Abstract
Objective
This study tested a pathway whereby acupuncturists’ communication of optimism for treatment effectiveness would enhance patients’ satisfaction during treatment, which in turn would contribute to better pain and function outcomes for patients with osteoarthritis of the knee.
Methods
Secondary analysis from a 2 arm (real vs. sham acupuncture, high vs. neutral expectations) RCT. 311 patients with knee osteoarthritis received acupuncture over 10–12 sessions. Coders rated the degree to which acupuncturists communicated optimism for the treatment’s effectiveness. Satisfaction with acupuncture was assessed 4 weeks into treatment. Pain and function were assessed 6 weeks following treatment.
Results
Patients experiencing better outcomes were more satisfied with acupuncture during treatment, were younger, and had better baseline pain and function scores. Satisfaction during treatment was greater when patients interacted with more optimistic clinicians and had higher pretreatment expectations for acupuncture efficacy.
Conclusion
Acupuncturists’ communication of optimism about treatment effectiveness contributed to pain and function outcomes indirectly through its effect on satisfaction during treatment. Future research should model pathways through which clinician-patient communication affects mediating variables that in turn lead to improved health outcomes.
Practical Implications
While clinicians should not mislead patients, communicating hope and optimism for treatment effectiveness has therapeutic value for patients.
1. Introduction
The way in which clinicians and patients communicate with one another has predicted a number of biomedical, functional, and psychological health outcomes subsequent to that consultation. (1–5) These findings suggest that effective communication accomplishes more than just greater patient satisfaction, understanding, and commitment to treatment; it actually helps people get and stay healthier. However, a closer examination of this research reveals a much more complicated picture. Communication is often not related to outcomes, or the findings are inconsistent.(2;5;6) Moreover, rarely has this research tried to identify the mechanisms or ‘pathways’ through which clinician-patient communication can lead to longer, healthier, and happier lives. (2;7–9)
Understanding the pathways through which clinician communication could lead to better health outcomes is important within the context of acupuncture treatment where the patient’s participation in treatment and interactions with the clinician can contribute to effects associated with the overall therapeutic experience.(10;11) Whereas communication could contribute to improved health in a number of ways (e.g., increased adherence, self-care skills), one way an acupuncturist’s communication could have health benefits is by elevating a patient’s belief in the value of treatment. This pathway likely will be particularly influential on patient-reported outcomes such as pain, function, and well-being. Positive expectations for treatment success are purportedly one of the processes underlying placebo effects (12;13) as well as other non specific, psychological effects associated with having received treatment and not directly tied to the treatment mechanism itself. (14)
We contend that expectancy effects are not illusory but real with therapeutic significance. A clinician’s communication with a patient can contribute to improved pain and functioning by raising expectations for treatment success and raising positive feelings toward the clinician and treatment.(12;15) While expectancy and affect can be distinguished from one another theoretically,(12) in reality they often go hand in hand, in that communicating an anticipated positive or negative outcome will influence both beliefs and feelings. While the relationship between psychological (e.g., how patients interpret their symptoms) and physiological (e.g., changes in neurobiological processes in the brain) processes is beyond the scope of this paper, a sizeable body of research indicates that patient expectations for treatment success are often associated with health improvements, particularly for subjective health outcomes such as pain and function.(16–18)
In this study, we examine the pathway linking clinician communication→patient perception of the value of treatment→post consultation pain and physical function outcomes within the context of acupuncture treatment for patients suffering from osteoarthritis (OA) of the knee. This investigation extends previous research in three ways.
First, this study goes beyond correlational evidence and models a specific pathway through which communication can contribute to better health. Second, previous research on the therapeutic benefits of clinician-patient communication, particularly in the context of acupuncture treatment, has hypothesized direct effects of communication on outcomes and ignored the possibility of indirect influences. For example, Kaptchuk et al.(19) reported that patients with irritable bowel syndrome had lower symptom severity and higher quality of life three weeks into treatment when their clinicians displayed an ‘augmented’ communication style (i.e., expressing empathy, care, friendliness, active listening, and positive expectations for success) than when using a ‘limited’ style (i.e., intentionally communicating little with the patient). In contrast, our earlier analysis of clinician communication of expectations (see Suarez-Almazor et al.(20)) found that only one of several pain and function outcomes was directly related to clinicians’ communication. Specifically, OA patients in the ‘high expectations’ condition (whose acupuncturists expressed hope and optimism that treatment would reduce pain and improve function) reported better joint-specific pain control compared to patients whose clinicians were assigned to the ‘neutral expectations’ condition (whose acupuncturists expressed uncertainty and a ‘wait and see’ approach about whether treatment would work). Neither the Suarez-Almazor et al. or the Kaptchuk et al. studies explored the possibility of indirect effects of communication that contribute to improved outcomes through a psychological mechanism such as positive affect and higher efficacy expectations.(9)
Finally, in contrast to the above studies, we examine communication effects in relation to a clinician’s individual communication style rather than to the clinician’s assignment to an experimental condition. In other words, clinicians assigned to an experimental condition will have some individual variation in communication.(21;22) For example, two clinicians assigned to the same experimental condition, such as convey optimism, may both communication some degree of optimism, yet one might be perceived as somewhat more optimistic than the other. This investigation tests the effects directly and indirectly associated with an acupuncturist’s actual communication of expectations during the important initial visit where treatment expectations are first discussed.
