Abstract
We report preliminary results for unstable sacral fractures treated with a modified posterior triangular osteosynthesis. Seven patients were admitted to our trauma center with an unstable sacral fracture. The average age was 31 years (22–41). There were four vertical shear lesions of the pelvis and three transverse fracture of the upper sacrum. The vertical shear injuries were initially treated with an anterior external fixator inserted at the time of admission. Definitive surgery was performed at a mean time of 9 days after trauma. The operation consisted in a posterior fixation combining a vertebropelvic distraction osteosynthesis with pedicle screws and a rod system, whereby the transverse fixation was obtained using a 6 mm rod as a cross-link between the two main rods. Late displacement of the posterior pelvis or fracture was measured on X-ray films according to the criteria of Henderson. The patients were followed-up for a minimum time of 12 months. Four patients who presented with a pre-operative perineal neurological impairment made a complete recovery. No iatrogenic nerve injury was reported. One case of deep infection was managed successfully with surgical debridement and local antibiotics. All patients complained of symptoms related to the prominence of the iliac screws. The metalwork was removed in all cases after healing of the fracture, at a mean time of 4.3 months after surgery. No loss of reduction of fracture was seen at final radiological follow-up. The preliminary results are promising. The fixation is sufficiently stable to allow an immediate progressive weight-bearing, and safe nursing care in polytrauma cases. The only problem seems to be related to prominent heads of the distal screws.
Keywords: Sacrum fracture, Triangular osteosynthesis
Introduction
Stabilization of unstable sacrum fractures represent a major challenge in the treatment of pelvic ring injuries. Unstable sacrum fractures represent severe injuries, accompanied by a high mortality and morbidity due to pain and malunion [1, 9]. The goal of surgical fixation is the reconstruction of the spine-pelvic-junction to allow early weight-bearing and to facilitate nursing care, particularly for multiply injuried patients.
External fixation is a viable option for sacral fractures associated with vertical shear lesion of the pelvis if vital parameters do not allow definitive reduction and fixation [8], but if used alone it is inadequate in treating comminuted sacral injuries, or transverse displaced fracture of the upper sacrum [14].
Various options for internal fixation have been proposed, including percutaneous iliosacral screws [4], transiliac bars [21, 22], sacral rods [19], posterior small plates [13], or vertical stabilization alone [7].
None of these techniques can, however, provide adequate fixation for early unrestricted weight-bearing and secure mobilization of patients in the presence of vertically unstable pelvic fractures.
On the other hand, a transverse fracture of the upper sacrum, or “suicidal jamper’s fracture” described by Roy-Camille [14], represents a specific entity, and is often a displaced fracture associated with perineal neurological deficit. In the case of displacement, a surgical treatment, consisting of open reduction and stabilization with lumboiliac plates, lumbosacral plates or Harrington rods associated with a transverse bi-iliac bar, is mandatory [14].
Some authors [7, 16] have introduced the technique of triangular posterior osteosynthesis (TPO) in the treatment of vertically unstable pelvic fracture. Recents articles [11, 20] have confirmed good clinical results. This is a biplanar fixation able to counterbalance the forces on the posterior pelvic ring during unipodal stance, so as to allow early weight-bearing.
The purpose of this paper is to show our preliminary results of unstable sacral fractures treated with a modified PTO.
Materials
Between October 2002 and March 2003, seven patients with unstable sacral fractures were admitted to our trauma center. In three cases, the patients were suicidal jumpers, two cases were victims of a parachute accident, one case was knocked down, and the last case was a motorcycle accident. All patients were seriously injured and so received a total-body CT scan at the time of emergency admission. In all cases, there were associated osseous lesions (Table 1).
Table 1.
