Abstract
Direct comparison of the correction of scoliosis achieved by different surgical methods is usually limited by the heterogeneity of the patients analyzed (their age, curve pattern, curve magnitude, etc.). The hypothesis is that an analysis of comparable scoliotic curves treated by different implant systems could detect subtle differences in outcome. The objective of this study was therefore: (1) to measure the 3D radiological parameters of scoliotic deformity and to quantify their postoperative changes, and (2) to compare the radiographic results achieved with one anterior and one posterior instrumentation methods applied to similar curves but representing different mechanisms of correction. Material and methods: The clinical notes and radiographs of 46 patients operated on for adolescent idiopathic scoliosis were reviewed. The inclusion criteria consisted of: a single thoracic curve, right convex, a frontal Cobb angle minimum of 45° and a maximum of 65°, flexibility on a lateral bending test of more than 30%, and a Risser test value of between 1 and 4. The operative procedures were: Cotrel-Dubousset instrumentation (CDI) for 25 patients (the CD group) and correction by anterior instrumentation (Pouliquen plate) for 21 patients (the ANT group). Preoperative and postoperative long cassette standing antero-posterior and lateral radiographs were examined. The frontal and sagittal thoracic Cobb angle, apical vertebra transposition (AVT), apical vertebra rotation (AVR), lowest instrumented vertebra (LIV) tilt, C7 vertebra shift and rib cage shift (RCS) were all compared. A computed reconstruction was produced with Rachis-91 software. Vertebral axial rotation angle was evaluated throughout the spine. Results: Postoperative assessment revealed a mean correction of the frontal Cobb angle of 37.0° for the CD group and 41.0° for the ANT group. The AVT operative correction was 45.8 and 42.7 mm, respectively, and AVR correction was 1.8 and 12.6°, respectively. The postoperative change of the sagittal Th4–Th12 Cobb angle was not significant for any method but it was significant (P=0.05) for the CD group if the curves were divided preoperatively into hypokyphotic and normokyphotic subgroups and then analyzed separately. Computed assessment demonstrated a correction of segmental axial rotation of more than 50% in the main thoracic curve in the ANT group, significantly more than that in the CD group (P<0.001). Conclusions: Anterior instrumentation provided better correction of the vertebral axial rotation and of the rib hump. CD instrumentation was more powerful in translation and more specifically addressed the sagittal plane: the postoperative thoracic kyphosis angle increased in the hypokyphotic curves and slightly decreased in the normokyphotic curves.
Keywords: 3D scoliosis correction
Introduction
The objective of surgical treatment of idiopathic scoliosis is to obtain a stable and balanced spine. The correction of the primary curve should be 3D [12]. Rotational deformity of the thoracic spine, developing in the transverse plane, and clinically expressed by the rib hump is probably the most difficult to address. Recently attention has been paid to the potential value of anterior surgery [1, 8, 14, 17, 21, 23]. An anterior approach spares the posterior back muscles, shortens the anterior column of the spine and provides a powerful force arm to rotate the vertebrae of the apical zone [14, 21]. Anterior surgery can avoid the fusion of one or even more vertebrae [1] and probably helps to avoid the crankshaft phenomenon [11] in immature patients. The quality of the interbody fusion appears equal that with the posterior fusion. On the other hand, the approach is considered more demanding, any subsequent hardware or septic complications are more difficult to treat and the long-term respiratory involvement of the transpleural approach is not clear.
We focused our study on biomechanical differences of correction of single thoracic curve with anterior versus posterior instrumentation. We believed that comparing 3D radiological patomorphology of spinal curves could assess them. Cotrel-Dubousset instrumentation (CDI) [6, 7] was taken for posterior correction while Pouliquen anterior plate [24] was chosen for anterior system. Although the comparison of devices is less interesting, comparing the mechanisms seems to be clinically important. We propose to consider different implant systems according to: (1) the number of implant sites, determining the number of available fixation points, (2) the anatomic location of implant sites in the vertebra, indicating the points of application of the corrective force, (3) the direction of the corrective force.
The two methods compared in our study represent markedly different mechanisms of action. The posterior Cotrel-Dubousset segmental multiple hook system involves a “derotation maneuver” with a prebent rod. It applies translation forces to the posterior elements (laminae, articular processes) of so-called strategic vertebrae of the curve. A multi-point application of the corrective force is provided and the direction of this corrective force is transverse, even if additional distraction is sometimes applied to the concavity. For an anterior instrumentation method, we have referred to the vertebral plating technique, practiced in a few centers whose medium-term results have already been published [24]. This system provides a segmental action and applies transverse forces to the vertebral bodies of the primary curve. The technique consists of a transpleural approach, through a single thoracotomy without detachment of the diaphragm, if the lowest instrumented level is not below L1. After the discs and cartilaginous vertebral end plates are removed, a titanium plate contoured for kyphosis is applied to the lateral surface of vertebral bodies on the convex side of the curve and gradually fixed with spongieous screws [24]. All vertebrae of primary curve are instrumented.