2. Methods
2.1. Overview of Research Design
The data reported in this study were from a nested two-stage RCT to determine the effects of clinician communication about treatment expectations on patients’ response to traditional acupuncture or sham acupuncture in OA of the knee (for complete methodological details, see Suarez et al. (20)). Patients were first randomized to one of three groups—waiting list, high expectations, or neutral expectations communication style—and then given an appointment with an acupuncturist trained in the assigned communication style (see below). The initial visit between acupuncturists and patients took place before the patient was randomly allocated to traditional acupuncture or sham; thus, the acupuncturist was unaware during the initial visit of what type of treatment the patient would eventually receive. Following the initial consultation, acupuncturists opened a sealed envelope (not in the presence of the patient) which alerted them to whether the patient was assigned to receive traditional or sham acupuncture. Participants were told that the study compared traditional vs. non-traditional acupuncture. Patients received the assigned acupuncture treatment twice weekly over a 5–6 week. All patients included in the current study had a minimum of 10 and no more than 12 acupuncture sessions. At the end of the trial, no statistically or clinically significant differences were observed between those receiving traditional acupuncture and those receiving sham with respect to pain or function outcomes.
2.2 Research participants
2.2.1 Acupuncturists
Six licensed acupuncturists trained in traditional Chinese medicine were recruited through the American College of Acupuncture & Oriental Medicine in Houston, Texas. All were male Chinese and had at least two years of clinical experience.
2.2.2 Patients
Patients who were 50 years old or older, with a physician diagnosis of knee OA were eligible to participate in the trial. Additional inclusion criteria were: (a) moderate to severe pain in the knee in the preceding two weeks, (b) no prior treatment with acupuncture, (c) stable treatment with nonsteroidal anti-inflammatory and analgesics in the previous month, (d) if receiving glucosamine, stable dosage for the past two months, and (e) no knee injections in the previous two months. Patients interested in participating mailed a postcard back to the study coordinators who subsequently called interested patients to complete a screening questionnaire, and if meeting eligibility requirements, were enrolled into the study. The study received IRB approval from the Baylor College of Medicine and the University of Texas MD Anderson Cancer Center.
2.3 Procedure
Upon arriving at the clinic, patients completed baseline measures that included reports of pain and function as well as their outcome expectations for acupuncture treatment (described below). Patients then had a 30 minute initial visit with the acupuncturist who provided information about the procedure, the anticipated outcomes of treatment, and answered questions, all in accordance with his assigned communication style of high vs. neutral expectations for treatment success. While patients had 9–11 additional treatment visits with the acupuncturist, the first visit was characterized by the most conversation, information exchange, and communication of treatment expectations. Subsequent visits consisted primarily of administering treatment. All visits were audio-recorded.
2.4 Communication style intervention
For the first half of the study, acupuncturists were randomized, three trained to communicate high expectations for treatment success and the other three trained to communicate uncertain, neutral expectations. In the second half of the study, the high expectations acupuncturists were retrained to act neutrally and vice-versa. Because one acupuncturist had to leave the study towards the end of the first half of the trial, only 4 acupuncturists participated in the second half.
Acupuncturists in the High Expectations group were trained to convey hope and optimism for treatment using positive statements such as “I expect this will work,” “you should see improvement,” “I have had excellent results with this treatment,” “I’ve had a lot of success with these kinds of symptoms,” and “I’m very optimistic that this will work for you.” A high expectations brochure was also developed and given to patients at their first visit. Acupuncturists randomized to the Neutral Expectations condition were trained to convey uncertainty and neutrality with statements such as “We just really aren’t certain if acupuncture will work for knee pain,” “We have had mixed results with this treatment for this condition,” “Different people have different results,” and “It works for some but not all patients.” A neutral expectations brochure was given to patients. The training consisted of two 2-day training sessions that included didactic instruction, one-on-one coaching, and group role play to practice assigned styles, with video-recording to provide feedback.