Pre-operative patient data
| Patient | Age (years) | Sex | Cause | Pre-operative neurological deficit | Type of fracture | Associated lesions | Delay to surgery (days) | Duration of surgery (min) |
|---|---|---|---|---|---|---|---|---|
| 1 | 33 | M | MVA | Yes | C | Thoracic injury | 8 | 100 |
| 2 | 22 | F | Knock downed | Yes | C | Bilateral calcaneum fractures | 1 | 90 |
| 3 | 26 | M | Suicidal jumper | C | Right pilon fracture | 10 | 110 | |
| Bilateral calcaneum fractures | ||||||||
| 4 | 31 | M | Suicidal jumper | Yes | Shaped H fracture | Left calcaneum fracture | 7 | 90 |
| Right Lisfranc fracture-dislocation | ||||||||
| 5 | 38 | M | Parachute accident | C | Sub-trochanteric femoral fracture | 17 | 115 | |
| 6 | 41 | M | Parachute accident | Yes | Shaped H fracture | Left calcaneum fracture | 12 | 90 |
| Right pilon fracture | ||||||||
| 7 | 26 | M | Suicidal jumper | Shaped H fracture | Right leg sub-amputation | 8 | 110 |
Following CT evaluation, an X-ray trauma series (AP, inlet and outlet of pelvis) was performed. An unstable fracture was defined as showing at least 1 cm of combined vertical displacement on initial inlet and outlet views, or a complete vertical sacral fracture with at least 1 cm of separation over the whole fracture surface on initial CT scan, or a transverse displaced fracture of the upper sacrum.
Table 2 summarizes the main data of the patients. The average age was 31 years (range 22–41). The Denis classification [2] was used to subdivide longitudinal sacral fractures associated with vertical shear lesion of the pelvis; while, for the transverse fracture we used the Roy-Camille classification [14].
Table 2.
Post-operative patient data
| Number of patients | 7 |
| Follow-up (months) | 11 (9–12) |
| Post-operative neurological deficit | 0 |
| Frank tenderness over distal screws | 2 |
| Skin lesion | 0 |
| Deep infection | 1 |
| Loss of reduction | 0 |
| Fracture healing | 7 |
| Implant removal (between 3 months and 6 months) | 7 |
Four of these patients (type C pelvic injuries) who were haemodynamically unstable were treated with an anterior external fixation on admission. Two of them presented a bilateral zone II sacral fracture, one presented a right zone II and left zone III sacral fracture, and one case a unilateral zone II sacral fracture, according to the Denis classification [2]. The transverse upper sacrum fracture was type II in all cases (Fig. 1). The surgery was performed after a mean time of 9 days (range 1–17) following trauma, once patients were stabilized. In three of the four patients with type C pelvic injuries, the anterior external fixation was removed, and an anterior pelvic ring fixation was performed by plating the pubic rami and symphysis. In the one case, the external fixator was left in place until fracture healing.
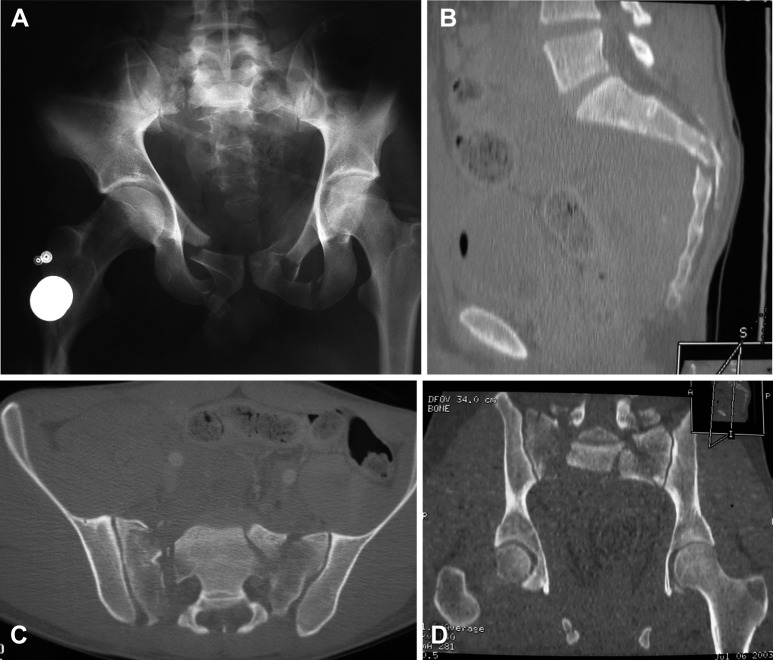
Fig. 1.