Several anterior devices have been developed including the anterior TSRH [28], Harms-MOSS [1], Zielke [20, 31], Halm [14], Hopf [17] and Eclipse [23]. Comparison of the correction obtained after anterior versus posterior surgery can be made directly if similar curves are instrumented by each technique. In practice the anterior approach is mainly used for lumbar and thoracolumbar curves [1, 14, 28] while posterior instrumentation is often preferred for the thoracic level. That is why we attempted to evaluate the correction achieved with two different implant systems applied to groups of patients with scoliosis of a comparable pattern and degree of deformity. Due to this initial selection, the scoliotic curves presented similar mechanical properties and the postoperative morphology of the spines could be directly compared. Factors such as morbidity, blood loss, extensiveness of anterior versus posterior liberation of the curve, instrumentation complexity, quality of spinal fusion, postoperative bracing or the cost of treatment were not analyzed in this study.
Material
The criteria for inclusion in the study were as follows: an adolescent idiopathic single right thoracic curve (Lenke type 1 [27], King type 3 [18]), the superior limit vertebra at Th4 or Th5, apical vertebra at Th8 or Th9, the inferior limit vertebra at Th12 or L1, a Cobb angle [5] value of 45° minimum and 65° maximum, angular correction of the thoracic curve on a lateral bending radiograph of 30% minimum, the presence of a compensatory non-structural left lumbar curve fully corrected on a lateral bending test, the presence of a compensatory non-structural left upper thoracic curve, limited proximally by a horizontal Th1 vertebra, the lowest instrumented vertebra (LIV) not below L2, a Risser test [25] value of one minimum and four maximum, females after the menarche, no previous brace treatment and with full documentation accessible.
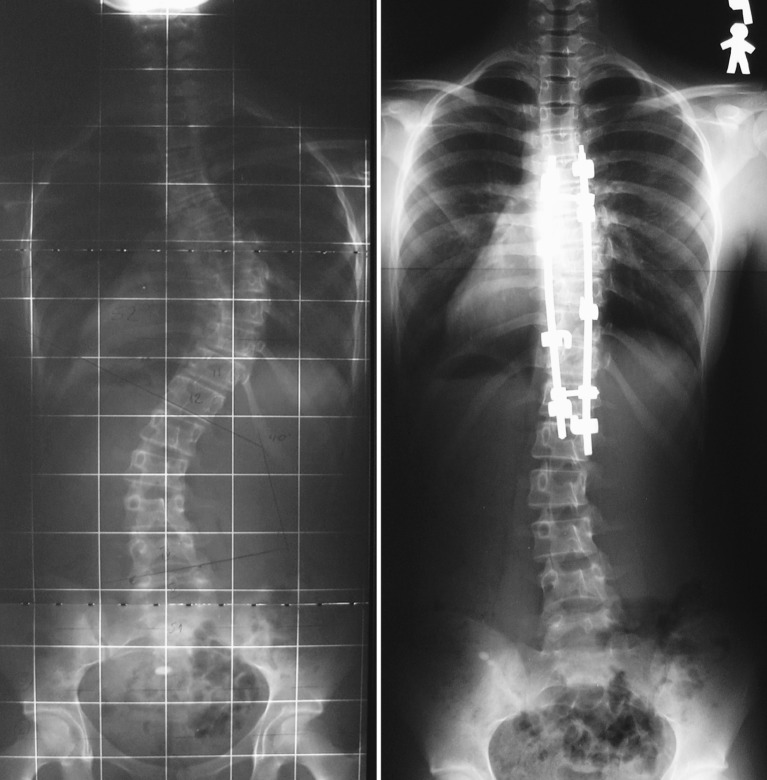
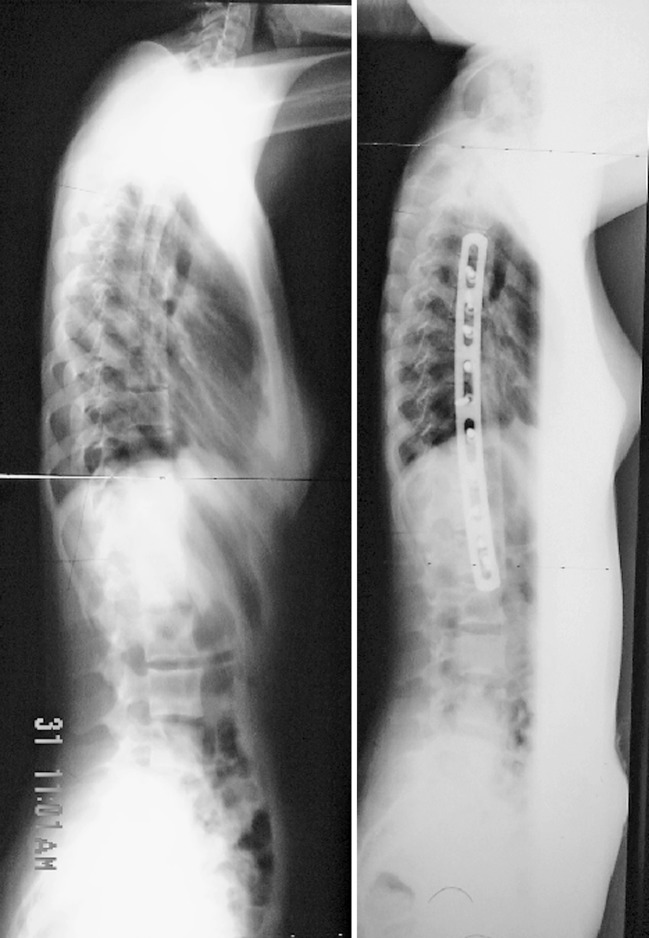
The clinical charts and radiographs of 46 patients were evaluated. About 25 patients underwent CDI at the Institution 1 (the CD group, Fig. 1). Twenty-one patients were corrected by anterior plating at the Institution 2 (the ANT group, Fig. 2).
