Abstract
Polyetheretherketone (PEEK) is a novel polymer with potential advantages for its use in demanding orthopaedic applications (e.g. intervertebral cages). However, the influence of a physiological environment on the mechanical stability of PEEK has not been reported. Furthermore, the suitability of the polymer for use in highly stressed spinal implants such as intervertebral cages has not been investigated. Therefore, a combined experimental and analytical study was performed to address these open questions. A quasi-static mechanical compression test was performed to compare the initial mechanical properties of PEEK-OPTIMA polymer in a dry, room-temperature and in an aqueous, 37°C environment (n=10 per group). The creep behaviour of cylindrical PEEK polymer specimens (n=6) was measured in a simulated physiological environment at an applied stress level of 10 MPa for a loading duration of 2000 hours (12 weeks). To compare the biomechanical performance of different intervertebral cage types made from PEEK and titanium under complex loading conditions, a three-dimensional finite element model of a functional spinal unit was created. The elastic modulus of PEEK polymer specimens in a physiological environment was 1.8% lower than that of specimens tested at dry, room temperature conditions (P<0.001). The results from the creep test showed an average creep strain of less than 0.1% after 2000 hours of loading. The finite element analysis demonstrated high strain and stress concentrations at the bone/implant interface, emphasizing the importance of cage geometry for load distribution. The stress and strain maxima in the implants were well below the material strength limits of PEEK. In summary, the experimental results verified the mechanical stability of the PEEK-OPTIMA polymer in a simulated physiological environment, and over extended loading periods. Finite element analysis supported the use of PEEK-OPTIMA for load-bearing intervertebral implants.
Keywords: PEEK, Material properties, Creep, Cages, Fusion
Introduction
Polyetheretherketone (PEEK) polymer has been proposed for use in demanding, long-term orthopaedic applications. PEEK is a high-performance biomaterial which combines chemical and hydrolysis resistance, resistance to the effects of ionizing radiation, high strength and good tribological properties with extensive biocompatibility [19, 27, 37]. PEEK is a thermoplastic which can be easily processed into complex implant forms. Moreover, this biomaterial can be repeatedly sterilized using conventional steam, gamma and ethylene oxide processes without significant deterioration.
Implants based on the PEEK polymer have been developed in the last decade as an alternative to conventional metallic devices. PEEK devices may provide several advantages over the use of conventional orthopaedic materials, including the lack of metal allergies, radiolucency, low artefact on magnetic resonance imaging scans and the possibility to tailor mechanical properties [7]. PEEK polymer devices were first reported for fracture fixation, using carbon reinforcement in a PEEK matrix [8, 17]. Iso-elastic, carbon-reinforced PEEK hip prosthesis components have been proposed to address the modulus mismatch between the bone and implant material in order to improve load transfer [2, 3, 18, 34]. Uncoated and titanium-coated PEEK has been suggested for use in dental implantology [9, 11].
The in vivo performance of orthopaedic devices is highly dependent on the intrinsic mechanical properties of the chosen implant material. Bulk mechanical, interfacial and wear properties for hydroxyapatite- and carbon-reinforced PEEK polymers have been reported [1, 4, 8, 23, 25, 39]. However, non-reinforced PEEK is increasingly the material of choice for orthopaedic applications. No data for the initial mechanical properties of pure PEEK polymer in a physiological environment have been published. An aqueous, body temperature environment has been shown to substantially influence the mechanical properties of other medical-grade polymers such as ultra-high molecular weight polyethylene (UHMWPE) [12, 21]. Furthermore, orthopaedic polymers are susceptible to creep, the time dependent, non-recoverable material flow in response to continuous loading, which can result in a significant alteration of implant geometry and biomechanical performance. Creep deformation of pure PEEK in a dry environment has been reported to vary from less than 0.1% per month at room temperature to more than 1% per month at elevated temperatures for stress levels relevant to orthopaedic applications (5–10 MPa) [36].
An increasing number of PEEK devices for interbody fusion are now available. A primary advantage of fusion devices made from PEEK is the undisturbed radiographic evaluation of progression towards bone fusion. The lower elastic modulus of PEEK may minimize stress shielding effects, or even potentially have a stimulatory effect on bone generation [16, 27] and lead to a better fusion than that achieved with metallic cages. Furthermore, PEEK has been shown to be harmless to the spinal cord in site-specific biocompatibility tests [32]. Intervertebral cages are subjected in vivo to complex, three-dimensional loading conditions characterized by high compressive loads which vary spatially and temporally with flexion, extension and side-bending motions. Biomechanical testing and pre-clinical results have recently been reported for PEEK cervical cages and/or anterior plating devices for spinal fusion [10, 13, 20, 20, 24, 33, 38]. While the biomechanical performance of conventional metallic lumbar intervertebral devices has been extensively evaluated through in vitro testing [28] and finite element analysis [30, 31], the performance of PEEK lumbar fusion cages has not been reported.
