30.36 | 73.92 ± 7.25 |
| Role (physical) | 37.61 ± 38.92 | 41.56 ± 40.23 | 41.77 ± 12.11 |
| Role (emotional) | 42.07 ± 46.86 | 62.40 ± 45.17 | 61.46 ± 6.28 |
| Mental | 54.85 ± 17.02 | 62.79 ± 20.31 | 55.38 ± 5.88 |
| Energy | 54.07 ± 14.86 | 60.60 ± 19.76 | 63.23 ± 7.75 |
| Pain | 16.01 ± 15.11 | 49.99 ± 22.91 | 46.54 ± 7.32 |
| Health perception | 62.16 ± 21.13 | 61.25 ± 21.24 | 61.46 ± 7.20 |
Implant positioning
Post-operative X-rays showed that the CHARITÉ Artificial Disc was in the desired position in 6/13 patients. In five patients, lateral X-rays revealed the centre of the CHARITÉ Artificial Disc was in line with the midline of the vertebral body instead of lying slightly dorsal to the midline. Two patients showed a 2 mm leftwards displacement of the CHARITÉ Artificial Disc in anteroposterior X-rays, but there was no correlation between implant position and changes in bone density.
Restoration of intervertebral space height
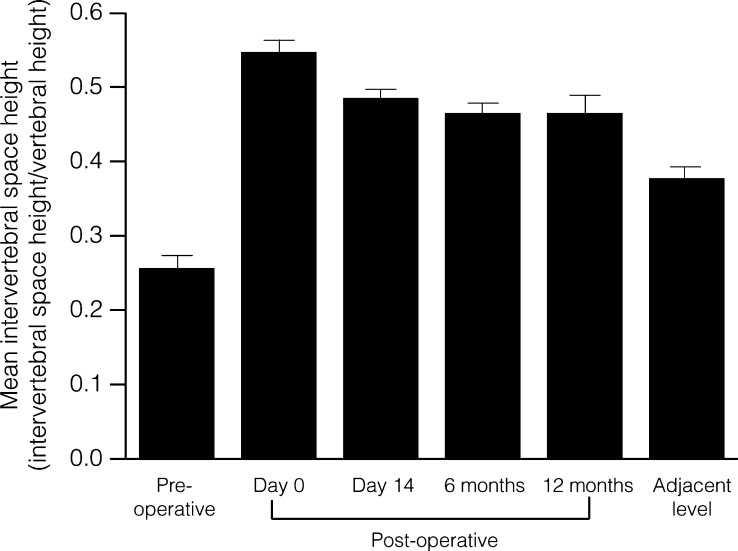
The mean intervertebral space height at the operated level was increased by a factor of 2.1 immediately after implantation of the CHARITÉ Artificial Disc (Fig. 1). Post-operative intervertebral space height changed little between the immediate post-operative measurement and that at 6 months. Between 6 and 12 months, intervertebral space height at the operative level was maintained at a value 1.8 times greater than the pre-operative height. The 12-month post-operative intervertebral space height at the operated level was 1.2 times greater than the height of the adjacent intervertebral space. There was no correlation between intervertebral space height and changes in bone density. In every case, the smallest possible core was used to be as close as possible to the physiological intervertebral space height.
Fig. 1.
Progression of intervertebral space height following disc replacement. Intervertebral space height is normalised to the height of the adjacent vertebrae. The intervertebral space height of the level above the operated segment is also shown
Post-operative distribution of the areas of maximum subchondral bone density
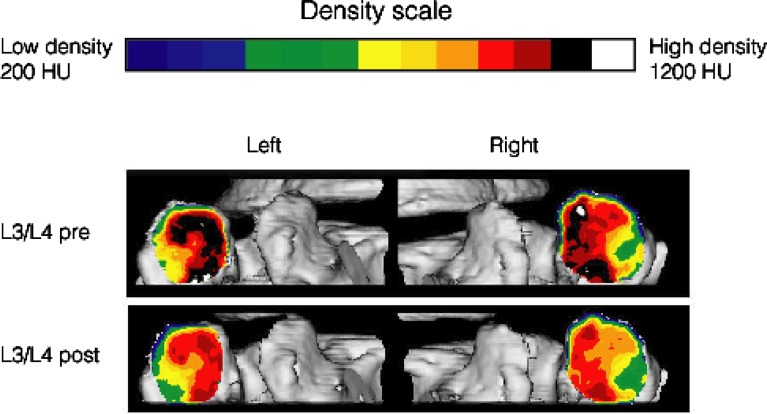
Qualitative analysis of the subchondral bone density distribution in the 3D colour images produced pre-operatively and at 6 months post-operatively, showed that there was no change in the distribution of the areas of maximum subchondral bone density in any of the 13 patients. A typical example is shown in Fig. 2.