Fig. 1.
Preoperative and postoperative frontal radiographs of a patient from CD group
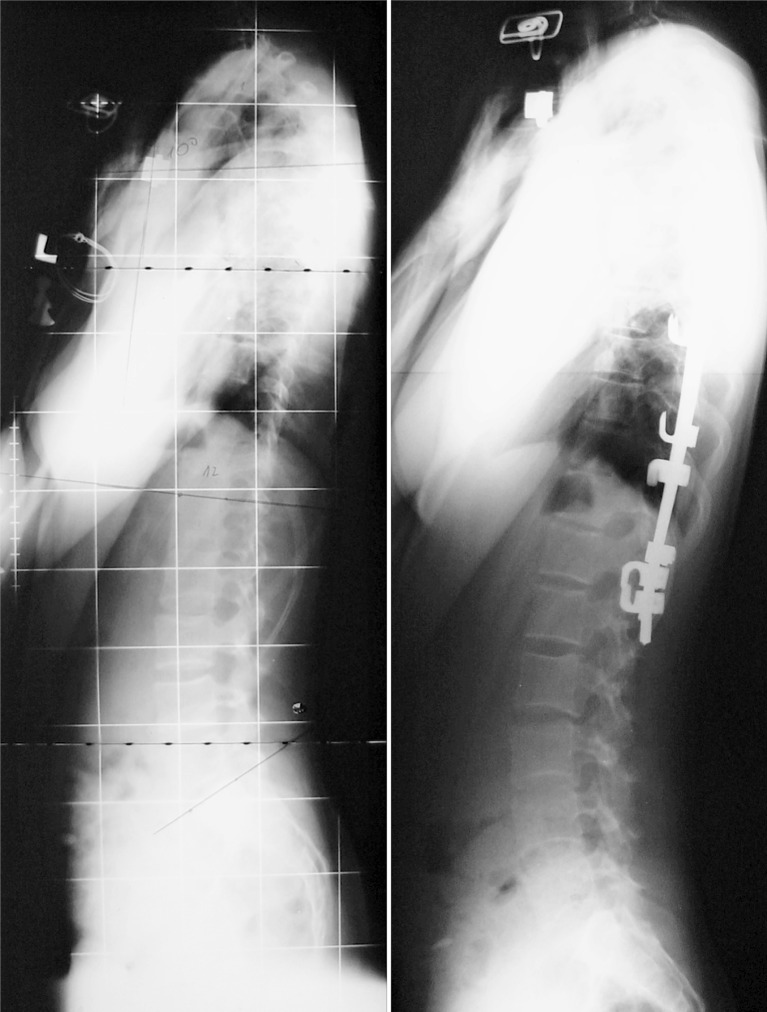
Fig. 2.
a Preoperative and postoperative frontal radiograph of a patient from ANT group. b Preoperative and postoperative lateral radiograph of a patient from ANT group
The 25 patients of the CD group represented a consecutive series of patients meeting the inclusion criteria and having suitable documentation derived from 342 CD procedures executed in the Hôpital Saint Vincent-de-Paul, Paris 1989–1994. The mean follow-up was of 3.5 years (from 2 to 8 years). The 21 patients of the ANT group were representative of the 235 patients who fulfilled the inclusion criteria, and who were treated by anterior plating in the Hôpital Necker-Enfants Malades, Paris between 1977 and 1995. The mean follow-up was of 6 years (from 2 to 19 years).
The CD group included 20 girls and five boys, and the ANT group 17 girls and four boys. In all cases the instrumentation and fusion involved the whole thoracic curve from the superior limit vertebra to the inferior limit vertebra. In the CD group the LIV was the inferior limit vertebra in ten cases, one level below the inferior limit vertebra in 14 cases and two levels below in one case. In the ANT group the LIV was the inferior limit vertebra in five cases, one level below the inferior limit vertebra in 12 cases and two levels below the inferior limit vertebra in four cases. Of the 46 curves, the LIV was Th12 in six cases, L1 in 26 cases and L2 in 14 cases. The rest of the lumbar spine was spared from fusion. An iliac autograft and rib autograft were used during posterior and anterior surgery, respectively, to enhance the spinal fusion.
