Abstract
Objective To assess the effectiveness and safety of melatonin in treating severe sleep problems in children with neurodevelopmental disorders.
Design 12 week double masked randomised placebo controlled phase III trial.
Setting 19 hospitals across England and Wales.
Participants 146 children aged 3 years to 15 years 8 months were randomised. They had a range of neurological and developmental disorders and a severe sleep problem that had not responded to a standardised sleep behaviour advice booklet provided to parents four to six weeks before randomisation. A sleep problem was defined as the child not falling asleep within one hour of lights out or having less than six hours’ continuous sleep.
Interventions Immediate release melatonin or matching placebo capsules administered 45 minutes before the child’s bedtime for a period of 12 weeks. All children started with a 0.5 mg capsule, which was increased through 2 mg, 6 mg, and 12 mg depending on their response to treatment.
Main outcome measures Total sleep time at night after 12 weeks adjusted for baseline recorded in sleep diaries completed by the parent. Secondary outcomes included sleep onset latency, assessments of child behaviour, family functioning, and adverse events. Sleep was measured with diaries and actigraphy.
Results Melatonin increased total sleep time by 22.4 minutes (95% confidence interval 0.5 to 44.3 minutes) measured by sleep diaries (n=110) and 13.3 (−15.5 to 42.2) measured by actigraphy (n=59). Melatonin reduced sleep onset latency measured by sleep diaries (−37.5 minutes, −55.3 to −19.7 minutes) and actigraphy (−45.3 minutes, −68.8 to −21.9 minutes) and was most effective for children with the longest sleep latency (P=0.009). Melatonin was associated with earlier waking times than placebo (29.9 minutes, 13.6 to 46.3 minutes). Child behaviour and family functioning outcomes showed some improvement and favoured use of melatonin. Adverse events were mild and similar between the two groups.
Conclusions Children gained little additional sleep on melatonin; though they fell asleep significantly faster, waking times became earlier. Child behaviour and family functioning outcomes did not significantly improve. Melatonin was tolerable over this three month period. Comparisons with slow release melatonin preparations or melatonin analogues are required.
Trial registration ISRCT No 05534585.
Introduction
Children with neurological and developmental disorders have a higher prevalence of sleep disturbances than their unaffected peers.1 Sleeping difficulties are often chronic and can result in additional learning and behaviour problems,2 affect the whole family’s health and wellbeing, and impair ability to continue in employment or further education.3 Despite limited evidence of the effectiveness of exogenous melatonin and some concerns regarding safety, it is commonly prescribed to children with neurodevelopmental delay, with wide variations in dose,4 because of its sleep phase shifting and hypnotic properties5 6.
Systematic reviews have looked at the effect of melatonin on sleep parameters4 7 8 9 10 with recommendations that additional randomised trials of melatonin be undertaken in children with sleep disorders and neurodevelopmental disorders, autism, or intellectual disability.4 7 8 We were commissioned to carry out this study after successfully replying to a call from the Health Technology Assessment Programme (part of the UK National Institute of Health Research) to assess the use of melatonin in children with impaired sleep and neurodevelopmental disorders.
Methods
Study design and oversight
This randomised, parallel group, double masked, multicentre, placebo controlled, phase III trial was undertaken at 19 sites in England and Wales. The trial was independently overseen by an independent data safety monitoring committee and a trial steering committee.
Study population
Children were eligible to participate if they were aged between 3 years and 15 years 8 months at registration visit, had a neurodevelopmental disorder scoring 1.5 SD or more below the mean on the adaptive behaviour assessment system (ABAS),11 and had a sleep disorder reported by parents for at least the past five months characterised as failing to fall asleep within one hour of “lights off” in three nights out of five or achieving less than six hours of continuous sleep in three nights out of five, or both. Children were required to be free from drugs that could cause sleepiness and no have taken no melatonin within the preceding five months. At registration, parents/carers were provided with a booklet of advice on previously trialled and standardised sleep behaviour treatment.12 This was used as a run in to ensure that children who progressed to the randomisation phase did not include those whose sleep disorder could have been amenable to treatment with non-pharmacological intervention. Sleep was monitored during the registration period by using sleep diaries completed by parents, and children were randomised if they continued to fulfil the eligibility criteria with the sleep disorder criteria evident from these sleep diaries.
Study intervention
The child’s age appropriate bedtime was established at the start of the registration period and the trial drug was administered 45 minutes before this time either orally or through a feeding tube if required. If the child was tube fed, the capsule was opened and the study treatment suspended in an appropriate medium.12 At randomisation, each child was given 0.5 mg. At each of four weekly intervals, the child’s sleep pattern, as recorded on the sleep diary, was reviewed and the dose was increased to the next dose increment on the basis that the child fulfilled the sleep disorder eligibility criteria, had received at least five of the possible seven doses in the preceding week, and had not experienced any serious adverse events. There was a maximum of three dose increments from 0.5 mg, 2 mg, 6 mg, and a maximum of 12 mg. Step down in dose was possible if adverse effects were experienced at a higher dose. Participants were followed up for 12 weeks from randomisation with a combination of home visits, telephone calls, and clinic attendance.
Randomisation
The trial statistician generated randomisation lists in Stata (release 9, College Station, TX) in a 1:1 ratio using block randomisation with random variable block lengths of two and four stratified by centre. The statistician had no further access until determination of the analysis population. The placebo capsules and contents were identical in internal and external appearance. Treatment packs were numbered sequentially and dispensed by the pharmacy of each site. Treatment packs held enough drugs for the 12 week period and allowed for potential dose escalation. All trial staff and participants were blind to treatment allocation throughout the trial.
Measuring sleep
The trial design included both subjective (diary) and objective (actigraphy) measures of sleep, as recommended by Sadeh.13 There are benefits with each approach and reasons why the results might not be concordant4 7; for example, sleep diaries would not detect periods when the child was awake but not disturbing the household (a particular concern for determining sleep onset latency), and actigraphy could interpret restless sleep as being awake. Between registration and study completion, parents were asked to complete weekly sleep diaries.
The actigraph (MicroMini-Motionlogger, Ambulatory Monitoring, New York), an accelerometer, is worn on the wrist and movement is monitored continuously and stored within the unit. Subsequent analysis of frequency and pattern of movement by means of validated algorithms permits detection of basic sleep-wake patterns.13 Children wore the actigraph continuously between registration and randomisation and the 12th week after randomisation.