Fig. 2.
3D colour map of facet joint subchondral bone density produced by CT osteoabsorptiometry at the pre-operative and 6-month post-operative visits. The dorsal aspects of the left and right facet joints at L3/L4 for patient 4 are shown. The distribution of the areas of maximum subchondral bone density were unchanged after 6 months. The overall bone density, however, decreased uniformally
Post-operative changes in subchondral bone density at the operated level
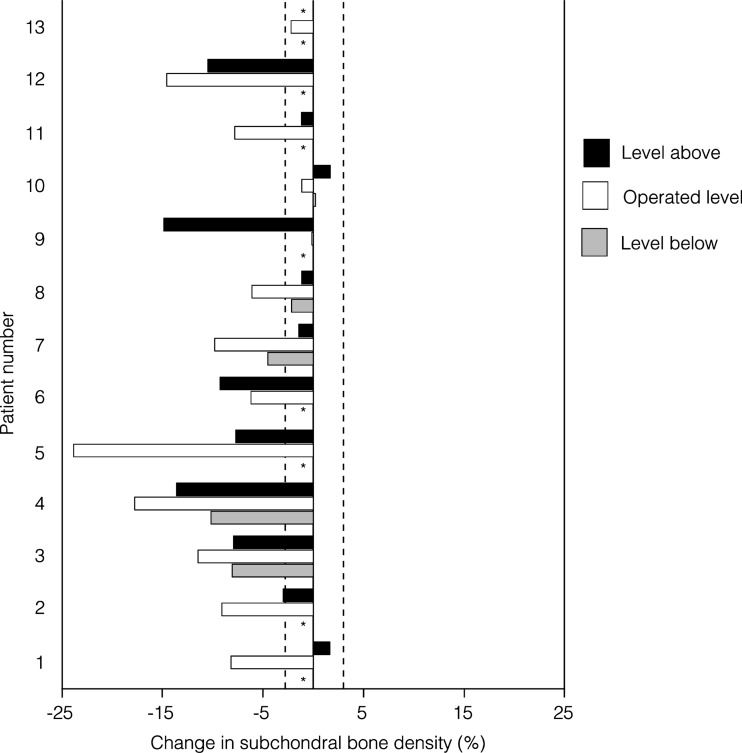
Percentage changes in subchondral bone density for the measured zones are shown in Table 3. Subchondral bone density was studied in the facet joints at the operated level in all 13 patients. A total of 52 zones were studied. Any changes in bone density of ≥3% were considered significant [29]. Significant decreases (≥3%) in subchondral bone density were seen in 43/52 (82.7%) zones (Table 3). There were no significant changes in density in seven (13.5%) zones, and significant increases in density in two (3.8%) zones. When the mean change in subchondral bone density at the operated level was calculated for each patient, there were significant post-operative decreases in 10/13 (76.9%) patients (Fig. 3). No significant changes in mean subchondral bone density at the operated level were seen in the remaining three (23.1%) patients. Overall, there was a mean decrease in subchondral bone density of the facet joints at the operated level of 9.08%.
Table 3.