2.5 Coding communication of expectations
Five coders, undergraduates working in a communication research lab and blind to the study’s design and goals, independently listened to the audio-recordings of the initial interview and then rated the acupuncturist’s communication of expectations for treatment effectiveness using a 0–10 cm visual analogue scale. One pole of the scale was labeled Neutral Expectations for Treatment Success and the other end High Expectations for Treatment Success. Audio-recordings of the second, mid-point, and final sessions were also rated. Prior to coding, each coder participated in a 2 ½ hour training session on the various ways clinicians communicate expectations and uncertainty for treatment success. Although all sessions were audio-recorded, acupuncturists did not know which sessions would be rated. Each acupuncturist-patient interaction was coded by at least two coders. Consistency among coders’ ratings was acceptable (intraclass correlation = .74). For each interaction, coders’ ratings were averaged to create the communication score for that acupuncturist in that encounter.
2.6 Baseline expectations, perceived treatment value, and outcome measures
To control for baseline expectations about acupuncture as a treatment for arthritis, patients completed a 10 items tapping into their general beliefs about acupuncture effectiveness (e.g., “Acupuncture is an effective treatment for arthritis of the knee,” “Acupuncture can cure arthritis,” “I am not sure acupuncture can improve knee pain”(R), etc). Patients completed this measure before randomization to their initial visit with the acupuncturist. Reliability for this measure was .88.
Patients’ perceptions of the value of treatment were assessed using the Satisfaction with Knee Procedure (SKIP) (20), which has six Likert scale items (with 5-point response scales) for assessing the patient’s perception of treatment to date. Items include: “I would recommend acupuncture to my family if they needed care for the same problem,” “I feel acupuncture is worthwhile for my knee arthritis,” “All things considered, my perceptions of acupuncture are generally negative” (reverse), “I feel I was helped by the acupuncture,” “I am dissatisfied with the functioning of my knees after acupuncture” (reverse), and “Undergoing acupuncture was a waste of time” (reverse). Assessments of patients’ perceived value of treatment were collected at four weeks into treatment. At the 4 week assessment, patients had received 6–8 treatments with up to 4–6 remaining. Cronbach's alpha for this measure was 0.91.
The two primary outcomes for this study were the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) function and pain subscales.(23) These measures were collected at baseline and 6 weeks following the end of treatment. Cronbach’s alphas were .86 and .96 for the pain and function subscales, respectively.
2.7 Statistical analysis
Because there were no significant effects associated with real or sham acupuncture, data from both groups were pooled for analysis. Three sets of analyses were performed. Two multivariable linear regression models were constructed, one each for the pain and function outcome measures. The following variables served as predictors—patient’s demographic characteristics (age, race, education, and gender), baseline pain (or function) score, baseline measure of patient’s belief that acupuncture could help his/her knee problem, ratings of the clinicians’ communication of expectations at the initial visit, and patients’ satisfaction with acupuncture four weeks into treatment. We chose to use communication scores at the initial consultation because the first visit is the one consisting of the most talk between clinician and patient and the one where explanation of treatment and its possible benefits takes place. A third regression analysis was conducted using satisfaction at four weeks into treatment as the outcome and the patient’s demographic characteristics, baseline beliefs that acupuncture could help their knee problem, baseline pain (or function) score, and the clinicians’ communication of expectations as predictors. All regression analyses controlled for effects of patients nested within clinicians by treating individual clinicians as a random variable in the regression models.
Second, two structural equation models used path analytic techniques to investigate direct, indirect, and total effects of each modeled variable on other modeled variables and on the pain and function outcomes.(24) For each path analytic model, its exogenous variables were baseline communication, baseline patient expectation, and baseline pain or function as appropriate for the outcome being tested. Each model’s endogenous variables were satisfaction with acupuncture 4 weeks into treatment and 6 weeks post treatment pain or function. Because the distributions of a number of modeled variables were non-normal in nature, a Spearman rho correlation matrix was considered appropriate for use and was obtained for the analyses. All structural equation modeling of path analyses was conducted with LISREL software, version 8.80 (Scientific Software International, Lincolnwood, Ill).
3. Results
3.1 Overview
A total of 455 participants consented and received either real or sham acupunctures (an additional 72 in the wait list group were not included in this study). Between the initial visit and 6 weeks post treatment survey, an additional 33 patients did not complete treatment and another 111 patients failed to complete measures across all time points leaving a final sample of 311 for the 6-week post treatment assessment of pain and function outcomes. Characteristics of the sample included in the analysis are provided in Table 1. Patient characteristics did not differ between high vs. neutral expectations groups.
Table 1.