Methods
The patients’ height and the rib hump height on Adams’ forward bending test were noted. No surface topography of the patients was recorded and no more clinical data suitable for statistical analyses were found in the charts.
Standing antero-posterior and lateral radiographs included the whole spine and pelvis (long cassette) [10]. The pelvis in each case was level. The following elements were defined on each radiograph: the superior and inferior limit vertebra, the apical vertebra, the LIV, the central sacral line (CSL) [18], the stable vertebra of King [18]. The CSL was drawn as a vertical line bisecting the sacrum (CSVL) [19].
The following parameters were measured on the radiographs: the frontal Cobb angle [5], the sagittal thoracic Cobb angle between the superior plate of Th4 and the inferior plate of Th12, the apical vertebra transposition (AVT) defined as the distance between the CSL and the center of the apical vertebra or the center of the apical disc, the apical vertebra axial rotation (AVR) according to Perdriolle [22], the tilt of the LIV, the C7 shift defined as the horizontal distance from the CSL to the tip of the spinous process of C7, and the rib cage shift (RCS) defined as the difference of two horizontal distances from the CSL to the most lateral thoracic contour: one on the convex and the other on the concave side. For the AVT, C7 shift and the RCS, positive values denoted rightward displacement and negative values denoted leftward displacement as measured from the CSL. For the sagittal Cobb angle, negative values denoted lordosis between Th4 and Th12. For the LIV tilt, negative values denoted a vertebral tilt towards the left.
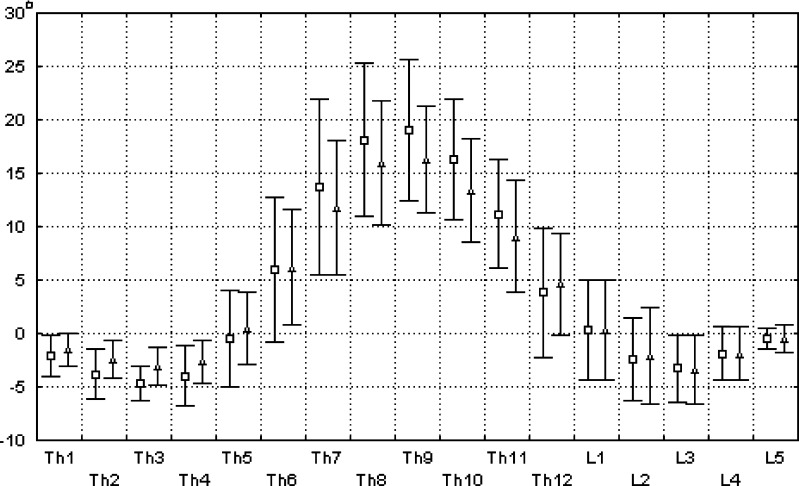
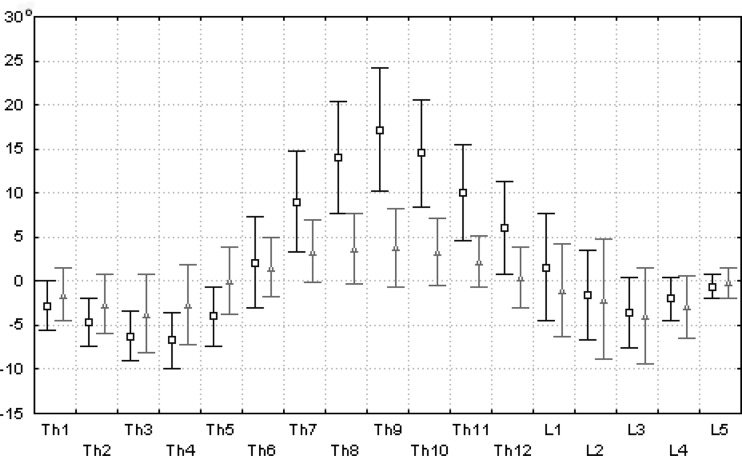
The 3D reconstruction of radiographs was made according to direct linear transformation principles [4, 16]. From the a-p and lateral radiographs the aspects of the thoracic, lumbar, and sacral vertebrae were digitized by means of a sonic digitizer GP-9 (SAC, USA) connected to a standard PC. The software was RACHIS 91TM made by Hecquet and Rachis [15] and Graf et al. [13]. Apart from the C7 shift and the rib cage shift, all the parameters previously measured manually, were calculated by the program and analyzed segmentally. A view of the spine from above (top view) was created for each curve. Preoperative and postoperative vertebral axial rotation angles were calculated by the RACHIS software for each segment and compared between the two groups (Figs. 3, 4).
Fig. 3.
Segmental vertebral axial rotation angle (in degrees) in the ANT group (N=21) measured by RACHIS software according to the Perdriolle method. The values are presented as the mean ± SD for each vertebral level. Squares indicate mean preoperative values and triangles indicate mean postoperative values
Fig. 4.