A Pre-operative antero posterior X-ray, and CT scan, B sagittal view, C coronal view, D frontal view, of an H sacral fracture
Four patients (one with transverse upper sacrum fracture and three with vertical shear lesion of the pelvis) showed perineal neurological deficit.
Radiological investigations consisted of AP, inlet and outlet views performed during the immediate post-operative period and repeated at follow-up. The vertical displacement of fracture before and after surgery was measured by constructing horizontal reference lines through bony landmarks according to Henderson [6].
Residual post-operative displacement and late displacement of the posterior pelvis or fracture were measured by an independent observer. Failure was defined as at least 1 cm of combined vertical displacement of the posterior pelvis or fracture compared with immediate post-operative X-ray.
Operative procedure
The patient was placed in a prone position. An image intensifier was used. A longitudinal approach to the lumbosacral spine was made, and the thoracolumbar fascia and the paravertebral muscle mass were dissected. The fracture was exposed. In the four cases in whom neurological deficit were diagnosticated, a laminectomy was made at the sacral level. In order to perform the triangular osteosynthesis, we used the Click’X system (Synthes, Oberdorf, Switzerland).
Pedicle screws were first inserted in the pedicle of L4. Subsequently caudal screws were implanted into the iliac bone, through the posterior-superior-iliac-spine (PSIS) and parallel to the sacroiliac joint. Four screws were inserted, even in the case of unilateral fracture of the sacrum. We found it important to make a bone window with a reamer in order to allow a deeper seating of the screw head, preventing prominence of the metalwork under the soft tissues. Once the four screws were inserted, reduction was carried out.
Connecting rods were inserted and tightened initially only over the proximal pedicle screws of L4. The pedicle screws were used as “joysticks” in order to achieve reduction in the vertical and horizontal direction. Reduction was also obtained using an AO distractor over the pedicle screws, or with the help of a bone hook, used to grasp the iliac wing. At this point, the USS connecting rod was tightened over the distal (PSIS) screws, therefore stabilizing the fracture.
In order to obtain stabilization in the horizontal plane, we did not use a sacroiliac screw fixation or transacral plate, but a 6-mm rod was inserted as a transversal cross-link between the two longitudinal connecting rods. When faced with a transvere upper sacrum fracture, a sagittal alignment was not attempted, instead the fracture was stabilized in its displaced position. After copious irrigation, the surgical wound was closed on two suction drains. In cases in which the sacral fracture was associated with pubic symphysis disruption, the latter was also stabilized. Technically, the anterior pelvic fixation was performed firstly in all cases (Fig. 2).
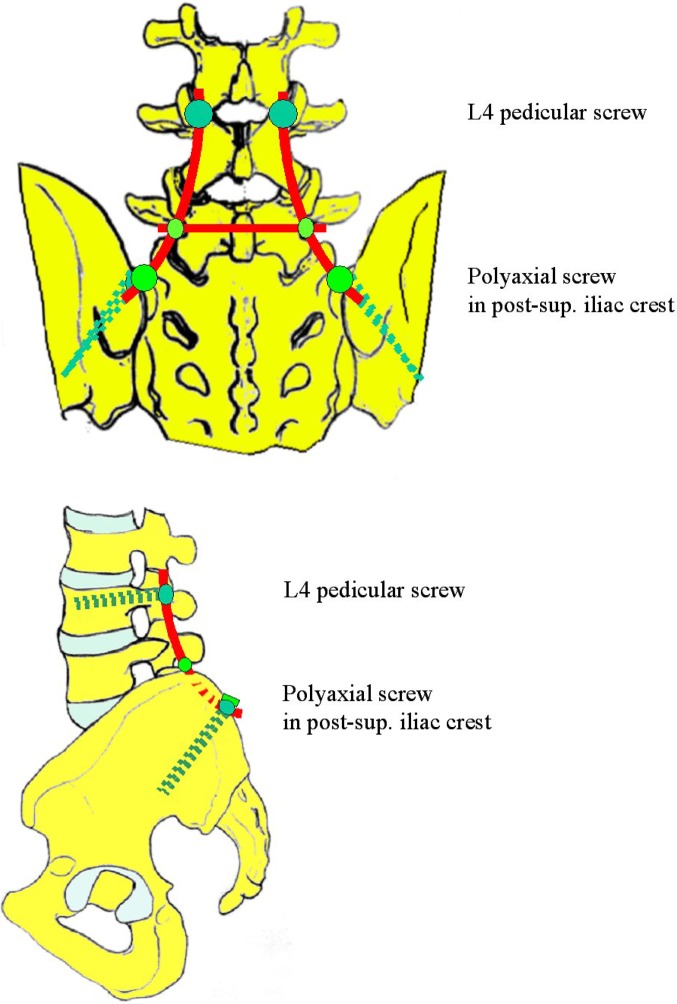
Fig. 2.