Study outcomes
The primary outcome was total sleep time, measured by diaries completed by parents. Each night the minutes between the times that the child went to sleep and woke up the next morning were calculated minus any night time awakenings. A minimum of five out of seven nights’ data at baseline (the week before randomisation) and during the final week were required and the weekly average calculated at each time point.
Secondary sleep outcomes included total sleep time measured by actigraphy; sleep onset latency measured by diaries and actigraphy; and sleep efficiency (the proportion of time spent in bed asleep) measured by actigraphy. Sleep onset latency measured the time taken for a child to go to sleep from “snuggle down” time recorded on the sleep diary for both sleep diary and actigraphy measures, with onset of sleep determined by the respective methods.
Four questionnaires were completed at baseline and at the final visit: the composite sleep disturbance index (CSDI; based on allocating scores according to the frequency and duration of sleep problems reported by parents in questionnaires)14 15 16; the aberrant behaviour checklist (ABC) to assess behavioural problems17 18; the family impact module of the paediatric quality of life inventory (PedsQL) to assess the quality of life of the care giver19; and the Epworth sleepiness scale (ESS) to assess the daytime sleepiness of the care giver.20 We used a seven point Likert scale to assess parental perception of child’s sleep quality.
We measured salivary melatonin concentrations for each participant to calculate dim light melatonin onset (DLMO). Melatonin is a hormone produced by the pineal gland in a circadian rhythm influenced by light levels. Concentrations are usually low during the day, but as evening approaches they start to rise sharply peaking at around midnight. The beginning of this rise is what is known as the dim light melatonin onset time. Salivary samples were collected at two time points on the night before the randomisation clinic visit and at the beginning of the 11th week with two nights of trial treatment omitted. Saliva samples were collected hourly from 5 pm until the child’s usual bedtime. A minimum of 2 ml of saliva was obtained by asking the child to spit into a tube or by placing a saliva sponge in the buccal cavity of the child’s mouth.
Saliva samples were also taken for DNA analysis to identify genetic polymorphisms associated with the sleep outcomes. DNA analyses are ongoing.
Safety assessments
A paediatrician physically examined the children at the screening and final visits. The frequency and severity of spontaneously reported adverse events were recorded weekly along with prompted reports of adverse events of interest (treatment emergent signs and symptoms) covering somnolence, increased excitability, mood swings, rash, hypothermia, and cough. Weekly seizure diaries recording the type and number of seizures were completed for those children with a pre-existing diagnosis of epilepsy. The Investigator’s Brochure was referred to in the assessment of causality and expectedness.
Exploratory analyses
Interactions between treatment and autism, the type of sleep disorder (categorised as delayed sleep onset, poor sleep maintenance, or both), baseline measurements, and child’s age and weight were considered for the primary outcome and sleep onset latency as post hoc analyses.
Additional analyses assessed whether there was a change in morning wake up time and number and duration of night awakenings to determine whether the observed increase in total sleep time was explained by reduced sleep onset latency.
Statistical considerations
We used the “intention to treat” principle throughout and undertook analyses with SAS (version 9.1.3, Cary, NC). Results are presented with 95% confidence intervals. Continuous outcomes are presented with means and standard deviations at baseline, at study completion (week 12), and for the change from baseline for each group. We used analysis of covariance to adjust results for the dependent variables (total sleep time, sleep onset latency) measured at baseline and in exploratory analyses for treatment covariate interactions.
The trial was originally designed with two primary outcomes: total sleep time according to the sleep diary and sleep onset latency measured with actigraphy. During trial recruitment we observed high rates of missing data (66%) for actigraphy so we re-designated sleep onset latency as a secondary outcome and removed the Bonferroni multiplicity adjustment21 in a protocol amendment. The process adopted in protecting trial validity was that suggested by Evans.22
Total sleep time was powered at 80% with a 5% significance level to detect a change from baseline of one hour between the melatonin and placebo group with a common standard deviation of 1.7.23 24 Allowing for 20% missing data based on observed rates at the time of the amendment, we calculated we needed 57 participants in each group.
We reassessed the estimate of the common standard deviation used in the sample size calculation after the first 20 participants as 1.2 (95% confidence interval 0.8 to 1.7), and the independent data safety monitoring committee recommended the trial continue without revision of the sample size calculation for the estimated standard deviation used.
Results
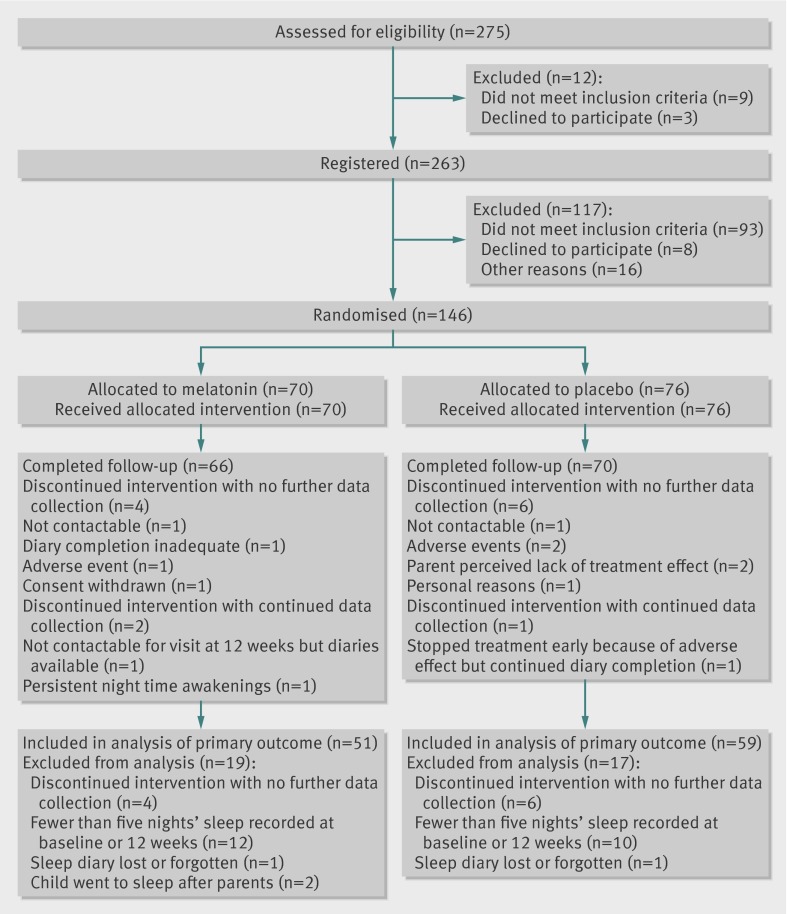
The first participants were registered and randomised on 11 December 2007 and 28 January 2008, respectively, and the last registered and randomised on 7 May 2010 and 4 June 2010. All children had intellectual/learning disability and included those with epilepsies, autistic spectrum disorders, and a range of genetic and chromosomal disorders. The CONSORT diagram shows the screening, randomisation, and follow-up of the patients . Baseline characteristics were similar between the groups (table 1).