Segmental vertebral axial rotation angle (in degrees) in the CD group (N=25) measured by RACHIS software according to Perdriolle’s method. The values are presented as the mean ± SD for each vertebral level. Squares indicate mean preoperative values and triangles indicate mean postoperative values
A comparison of the preoperative parameters was made to assess the initial similarity of groups. All the parameters were also compared postoperatively. The minima, maxima, means and standard deviations were calculated for each parameter. The normal distribution was determined. The Student’s t-test was used for normal ranged parameters, and the Mann–Whitney or Wilcoxon test for not normal range. The parameters measured manually were compared with those calculated by the RACHIS software, and the correlation was established using the Pearson’s linear coefficient. A P value of 0.05 was considered significant. The STATISTICA software (StatSoft, USA) was used.
An additional analysis was performed in the CD group for the operative sagittal Cobb angle correction. Two subgroups were identified according to the angle of kyphosis as measured on the preoperative lateral radiographs. These were a hypokyphotic subgroup, consisting of 14 curves with a sagittal Th4–Th12 angle of less than 15° and a normokyphotic subgroup, which consisted of 11 curves with an angle of more than 15°. The operative change of the thoracic kyphosis angle was calculated separately for each subgroup.
Results
On the preoperative radiographs there were no statistically significant differences (P<0.05) between the CD group and the ANT group regarding the values of the frontal and sagittal Cobb angle, AVT, AVR, C7 shift and rib cage shift (Table 1). The two groups contained curves fully comparable in terms of severity of deformity.
Table 1.
Preoperative and postoperative values of measured parameters
| CD (N=25) | ANT (N=21) | CD versus ANT | Postoperative versus preoperative | |||
|---|---|---|---|---|---|---|
| CD | ANT | |||||
| Cobb angle (degrees) | Preoperative | 53.6±7.03 (45.0–65.0 | 49.5±6.71(45.0–65.0) | NS | ||
| S | S | |||||
| Postoperative | 16.2±6.6 (5.0–36.0) | 8.0±4.2 (0.0–15.0) | S1 | |||
| AVT (mm) | Postoperative | 50.4±16.5 (15.0–86.0) | 42.2±15.4 (22.0–86.0) | NS | ||
| S | S | |||||
| Postoperative | 4.6±12.6 (−28.0–27.0) | -0.5±7.0 (−18.0–16.0) | NS | |||
| AVR (degrees) | Preoperative | 21.4±6.3 (10.0–30.0) | 18.0±5.5 (10.0–30.0) | NS | ||
| NS | S | |||||
| Postoperative | 19.6±5.8 (10.0–30.0) | 5.3±4.4 (0.0–15.0) | S1 | |||
| LIV tilt (degrees) | Preoperative | 21.3±4.6 (13.0–30.0) | 18.2±5.4 (6.0–28.0) | NS | ||
| S | S | |||||
| Postoperative | 2.4±4.5 (−12.0–10.0) | 2.4±2.6 (−2.0–9.0) | NS | |||
| C7 shift (mm) | Preoperative | 6.5±16.5 (−30.0–40.0) | 5.2±11.8 (−15.0–40.0) | NS | ||
| S | S | |||||
| Postoperative | 10.6±12.8 (−40.0–18.0) | -1.8±7.6 (−20.0–10.0) | S | |||
| Rib cage shift (mm) | Preoperative | 48.1±30.5 (10.0–110.0) | 37.3±20 (10.0–105.0) | NS | ||
| S | S | |||||
| Postoperative | -25.3±20.6 (−75.0–15.0) | -19.5±10.7 (−35.0–0.0) | S | |||
| Sagittal Cobb angle Th4–Th12 (degrees) | Preoperative | 18.6±11.3 (−8.0–37.0) | 21.0-11.3 (4.0–33.0) | NS | ||
| NS | NS | |||||
| Postoperative | 19.5±7.7 (6.0–38.0) | 21.5±8.0 (8.0–34.0) | NS | |||
All the values are expressed as the mean ± SD followed by the minimum and maximum values in brackets AVT Apical vertebra transposition, AVR Apical vertebra rotation, LIV lowest instrumented vertebra, S difference significant at P<0.05, S1 difference significant at P<0.001, NS difference not significant, CD Cotrel-Dubousset group, ANT anterior surgery group
No deaths, neurologic complications, infections or hardware problems occurred in either group. No additional external support was used both for the CD and the ANT patients. The patients’ height increased after operation in each group (P<0.01). The increase was significantly superior in the CD group compared to that in the ANT group (P<0.01), Table 2. The rib hump, as assessed by Adams’ forward bending test, significantly decreased after both the CD procedure and anterior plating (P<0.01). A significantly greater correction of the rib hump (P<0.001) was noted in the ANT group than in the CD group.
Table 2.