The technique of fixation
Results
The seven patients were followed-up for a minimum of 12 months (range 12–17 months). In the four patients with neurologic impairment, a slow but complete recovery was found. In no case was an iatrogenic nerve lesion observed.
The operation lasted between 90 min and 120 min. In the course of the post-operative management, two patients were unable to bear weight early due to lower-limb-associated fractures. Those patients were nevertheless operated on in order to allow safe mobilization during nursing care. The other five patients started bearing weight 24 h after surgery.
One case of deep infection was reported. It was treated with prompt debridement, lavage and local antibiotic-loaded beads, renewed every 6 weeks, up against the fracture union, for 5 months. This case was managed with subsequent removal of the hardware, resulting in complete resolution of the infection. All seven patients presented complaints related to distal screws inserted in the region of the PSIS. In particular, two patients complained of tenderness around the screws, but in no case were skin lesions observed. No loosening of the hardware occurred.
At final radiological follow-up, no loss of reduction was observed with respect to an immediate post-operative X-ray. The fracture union was judged by X-ray, evaluating the presence of callus formation. The mean time of fracture healing was 4 months (range 3–6 months).
The implant was removed at a mean of 4.3 months (3.5–6.5) after surgery due to mild complaints in four cases related to the metalwork, frank tenderness around the PSIS screw in two cases and deep infection in one case (Table 2, Figs. 3, 4)..
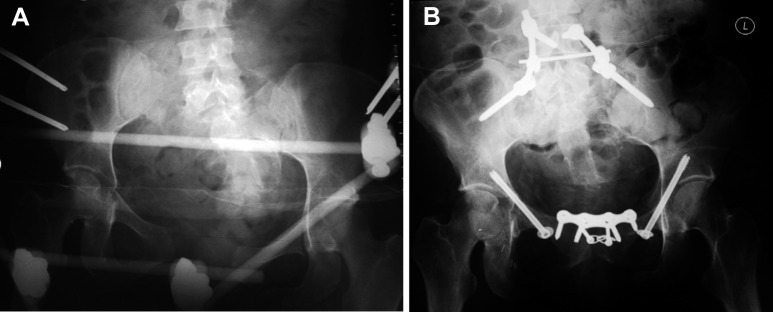
Fig. 3A-C.