Screening, randomisation, and follow-up of children with neurodevelopmental disorders and sleep disorders allocated to melatonin or placebo
Table 1.
Baseline characteristics of children with neurodevelopmental disorders in study of effect of melatonin on sleep problems
| Baseline characteristic | Melatonin (n=70) | Placebo (n=76) |
|---|---|---|
| No (%) of boys | 49 (70) | 48 (63) |
| Mean (SD; range) age (months) | 106 (34.8; 44-181) | 100.7 (37.4; 37-186) |
| Mean (SD; range) ABAS-GAC score | 50.8 (9.9; 40-73) | 51.9 (11.3; 10-74) |
| No (%) by neurodevelopmental delay: | ||
| Developmental delay (DD) alone | 13 (19) | 9 (12) |
| DD and epilepsy | 8 (11) | 5 (7) |
| DD and autistic spectrum disorder (ASD) | 30* (43) | 30 (39) |
| DD, ASD, epilepsy | 0 | 3 (4) |
| DD and “other” | 19* (27) | 29 (38) |
| No (%) by sleep disorder†: | ||
| Delayed sleep onset | 27 (40.3) | 29 (39.2) |
| Poor sleep maintenance | 10 (14.9) | 16 (21.6) |
| Poor sleep onset and maintenance | 30 (44.8) | 29 (39.2) |
ABAS GAC=adaptive behaviour assessment system-general adaptive composite.
*One participant was re-classified from having DD and “other” to DD and ASD by independent assessment by PG and RA.
†Not classified for three participants receiving melatonin and two receiving placebo.
The proportion of randomised participants who completed follow-up was high at 94% (66/70) for melatonin and 92% (70/76) for placebo. Proportions included within the primary outcome analysis were 73% (51/70) for melatonin and 78% (59/76) for placebo, largely because of the longitudinal data required (minimum of five nights’ complete sleep diary). We conducted a range of sensitivity analyses with regards to the missing data. These sensitivity analyses, which included reducing the number of nights’ sleep required to contribute to the analysis and imputing worse/best recorded sleep parameters to complete the sleep diaries, showed the robustness of conclusions.
Dose escalation
Table 2 shows that participants randomised to placebo titrated more rapidly up to the maximum dose capsules. Twelve weeks after randomisation only 19 (38%) participants receiving active melatonin had escalated to the maximum dose (12 mg) compared with 49 (83%) receiving placebo. Nine children (18%) in the active group remained taking the lowest dose (0.5 mg) compared with one child (2%) in the placebo group.
Table 2.
Dose escalation for participants included in primary outcome analysis of effect of melatonin on sleep problems in children with neurodevelopmental disorders
| No (%) receiving melatonin (n=51*) | No (%) receiving placebo (n=59) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0.5 mg | 2 mg | 6 mg | 12 mg | 0.5 mg | 2 mg | 6 mg | 12 mg | ||
| Dose escalation phase | |||||||||
| Baseline | 51 (100) | 0 | 0 | 0 | 59 (100) | 0 | 0 | 0 | |
| Week 1 | 19 (37) | 32 (63) | 0 | 0 | 10 (17) | 49 (83) | 0 | 0 | |
| Week 2 | 13 (26) | 15 (29) | 23 (45) | 0 | 4 (7) | 15 (25) | 40 (68) | 0 | |
| Week 3 | 10 (20) | 15 (29) | 8 (16) | 18 (35) | 1 (2) | 9 (15) | 18 (31) | 31 (53) | |
| Week 4 | 9 (1) | 13 (26) | 10 (20) | 19 (37) | 1 (2) | 4 (7) | 12 (20) | 42 (71) | |
| Dose maintenance phase | |||||||||
| Week 5 | 9 (18) | 13 (26) | 10 (20) | 19 (37) | 1 (2) | 5 (9) | 10 (17) | 43 (73) | |
| Week 6 | 9 (18) | 12 (24) | 10 (20) | 20 (39) | 1 (2) | 3 (5) | 9 (15) | 46 (78) | |
| Week 7 | 8 (16) | 11 (22) | 12 (24) | 20 (39) | 1 (2) | 3 (5) | 5 (9) | 50 (85) | |
| Week 8 | 8 (16) | 11 (22) | 12 (24) | 19 (38) | 1 (2) | 3 (5) | 6 (10) | 49 (83) | |
| Week 9 | 8 (16) | 11 (22) | 11 (22) | 20 (40) | 1 (2) | 3 (5) | 6 (10) | 49 (83) | |
| Week 10 | 9 (18) | 10 (20) | 12 (24) | 19 (38) | 1 (2) | 4 (7) | 5 (9) | 49 (83) | |
| Week 11 | 9 (18) | 10 (20) | 12 (24) | 19 (38) | 1 (2) | 5 (9) | 4 (7) | 49 (83) | |
| Week 12 | 9 (18) | 10 (20) | 12 (24) | 19 (38) | 1 (2) | 4 (7) | 5 (9) | 49 (83) | |
*At each of weeks 8-12 one child was withdrawn, total=5.
Sleep outcomes
Table 3 provides results for primary and secondary sleep outcomes. Melatonin increased total sleep time as measured with sleep diaries (P=0.04), the primary outcome, but the confidence interval excluded the 60 minute value determined to be the minimum clinically relevant. The increase in total sleep time was reduced as measured by actigraphy (P=0.36). A range of prespecified sensitivity analyses showed the robustness of conclusions to missing data.
Table 3.