Percentage change in subchondral bone density at 6 months
| Measured zone | Patient number | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11a | 12a | 13a | |
| L3/L4 left (dorsal) | −9.85 | −13.91 | −1.21 | −2.01 | −11.22 | 0.69 | −0.88 | −9.43 | |||||
| L3/L4 right (dorsal) | −9.29 | −9.81 | −1.43 | 1.25 | −9.06 | 2.61 | −1.38 | −8.09 | |||||
| L3/L4 left (ventral) | −5.43 | −16.35 | −2.24 | −1.61 | −17.42 | −0.72 | −3.32 | −13.86 | |||||
| L3/L4 right (ventral) | −7.10 | −14.21 | −0.88 | −3.65 | −21.67 | 4.16 | 0.93 | −10.46 | |||||
| Mean change | −7.92 | −13.57 | −1.44 | −1.51 | −14.84 | 1.69 | −1.16 | −10.46 | |||||
| L4/L5 left (dorsal) | 1.22 | −2.10 | −21.32 | −17.43 | −8.83 | −9.27 | −10.01 | −10.37 | 14.43 | 0.51 | −9.46 | −12.52 | −3.57 |
| L4/L5 right (dorsal) | 1.29 | −3.40 | −4.58 | −15.52 | −6.87 | −8.31 | −14.62 | −3.59 | −6.76 | 0.08 | −9.90 | −19.42 | −9.87 |
| L4/L5 left (ventral) | 1.41 | −2.79 | −14.00 | −22.33 | −8.37 | −10.05 | −3.85 | −2.82 | 5.21 | −4.39 | −4.20 | −10.47 | 1.86 |
| L4/L5 right (ventral) | 2.67 | −3.65 | −5.84 | −15.65 | −6.67 | −9.41 | −10.63 | −7.52 | −13.41 | −0.74 | −7.61 | −15.77 | 2.77 |
| Mean change | 1.65 | −2.99 | −11.44 | −17.73 | −7.69 | −9.26 | −9.78 | −6.08 | −0.13 | −1.14 | −7.79 | −14.55 | −2.20 |
| L5/S1 left (dorsal) | −17.67 | −9.57 | −6.12 | −8.52 | −39.96 | −11.18 | −2.74 | −1.07 | −0.25 | ||||
| L5/S1 right (dorsal) | −5.10 | −10.66 | −5.08 | −10.61 | −23.38 | −2.43 | −9.18 | −2.25 | 0.39 | ||||
| L5/S1 left (ventral) | −6.30 | −8.79 | −11.44 | −9.33 | −18.06 | −7.02 | −1.01 | −1.27 | 1.20 | ||||
| L5/S1 right (ventral) | −3.55 | −7.25 | −9.54 | −12.15 | −13.77 | −4.08 | −5.10 | −3.99 | −0.44 | ||||
| Mean change | −8.16 | −9.07 | −8.05 | −10.15 | −23.79 | −6.18 | −4.51 | −2.15 | 0.23 | ||||
Bold indicates operated level
†Patients who were fused at L5/S1 due to bisegmental osteochondritis
Fig. 3.
Mean post-operative changes in facet joint subchondral bone density. The mean change in subchondral bone density at the operated levels was calculated for all 13 patients. Changes in subchondral bone density for the levels above and below the operated segment were calculated for 12 and 5 patients, respectively. The dotted line represents the 3% significance level. *Subchondral bone density data for indicated level not available. †Indicates patients who were fused due to bisegmental osteochondrosis
Post-operative changes in subchondral bone density at the adjacent levels
Subchondral bone density was studied in the facet joints of the levels adjacent to the operated segment in 12 of the 13 patients. A total of 68 zones in 17 adjacent levels (12 at the level above the operated segment, five at the level below) were studied. Significant decreases in subchondral bone density were recorded in 39/68 (57.4%) zones (Table 3). Of the remaining zones, there was no change in density in 28 (41.2%) zones and a significant increase in density in the remaining one (1.5%) zone. When the mean change in subchondral bone density at the adjacent levels were calculated for each patient, there were significant decreases at the level above the operated segment in 6/12 (50.0%) patients (Fig. 3). In the remaining six (50.0%) patients, there was no overall change in bone density. Subchondral bone density at the level below the operated segment was decreased in 3/5 (60.0%) patients with no change in the remaining two (40.0%) patients. Overall, there was a mean decrease in subchondral bone density of the facet joints at the adjacent levels of 5.42%.
Discussion
Replacement of degenerated lumbar intervertebral discs with the CHARITÉ Artificial Disc was not associated with increased load on the facet joints at the operative or adjacent spinal segments. The distribution of the areas of maximum subchondral bone density were the same pre-operatively and 6 months post-operatively. This provides strong evidence that disc replacement did not lead to additional stress on the facet joints [2, 30]. Decreases in subchondral bone density of the facet joints may indicate a reduction in loading compared with pre-operative facet joint loads and restoration of normal facet joint loading. These morphological findings were accompanied by improvements in clinical outcomes. Considerable improvements in function and quality of life were measured in ODI and SF-36 scores. Pain relief was significant with particularly noticeable improvements in the VAS back pain and SF-36 pain intensity scores.