Baseline demographic and visit characteristics by expectations condition (N = 311)
| Variable | High Expectations (N = 157) |
Neutral Expectations (N = 154) |
P Value |
|---|---|---|---|
| Mean Age (SD) | 65.2 (9.0) | 64.0 (8.0) | .26 |
| Female (%) | 66 | 62 | .09 |
| Ethnicity: | .18 | ||
| African-American (%) | 15 | 18 | |
| Caucasian (%) | 69 | 71 | |
| Hispanic (%) | 9 | 9 | |
| Other (%) | 7 | 2 | |
| Education: | .22 | ||
| High school or less (%) | 22 | 21 | |
| Some college (%) | 31 | 23 | |
| College/post grad degree (%) | 47 | 56 | |
| Baseline Scores: | |||
| Duration of knee pain—years (SD) | 8.6 (9.7) | 8.7 (9.4) | 0.97 |
| Efficacy expectations—acupuncture range 1–5 (SD) | 3.6 (0.5) | 3.6 (0.6) | 0.98 |
| WOMAC function—range 0–100 (SD) | 44.6 (18.3) | 44.4 (17.4) | .95 |
| WOMAC pain—range 0–100 (SD) | 44.8 (18.4) | 35.9 (18.0) | .59 |
At visit 1, average communication scores in the high and neutral expectations group were 8.2 (sd = 1.8) and 2.8 (sd = 2.2), respectively on a 10 cm visual analogue scale. Over time scores moved toward the middle of the scale for both the high (means = 6.8, 6.2, and 6.4 for the 2nd, mid, and last visit) and neutral (means = 4.9, 5.3, and 5.2 for the 2nd, mid, and last visit) expectations groups. Also, individual acupuncturists were somewhat variable in their communication scores over time. For example, among acupuncturists in the high expectations group, communication style at visit 1 was weakly correlated with communication style at the other visits (correlations ranged from 0.18 to 0.23). Acupuncturists communicating neutral expectations were also variable after visit 1 with correlations between communication scores at the initial visit and at subsequent visits ranging −0.12 to 0.18. Taken collectively, the evidence indicates that acupuncturists communicated expectations strongest in the initial visit and moved to the center of the expectations scale over time, which is not surprising since the initial visit was characterized by the most conversation, and subsequent visits primarily focused on the treatment itself.
Finally, the patient’s pre-visit baseline expectation for acupuncture effectiveness was not correlated with the acupuncturist’s communication style (r = 0.02, ns), confirming that the clinician’s communication style and the patient’s baseline efficacy expectations would produce independent effects in statistical models, since patients’ expectations were measured before the initial encounter.
3.2 Multivariate analysis
Table 2 presents the results of the regression analyses for pain and function outcomes. As hypothesized, patients’ mid treatment satisfaction with acupuncture predicted pain and function outcomes 6 weeks following treatment. In addition, patients who were older and had worse pain and poorer function at baseline reported worse outcomes following treatment. Although the clinician’s communication did not independently predict pain and function outcomes, it did predict, along with baseline expectations for treatment effectiveness, satisfaction with acupuncture 4 weeks into treatment (Table 3). The only other predictor of mid-treatment satisfaction was race, as non-white patients were more positive about acupuncture at 4 than were white patients. Upon further analysis, this finding is attributed to Hispanic patients, with no differences among patients reporting to be of Caucasian, Africa-American, or ‘other’ race.
Table 2.
Predictors of Pain and Function Outcomes 6 weeks Following Treatment
| Paina | Functiona | |||
|---|---|---|---|---|
| Estimate (SE) | P | Estimate (SE) | P | |
| Patient age | 0.31 (0.10) | 0.002 | 0.21 (0.09 | 0.02 |
| Patient education (< HS, HS or some college, college graduate) | −0.28 (1.65) | ≥0.20 | −2.15 (1.50) | 0.15 |
| Patient sex = Female (ref = male) | −1.86 (1.85) | ≥0.20 | −0.66 (1.69) | ≥0.20 |
| Patient race = non-white (ref = white) | −0.52 (1.98) | ≥0.20 | 0.48 (1.77) | ≥0.20 |
| Patient baseline pain | 0.54 (0.05) | < 0.0001 | -- | -- |
| Patient baseline function | -- | -- | 0.55 (0.05) | < 0.0001 |
| Patient baseline expectations about acupuncture | −0.96 (1.99) | ≥0.20 | 1.88 (1.80) | ≥0.20 |
| Clinician communication of expectations at visit 1b | 0.03 (0.27) | ≥0.20 | −0.12 (0.24) | ≥0.20 |
| Patient satisfaction with acupuncture (at 4 weeks) | −6.87 (1.41) | 0.0001 | −7.19 (1.29) | < 0.0001 |
Higher scores on the pain and function measures represent worse outcomes. A negative estimate between a predictor and the outcome would indicate a better outcome with a higher score on the predictor variable.