Primary and secondary sleep outcomes in study of effect of melatonin on sleep problems in children with neurodevelopmental disorders. Figures are means (SD)
| Melatonin | Placebo | Adjusted difference | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No of children | Baseline | Week 12 | Change | No of children | Baseline | Week 12 | Change | |||
| Sleep diary | ||||||||||
| Total sleep (min) | 51 | 530.8 (64.8) | 571.3 (72.0) | 40.5 (71.8) | 59 | 545.5 (66.0) | 558.0 (68.9) | 12.5 (52.5) | 22.4 (0.5 to 44.3)* | |
| Sleep onset latency (min) | 54 | 102.0 (72.6) | 54.8 (51.9) | −47.2 (64.4) | 59 | 102.1 (57.7) | 92.4 (63.0) | −9.7 (49.6) | −37.5 (−55.3 to −19.7)† | |
| Actigraphy | ||||||||||
| Total sleep (min) | 30 | 434.2 (72.3) | 449.9 (73.8) | 15.7 (63.6) | 29 | 412.3 (83.2) | 420.6 (82.9) | 8.3 (52.0) | 13.3 (−15.5 to 42.2) | |
| Sleep onset latency (min) | 24 | 126.8 (71.5) | 68.4 (41.0) | −58.3 (53.7) | 25 | 107.8 (54.9) | 104.1 (59.5) | −3.71 (47.4) | −45.3 (−68.8 to −21.9)† | |
| Sleep efficiency‡ (%) | 30 | 65.4 (11.3) | 70.23 (11.3) | 4.8 (9.8) | 28 | 63.3 (12.3) | 64.83 (11.7) | 1.56 (9.5) | 4.03 (−0.6 to 8.7) | |
*P<0.05.
†P<0.001.
‡No of minutes spent sleeping in bed/total No of minutes spent in bed)×100.
Melatonin reduced sleep onset latency when measured by both sleep diaries (P<0.001) and actigraphy (P<0.001). The size of the improvement was larger when measured by actigraphy (37.5 v 45.3 minutes). Sleep efficiency did not improve with melatonin (P=0.09).
Questionnaire outcomes
Table 4 summarises the questionnaire outcomes. The composite sleep disturbance index (CSDI) showed a significant reduction favouring melatonin, indicating that parents thought the frequency and duration of sleep problems had reduced after treatment with melatonin. The Epworth sleepiness scale showed a clinically small but statistically significant improvement of 1.6 points on the 24 point scale for melatonin compared with placebo.
Table 4.
Outcomes of questionnaires used to determine effect of melatonin on sleep problems in children with neurodevelopmental disorders. Figures are mean (SD) scores
| Melatonin | Placebo | Adjusted difference (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No of children | Baseline | Week 12 | Change | No of children | Baseline | Week 12 | Change | |||
| CSDI scale 0-12 | 60 | 7.5 (2.4) | 5.1 (2.9) | −2.4 (2.8) | 65 | 7.0 (2.1) | 5.8 (2.5) | −1.3 (2.2) | −1.00 (−1.8 to −0.2)* | |
| Aberrant behaviour checklist: | ||||||||||
| Irritability, agitation, crying (scale 0-45) | 64 | 16.6 (10.3) | 13.5 (10.1) | −3.1 (6.6) | 68 | 15.5 (10.3) | 13.6 (10.0) | −1.9 (6.7) | −1.0 (−3.1 to 1.2) | |
| Lethargy, social withdrawal (scale 0-48) | 60 | 12.4 (9.6) | 9.3 (8.3) | −3.1(6.2) | 67 | 10.8 (8.8) | 8.0 (7.5) | −2.8(6.0) | 0.3 (−1.5 to 2.1) | |
| Stereotypic behaviour (scale 0-21) | 64 | 6.1 (4.9) | 5.1 (4.5) | −1.0 (3.6) | 69 | 5.0 (4.8) | 4.3 (4.1) | −0.7 (3.4) | 0.1(−0.9 to 1.2) | |
| Hyperactivity, non- compliance (scale 0-48) | 64 | 23.5 (9.9) | 18.6 (10.4) | −4.9 (7.7) | 68 | 21.9 (11.1) | 18.9 (11.2) | −3.0 (8.5) | −1.5 (−4.1 to 1.2) | |
| Inappropriate speech (scale 0-12) | 64 | 4.8 (3.2) | 3.5 (2.7) | −1.3 (2.7) | 67 | 3.7 (3.2) | 3.2 (3.2) | −0.6 (2.2) | −0.4 (−1.1 to 0.4) | |
| PedsQL family impact module: | ||||||||||
| HRQoL (scale 0-100) | 64 | 53.3 (17.5) | 58.7 (20.8) | 5.4 (14.7) | 69 | 56.2 (18.0) | 57.5 (20.6) | 1.3 (15.7) | 3.5 (−1.6 to 8.7) | |
| Family functioning (scale 0-100) | 64 | 50.2 (21.3) | 56.6 (23.6) | 6.4 (16.9) | 69 | 50.1 (22.8) | 52.1 (23.7) | 2.0 (14.6) | 4.4 (−0.8 to 9.7) | |
| ESS (scale 0-24) | 62 | 6.7 (5.4) | 5.4 (4.5) | −1.3 (5.0) | 66 | 6.9 (5.3) | 7.1 (5.0) | 0.3 (3.8) | −1.6 (−2.9 to −0.3)* | |
CSDI=composite sleep disturbance index; PedsQL=paediatric quality of life inventory; HRQoL=health related quality of life; ESS=Epworth sleepiness scale.
*P<0.05
†Higher scores are worse for CSDI, ABC, and ESS, and lower scores are worse for PedsQL.
The results of the other measures tended to favour melatonin but were not significant (table 5).
Table 5.
Global measure of parents’ perception of child’s sleep quality in study of effect of melatonin on sleep problems in children with neurodevelopmental disorders. Figures are means (SD)
| Melatonin (n=52) | Placebo (n=55) | Adjusted difference (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Week 12 | Change | Baseline | Week 12 | Change | |||
| Mean % of dissatisfied night sleeps | 31.3 (34.3) | 24.0 (33.2) | −7.3 (35.5) | 33.7 (35.3) | 31.0 (36.3) | −2.7 (36.9) | −5.9 (−17.8 to 6.1) | |
| Mean scores | 3.8 (1.2) | 3.4 (1.4) | −0.4 (1.4) | 4.0 (1.3) | 3.7 (1.2) | −0.3 (1.4) | −0.2 (−0.7 to 0.2) | |
Salivary melatonin
After randomisation, 67% (47/70) and 79% (60/76) of participants on melatonin and placebo, respectively, provided saliva samples for the calculation of dim light melatonin onset, of which 15 and 12, respectively, were of insufficient volume for analysis and the time of onset could not be ascertained for 25 (melatonin) and seven (placebo) participants. This difference between the two groups was not detected before randomisation. Where onset could not be calculated the reasons were possible contamination (23 melatonin and three placebo); high baseline concentrations (two melatonin), and low volume (four placebo). The limited data prevent meaningful analysis of the impact of this phenomenon on treatment response.