Do the morphological findings suggest that there was not only an absence of facet joint degeneration upon disc replacement but also a reversal of existing disease? In 10/13 patients, there were significant decreases in the mean subchondral bone density of the facet joints at the operated level. Similar decreases were seen in the facet joints of 9/17 (53%) levels adjacent to the operated segment. Comparable studies in the literature are scarce. Messner et al. [26] reported decreased bone density of rabbit knee joint after sham operation. Increased rest behaviour following sham operation was noted post-operatively. It is unlikely that the decreased subchondral bone density of the facet joints reported in this study was due to post-operative immobilisation of the patients, as normal movement and load-bearing behaviour was achieved between 6 and 8 weeks post-operatively in all patients.
Restoration of intervertebral space height alone would be expected to restore normal facet joint loading and thereby decrease subchondral bone density [13, 22, 34]. Although restored intervertebral space height is likely to contribute to decreased load at the operated level, decreases in subchondral bone density observed in facet joints at adjacent levels in this study indicate that this is not the only factor involved. It is possible that improved segmental kinematics may lead to a decreased load to the facet joints at the adjacent level, as well as contributing to the decreased load at the operated level. Further study is required to establish the baseline for healthy subchondral bone density and to compare this baseline with long-term measurements in patients undergoing disc replacement.
Post-operative lateral and anteroposterior X-rays showed that the CHARITÉ Artificial Disc was not in the ideal position in some patients. However, changes in subchondral bone density in patients with misplaced discs were not different from those in the other patients (data not shown), and thus there appeared to be no functional consequence of these minor misplacements. In previous studies, there was no discernible negative impact on clinical outcome following similar minor misplacements of the CHARITÉ Artificial Disc [7, 24, 40]. Using a non-linear 3D finite element model of the L3/L4 motion segment, Dooris et al. [11] estimated that facet joint loading following ventral misplacement of an artificial disc was 2.5 times greater than in an intact spinal segment. However, the minor misplacement of the CHARITÉ Artificial Disc reported in this study did not appear to affect facet joint loading, as measured by subchondral bone density.
Conclusions
In this study, significant pain relief following disc replacement with the CHARITÉ Artificial Disc was accompanied by morphological observations indicating maintenance of facet joint integrity. In fact, decreases in facet joint subchondral bone density suggest a normalisation of facet joint integrity. It appears likely that these beneficial effects on facet joint integrity are due to restored intervertebral space height and recovered kinematics. Further study is required to confirm these findings.
Acknowledgement
This study was performed in accordance with the laws of Germany.
References
- 1.Adams MA, Hutton WC. The mechanical function of the lumbar apophyseal joints. Spine. 1983;8:327–330. doi: 10.1097/00007632-198304000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Anetzberger H, Muller-Gerbl M, Scherer MA, Metak G, Blumel G, Putz R. Change in subchondral mineralization after reconstruction of the anterior cruciate ligament of the sheep. Unfallchirurg. 1994;97:655–660. [PubMed] [Google Scholar]
- 3.Anetzberger H, Schulz C, Pfahler M, Refior HJ, Muller-Gerbl M. Subchondral mineralization patterns of the glenoid after tear of the supraspinatus. Clin Orthop. 2002;404:263–268. doi: 10.1097/00003086-200211000-00040. [DOI] [PubMed] [Google Scholar]
- 4.Berven S, Tay BB, Colman W, Hu SS. The lumbar zygapophyseal (facet) joints: a role in the pathogenesis of spinal pain syndromes and degenerative spondylolisthesis. Semin Neurol. 2002;22:187–196. doi: 10.1055/s-2002-36542. [DOI] [PubMed] [Google Scholar]