Post-operative X-ray view of lumbo-iliac fixation. A Antero posterior view, B AP localized view, C X-ray after healing and removed material
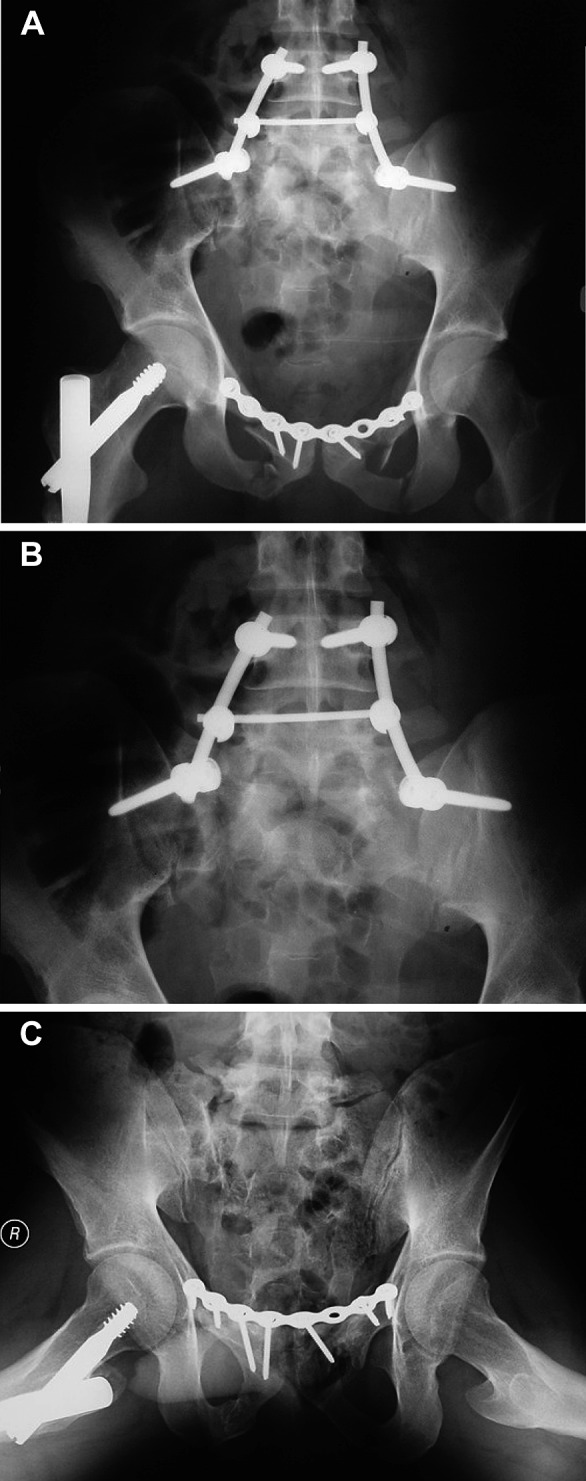
Fig. 4A,B.
Case no. 3, treated initially by external fixation without sufficient reduction. Revision at 3 weeks with laborious but excellent reduction
Discussion
Fractures of the sacrum represent a wide spectrum of lesions, ranging from a simple fracture of the sacral ala, transverse fracture, to comminuted fractures associated with vertical shear lesion of the pelvis.
In the past, often these fractures—in particular the transverse fractures—were undiagnosed and untreated, resulting in neurological deficit [7, 14]. Moreover, the absence of satisfactory surgical techniques to treat those injuries led some authors to advocate non-operative treatment [1, 3].
In our series, the patients were multiply injured, so a total CT scan enabled a diagnosis to be made. Some authors have shown that a stable early open reduction and fixation of these fractures is very important to allow early mobilization and reduce morbidity [9] and mortality [5].
In fact, unprotected weight-bearing in this type of fracture has been associated with post-operative complications, such as loss of reduction and secondary neural impairment [17]. Nevertheless, it can be difficult to obtain a stable fixation of the sacrum itself, particularly because the lumbosacral junction must resist large forces as well as allowing motion [10]. Biomechanical studies have showed that transforaminal sacral fractures, in a cadaveric model, fixed with transiliac plates, sacral screws, transiliac compression rods or local plates, were less stable when compared with the intact pelvis [18]. This finding correlated clinically with secondary vertical displacement despite fixation.
Recently, Griffin et al. [4] have shown that the use of percutaneous iliosacral screw fixation may be a good technique to manage vertically unstable sacral fractures, but there are some anatomic limitations, and in order to prevent fixation failure prolonged bed rest is often necessary.