Tolerability outcomes
Table 6 shows the number of participants experiencing any treatment emergent sign or symptom (TESS). No formal statistical tests were undertaken, and the results for each group seemed similar. Seven serious adverse events were reported, of which two (one in the placebo group and one in the melatonin group) were considered related to the study drug in a blinded assessment.
Table 6.
Treatment emergent signs and symptoms (TESS) in study of effect of melatonin on sleep problems in children with neurodevelopmental disorders
| Event | Melatonin (n=70) | Placebo (n=76) | |||
|---|---|---|---|---|---|
| No (%) of children | Events | No (%) of children | Events | ||
| Prompted adverse events report (TESS) | |||||
| Coughing | 22 (31.4) | 36 | 28 (36.8) | 42 | |
| Mood swings | 16 (22.9) | 34 | 17 (22.4) | 25 | |
| Vomiting | 15 (21.4) | 29 | 18 (23.7) | 32 | |
| Increased excitability | 13 (18.6) | 23 | 16 (21.1) | 19 | |
| Rash | 11 (15.7) | 17 | 8 (10.5) | 10 | |
| Somnolence | 9 (12.9) | 14 | 10 (13.2) | 13 | |
| Hypothermia | 6 (8.6) | 8 | 4 (5.3) | 4 | |
| Increased activity* | 6 (8.6) | 12 | 9 (11.8) | 13 | |
| Nausea* | 3 (4.3) | 3 | 11 (14.5) | 13 | |
| Dizziness | 1 (1.4) | 2 | 5 (6.6) | 6 | |
| Breathlessness* | 1 (1.4) | 2 | 1 (1.3) | 1 | |
| Hung-over feeling* | 1 (1.4) | 1 | 0 (0) | 0 | |
| Tremor* | 0 (0) | 0 | 0 (0) | 0 | |
| Seizures | 0 (0) | 0 | 1 (1.3) | 1 | |
| Unprompted adverse events spontaneously reported | |||||
| Fatigue | 8 (11.4) | 14 | 8 (10.5) | 10 | |
| Headache | 10 (14.3) | 12 | 7 (9.2) | 14 | |
| Other | 31 (44.3) | 82 | 40 (52.6) | 107 | |
*Originally included within TESS but removed in April 2009.
Sixteen children (eight in each group) had a diagnosis of epilepsy before randomisation. Thirteen of these 16 children experienced seizures in the period between randomisation and the end of the study; none showed any deterioration in seizure control or emergence of a new seizure type during this period. No child developed seizures or a new diagnosis of epilepsy.
Exploratory analyses
Tables 7 and 8 show the results of exploratory analyses . The treatment effect was not modified by the presence of autism (P=0.85) or by the type of initial sleep disorder as reported by care givers for total sleep time (P=0.56) or sleep onset latency (autism P=0.56, sleep disorder P=0.43). Inclusion of age or weight in the models did not improve the fit. The magnitude of sleep onset latency as determined by baseline sleep diaries, however, modified the treatment effect for sleep onset latency such that melatonin had a greater effect in those with a greater problem of getting to sleep (P=0.009); this was not evident for total sleep time (P=0.19).
Table 7.
Frequency and duration of night time awakenings and wake up time in study of effect of melatonin on sleep problems in children with neurodevelopmental disorders
| Melatonin (n=51) | Placebo (n=59) | Adjusted difference (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Week 12 | Change | Baseline | Week 12 | Change | |||
| No of wakes | 0.9 (1.3) | 0.8 (1.2) | −0.1 (−0.4 to 0.1) | 0.7 (1.6) | 0.6 (1.5) | −0.1 (−0.3 to 0.1) | 0.0 (−0.3 to 0.3) | |
| Total duration of nightly wakes (min) | 24.5 (32.7) | 16.8 (26.3) | −7.7 (−15.5 to 0.2) | 11.0 (17.4) | 9.7 (22.3) | −1.3 (−8.6 to 6.0) | 2.8 (−6.2 to 11.7) | |
| Wake up time (min from midnight) | 443.1 (59.1) | 426.4 (66.2) | −16.7 (−103.3 to 70.0) | 453.9 (54.6) | 464.8 (57.3) | 10.9 (−77.1 to 98.9) | −29.9 (−46.3 to −13.6)* | |
*P<0.001.
Table 8.
Exploratory regression models in study of effect of melatonin on sleep problems in children with neurodevelopmental disorders. Figures are estimates (95% confidence intervals)
| Total sleep time (min) | Sleep onset latency (min) | |
|---|---|---|
| Autism | ||
| Model A (12 week mean=baseline mean+treatment group+autism): | ||
| Intercept | 218.3 (125.3 to 11.3) | 43.5 (23.3 to 63.8) |
| Mean at baseline | 0.6 (0.5 to 0.8)*** | 0.5 4 (0.4 to 0.6) |
| Treatment | 22.8 (0.8 to 44.8 )* | −37.1 (−54.9 to −19.2)*** |
| Autism | −6.9 (−28.9 to 15.2) | −7.7 (−25.7 to 10.3) |
| Model B (12 week mean=baseline mean+treatment group+autism+treatment group×autism): | ||
| Intercept | 218.7 (125.2 to 312.2) | 41.4 (19.7 to 63.0) |
| Mean at baseline | 0.6 (0.5 to 0.8)*** | 0.5 (0.4 to 0.6)*** |
| Treatment | 21.0 (−8.1 to 50.1)* | −32.5 (−56.3 to −8.6)*** |
| Autism | −8.8 (−39.3 to 21.6)** | −2.6 (−27.7 to 22.6) |
| Treatment×autism | −4.1 (−40.3 to 48.5)*** | −10.5 (−46.6 to 25.6) |
| Sleep disorder | ||
| Model A (12 week mean=baseline mean+treatment group+sleep disorder): | ||
| Intercept | 212.9 (118.4 to 307.4) | 53.3 (28.7 to 77.9) |
| Mean at baseline | 0.6 (0.5 to 0.8)*** | 0.5 (0.4 to 0.7)*** |
| Treatment | 23.2 (0.6 to 45.7)* | −41.5 (−58.9 to −24.0)‡ |
| Sleep disorder (maintenance v onset) | 7.2 (−26.2 to 40.5) | −29.1 (−56.9 to −1.3) |
| Sleep disorder (maintenance and onset v onset) | 3.5 (−20.8 to 27.8) | −14.1 (−33.6 to 5.4) |
| Model B (12 week mean=baseline mean+treatment group+sleep disorder category+treatment group×sleep disorder : | ||
| Intercept | 208.8 (112.1 to 305.4) | 58.2 (32.1 to 84.4) |
| Mean at baseline | 0.6 (0.5 to 0.8)*** | 0.5 (0.4 to 0.7)*** |
| Treatment | 30.5 (−5.6 to 66.5) | −50.0 (−77.9 to −22.0)*** |
| Sleep disorder (maintenance v onset) | 12.1 (−30.6 to 54.8) | −43.1 (−78.0 to −8.2) |
| Sleep disorder (maintenance and onset v onset) | 9.2 (−24.5 to 42.9) | −17.5 (−43.8 to 8.8) |
| Treatment× Sleep disorder (maintenance v onset) | −12.1 (−80.9 to 56.7) | 35.3 (−17.9 to 88.5) |
| Treatment× Sleep disorder (maintenance and onset v onset) | −12.1 (−61.1 to 36.9) | 7.0 (−31.6 to 45.5) |
| Baseline interaction | ||
| Model (12 week mean=baseline mean+treatment group+baseline mean×treatment group: | ||
| Intercept | 160.6 (36.7 to 284.6) | 18.3 (−6.2 to 42.7) |
| Mean at baseline | 0.7 (0.5 to 1.0)*** | 0.7 (0.5 to 0.9)*** |
| Treatment | 143.1 (−38.2 to 324.6) | −0.4 (−33.1 to 32.4) |
| Mean baseline×treatment | −0.2 (−0.6 to 0.1) | −0.4 (−0.6 to −0.9)** |
*P<0.05, **P<0.01, ***P<0.001.