Higher communication scores represent more optimistic and confident communication
Table 3.
Predictors of Patients’ Satisfaction with Acupuncture 4 weeks into Treatment
| Satisfaction with acupuncture (at 4 weeks) |
||
|---|---|---|
| Estimate (SE) | P | |
| Patient age | 0.003 (0.004) | ≥0.20 |
| Patient education (< HS, HS or some college, college graduate) | −0.03 (0.07) | ≥0.20 |
| Patient sex = Female (ref = male) | 0.04 (0.08) | ≥0.20 |
| Patient race = non-white (ref = white) | 0.16 (0.08) | 0.04 |
| Patient baseline expectations about acupuncture | 0.34 (0.08) | < 0.0001 |
| Clinician communication of expectations at visit 1a | 0.02 (0.01) | 0.04 |
Higher communication scores represent more optimistic and confident communication
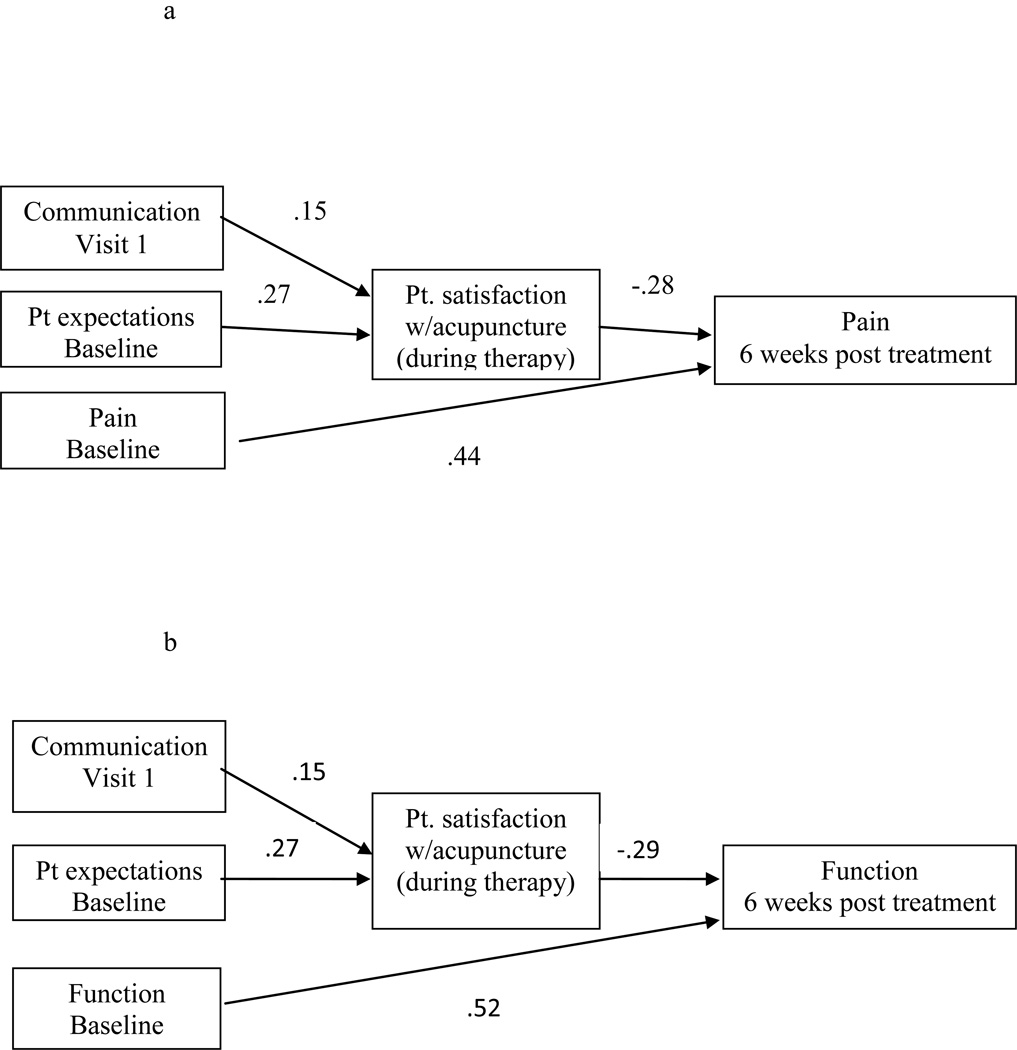
3.3 Path Analyses for the 6-week pain and function outcomes
3.3.1 The pain model
The path model for the outcome pain at 6 weeks post treatment is displayed in Figure 1a. The model exhibited good fit across a number of overall model fit indices: chi square (0.76, df=3, non-significant p=0.86); root mean square error of approximation=0.00; comparative fit index=1.00; and standardized root mean square residual=0.011. All individual path model coefficients were statistically significant (p<0.05); in addition, all modeled indirect and total effects were also statistically significant (p<0.05). The significant total effects of communication and patient expectation on 6-weeks pain (total effect6-week pain, communication=−0.04, p<0.05; total effect6-week pain, patient expectation=−0.07, p<0.05) included significant direct effects on satisfaction at 4 weeks and significant indirect effects on pain at 6 weeks post treatment.