Polyetheretherketone polymer is a promising material for use in demanding spinal applications. However, the mechanical integrity of the polymer in a physiological environment and its suitability for use in highly stressed implants such as intervertebral cages have not been adequately investigated. Therefore, a combined experimental and analytical study was performed to address these open questions with the following specific goals: (1) to compare the initial mechanical properties of PEEK-OPTIMA in dry, room temperature and in aqueous, body temperature conditions, (2) to determine the creep properties of this material in an aqueous, body-temperature environment and (3) to compare the biomechanical performance of different intervertebral cage types made from the PEEK polymer to that of titanium cages under complex loading conditions.
Methods
Quasi-static compressive testing
A compressive test was designed according to the American Society for Testing and Materials (ASTM) testing standard D695-02 [6] to determine the elastic modulus. Cylindrical test specimens were machined from stock PEEK-OPTIMA LT1 rod material (Grade LTIR30, Invibio, Lancashire, UK), with dimensions 12.7 mm diameter by 50.8 mm length to fulfil the required slenderness ratio of 11–16. Two groups (n=10 per group) were tested. Specimens to be tested in a simulated physiological environment were conditioned in a saline solution (0.15 M NaCl) at 37°C (±1°C) for 48 h before testing. The compressive tests were performed on an MTS 858 Bionix servohydraulic testing machine (MTS Systems Corporation, Eden Prairie, MN, USA). Specimens were compressed at 0.02 mm/s to a maximum load of 5,000 N. The samples were centred under the hydraulic actuator and compressive loads were applied through a ball joint to ensure a purely axial force. The compressive force data were measured by an integrated load cell (±1 N), displacement data were measured by the position of the hydraulic actuator (±1 μm) and collected at a sampling rate of 10 Hz. From force, length and geometric data, the engineering stress and strain were calculated. The modulus of elasticity was determined by taking the tangent to the linear portion of the stress–strain curve. Differences in elastic modulus between groups were evaluated for statistical significance using a Student’s t-test, with a significance level of P=0.05.
Creep testing
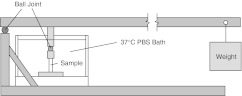
The creep test was based on ASTM D2990-01 [5], with some practical modifications. Cylindrical specimens were machined with a diameter of 6 mm and a length of 22.5 mm to fulfil the required slenderness ratio. A multi-station creep testing apparatus was constructed to load three specimens simultaneously and independently. The testing apparatus was designed to apply a constant vertical load on each of the specimens separately via a second class lever arrangement using weights suspended from a freely-pivoting cantilevered beam (Fig. 1). The load was transferred from the beam to the samples by a ball joint to ensure pure axial compressive loading. Specimens were contained within a saline bath (0.15 M NaCl+0.01% sodium azide to prevent bacterial growth), heated to 37°C (±1°C) by an immersion heater. The samples were conditioned in the bath for 70 h prior to loading. The testing apparatus was placed in a stable environment, free from vibrations. An axial compressive stress of 10 MPa was chosen for the nominal load, based on preliminary finite element analyses of the stress state within representative PEEK intervertebral cage designs during daily activities (unpublished data). Six specimens were loaded and four control samples were kept unloaded for reference in the same bath conditions.
Fig. 1.
Schematic illustration of creep-testing apparatus
The length of each sample was measured prior to loading with a precision micrometer (Mitutoyo, Japan; ±1 μm). The lengths of the samples, loaded and reference, were measured at 6, 12 and 30 min ; 1, 2, 5, 20, 70, 100, 200, 500, 700, 1,000 and 2000 h (12 weeks) after loading was begun. At each of these time points, the samples were briefly unloaded and elastic strain recovery allowed. Each sample was taken out of the bath, blotted quickly and the length measured immediately with the precision micrometer. After each measurement, the loaded samples were replaced in the loading set-up and the reference samples in their reference position. The total time duration of the measurement procedure was approximately 5 min. Although measuring the creep of unloaded specimens is in contrast to the ASTM specification, this procedure has been employed previously for the determination of creep in UHMWPE specimens and eliminates errors in specimen length originating from play in the linkages of the apparatus [22].
Compressive creep was calculated for each specimen by subtracting the specimen length measured at each time interval from the initial length of the specimen. Compressive creep strain was calculated by dividing the compressive creep by the original length of the specimen. Each creep strain measurement was then corrected by subtracting the average strain of the reference samples, measured at the same time and temperature.