Operative correction of clinical and radiological parameters
| CD (N=25) | ANT (N=21) | CD versus ANT | |
|---|---|---|---|
| Trunk height increase (cm) | 2.5±1.0 (0.0–4.0) | 1.3±1.3 (−1.0 to 3.5) | S1 |
| Rib hump correction (%) | 46.7±18.7 (14.0–85.0) | 80.8±14.6 (57.0–100.0) | S1 |
| Cobb angle correction (degrees) | 37.0±6.1 (28.0–50.0) | 41.0±7.9 (32.0–60.0) | NS |
| Apical vertebra transposition correction (mm) | 45.8±12.9 (13.0–74.0) | 42.7±14.7 (28.0–89.0) | NS |
| Apical vertebra rotation correction (degrees) | 1.8±4.4 (−5.0 to 10.0) | 12.6±3.9 (5.0–22.0) | S1 |
| Sagittal Cobb angle correction (degrees) | 0.8±10.2 (−14.0 to 19.0) | 0.4±9.0 (−14.0 to 15.0) | NS |
| Correction of the tilt of the lowest instrumented vertebra (degrees) | 18.8±4.7 (10.0–29.0) | 15.3±6.8 (3.0–27.0) | S |
| Correction of C7 shift (mm) | 17.9±11.7 (0.0–40.0) | 9.0±9.8 (0.0–40.0) | S |
| Correction of rib cage shift (mm) | 73.4±26.4 (41.0–130.0) | 56.8±19.9 (25.0–117.0) | S |
All the values are expressed as the mean ± SD followed by the minimum and maximum values in brackets S difference significant at P<0.05, S1 difference significant at P<0.001, NS difference not significant, CD Cotrel-Dubousset group, ANT anterior surgery group
The preoperative and postoperative values of the radiological parameters for each method are summarized in Table 1, and the operative correction is given in Table 2.
In the CD hypokyphotic subgroup the sagittal Cobb angle before operation was 5.4±8.2° while, after operation, it increased of 6.0±9.5°, P<0.05 (Fig. 5). In the CD normokyphotic subgroup the sagittal Cobb angle, before operation, was 26.7±6.8° while, after operation, it decreased of 8.9±9.0° (P<0.05).
Fig. 5.
Preoperative and postoperative lateral radiographs of a patient from CD hypokyphotic subgroup
The segmental vertebral axial rotation angle calculated by the RACHIS software for the totality of patients from the CD and ANT groups is presented in Figs. 3 and 4, respectively.
Good correlation was found between manually assessed and software derived parameters, with Pearson coefficients of 0.93, 0.81, and 0.91 for the Cobb angle, AVT, and AVR, respectively (P<0.001).
Discussion
Although this is a retrospective study, we believe that the selected material is representative for each surgical method. The two analyzed methods were not alternatives. They represented the pattern of treatment approach practiced in two different universities. For the anterior instrumentation we used the Nécker-Enfants Malades material because anterior correction of moderate flexible thoracic curves was routinely performed in that orthopedic school both before and after the introduction of the CD system [24]. In the two pediatric orthopedic departments engaged in the study the material retained for analysis represented a consecutive series of patients fulfilling the inclusion criteria. For each method the data originated from a considerable number of patients operated on with one technique and by one operative team. The selection of material enabled analysis of mechanically similar curves, so differences in the immediate outcome could be attributed to the specificity of the mechanical action of each device. Wattenbarger et al. [29] compared single rod and double rod instrumentation applied to curves similar with respect to both curve pattern and curve magnitude. However, in both single rod and double rod instrumentation there was the same strategic vertebrae disposition and the same mechanism of correction. We chose 65° as the maximal initial Cobb angle because we believed that the interference of secondary growth changes in vertebrae (wedging, intravertebral torsion), discs, ribs, ligaments, and muscles could be minimized [26].
The CSL was drawn according to Lonstein and Carlson [19] in order to avoid eventual CSL obliquity if the iliac crests were not level. In ten cases we found one iliac crest higher than the other while the femoral heads were level. On each radiograph we prolonged the CSL distally to reach the middle of the symphysis pubis to prove that the pelvis was not rotated with respect to the plane of the X-ray cassette. While this seemed necessary, as small axial rotation angles had to be measured, it markedly limited the number of cases suitable for analysis, because the whole pelvis had to be seen on the radiograph. The lack of adequate documentation and the strict inclusion criteria were responsible for the limited number of patients, i.e. only 46 of the 577 cases reviewed.
The operative correction of the Cobb angle and the AVT was similar in the CD and the ANT groups. The AVT after anterior instrumentation was reduced to zero on the average and to negative values for ten curves. This hypercorrection was observed to a lesser extent in the CD group. Spinal coronal balance, as assessed by the C7-shift revealed a left decompensation in both groups, particularly in the CD (Table 1). This was only found retrospectively on the radiographs but had not been clinically visible, in opposition to Bridwell et al. finding [3].
In the CD group after a rod derotation maneuver, which uses a strictly transversal corrective force, we observed the elongation of the instrumented portion of the spine. A 3D displacement of vertebrae under a unidimensional corrective force occurred regardless of the type of device used.
The CD instrumentation was designed with the idea of restoring the normal sagittal contour of the scoliotic spine. However, the data concerning the angle of thoracic kyphosis were ambiguous for the CD group because they indicated no postoperative change of the sagittal Th4–Th12 Cobb angle. A similar observation was reported by Wattenbarger et al. [29]. Further analysis of the CD group revealed two subgroups of curves: the true hypokyphotic and the normokyphotic one. Separate analyses were performed for each subgroup as proposed by Bridwell et al. [2]. The postoperative sagittal Cobb angle increased in the hypokyphotic subgroup while it decreased in the normokyphotic subgroup.