No differences were observed between groups for change in average duration or frequency of night time awakenings.
Children woke 16.7 minutes earlier than at baseline after 12 weeks of treatment with melatonin, compared with children in the placebo group who woke an average of 10.9 minutes later than at baseline (table 7). The comparison between groups was significant (P<0.001), with children in the melatonin group waking on average 29.9 minutes earlier than children in the placebo group after adjustment for baseline (95% confidence interval 13.6 to 46.3).
Discussion
In children with neurodevelopmental disorders and sleep problems, immediate release melatonin was found to be more effective than placebo in increasing total sleep time and reducing sleep onset latency. In this randomised double masked placebo controlled trial, adverse effects were few, mild in degree, and distributed equally between the two groups with no increase in, or new onset of, epileptic seizures. Total sleep time increased by an average of 23 minutes and sleep onset latency reduced by an average of 38 minutes.
Relation to other studies
Several systematic reviews have aimed to determine the effect of melatonin on sleep parameters (table 9). The inclusion criteria of the systematic reviews vary as do the conclusions regarding the effect of melatonin, from definitive absence of effect10 to evidence of effect,8 and emphasising the need for large confirmatory randomised controlled trials.4 7
Table 9.
Summary of findings from systematic reviews of melatonin v placebo to treat sleep disorders
| Population | Total sleep time (TST) | Sleep onset latency (SOL) | Authors’ conclusions | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No of trials | No of children | Estimate (95% CI) | No of trials | No of children | Estimate (95% CI) | ||||
| Buscemi,10 12 trials, 7 crossover | Secondary sleep disorders; heterogeneous population | 9 | 382 | WMD: 15.6 (7.2 to 24.0) | 6 | 163 | WMD: −13.2 (−27.3 to 0.9) | No significant effect on SOL and small and clinically unimportant effect on sleep efficiency | |
| Braam,8 9 trials, 7 crossover | Intellectual disability, adults and children | 7 | 257 | WMD: 49.8 (34.2 to 64.8) | 7 | 273 | WMD: −33.8 (−42.97 to −24.70) | Decreases sleep latency and increases total sleep time | |
| Rossignol,7 5 controlled trials, 5 crossover, 57 patients | Autistic spectrum disorders | 5 | 5 | Hedge’s g: 1.07 (0.49 to 1.65); Glass’s Δ: 0.93 (0.33 to 1.53)* | 5 | 57 | Hedge’s g: 2.46 (1.96 to 2.98); Glass’s Δ: 1.28 (0.67 to 1.89)† | Improved sleep parameters and minimal side effects. Call for large RCT | |
| Phillips,4 3 cross over studies, 35 children | Children with neurodevelopmental disabilities | No meta-analysis | No meta-analysis | Might be effective in reducing SOL. No evidence of effect on TST. Call for large RCT | |||||
WMD=weighted mean difference.
*44 min longer TST with melatonin.
†39 min shorter SOL with melatonin.
The trials included within each meta-analysis were heterogeneous in terms of populations of patients and the dose, time, and durations of study treatments. Of methodological concern are the number of small trials, suspicions of outcome reporting bias25 within the trials,26 and the use of a crossover design, the suitability of which has been questioned because of the impact on the circadian timing system outlasting drug washout periods.8 27
The impact of varying methods used to measure sleep, while not considered to be of importance in Buscemi and colleagues,10 has been discussed by Rossignol and Frye7 and Philips and Appleton.4 The differences in the methods used are evident in the results of our study, particularly for total sleep time. The difference could in part be attributed to night wakenings missed by parents, though, as described by Philips and Appleton,4 the relevance and clinical importance of changes in sleep pattern that are not noted by parents and do not disrupt their own sleep is debatable.
The effect estimate of melatonin on total sleep time in our study is largely consistent with that reported by Buscemi and colleagues,10 while the estimates reported by Rossignol and Frye7 and Braam and colleagues8 in patients with intellectual disability and autistic spectrum disorders extend to the upper limit of our confidence interval. This is in contrast with a recent open label dose escalation study of 24 children with autism, which reported no improvement on total sleep time.28 Our exploratory analysis did not identify autism as a modifier of treatment effect, suggesting the differences in the size of effect are not explained by differences in populations of patients.
The effect of melatonin on sleep onset latency was both clinically and statistically significant based on both sleep diaries and actigraphic measures. The minimum clinically relevant difference defined a priori was 30 minutes and was held within the confidence intervals for both sleep diaries and actigraphy. This reduction is consistent with other reports of the use of melatonin in typically developing children (35 minutes),29 children with intellectual disabilities (34 minutes),8 and children with autism (39 minutes).7 In keeping with a recent study on typically developing children we found that melatonin was most effective for those children with the longest sleep latency.29 The finding that our children receiving melatonin woke earlier than controls by the end of the three month study is interesting and has not been previously reported in children with neurodevelopmental disorders. It is consistent with the effect of melatonin in laboratory controlled studies30 and suggests that evening exogenous melatonin advances sleep phase over time and therefore children fall asleep earlier but also wake earlier, explaining the smaller effect on total sleep time.