Finite element model
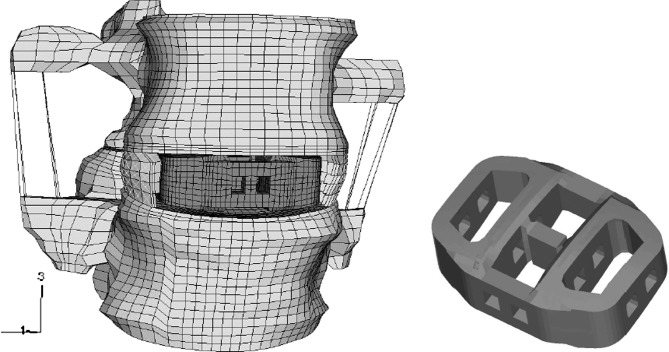
An accurate three-dimensional finite element (FE) model of the convex SynCage-LR (Synthes, Bettlach, CH, USA) was developed and inserted in a validated, three-dimensional, nonlinear FE model of a L2–L3 functional spinal unit (FSU) (Fig. 2). Details of the model development have been given elsewhere [30, 31], and are briefly summarised here. The geometry of the model was based on CT scans of a healthy, young cadaver specimen. The material properties were adapted from previous finite element studies and assumed to be linear, homogeneous and isotropic. For validation, the results of this model were compared to experimental data [14, 29]. The relationship between force and displacement, the resulting nucleus pressure as well as the maximum principal strain at several locations on the vertebra were found to be in good agreement.
Fig. 2.
Finite element model of a L2–L3 functional spinal unit (left) and the SynCage-LR intervertebral cage (right)
An anterior insertion of an intervertebral cage was modelled by removing the anterior longitudinal ligament, the nucleus pulposus and the necessary amount of fibre and annular elements. The cage size was chosen according to the space between the vertebrae, as proposed by the manufacturer, to restore lordosis and disc height..
Changes in the load transfer due to the implantation were investigated comparing intact and instrumented FSUs. Instrumented FSUs included either a modified SynCage (flattened inferior and superior faces) or a convex SynCage-LR made from either PEEK or titanium to assess design and material differences. A nonlinear, three-dimensional contact definition was used between the implant and the neighbouring endplates for the SynCage-LR. Between the surfaces of the simplified, flat SynCage and the anatomically curved endplates, this contact definition was not appropriate. Therefore gap elements were introduced here, with the contact direction chosen perpendicular to the cage surfaces. To include the effect of the small teeth on the original cage surfaces, a friction coefficient of 0.8 was defined for all contact interactions. The model was loaded with either pure axial compression (1,000 N) or pure bending moments (up to 8 Nm, with a 400 N axial compressive preload) in all three anatomical planes. ABAQUS 6.3 was used to solve all models (HKS, Pawtucket, USA).
Results
Material property testing
The modulus of elasticity of PEEK-OPTIMA samples tested in a 37°C aqueous environment was 1.8% lower than that of samples tested in a dry, room temperature environment. The standard deviation of the calculated modulus values was very low. Therefore, while temperature and humidity had a statistically significant (P<0.001) influence on the elastic modulus, the difference was nevertheless small (Table 1).
Table 1.
Initial elastic modulus
| Elastic modulus (GPa) @ Dry, room temperature | Elastic Modulus (GPa) @ Wet, 37°C | |
|---|---|---|
| Average | 3.51 | 3.57 |
| Standard deviation | 0.02 | 0.02 |
The corrected creep strains were plotted as a function of linear and logarithmic time (Fig. 3). The strain increased more rapidly in the first few hours, followed by a reduced rate of creep later in the experiment, approaching a steady state after 2000 hours of loading. Approximately 80% of the total creep strain was achieved within the first 200 h. Creep strain data was best fit by a logarithmic function (r2=0.964) with an average slope of 5.715×10−5 (1/log[min]) for an applied pressure of 10 MPa. The total creep after 2000 hours at a stress level of 10 MPa was less than 0.1%. For comparison, the total corrected creep strain for PEEK polymer tested in a dry, room-temperature environment is approximately 0.04% [36].
Fig. 3.