A first technique of lumbopelvic distraction spondylodesis for the treatment of sacrum fracture was proposed by Kach [7]. This technique does not guarantee the rotational stability of the posterior pelvis. PTO combines a vertical (lumbopelvic) and horizontal (iliosacral) fixation, providing a good degree of protection against cranial migration of the injuried half of the pelvic ring [15] by transferring vertical loads from the lower lumbar spine to the ilium. The sacral fracture result partially protected from these loads and the horizontal component stabilizes the fracture in the horizontal plane, so resisting certain counterforces, such as the internal rotation observed in a biomechanical study [17]. The PTO for unstable sacral fractures provides greater immediate post-operative stability compared with iliosacral screw fixation, as shown in an experimental study [17].
In our cases, we have always performed a lumbopelvic fixation, anchoring the inferior screws into the ilium without direct sacral or sacroiliac joint fixation, as described in the original technique, in which the use of transacral plating or iliosacral screws were suggested [16].
The horizontal fixation was performed with a 6-mm rod used as a cross-link. The idea was to perform a PTO without touching the sacrum and reduce the necessity to put the hardware at the fracture site, which is technically demanding [7, 14, 16, 17]. We also noted the possibility of obtaining intraoperatively a good reduction in cases of vertically unstable sacral fractures associated with type C pelvis injuries. Observing the preliminary results, the impression is that this model of stabilization allows good results and in no case was material loosening or fracture displacement found at the latest follow-up.
The main purpose of this procedure is to transmit the load of the trunk to the pelvis, sparing the sacrum completely. Probably, the good resistance showed by our technique of fixation may also be related to routine fixation of the anterior pelvic ring. In fact, it has been demonstrated [17] that one iliosacral screw and unilateral TPO is sufficient in cases in whom the anterior pelvic ring was addressed.
In the case of transverse upper sacrum fracture, the surgical indication was related to displacement of the fracture, as suggested by Roy-Camille et al. [14]. The latter described the use of osteosynthesis with vertical support in sacrum fracture. Our PTO technique does not enable different correction of the sagittal alignment to the lumboiliac or lumbosacral plates [14], showing the same problem of Harrington rod fixation [14]. The substantial difference is that our fixation permits stabilization in the sagittal plane. Novkov et al. [12] advocated a non-operative reduction in a case report of fracture dislocation of S1. The drawback of this treatment was the long bed rest time with a skeletal traction (60 days) and a persistence of bladder and bowel disfunction until 13 months after injury. The surgical management permits a nerve decompression, if necessary, and the fixation stabilizing an unstable fracture allows secure early mobilization. As described in the literature [16], a sacral fracture usually heals, even in the presence of an inadequate reduction. This statement was confirmed in our series and in another report [12]; nevertheless, none of the patients with a transverse fracture of the sacrum complained of discomfort in the sacral region at follow-up. We think that in cases in whom the displacement is not very important (some type II fractures), it is not necessary to obtain an anatomical sagittal alignment.
The only problem encountered with our technique and material was the necessity to remove the metalwork shortly after fracture healing, due to local complaints. In fact, the head of the distal screw can be very prominent, and despite the bone window performed in order to bury the head of the screw, nearly all patients referred symptoms. Nevertheless, no cases of skin necrosis were found in this preliminary series. During the early phase of rehabilitation, care should be taken to prevent pressures sores over the distal screws.
In conclusion, we found that TPO, as we have described it in this report, can be useful in treating unstable sacral fractures. Although our data are not supported by biomechanical studies, the use of a cross-link rod seems to be sufficient to obtain horizontal stability of fixation, obviating the need for a posterior fixation using transacral plates or iliosacral screws.