A significant (P<0.001) postoperative decrease of the apical vertebra axial rotation angle (AVR) was found only in the ANT group. Segmental change of the axial vertebral rotation angle was calculated by the RACHIS software (Fig. 4) and demonstrated on the top views of the spine. We found this program suitable for both understanding and evaluating the operative correction of the scoliotic spine.
In five patients in the ANT group, the postoperative rib hump height on the Adams’ forward bending test was judged as zero. Such a result was never observed in the other group. A significant correction of rib hump height following anterior instrumentation has been reported previously [1, 14, 24]. In the ANT group scoliosis was corrected by pushing vertebral bodies towards the midline with a titanium plate. Majd et al. [21] used rod rotation followed by the axial compression. Pure compression has been used in the anterior Eclipse instrumentation [23]. This means that derotation of the apical vertebra is possible with different implant manipulations. We believe that the point of application of the corrective force on vertebral bodies and positive shortening of the anterior column of the spine are essential to obtain vertebral derotation inside the curve.
The intraoperative maneuver, consisting of CD rod derotation, did not result in a significant decrease of the vertebral axial rotation angle. It would be interesting to study the posterior segmental systems of translation and countertorsion, based on the use of pedicle screws. We were unable to collect the study group fulfilling strict inclusion criteria. Correction of thoracic hypokyphosis, translation of the apex of the curve to the midline and multi-point solid fixation seem to be the advantages of the CDI. Our observation of the lack of correlation between clinical reduction of the rib hump (47% on the average) and the radiologically measured reduction in the vertebral axial rotation angle (8% on the average) in the CD group are in accordance with Willers et al. [30].
The anterior correction of a single thoracic scoliosis has been relatively rarely performed [1]. Endoscopic techniques suggest new arguments for reconsidering the thoracic anterior approach [23]. A 3D correction of scoliotic curve with endoscopic techniques should be investigated.
This paper does not indicate the authors’ preferences for scoliosis surgery, since radiological parameters constitute only a part of the global outcome [9]. Apart from mechanical considerations, other factors such as the method’s aggressiveness, instrumentation complexity, quality of spinal fusion or cost may influence the therapeutic choice. Operative correction of scoliosis does not restore the normal spine either morphologically or functionally. We believe that the trend towards morphologically perfect correction is justified but it should not dominate the goal of surgical treatment of scoliosis, which is a stable, long-term correction performed with maximum safety for the child.
Conclusions
Anterior instrumentation provided better correction of the vertebral axial rotation and of the rib hump. The CD instrumentation was more powerful in translation and more specifically addressed the sagittal plane: the postoperative thoracic kyphosis angle increased in the hypokyphotic curves and slightly decreased in the normokyphotic curves.
Acknowledgements
The study was partially supported by Polish Committee for Scientific Research, grant KBN 4PO5E 07212. No other benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
References
- 1.Betz RR, Harms J, Clements DH, III, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine. 1999;24:225–239. doi: 10.1097/00007632-199902010-00007. [DOI] [PubMed] [Google Scholar]
- 2.Bridwell KH, Betz R, Capelli AM, et al. Sagittal plane analysis in idiopathic scoliosis patients treated with Cotrel-Dubousset instrumentation. Spine. 1990;15:921–926. doi: 10.1097/00007632-199009000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Bridwell KH, McAllister JW, Betz RR, et al. Coronal decompensation produced by Cotrel-Dubousset “derotation” maneuver for idiopathic right thoracic scoliosis. Spine. 1991;16:769–777. doi: 10.1097/00007632-199107000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Brown RH, Burstein AH, Nash CL, et al. Spinal analysis using a three-dimensional radiographic technique. J Biomech. 1976;9:355–365. doi: 10.1016/0021-9290(76)90113-5. [DOI] [PubMed] [Google Scholar]
- 5.Cobb JR (1948) Outline for the study of scoliosis. Course Lectures American Academic of Orthopaedics, p 261
- 6.Cotrel Y, Dubousset J. Nouvelle technique d’ostéosynthèse rachidienne segmentaire par voie postérieure. Rev Chir Orthop. 1984;70:489–494. [PubMed] [Google Scholar]