Average corrected creep strain for PEEK-OPTIMA as a function of a linear and b logarithmic time. The total creep strain after 2000 hours in a 37°C aqueous environment at an applied stress of 10 MPa was on average less than 0.1%. For reference, the corrected creep strain for standard PEEK polymer (450 G) in a dry, 23°C environment is also plotted [34]
Finite element analysis
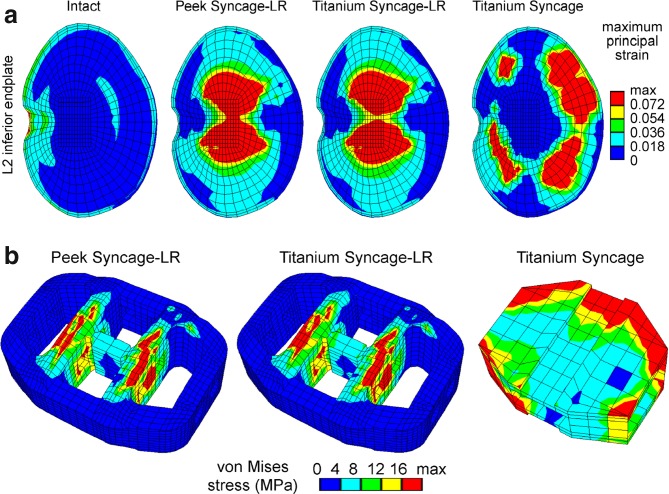
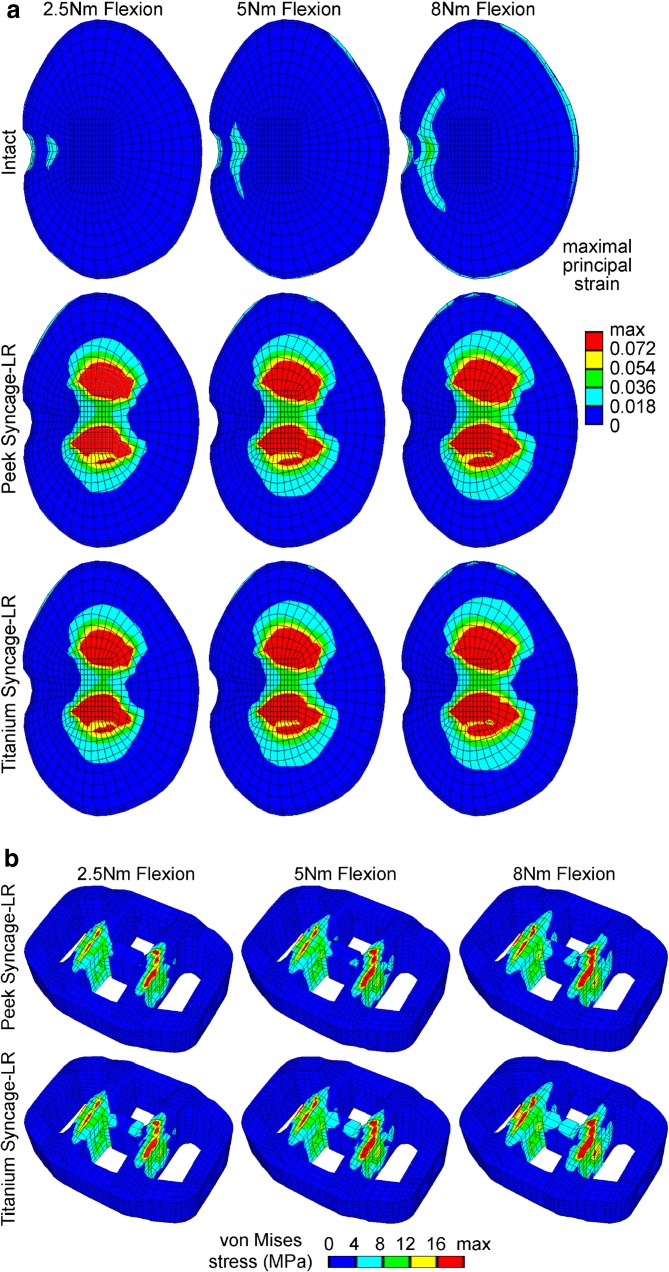
The insertion of an intervertebral cage substantially altered the load transfer through the functional spinal unit for pure compression (Fig. 4), flexion-extension (Fig. 5), lateral bending (Fig. 6) and axial rotation. Stress and strain maxima were increased for all cage types compared to the intact situation. For example, for compression loading, L2 inferior endplate maximum strain values increased by 928% and 923%, respectively, following insertion of titanium and PEEK cages of similar geometry. For flexion loading, maximum strain values within the cancellous bone of L3 increased by 719% and 741%, respectively, following insertion of PEEK and titanium cages. Similar trends were observed for all loading conditions. Differences in the altered stress and strain distributions were more evident between the two cage designs (flat SynCage vs. convex SynCage-LR) than for the two materials investigated (PEEK and titanium), Fig. 4a. Maximum contact stresses with the flat SynCage tended to be locally distributed around the periphery of the implant, whereas the contact stresses with the SynCage-LR were more evenly distributed across the centre of the endplate.
Fig. 4.
a Maximal principal strain distribution in the inferior L2 endplate due to 1,000 N of compression. From left to right Intact, PEEK SynCage-LR, titanium SynCage-LR, flat SynCage. b Von Mises stress distribution in the cages due to 1,000 N of compression. From left to right PEEK SynCage-LR, titanium SynCage-LR, flat SynCage
Fig. 5.