Figure 1.
a: Pathway of Clinician Communication Effects on Pain Outcomes
b: Pathway of Clinician Communication Effects on Function Outcomes
3.3.2 The function model
The path model for function at 6 weeks post treatment is displayed in Figure 1b. This model also exhibited good fit across a number of overall model fit indices: chi square (3.83, df=3, non-significant p=0.28); root mean square error of approximation=0.03; comparative fit index=0.99; and standardized root mean square residual=0.024. As with the pain model, all individual path model coefficients were statistically significant, as were all modeled indirect and total effects. As in the pain model, the significant total effects of communication and patient expectation on 6-week function (total effect6-week function, communication=−0.04, p<0.05; total effect6-week function, patient expectation=−0.08, p<0.05) included significant direct effects (displayed in Figure 1b) on satisfaction at 4 weeks and significant indirect effects on function 6 weeks post treatment.
4. Discussion and conclusion
4.1 Discussion
While rich in tradition, much of previous research on clinician-patient communication and health outcomes has suffered from a serious limitation—the failure to model pathways through which communication can contribute to improved health outcomes and to explicate the mechanism for these effects. While clinician-patient communication could have a direct effect on some health outcomes (e.g., reducing psychological distress with supportive verbal and nonverbal behaviors), more often communication will affect health outcomes through a more indirect or mediated route.(7;9) In this study, we tested one such pathway, enhancing the perceived value of treatment, in the context of acupuncture therapy for osteoarthritis of the knee. The results of this study have several important research and clinical implications.
First, our results demonstrate how communication can contribute to better health outcomes through its effects on proximal and intermediate factors. In this study, the degree to which clinicians communicated optimism and confidence that acupuncture could help the patient did not directly predict pain and function outcomes. However, the clinician’s communication about treatment effectiveness during that initial visit did predict patients’ satisfaction with acupuncture 4 weeks into treatment. This in turn predicted patient reported pain and function outcomes 6 weeks following treatment.
Our findings offer an interesting contrast to those of Kaptchuk et al.(19) who found that ‘augmented’ (i.e., more patient-centered) communication by acupuncturists predicted better quality of life and less symptom distress among patients suffering from irritable bowel syndrome compared to those patients whose clinician used ‘limited’ communication (little conversation, and patients were told clinicians could not talk to them about the study). The Kaptchuk et al. study did not test a psychological mechanism that might link communication to outcome. Yet, it does raise the question of what elements of clinician-patient communication are powerful enough to have significant direct effects on health outcomes. Conversely, the failure to test for indirect or mediated effects may in part explain the null results often reported in previous studies that examine relationships between clinician-patient communication and health outcomes.
Second, our findings also support what many clinicians know to be true—patients’ beliefs in the effectiveness of treatment have therapeutic value, especially for patient-reported outcomes such as pain and function. In our study, while patients’ baseline expectation that acupuncture would effectively treat their OA knee symptoms did not predict outcomes at 6-weeks post treatment, it did predict satisfaction with acupuncture 4 weeks into treatment. In other words, patients more optimistic they would benefit from acupuncture subsequently were happier with treatment results midway through therapy. Because perceptions can change over time, a clinician’s communication about the potential value of treatment can either augment or detract from patients’ initial expectations, which in this study were linked to post treatment outcomes regarding OA patients’ pain and physical function. Our study did not ascertain whether communication affected neurobiological processes that have analgesic effects (13;25) or if it simply influenced how patients interpreted the value of treatment, but these questions should be the subject of future research.
Third, our findings that acupuncturists were unable to consistently maintain levels of either neutral or high expectations across time is likely due to the fact that treatment sessions subsequent to the first visit involved mostly the acupuncture treatment with less conversation about treatment and outcome expectations. Still, this issue of whether clinicians are consistent in their communication about treatment is a topic worthy of future research, especially with respect to its clinical implications. For example, clinicians may be able to maintain the therapeutic benefits of both optimism and honesty by acknowledging an initial course of treatment is not working as effectively as hoped, but alternative treatments are available that might fare better.