- 7.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Rel Res. 1988;227:10–23. [PubMed] [Google Scholar]
- 8.D’Andrea LP, Betz RR, Lenke LG, et al. The effect of continued posterior spinal growth on sagittal contour in patients treated by anterior instrumentation for idiopathic scoliosis. Spine. 2000;25:813–818. doi: 10.1097/00007632-200004010-00009. [DOI] [PubMed] [Google Scholar]
- 9.D’Andrea LP, Betz RR, Lenke LG, et al. Do radiographic parameters correlate with clinical outcomes in adolescent idiopathic scoliosis?. Spine. 2000;25:1795–1802. doi: 10.1097/00007632-200007150-00010. [DOI] [PubMed] [Google Scholar]
- 10.DeSmet AA. Radiology of spinal curvature. St Louis: CV Mosby Company; 1985. pp. 23–108. [Google Scholar]
- 11.Dubousset J, Herring JA, Shufflebarger H. The crankshaft phenomenon. J Pediatr Orthop. 1989;5:541–550. doi: 10.1097/01241398-198909010-00008. [DOI] [PubMed] [Google Scholar]
- 12.Dubousset J. Three-dimensional analysis of the scoliotic deformity. In: Weinstein SL, editor. The pediatric spine. New York: Raven Press; 1994. pp. 479–496. [Google Scholar]
- 13.Graf H, Hecquet J, Dubousset J. Approche tridimensionnelle des déformations rachidiennes. Rev Chir Orthop. 1983;69:407–416. [PubMed] [Google Scholar]
- 14.Halm HF, Liljenqvist U, Niemeyer T, et al. Halm-Zielke instrumentation for primary stable anterior scoliosis surgery: operative technique and 2-year results in ten consecutive adolescent idiopathic scoliosis patients within a prospective clinical trial. Eur Spine J. 1998;7:429–434. doi: 10.1007/s005860050103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hecquet J, Rachis TM (1998) Manuel opératoire. Paris
- 16.Hindmarsh J, Larsson J, Mattsson P. Analysis of changes in the scoliotic spine using a three-dimensional radiographic technique. J Biomech. 1989;13:279–290. doi: 10.1016/0021-9290(80)90370-X. [DOI] [PubMed] [Google Scholar]
- 17.Hopf CG, Eysel P, Dubousset J. Operative treatment of scoliosis with Cotrel-Dubousset-Hopf instrumentation New anterior spinal device. Spine. 1997;22:618–627. doi: 10.1097/00007632-199703150-00008. [DOI] [PubMed] [Google Scholar]
- 18.King HA, Moe JH, Bradford DS, et al. The selection of fusion level in thoracic idiopathic scoliosis. J Bone Joint Surg. 1983;65:1302–1313. [PubMed] [Google Scholar]
- 19.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg. 1984;66:1061–1071. [PubMed] [Google Scholar]
- 20.Lowe T, Peters JD. Anterior spinal fusion with Zielke instrumentation for idiopathic scoliosis. Spine. 1993;18:423–426. [PubMed] [Google Scholar]
- 21.Majd ME, Castro FP, Holt RT. Anterior fusion for idiopathic scoliosis. Spine. 2000;25:696–702. doi: 10.1097/00007632-200003150-00008. [DOI] [PubMed] [Google Scholar]
- 22.Perdriolle R (1979) La scoliose. Son étude tridimensionnelle. Maloine SA Éditeur, Paris
- 23.Picetti G, Blackman RG, O’Neal K, et al. Anterior endoscopic correction and fusion of scoliosis. Othopedics. 1998;21:1285–1287. doi: 10.3928/0147-7447-19981201-09. [DOI] [PubMed] [Google Scholar]
- 24.Pouliquen JC, Rigault P, Padovani JP, et al. Redressement par plaque des scolioses Résultats de 99 cas vus avec recul. Rev Chir Orthop. 1984;70:93–108. [PubMed] [Google Scholar]
- 25.Risser JC. The iliac apophysis: an invaluable sign in the management of scoliosis. Clin Orthop. 1958;11:111–119. [PubMed] [Google Scholar]
- 26.Shufflebarger HL. Theory and mechanisms of posterior deformation spinal systems. In: Weinstein SL, editor. The pediatric spine. New York: Raven Press; 1994. pp. 1515–1543. [Google Scholar]
- 27.Sweet FA, Lenke LG, Bridwell KH, et al. Prospective radiographic and clinical outcomes and complications of single solid rod instrumented anterior spinal fusion in adolescent idiopathic scoliosis. Spine. 2001;26:1956–1965. doi: 10.1097/00007632-200109150-00005. [DOI] [PubMed] [Google Scholar]
- 28.Turi M, Johnston CE, II, Richards BS. Anterior correction of idiopathic scoliosis using TSRH instrumentation. Spine. 1993;18:417–422. [PubMed] [Google Scholar]
- 29.Wattenbarger JM, Richards BS, Herring JA. Comparison of single-rod instrumentation with double-rod instrumentation in adolescent idiopathic scoliosis. Spine. 2000;25:1680–1688. doi: 10.1097/00007632-200007010-00011. [DOI] [PubMed] [Google Scholar]
- 30.Willers U, Transfeldt EE, Hedlund R. The segmental effect of Cotrel-Dubousset instrumentation on vertebral rotation, rib hump and the thoracic cage in idiopathic scoliosis. Eur Spine J. 1996;5:387–393. doi: 10.1007/BF00301966. [DOI] [PubMed] [Google Scholar]
- 31.Zielke K. Ventrale derotationspondylodese bahandung sergebnisse bei idiopatischen lumbalskoliossen. Z Orthop. 1982;120:320–329. doi: 10.1055/s-2008-1051620. [DOI] [PubMed] [Google Scholar]