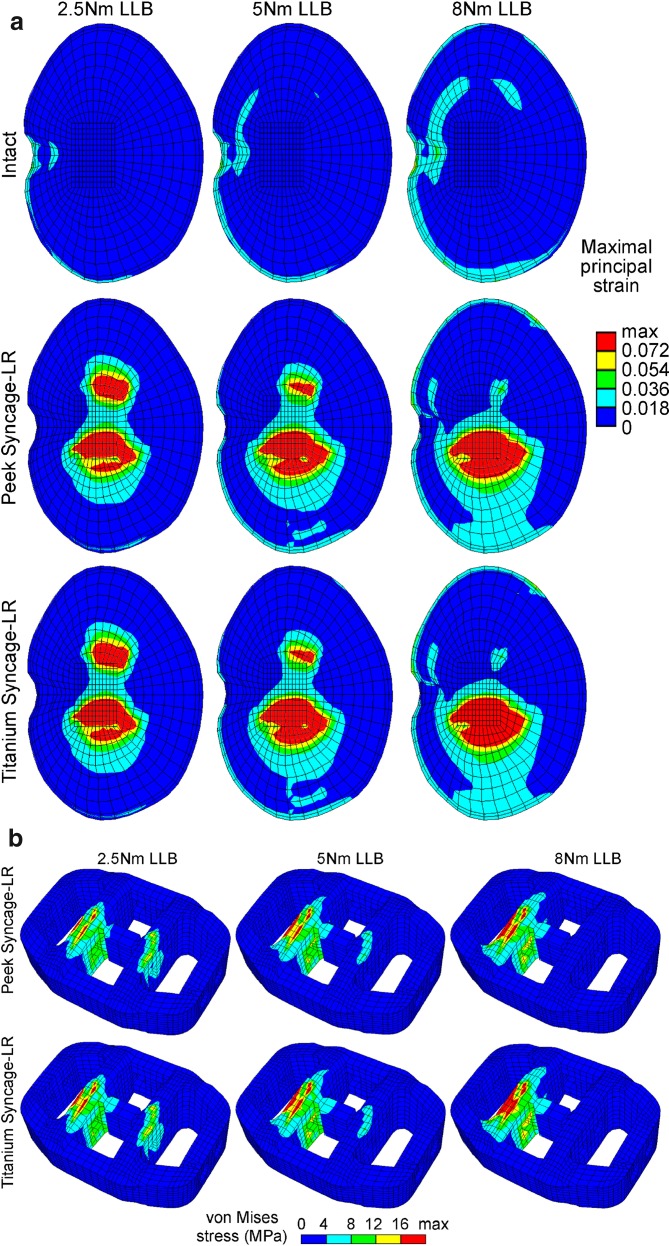
a Maximal principal strain in the inferior endplate of L2 due to flexion. From left to right 2.5 Nm, 5 Nm, 8 Nm. From top to bottom Intact, PEEK SynCage-LR, titanium SynCage-LR. b Von Mises stress in the SynCage-LR due to flexion. From left to right 2.5 Nm, 5 Nm, 8 Nm. Top row PEEK SynCage-LR, bottom row Titanium SynCage-LR
Fig. 6.
a Maximal principal strain in the inferior endplate of L2 due to left lateral bending. From left to right 2.5 Nm, 5 Nm, 8 Nm. From top to bottom Intact, PEEK SynCage-LR, titanium SynCage-LR. b Von Mises stress in the SynCage-LR due to left lateral bending. From left to right 2.5 Nm, 5 Nm, 8 Nm. Top row PEEK SynCage-LR, bottom row Titanium SynCage-LR
Regarding the material differences, titanium cages produced increased areas of high strain within the adjacent vertebrae under compression and lateral bending. Additionally the resulting strain maxima were different: for 8 Nm of flexion, for example, the strain maximum in the cancellous bone of L3 was 22% higher, following the insertion of a titanium cage than after the implantation of one made from PEEK. In the cages themselves, slightly lower stresses and decreased areas of high stresses were seen in a SynCage-LR made from PEEK, compared to an identical design in titanium, for compression, flexion, lateral bending and axial rotation, Figs. 4b, 5b, 6b. Maximum von Mises stresses within the PEEK cage were 45.7 MPa, 31.5 MPa, 52.6 MPa and 32.7 MPa for 1,000 N compression, 8 Nm flexion, 8 Nm lateral bending and 2.5 Nm axial rotation respectively.
Numerical singularities precluded solution of the intact model for extension moments greater than 5 Nm and axial rotation greater than 2.5 Nm for the models including a cage.
Discussion
Although PEEK has been proposed for use in demanding orthopaedic applications, the mechanical integrity of the polymer in a physiological environment has not been documented. Furthermore, the suitability of the polymer for use in highly stressed implants such as intervertebral cages and the potential biomechanical advantages of PEEK implants for spinal applications have not been investigated. Therefore, a combined experimental and analytical study was performed to address these open questions.
Testing in an aqueous 37°C environment showed a statistically significant but marginal influence on the initial mechanical properties of PEEK-OPTIMA. The measured difference in properties would not invalidate implant designs based on previously published material properties obtained in a dry, room temperature testing. PEEK-OPTIMA can therefore be considered mechanically stable in vivo, as it does not demonstrate the substantial changes in mechanical properties with temperature and hydration which have been observed for other medical grade polymers such as polyurethanes and polyethylenes [12, 21]. Nevertheless, final proof-testing of PEEK orthopaedic implants should be conducted in a simulated physiological environment.