References
- 1.Court-Brown CM, Gertzbein SD. The management of burst fractures of the fifth lumbar vertebra. Spine. 1987;12:308–312. doi: 10.1097/00007632-198704000-00022. [DOI] [PubMed] [Google Scholar]
- 2.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop. 1988;227:67–81. [PubMed] [Google Scholar]
- 3.Frederickson BE, Yuan HA, Miller HE. Burst fractures of the fifth lumbar vertebra. J Bone Joint Surg Am. 1982;64:1088–1094. [PubMed] [Google Scholar]
- 4.Griffin DR, Starr AJ, Reinert CM, Jones AL, Whitlock S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral crews: does posterior injury pattern predict fixation failure. J Orthop Trauma. 2003;17:399–405. doi: 10.1097/00005131-200307000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Gutenberg B, Goldie I, Slätis P. Fixation of the pelvic fractures and dislocations. Acta Orthop Scand. 1978;49:278–286. doi: 10.3109/17453677809005765. [DOI] [PubMed] [Google Scholar]
- 6.Henderson RC. The long term results of nonoperatively treated major pelvic disruptions. J Orthop Trauma. 1989;3:41–47. doi: 10.1097/00005131-198903010-00008. [DOI] [PubMed] [Google Scholar]
- 7.Käch K, Trentz O. Distraction spondylodesis of the sacrum in “vertical shear lesions” of the pelvis. Unfallchirurg. 1994;97:28–38. [PubMed] [Google Scholar]
- 8.Kellam JF. The role of external fixation in pelvic disruptions. Clin Orthop Relat Res. 1989;241:66–82. [PubMed] [Google Scholar]
- 9.Latenser BA, Gentilello LM, Tarver AA, Thalgott JS, Batdorf JW. Improved outcome with early fixation of skeletally unstable pelvic fracture. J Trauma. 1991;31:28–31. doi: 10.1097/00005373-199101000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Levine AM. Fracture of the sacrum. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma. 3. Philadelphia: Elsevier; 2003. pp. 1031–1051. [Google Scholar]
- 11.Nothofer W, Thonke N, Neugebauer R. Die therapie instabiler sakrumfracturen bei beckenringbrüchen mit dorsaler sakrumdistanzosteosynthese. Unfallchirurg. 2004;107:118–127. doi: 10.1007/s00113-004-0725-y. [DOI] [PubMed] [Google Scholar]
- 12.Novkov HV, Tanchev PJ, Gyorev IS. Severe fracture-dislocation of S1 in a 12-year-old boy. A case report. Spine. 1996;21:2500–2503. doi: 10.1097/00007632-199611010-00019. [DOI] [PubMed] [Google Scholar]
- 13.Pohlemann T, Angst M, Schneider E, Ganz R, Tscherne H. Fixation of transforaminal sacrum fractures: a biomechanical study. J Orthop Trauma. 1993;7:107–117. doi: 10.1097/00005131-199304000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum. Suicidal jumper’s fracture. Spine. 1985;10:838–845. doi: 10.1097/00007632-198511000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Russe OJ, Schildhauer TA, Muhr G (1996) Biomechanical comparison of a new triangular osteosynthesis and two established fixation techniques in type C pelvic ring fractures. Trans Can Orthop Res Soc
- 16.Schildhauer TA, Josten C, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma. 1998;12:307–314. doi: 10.1097/00005131-199806000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Schildhauer TA, Ledoux WR, Chapman JR, Henley MB, Tencer AF, Routt ML., Jr Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17:22–31. doi: 10.1097/00005131-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Simonain PT, Routt C, Jr, Harrington RM, Tencer AF. Internal fixation for the transforaminal sacral fracture. Clin Orthop. 1996;323:202–209. doi: 10.1097/00003086-199602000-00028. [DOI] [PubMed] [Google Scholar]
- 19.Stocks GW, Gabel GT, Noble PC, Hanson GW, Tullos HS. Anterior and posterior internal fixation of vertical shear fractures of the pelvis. J Orthop Res. 1991;9:237–245. doi: 10.1002/jor.1100090212. [DOI] [PubMed] [Google Scholar]
- 20.Tiemann AH, Schmidt C, Josten C. Triangular vertebropelvine stabilisation of unstable posterior pelvic ring fractures. Zentralbl Chir. 2003;128:202–208. doi: 10.1055/s-2003-38533. [DOI] [PubMed] [Google Scholar]
- 21.Tile M. Pelvic ring fractures: should they be fixed. J Bone Joint Surg Br. 1988;70:1–12. doi: 10.1302/0301-620X.70B1.3276697. [DOI] [PubMed] [Google Scholar]
- 22.Tile M. Fractures of the pelvis and acetabulum. 2. Baltimore: Williams & Wilkins; 1995. pp. 22–36. [Google Scholar]