Results for dim light melatonin onset were disappointing. If samples are taken regularly for a 24 hour period the onset should be measurable, whenever it occurs. For practical reasons, however, it is common in paediatric populations to take five swabs before bedtime. It is therefore possible to “miss” an onset that precedes sampling or occurs when sampling has finished. Some of the contamination and high baseline values in the melatonin arm could reflect children who are poor metabolisers and whose concentrations of exogenous melatonin had accumulated during the study; however, it might also reflect that the dose of melatonin was not actually omitted on the two nights as required in the protocol.
Only low doses of melatonin are required to alter the sleep phase in typically developing children, and, in this study, there was support for starting treatment with a low dose of melatonin with 18% of children needing only 0.5 mg melatonin. Although high doses might usefully promote the sedative action of melatonin in some children with neurodevelopmental disorders, this might not be the case for slow metabolisers of melatonin.31
Measures of child behaviour and family quality of life tended to favour melatonin but were not significant. There are several possible explanations for this, including the possibility that our measures were not sensitive enough over this time period. We speculate that this might also be because of the relatively minor effect melatonin had on total sleep time across this study.
Strengths and limitations
This was the first randomised controlled trial specifically designed and powered to assess the impact of melatonin on total sleep time over a three month period. We used subjective and objective assessments of sleep and had a standardised parental sleep behavioural intervention before treatment with melatonin during which a routine bedtime was established. We also had a systematic dose escalation protocol and included secondary outcomes such as behavioural function and quality of life measures. The study had a relatively long duration (one month behavioural intervention and then three month drug trial) and wide inclusion criteria across all children with neurodevelopmental delay, maximising generalisability of results to everyday clinical practice.
A limitation is the relatively high number of participants who were either unable to tolerate actigraphy or in whom actigraphy equipment failed. Unfortunately, the combination in many children of both autistic spectrum disorders (in particular sensory sensitivities) and severe learning difficulties meant that actigraphy was often not well tolerated, and more watches were broken or lost than expected. We have considerable previous clinical and research experience using actigraphy, but few studies have attempted to use actigraphy for this period of time in this particular population. In a shorter open label study of children with autism and normal intelligence, 25% of actiwatches still needed to be used in alternative places.28 Although we decided not to use non-standard actigraphy placements such as shoulder/waist for this study, this should be an important consideration for future similar trials. Carers’ diaries, even for this prolonged period, were well received in this study in contrast with other reports.7 32
Our 95% confidence intervals for total sleep time did not contain the minimum clinically important difference of 60 minutes that we defined before the study. Although this figure was reached through consensus with experts and carers at the time, we acknowledge the growing body of evidence suggesting that smaller increase in total sleep time might be worthwhile over cumulative nights.33 Our definition of a sleep disorder did not vary across the age range of children included, potentially meaning that younger children experienced greater deviation from sleeping habit norms than older children, though exploratory analyses found no effect of age or weight.
Our findings provide valuable evidence about the dosing, tolerability, and effect of using melatonin in children with neurodevelopmental and sleep disorders. They explain that although (standard) immediate release melatonin significantly reduces sleep onset latency, there is a more limited increase in total sleep time that might arise as a result of increasingly early waking time in the morning. Melatonin seemed tolerable in this population of children with a range of neurological and developmental disorders. We cannot comment on the efficacy of slow release or combined preparations, which could be important alternatives. Only head to head trials with other drugs, including slow release melatonin and hypnotics/sedatives, will help clinicians and families decide which is the safest and most effective.
What is already known on this topic
Sleep disorders are common in children with neurodevelopmental disorders
In these children, melatonin is widely prescribed at varying doses
Systematic reviews have had inconsistent conclusions
What this study adds
Children given melatonin fall asleep earlier, but after three months’ treatment also wake up earlier
The major effect of melatonin is on sleep latency, rather than total sleep time
Doses of melatonin as low as 0.5 mg can be effective
The presence of autism is not a significant moderator of treatment effect
We thank the children and families who participated in this study. We acknowledge the support of the National Institute for Health Research, through the Medicines for Children Research Network (MCRN) and local research networks. The study was included on the UK CRC portfolio and supported by the UK Medicines for Children Research Network (MCRN) and conducted through the MCRN clinical trials unit. We also thank the independent trial steering committee (chaired by Stuart Logan, Andy Vail, and Anthony McShane) and independent data monitoring committee (chaired by Anthony Marson, David Jones, and John Gibbs) and Sally Eagle for additional analyses. The trial supplies, active drug and placebo, were manufactured by Penn Pharmaceuticals for which costs were provided by Alliance Pharma, who had no other involvement in the study.
Contributors: PG and RA were involved in the design of the study, the funding application, development of the protocol, and recruitment of patients as a local principal investigator, was co-chief investigator for the trial and a member of the trial management group, and co-wrote the paper. CG contributed to the design of the study and the funding application, led the statistical team covering development of the data collection tool, helped in data monitoring, co-wrote the statistical analysis plan, was a member of the trial management group, and co-wrote the paper. APJ was a member of the trial management group, cleaned and analysed the data, co-wrote the statistical analysis plan, prepared the monitoring reports and the final report, and commented on drafts of the paper. LW contributed to the design of the study and the funding application, advised on the use of actigraphy and outcomes reported by patients, was a member of the trial management group, and commented on drafts of the paper. PRW led the design of the trial, the funding application, and development of the protocol, was a member of the trial management group, and commented on drafts of the final paper. AS was involved in the design of the protocol, the funding application, recruitment of patients as a local principal investigator, was a member of the trial management group, and provided comments on the draft paper. PM contributed to the design of the study and the funding application, advised on the use of actigraphy and outcomes reported by patients, was a member of the trial management group, and commented on drafts of the paper. WPW contributed to the design of the trial and the funding application, organised and analysed pre-protocol consumer involvement, helped to recruit patients as a local principal investigator, and commented on a draft of the paper. IC, TA, and AE were involved in the funding application, recruitment of patients as local principal investigators, and provided comments on the draft paper. PG is guarantor.
Funding: This project was funded by the NIHR Health Technology Assessment programme (project number 05/14/02) and will be published in full in Health Technology Assessment journal. See the HTA programme website for further project information. This report presents independent research commissioned by the National Institute for Health Research (NIHR). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme, or the Department of Health.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The study was approved through the UK Integrated Research Application System (IRAS) and review board of each participating centre. Written informed consent was obtained from the legal guardians of the children before randomisation. Informed written consent was obtained from study participants when this was possible.