The method used to measure total polymer creep did not fully conform to the ASTM testing standard. However, the chosen method eliminates inaccuracies that could be caused by play in the testing apparatus, and the same method has been used previously to determine the creep characteristics of polyethylene [22]. Furthermore, the static compressive loading represents a worst-case loading scenario for creep measurements, as no recovery of the specimens is allowed throughout the testing, in contrast to the dynamic loading experienced in vivo. The total test duration of 2000 hours far exceeds the test duration previously reported for polyethylene [22] and represents a more physiological relevant loading duration for implants designed to aid spinal fusion. The creep rate determined for PEEK-OPTIMA was approximately two orders of magnitude lower than that previously measured for medical grade polyethylene [22], whereas the total deformation of PEEK-OPTIMA was slightly increased in a 37°C, aqueous environment when compared to that measured at room temperature in a dry environment [36]. In practice, the total non-recoverable deformation of PEEK-OPTIMA would be negligible, with maximum 0.1% strain after 2000 hours at a stress level of 10 MPa, vanishingly small, compared to the time-dependent changes which could be expected in the surrounding bone due to remodelling effects. The reference samples expanded slightly during the experiment, most likely due to fluid absorption. Therefore, water absorption may counteract creep in vivo, and the corrected creep strain measured here can be considered a conservative estimate of the material’s creep behaviour. These results verify the mechanical stability of the PEEK-OPTIMA polymer in a simulated physiological environment, and over extended loading periods.
The finite element analyses approximated the loading situation existing in the initial time period after the implantation. Following cage insertion, high strains and stresses were concentrated in the contact areas between the cage and endplate, underlining the importance of sufficiently large contact zones. Contact stresses below the anatomically-shaped implant with curved surfaces tended to be more broadly distributed across the central endplate, whereas contact stresses around the flat implants tended to be concentrated around the periphery of the device. However, it has been shown previously that the local endplate strength increases towards the outer edges [15], and the integrity of similar intervertebral cage designs, relying only on peripheral support, has been demonstrated in previous experimental testing [35]. For the rather demanding loading conditions applied in the simulations, the determined maximum principal strains approached the limits of the elastic definition used for the materials in this model. Calculated local bone strains might exceed the yield strain reported for vertebral trabecular bone [26], so the possibility of local bone changes in response to mechanical loading cannot be excluded and implant subsidence may occur. However, this initial settling period might offer the possibility to achieve a larger, more congruent contact interface between cage and endplates, and in consequence, an enhanced stability. Furthermore, anterior lumbar interbody fusion with a standalone cage, as represented in this model, is a mechanically demanding application. The addition of supplemental posterior fixation (e.g. translaminar facet screws), a commonly used adjunt to the anterior implant, would provide a substantial load-sharing capacity and reduce the level of stresses generated within the vertebral bodies.
For the applied forces and moments, representing everyday loads, the stress and strain values determined in the cages themselves never approached the limits of the polymer’s or titanium’s intrinsic material strength. The resulting differences in load transfer due to the two cage materials were relatively small; nevertheless, a slight trend towards a more pronounced stress-shielding situation with titanium cages might be concluded from our results.
Model solutions could not be obtained for certain loading cases. The complexity of the contact definition at the cage-endplate interface, in conjunction with a realistic interface shape mismatch, resulted in a failure of the model solution at high extension and rotation moments. This numerical instability is consistent with experimental results demonstrating the limitations of standalone cages to stabilize a spinal motion segment under these types of loadings [28].
In summary, our experimental and finite element analysis established that PEEK-OPTIMA is a suitable material for load-bearing implants in the human body. Used in intervertebral cages, it performs at least as well as similar titanium implants, additionally offering the possibility of undisturbed radiographic fusion control due to its radio-translucency and potential benefits for the stimulation of bone formation due to the close match between the mechanical properties of the polymer and host bone.
Acknowledgements
PEEK-OPTIMA material provided by Invibio, Lancashire, UK. Financial support provided by Mathys Medical Ltd., Bettlach, Switzerland.
Footnotes
PEEK-OPTIMA is a specific medical grade of PEEK, supplied for use in human implantable devices.