- 5.Brinckmann P, Grootenboer H. Change of disc height, radial disc bulge, and intradiscal pressure from discectomy An in vitro investigation on human lumbar discs. Spine. 1991;16:641–646. doi: 10.1097/00007632-199106000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Butler D, Trafimow JH, Andersson GB, McNeill TW, Huckman MS. Discs degenerate before facets. Spine. 1990;15:111–113. doi: 10.1097/00007632-199002000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Buttner-Janz K, Hahn S, Schikora K, Link HD. Basic principles of successful implantation of the SB Charité model LINK intervertebral disk endoprosthesis. Orthopade. 2002;31:441–453. doi: 10.1007/s00132-001-0297-2. [DOI] [PubMed] [Google Scholar]
- 8.Carter DR, Orr TE, Fyhrie DP. Relationships between loading history and femoral cancellous bone architecture. J Biomech. 1989;22:231–244. doi: 10.1016/0021-9290(89)90091-2. [DOI] [PubMed] [Google Scholar]
- 9.Chen CS, Cheng CK, Liu CL, Lo WH. Stress analysis of the disc adjacent to interbody fusion in lumbar spine. Med Eng Phys. 2001;23:483–491. doi: 10.1016/S1350-4533(01)00076-5. [DOI] [PubMed] [Google Scholar]
- 10.Dai L, Cheng P, Zhang W, Xu Y, Tu K. Stress distribution and bone density in the lumbar spine. Chin Med Sci J. 1992;7:105–107. [PubMed] [Google Scholar]
- 11.Dooris AP, Goel VK, Grosland NM, Gilbertson LG, Wilder DG. Load-sharing between anterior and posterior elements in a lumbar motion segment implanted with an artificial disc. Spine. 2001;26:E122–E129. doi: 10.1097/00007632-200103150-00004. [DOI] [PubMed] [Google Scholar]
- 12.Dreyer SJ, Dreyfuss PH. Low back pain and the zygapophysial (facet) joints. Arch Phys Med Rehabil. 1996;77:290–300. doi: 10.1016/S0003-9993(96)90115-X. [DOI] [PubMed] [Google Scholar]
- 13.Dunlop RB, Adams MA, Hutton WC. Disc space narrowing and the lumbar facet joints. J Bone Joint Surg Br. 1984;66:706–710. doi: 10.1302/0301-620X.66B5.6501365. [DOI] [PubMed] [Google Scholar]
- 14.Fujiwara A, Tamai K, Yamato M, An HS, Yoshida H, Saotome K, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J. 1999;8:396–401. doi: 10.1007/s005860050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geisler FH, Blumenthal SL, Guyer RD, McAfee PC, Regan JJ, Johnson JP, et al. Neurological complications of lumbar artificial disc replacement and comparison of clinical results with those related to lumbar arthrodesis in the literature: results of a multicenter, prospective, randomized investigational device exemption study of Charite intervertebral disc Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1:143–154. doi: 10.3171/spi.2004.1.2.0143. [DOI] [PubMed] [Google Scholar]
- 16.Gillet P. The fate of the adjacent motion segments after lumbar fusion. J Spinal Disord Tech. 2003;16:338–345. doi: 10.1097/00024720-200308000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Goel VK, Goyal S, Clark C, Nishiyama K, Nye T. Kinematics of the whole lumbar spine. Effect of discectomy. Spine. 1985;10:543–554. doi: 10.1097/00007632-198507000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Goto K, Tajima N, Chosa E, Totoribe K, Kubo S, Kuroki H, et al. Effects of lumbar spinal fusion on the other lumbar intervertebral levels (three-dimensional finite element analysis) J Orthop Sci. 2003;8:577–584. doi: 10.1007/s00776-003-0675-1. [DOI] [PubMed] [Google Scholar]
- 19.Haher TR, O’Brien M, Dryer JW, Nucci R, Zipnick R, Leone DJ. The role of the lumbar facet joints in spinal stability. Identification of alternative paths of loading. Spine. 1994;19:2667–2670. [PubMed] [Google Scholar]
- 20.Hochschuler SH, Ohnmeiss DD, Guyer RD, Blumenthal SL. Artificial disc: preliminary results of a prospective study in the United States. Eur Spine J. 2002;11(Suppl 2):S106–S110. doi: 10.1007/s00586-002-0439-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001;10:314–319. doi: 10.1007/s005860000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kummer B. Basics of Pauwels’ theory of the functional adaptation of bones. Orthopade. 1995;24:387–393. [PubMed] [Google Scholar]