Data sharing: No additional data available.
Cite this as: BMJ 2012;345:e6664
Web Extra. Extra material supplied by the author
Appendix: Dose modification criteria
References
- 1.Krakowiak P, Goodlin-Jones B, Hertz-Picciotto I, Croen LA, Hansen RL. Sleep problems in chidren with autism spectrum disorders, developmental delays, and typical development: a population -based study. J Sleep Res 2008;17:197-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hill CM, Hogan AM, Karmiloff-Smith A. To sleep, perchance to enrich learning? Arch Dis Child 2007;92:637-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meltzer L, Mindell J. Relationship between child sleep disturbances and maternal sleep, mood and parenting stress: a pilot study. J Fam Psychol 2007;21:67-73. [DOI] [PubMed] [Google Scholar]
- 4.Phillips L, Appleton RE. Systematic review of melatonin treatment in children with neurodevelopmental disabilities and sleep impairment. Dev Med Child Neurol 2004;46:771-5. [DOI] [PubMed] [Google Scholar]
- 5.Czeisler C. Commentary:evidence for melatonin as a circadian phase-shifting agent. J Biol Rhythms 1997;12:618-23. [DOI] [PubMed] [Google Scholar]
- 6.Stone B, Turner C, Mills S, Nicholson A. Hypnotic activity of melatonin. Sleep 2000;23:663-9. [PubMed] [Google Scholar]
- 7.Rossignol DA, Frye RE. Melatonin in autism spectrum disorders: a systematic review and meta-analysis. Dev Med Child Neurol 2011;53:783-92. [DOI] [PubMed] [Google Scholar]
- 8.Braam W, Smits MG, Didden R, Korzilius H, van Geijlswijk M, Curfs LMG. Exogenous melatonin for sleep problems in individuals with intellectual disability: a meta-analysis. Dev Med Child Neurol 2009;51:340-9. [DOI] [PubMed] [Google Scholar]
- 9.Buscemi N, Vandermeer B, Hooton N, Pandya R, Tjosvold L, Hartling L, et al. The efficacy and safety of exogenous melatonin for primary sleep disorders. A meta-analysis. J Gen Intern Med 2005;20:1151-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buscemi N, Vandermeer B, Hooton N, Pandya R, Tjosvold L, Hartling L, et al. Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis. BMJ 2006;332:385-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrison P, Oakland T. Adaptive behaviour system-ABAS II. Pearson, 2008.
- 12.Montgomery P, Stores G, Wiggs L. The relative efficacy of two brief treatments for sleep problems in young learning disabled (mentally retarded) children: a randomised controlled tria. Arch Dis Child 2004:89:125-30. [DOI] [PMC free article] [PubMed]
- 13.Sadeh A. The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev 2011;15:259-67. [DOI] [PubMed] [Google Scholar]
- 14.Quine L. Helping parents to manage children’s sleep disturbance. An intervention trial using health professionals. HMSO, 1992.
- 15.Quine L. Sleep problems in children with mental handicap. J Mental Defic Res 1991;35:269-90. [DOI] [PubMed] [Google Scholar]
- 16.Richman N, Graham PJ. A behaviour screening questionnaire for use with three year old children. J Child Psychol Psychiatry 1971;12:5-33. [DOI] [PubMed] [Google Scholar]
- 17.Aman MG, Singh NN. Aberrant behavior checklist manual. Slosson Educational Publications, 1986.
- 18.Aman MG, Singh NN. Aberrant behavior checklist—community supplementary manual. Slosson Educational Publications, 1994.
- 19.Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P. The PedsQL family impact module: preliminary reliability and validity. Health Qual Life Outcomes 2004;2:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540-5. [DOI] [PubMed] [Google Scholar]
- 21.Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ 1995;310:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Evans S. When and how can endpoints be changed after initiation of a randomized clinical trial. PLOS Clin Trial 2007;2:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jan JE, Espezel H, Appleton RE. The treatment of sleep disorders with melatonin. Dev Med Child Neurol 1994;36:97-107. [DOI] [PubMed] [Google Scholar]
- 24.O’Callaghan FJ, Clarke AA, Hancock E, Hunt A, Osborne JP. Use of melatonin to treat sleep disorders in tuberous sclerosis. Dev Med Child Neurol 1999;41:123-6. [DOI] [PubMed] [Google Scholar]
- 25.Kirkham J, Dwan K, Altman D, Gamble C, Dodd S, Smyth R, et al. The impact of outcome reporting bias in randomised controlled trials on a cohort of systematic reviews. BMJ 2010;340:c365. [DOI] [PubMed] [Google Scholar]
- 26.Dwan KM. Outcome reporting bias in meta-analysis. University of Liverpool, 2009.
- 27.Kunz D, Mahlberg R, Muller C, Tilmann A, Bes F. Melatonin in patients with reduced REM sleep duration: two randomized controlled trials. J Clin Endocrinol Metab 2004;89:128-34. [DOI] [PubMed] [Google Scholar]
- 28.Malow B, Adkins K, McGrew S, Wang L, Goldman S, Fawkes D, et al. Melatonin for sleep in children with autism: a controlled trial examining dose, tolerability and outcomes. J Autism Dev Disord 2011;10.1007/s10803-011-1418-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van Geijlswijk IM, van der Heijden KB, Egberts ACG, Hubert PLM, Korzilius LM, Smits MG. Dose finding of melatonin for chronic idiopathic childhood sleep onset insomnia: an RCT. Psychopharmacology 2010;212:379-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lewy AJ, Sack RL. Exogenous melatonin’s phase-shifting effects on the endogenous melatonin profile in sighted humans: a brief review and critique of the literature. Biol Rhythms 1997;12:588-94. [DOI] [PubMed] [Google Scholar]
- 31.Braam W, van Geijlswijk I, Keijzer H, Smits MG, Didden R, Curfs LM. Loss of response to melatonin treatment is associated with slow melatonin metabolism. J Intellect Disabil Res 2010;54:547-55. [DOI] [PubMed] [Google Scholar]
- 32.McArthur AJ, Budden SS. Sleep dysfunction in Rett syndrome: a trial of exogenous melatonin treatment. Dev Med Child Neurol 1998;40:186-92. [DOI] [PubMed] [Google Scholar]
- 33.Jan JE, Reiter RJ, Bax MCO, Ribary U, Freeman RD, Wasdell MB. Long-term sleep disturbance in children: a cause of neuronal loss. Eur J Neurol 2010;14:380-90. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix: Dose modification criteria