References
- 1.Abu Bakar MS, Cheng MH, Tang SM, Yu SC, Liao K, Tan CT, Khor KA, Cheang P. Tensile properties, tension–tension fatigue and biological response of polyetheretherketone-hydroxyapatite composites for load-bearing orthopedic implants. Biomaterials. 2003;24:2245–2250. doi: 10.1016/S0142-9612(03)00028-0. [DOI] [PubMed] [Google Scholar]
- 2.Akay M, Aslan N. An estimation of fatigue life for a carbon fibre/poly ether ether ketone hip joint prosthesis. Proc Inst Mech Eng [H] 1995;209:93–103. doi: 10.1243/PIME_PROC_1995_209_325_02. [DOI] [PubMed] [Google Scholar]
- 3.Akay M, Aslan N. Numerical and experimental stress analysis of a polymeric composite hip joint prosthesis. J Biomed Mater Res. 1996;31:167–182. doi: 10.1002/(SICI)1097-4636(199606)31:2<167::AID-JBM3>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 4.Albert K, Schledjewski R, Harbaugh M, Bleser S, Jamison R, Friedrich K. Characterization of wear in composite material orthopaedic implants. Part II: The implant/bone interface. Biomed Mater Eng. 1994;4:199–211. [PubMed] [Google Scholar]
- 5.ASTM D2990–01 (2004) Standard test methods for tensile, compressive, and flexural creep and creep-rupture of plastics
- 6.ASTM D695–02 (2004) Standard test method for compressive properties of rigid plastics
- 7.Baidya KP, Ramakrishna S, Rahman M, Ritchie A. Quantitative radiographic analysis of fiber reinforced polymer composites. J Biomater Appl. 2001;15:279–289. doi: 10.1106/BKLQ-E2YG-D2LA-RG3R. [DOI] [PubMed] [Google Scholar]
- 8.Brown SA, Hastings RS, Mason JJ, Moet A. Characterization of short-fibre reinforced thermoplastics for fracture fixation devices. Biomaterials. 1990;11:541–547. doi: 10.1016/0142-9612(90)90075-2. [DOI] [PubMed] [Google Scholar]
- 9.Chabrier F, Lloyd CH, Scrimgeour SN. Measurement at low strain rates of the elastic properties of dental polymeric materials. Dent Mater. 1999;15:33–38. doi: 10.1016/S0109-5641(99)00011-1. [DOI] [PubMed] [Google Scholar]
- 10.Cho DY, Liau WR, Lee WY, Liu JT, Chiu CL, Sheu PC. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery. 2002;51:1343–1349. doi: 10.1097/00006123-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Cook SD, Rust-Dawicki AM. Preliminary evaluation of titanium-coated PEEK dental implants. J Oral Implantol. 1995;21:176–181. [PubMed] [Google Scholar]
- 12.Cripton PA (1993) Compressive characterization of ultra high molecular weight polyethylene with applications to contact stress analysis of total knee replacments. MSc Thesis, Queen’s University
- 13.Diedrich O, Kraft CN, Perlick L, Schmitt O. The posterior lumbar interbody fusion with cages (PLIF) and transpedicular stabilization. Zentralbl Neurochir. 2001;62:106–113. doi: 10.1055/s-2001-21796. [DOI] [PubMed] [Google Scholar]
- 14.Frei H, Oxland TR, Rathonyi GC, Nolte LP. The effect of nucleotomy on lumbar spine mechanics in compression and shear loading. Spine. 2001;26:2080–2089. doi: 10.1097/00007632-200110010-00007. [DOI] [PubMed] [Google Scholar]
- 15.Grant JP, Oxland TR, Dvorak MF. Mapping the structural properties of the lumbosacral vertebral endplates. Spine. 2001;26:889–896. doi: 10.1097/00007632-200104150-00012. [DOI] [PubMed] [Google Scholar]
- 16.Hunter A, Archer CW, Walker PS, Blunn GW. Attachment and proliferation of osteoblasts and fibroblasts on biomaterials for orthopaedic use. Biomaterials. 1995;16:287–295. doi: 10.1016/0142-9612(95)93256-D. [DOI] [PubMed] [Google Scholar]
- 17.Jockisch KA, Brown SA, Bauer TW, Merritt K. Biological response to chopped-carbon-fiber-reinforced peek. J Biomed Mater Res. 1992;26:133–146. doi: 10.1002/jbm.820260202. [DOI] [PubMed] [Google Scholar]
- 18.Katoozian H, Davy DT, Arshi A, Saadati U. Material optimization of femoral component of total hip prosthesis using fiber reinforced polymeric composites. Med Eng Phys. 2001;23:503–509. doi: 10.1016/S1350-4533(01)00079-0. [DOI] [PubMed] [Google Scholar]
- 19.Katzer A, Marquardt H, Westendorf J, Wening JV, von FG. Polyetheretherketone–cytotoxicity and mutagenicity in vitro. Biomaterials. 2002;23:1749–1759. doi: 10.1016/S0142-9612(01)00300-3. [DOI] [PubMed] [Google Scholar]
- 20.Krammer M, Dietl R, Lumenta CB, Kettler A, Wilke HJ, Buttner A, Claes L. Resistance of the lumbar spine against axial compression forces after implantation of three different posterior lumbar interbody cages. Acta Neurochir (Wien) 2001;143:1217–1222. doi: 10.1007/s007010100017. [DOI] [PubMed] [Google Scholar]