Finally, we cannot infer too much from the finding that Hispanic patients reported greater satisfaction during the course of treatment than did patients of other ethnicities because our Hispanic sample was small (n = 28). However, there is some evidence that Hispanic patients (at least women) perceive acupuncture to be more effective treatment than white patients.(26) Certainly, this should be a topic for future research.
4.2 Limitations
While our investigation was an RCT and found indirect effects of communication on outcomes through patients’ beliefs about the value of acupuncture during the course of therapy, the study had several limitations. First, while statistically significant, the effect of clinician communication on patient satisfaction with acupuncture was modest and less powerful than patients’ baseline expectations for treatment effectiveness. Second, we cannot confidently determine the degree to which the communication effects were primarily a function of the clinician’s communication during the initial visit or were the cumulative result of ‘staying on message’ about treatment expectations across multiple visits. However, as noted earlier, communication ratings at the initial visit had weak to moderate correlations with communication ratings at subsequent visits. Finally, while patient reported health states are an important outcome in and of themselves, what remains unanswered is whether the effects observed in this study were associated with psychological processes of interpretation of symptoms or due to neurophysiological changes that may have analgesic properties.
4.3 Conclusions
This study demonstrated that a clinician’s communication about treatment efficacy early in therapy influenced patients’ judgments of acupuncture’s effectiveness over the course of treatment which in turn predicted patient reports of pain and function 6-weeks post treatment. Hopefully, our analysis can serve as one model for future research on clinician-patient communication and health outcomes where potentially influential communication variables are identified and modeled within an explanatory framework hypothesizing their effects on relevant intermediate outcomes (e.g., adherence, raised expectations, self care skills) that in turn more directly affect health outcomes of interest.
4.4 Practice implications
Our research may raise ethical questions about the clinician’s veracity in communicating expected treatment outcomes when the clinical evidence associated with the treatment itself is equivocal. The counterargument, of course, is that being too uncertain and even negative about the value of treatment may contribute to a nocebo effect (as opposed to placebo) which actually hurts outcomes by raising the patient’s anxiety and diminishing hope in the effectiveness of certain therapies for pain and symptom management.(27) We are not suggesting that clinicians mislead patients. Rather, we are suggesting that the clinician’s communication about the potential value of treatment can play a role in how patients experience their treatment, which in turn can influence patient-reported health outcomes.
Acknowledgements
Supported by the National Institute of Arthritis and Musculoskeletal and Skin Disorders (NIAMS R01 AR49999) and Houston Health Services Research and Development Center of Excellence (HFP90-020) at the Michael DeBakey VA Medical Center. Dr. Suarez-Almazor holds a K24 career award from NIAMS, and is the Director of the Houston Center for Education and Research on Therapeutics supported by the Agency for Health Research and Quality (U18HS016093). This trial was registered at clinicaltrials.gov (NCT00059345).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Arora NK. Interacting with cancer patients: the significance of physicians' communication behavior. Soc Sci Med. 2003 Sep;57(5):791–806. doi: 10.1016/s0277-9536(02)00449-5. [DOI] [PubMed] [Google Scholar]
- 2.Griffin SJ, Kinmonth AL, Veltman MW, Gillard S, Grant J, Stewart M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med. 2004 Nov;2(6):595–608. doi: 10.1370/afm.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heisler M, Tierney E, Ackermann RT, Tseng C, Narayan KM, Crosson J, Waitzfelder B, Safford MM, Duru K, Herman WH, Kim C. Physicians' participatory decision-making and quality of diabetes care processes and outcomes: results from the triad study. Chronic Illn. 2009 Sep;5(3):165–176. doi: 10.1177/1742395309339258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ong LM, de Haes JC, Hoos AM, Lammes FB. Doctor-patient communication: a review of the literature. Soc Sci Med. 1995 Apr;40(7):903–918. doi: 10.1016/0277-9536(94)00155-m. [DOI] [PubMed] [Google Scholar]
- 5.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995 May 1;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 6.Rodin G, Mackay JA, Zimmermann C, Mayer C, Howell D, Katz M, Sussman J, Brouwers M. Clinician-patient communication: a systematic review. Support Care Cancer. 2009 Jun;17(6):627–644. doi: 10.1007/s00520-009-0601-y. [DOI] [PubMed] [Google Scholar]