- 23.Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 1988;13:375–377. doi: 10.1097/00007632-198803000-00029. [DOI] [PubMed] [Google Scholar]
- 24.Lemaire JP, Skalli W, Lavaste F, Templier A, Mendes F, Diop A, et al. Intervertebral disc prosthesis Results and prospects for the year 2000. Clin Orthop. 1997;337:64–76. doi: 10.1097/00003086-199704000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Lorenz M, Patwardhan A, Vanderby R., Jr Load-bearing characteristics of lumbar facets in normal and surgically altered spinal segments. Spine. 1983;8:122–130. doi: 10.1097/00007632-198303000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Messner K, Fahlgren A, Ross I, Andersson B. Simultaneous changes in bone mineral density and articular cartilage in a rabbit meniscectomy model of knee osteoarthrosis. Osteoarthritis Cartilage. 2000;8:197–206. doi: 10.1053/joca.1999.0290. [DOI] [PubMed] [Google Scholar]
- 27.Milz S, Boszczyk A, Putz R. Development and functional structure of the epiphyseal plate. Orthopade. 2002;31:835–840. doi: 10.1007/s00132-002-0359-0. [DOI] [PubMed] [Google Scholar]
- 28.Moore RJ, Crotti TN, Osti OL, Fraser RD, Vernon-Roberts B. Osteoarthrosis of the facet joints resulting from anular rim lesions in sheep lumbar discs. Spine. 1999;24:519–525. doi: 10.1097/00007632-199903150-00003. [DOI] [PubMed] [Google Scholar]
- 29.Muller-Gerbl M. The subchondral bonelate Advances in anatomy, embryology and cell biology. Springer Berlin and Heidelberg: GmbH & Co; 1998. [DOI] [PubMed] [Google Scholar]
- 30.Muller-Gerbl M, Putz R, Kenn R. Demonstration of subchondral bone density patterns by three-dimensional CT osteoabsorptiometry as a noninvasive method for in vivo assessment of individual long-term stresses in joints. J Bone Miner Res. 1992;7(Suppl 2):S411–S418. doi: 10.1002/jbmr.5650071409. [DOI] [PubMed] [Google Scholar]
- 31.Müller-Gerbl M, Putz R, Hodapp N, Schulte E, Wimmer B. Computed tomography-osteoabsorptiometry for assessing the density distribution of subchondral bone as a measure of long-term mechanical adaptation in individual joints. Skeletal Radiol. 1989;18:507–512. doi: 10.1007/BF00351749. [DOI] [PubMed] [Google Scholar]
- 32.Nachemson A. In vivo discometry in lumbar discs with irregular nucleograms Some differences in stress distribution between normal and moderately degenerated discs. Acta Orthop Scand. 1965;36:418–434. doi: 10.3109/17453676508988651. [DOI] [PubMed] [Google Scholar]
- 33.Panjabi MM, Krag MH, Chung TQ. Effects of disc injury on mechanical behavior of the human spine. Spine. 1984;9:707–713. doi: 10.1097/00007632-198410000-00010. [DOI] [PubMed] [Google Scholar]
- 34.Pauwels F. Short survey of mechanical stress of bone and its importance for the functional adaptation. Z Orthop Ihre Grenzgeb. 1973;111:681–705. [PubMed] [Google Scholar]
- 35.Vernon-Roberts B, Pirie CJ. Degenerative changes in the intervertebral discs of the lumbar spine and their sequelae. Rheumatol Rehabil. 1977;16:13–21. doi: 10.1093/rheumatology/16.1.13. [DOI] [PubMed] [Google Scholar]
- 36.Weishaupt D, Zanetti M, Boos N, Hodler J. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol. 1999;28:215–219. doi: 10.1007/s002560050503. [DOI] [PubMed] [Google Scholar]
- 37.White A, Panjabi M. Clinical biomechanics of the spine. Philadelphia: Lippincott, Williams and Wilkins; 1978. [Google Scholar]
- 38.Wolff J (1892) Das gesetz der transformation der knochen. Hirshwald Berlin
- 39.Yang KH, King AI. Mechanism of facet load transmission as a hypothesis for low-back pain. Spine. 1984;9:557–565. doi: 10.1097/00007632-198409000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Zeegers WS, Bohnen LM, Laaper M, Verhaegen MJ. Artificial disc replacement with the modular type SB Charite III: 2-year results in 50 prospectively studied patients. Eur Spine J. 1999;8:210–217. doi: 10.1007/s005860050160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zollner J, Rosendahl T, Herbsthofer B, Humke T, Eysel P. The effect of various nucleotomy techniques on biomechanical properties of the intervertebral disk. Z Orthop Ihre Grenzgeb. 1999;137:206–210. doi: 10.1055/s-2008-1037394. [DOI] [PubMed] [Google Scholar]