- 21.Kurtz SM, Villarraga ML, Herr MP, Bergstrom JS, Rimnac CM, Edidin AA. Thermomechanical behavior of virgin and highly crosslinked ultra-high molecular weight polyethylene used in total joint replacements. Biomaterials. 2002;23:3681–3697. doi: 10.1016/S0142-9612(02)00102-3. [DOI] [PubMed] [Google Scholar]
- 22.Lee KY, Pienkowski D. Compressive creep characteristics of extruded ultrahigh-molecular-weight polyethylene. J Biomed Mater Res. 1998;39:261–265. doi: 10.1002/(SICI)1097-4636(199802)39:2<261::AID-JBM13>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 23.Maharaj G, Bleser S, Albert K, Lambert R, Jani S, Jamison R. Characterization of wear in composite material orthopaedic implants. Part I: the composite trunnion/ceramic head interface. Biomed Mater Eng. 1994;4:193–198. [PubMed] [Google Scholar]
- 24.Matge G. Cervical cage fusion with 5 different implants: 250 cases. Acta Neurochir (Wien) 2002;144:539–549. doi: 10.1007/s00701-002-0939-0. [DOI] [PubMed] [Google Scholar]
- 25.Meyer MR, Friedman RJ, Del SH, Jr, Latour RA., Jr Long-term durability of the interface in FRP composites after exposure to simulated physiologic saline environments. J Biomed Mater Res. 1994;28:1221–1231. doi: 10.1002/jbm.820281012. [DOI] [PubMed] [Google Scholar]
- 26.Morgan EF, Keaveny TM. Dependence of yield strain of human trabecular bone on anatomic site. J Biomech. 2001;34:569–577. doi: 10.1016/S0021-9290(01)00011-2. [DOI] [PubMed] [Google Scholar]
- 27.Morrison C, Macnair R, MacDonald C, Wykman A, Goldie I, Grant MH. In vitro biocompatibility testing of polymers for orthopaedic implants using cultured fibroblasts and osteoblasts. Biomaterials. 1995;16:987–992. doi: 10.1016/0142-9612(95)94906-2. [DOI] [PubMed] [Google Scholar]
- 28.Oxland TR, Lund T. Biomechanics of stand-alone cages and cages in combination with posterior fixation: a literature review. Eur Spine J. 2000;9((Suppl 1)):S95–S101. doi: 10.1007/PL00010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Polikeit Finite element analysis of the lumbar. 2002;spine:clinical. [Google Scholar]
- 30.Polikeit A, Ferguson SJ, Nolte LP, Orr TE. Factors influencing stresses in the lumbar spine after the insertion of intervertebral cages: finite element analysis. Eur Spine J. 2003;12:413–420. doi: 10.1007/s00586-002-0505-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Polikeit A, Ferguson SJ, Nolte LP, Orr TE. The importance of the endplate for interbody cages in the lumbar spine. Eur Spine J. 2003;12:556–561. doi: 10.1007/s00586-003-0556-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rivard CH, Rhalmi S, Coillard C. In vivo biocompatibility testing of peek polymer for a spinal implant system: a study in rabbits. J Biomed Mater Res. 2002;62:488–498. doi: 10.1002/jbm.10159. [DOI] [PubMed] [Google Scholar]
- 33.Schulte M, Schultheiss M, Hartwig E, Wilke HJ, Wolf S, Sokiranski R, Fleiter T, Kinzl L, Claes L. Vertebral body replacement with a bioglass-polyurethane composite in spine metastases—clinical, radiological and biomechanical results. Eur Spine J. 2000;9:437–444. doi: 10.1007/s005860000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Soyer J. Experimental protocol for mechanical characterization of a femoral implant of carbon-Peek composite hip prosthesis in fatigue. Chirurgie. 1997;121:658–662. [PubMed] [Google Scholar]
- 35.Steffen T, Tsantrizos A, Aebi M. Effect of implant design and endplate preparation on the compressive strength of interbody fusion constructs. Spine. 2000;25:1077–1084. doi: 10.1097/00007632-200005010-00007. [DOI] [PubMed] [Google Scholar]
- 36.http://www.victrex.com/uk/pdfclickthru.asp?pdf=VicPropertiesUK.pdf
- 37.Wenz LM, Merritt K, Brown SA, Moet A, Steffee AD. In vitro biocompatibility of polyetheretherketone and polysulfone composites. J Biomed Mater Res. 1990;24:207–215. doi: 10.1002/jbm.820240207. [DOI] [PubMed] [Google Scholar]
- 38.Wilke HJ, Kettler A, Claes L. Stabilizing effect and sintering tendency of 3 different cages and bone cement for fusion of cervical vertebrae segments. Orthopade. 2002;31:472–480. doi: 10.1007/s00132-001-0288-3. [DOI] [PubMed] [Google Scholar]
- 39.Zhang G, Latour RA, Jr, Kennedy JM, Del SH, Jr, Friedman RJ. Long-term compressive property durability of carbon fibre-reinforced polyetheretherketone composite in physiological saline. Biomaterials. 1996;17:781–789. doi: 10.1016/0142-9612(96)81415-3. [DOI] [PubMed] [Google Scholar]