- 7.de Haes H, Bensing J. Endpoints in medical communication research, proposing a framework of functions and outcomes. Patient Educ Couns. 2009 Mar;74(3):287–294. doi: 10.1016/j.pec.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Schouten BC, Meeuwesen L. Cultural differences in medical communication: A review of the literature. Patient Educ Couns. 2006 Dec;64(1–3):21–34. doi: 10.1016/j.pec.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 9.Street RL, Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009 Mar;74(3):295–301. doi: 10.1016/j.pec.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 10.Huang W, Howie J, Taylor A, Robinson N. An investigation into the effectiveness of traditional Chinese acupuncture (TCA) for chronic stress in adults: a randomised controlled pilot study. Complement Ther Clin Pract. 2011 Feb;17(1):16–21. doi: 10.1016/j.ctcp.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 11.Paterson C, Dieppe P. Characteristic and incidental (placebo) effects in complex interventions such as acupuncture. BMJ. 2005 May 21;330(7501):1202–1205. doi: 10.1136/bmj.330.7501.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bensing JM, Verheul W. The silent healer: the role of communication in placebo effects. Patient Educ Couns. 2010 Sep;80(3):293–299. doi: 10.1016/j.pec.2010.05.033. [DOI] [PubMed] [Google Scholar]
- 13.Malani A, Houser D. Expectations mediate objective physiological placebo effects. Adv Health Econ Health Serv Res. 2008;20:311–327. [PubMed] [Google Scholar]
- 14.Verheul W, Sanders A, Bensing J. The effects of physicians' affect-oriented communication style and raising expectations on analogue patients' anxiety, affect and expectancies. Patient Educ Couns. 2010 Sep;80(3):300–306. doi: 10.1016/j.pec.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 15.Hyland ME. Using the placebo response in clinical practice. Clin Med. 2003 Jul;3(4):347–350. doi: 10.7861/clinmedicine.3-4-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mondloch MV, Cole DC, Frank JW. Does how you do depend on how you think you'll do? A systematic review of the evidence for a relation between patients' recovery expectations and health outcomes. CMAJ. 2001 Jul 24;165(2):174–179. [PMC free article] [PubMed] [Google Scholar]
- 17.Staal JB, Rainville J, Fritz J, van MW, Pransky G. Physical exercise interventions to improve disability and return to work in low back pain: current insights and opportunities for improvement. J Occup Rehabil. 2005 Dec;15(4):491–505. doi: 10.1007/s10926-005-8030-3. [DOI] [PubMed] [Google Scholar]
- 18.Graz B, Wietlisbach V, Porchet F, Vader JP. Prognosis or "curabo effect?": physician prediction and patient outcome of surgery for low back pain and sciatica. Spine (Phila Pa 1976) 2005 Jun 15;30(12):1448–1452. doi: 10.1097/01.brs.0000166508.88846.b3. [DOI] [PubMed] [Google Scholar]
- 19.Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE, Kirsch I, Schyner RN, Nam BH, Nguyen LT, Park M, Rivers AL, McManus C, Kokkotou E, Drossman DA, Goldman P, Lembo AJ. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008 May 3;336(7651):999–1003. doi: 10.1136/bmj.39524.439618.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suarez-Almazor ME, Looney C, Liu Y, Cox V, Pietz K, Marcus DM, Street RL., Jr A randomized controlled trial of acupuncture for osteoarthritis of the knee: effects of patient-provider communication. Arthritis Care Res (Hoboken) 2010 Sep;62(9):1229–1236. doi: 10.1002/acr.20225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Del PL, Mazzi M, Saltini A, Zimmermann C. Inter and intra individual variations in physicians' verbal behaviour during primary care consultations. Soc Sci Med. 2002 Nov;55(10):1871–1885. doi: 10.1016/s0277-9536(01)00314-8. [DOI] [PubMed] [Google Scholar]
- 22.Street RL, Jr, Gordon H, Haidet P. Physicians' communication and perceptions of patients: Is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007 Aug;65(3):586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988 Dec;15(12):1833–1840. [PubMed] [Google Scholar]
- 24.Wright S. The method of path coefficients. Ann Math Stat. 1934;5:161–215. [Google Scholar]
- 25.Lanotte M, Lopiano L, Torre E, Bergamasco B, Colloca L, Benedetti F. Expectation enhances autonomic responses to stimulation of the human subthalamic limbic region. Brain Behav Immun. 2005 Nov;19(6):500–509. doi: 10.1016/j.bbi.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Upchurch DM, Burke A, Dye C, Chyu L, Kusunoki Y, Greendale GA. A sociobehavioral model of acupuncture use, patterns, and satisfaction among women in the United States, 2002. Womens Health Issues. 2008 Jan;18(1):62–71. doi: 10.1016/j.whi.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Benedetti F, Lanotte M, Lopiano L, Colloca L. When words are painful: unraveling the mechanisms of the nocebo effect. Neuroscience. 2007 Jun 29;147(2):260–271. doi: 10.1016/j.neuroscience.2007.02.020. [DOI] [PubMed] [Google Scholar]