Abstract
Upregulation of tissue factor (TF) expression leads to increased patient morbidity and mortality in many solid tumor types. The goal of this study was to develop a positron emission tomography (PET) tracer for imaging of TF expression in pancreatic cancer.
Methods
ALT-836, a chimeric anti-human TF monoclonal antibody, was conjugated to 2-S-(4-isothiocyanatobenzyl)-1, 4, 7-triazacyclononane-1, 4, 7-triacetic acid (p-SCN-Bn-NOTA) and labeled with 64Cu. To compare the TF binding affinity of ALT-836 and NOTA-ALT-836, flow cytometry analysis was performed in three pancreatic cancer cell lines with different expression level of TF (from low to high: PANC-1, ASPC-1, and BXPC-3). PET imaging, biodistribution, blocking, and histology studies were performed on pancreatic tumor-bearing mice to evaluate the ability and specificity of 64Cu-NOTA-ALT-836 to target TF in vivo.
Results
There was no difference in TF binding affinity between ALT-836 and NOTA-ALT-836. 64Cu-labeling was achieved with high yield and specific activity. Serial PET imaging revealed that the uptake of 64Cu-NOTA-ALT-836 in BXPC-3 tumors (high TF expression) was 5.7 ± 0.5, 10.3 ± 0.5, and 16.5 ± 2.6 %ID/g at 4, 24, and 48 h post-injection respectively (n = 4), significantly higher than that in the PANC-1 and ASPC-1 tumors. Biodistribution data as measured by gamma counting were consistent with the PET findings. Blocking experiments and histology further confirmed the TF specificity of 64Cu-NOTA-ALT-836.
Conclusion
Herein we report the first successful PET imaging of TF expression. Persistent and TF-specific uptake of 64Cu-NOTA-ALT-836 was observed in pancreatic cancer models.
Keywords: Tissue factor (TF), Pancreatic cancer, Positron emission tomography (PET), Monoclonal antibody, 64Cu, ImmunoPET
Tissue factor (TF), also known as platelet tissue factor, factor III, thrombokinase, or CD142, is a 47 kDa transmembrane glycoprotein receptor present in subendothelial tissue, platelets, and leukocytes (1). The principal function of TF is to localize the coagulation serine protease factor VII/VIIa (FVII/VIIa) to the cell surface, thereby initiating the coagulation cascade. In normal human tissues, TF is only expressed in extravascular cells which comprise the vascular adventitia and organ capsules, forming a haemostatic barrier surrounding the vasculature to prevent blood loss (2). Damages to the endothelial lining of blood vessels can lead to the initiation of TF expression, which ultimately results in activation of the coagulation system (3). The expression of TF is upregulated in several scenarios such as thrombosis, tumor growth, metastasis, and angiogenesis (4, 5). Clinically, the pathologic consequences of unregulated activation of the coagulation system is a major cause of increased morbidity and mortality in cancer patients (6).
With about 44,030 estimated new cases and 37,660 estimated deaths in 2011 in the United States, pancreatic cancer is among the most incurable malignant diseases with a dismal 5-year survival rate of ∼5% (7). The majority of pancreatic adenocarcinoma has been found to be associated with several haemostatic complications such as venous and arterial thrombosis, migratory thrombophlebitis, pulmonary embolism, disseminated intravascular coagulation, and simultaneously aggressive tumor angiogenesis and metastasis (8, 9). It is now generally recognized that a strong correlation exists between the aberrant expression of TF and pancreatic cancer (10, 11), as well as many other solid tumor types such as breast cancer (4), glioma (12), leukemia (13), and lung cancer (14). This correlation signifies the potential for not only inhibiting tumor angiogenesis/metastasis and the associated thrombosis through modulation of TF signalling, but also using TF as a prognostic marker (15).
ALT-836 (formerly known as Sunol-cH36) is a chimeric anti-human TF monoclonal antibody that binds to the factor X (FX)-binding site in TF with nanomolar affinity, which can block the activation of FX and inhibit the coagulation cascade (16). Recently, ALT-836 has been evaluated in a phase 1 clinical trial in acute lung injury/acute respiratory distress syndrome (ALI/ARDS) (17). Based on the encouraging phase I results, a phase II clinical trial is currently ongoing. In addition, ALT-836 is in a phase I clinical trial for locally advanced or metastatic solid tumors.
Positron emission tomography (PET) imaging has been widely used in clinical oncology for tumor staging and for monitoring therapeutic efficacy (18-21). Although anti-TF antibodies have been used for imaging of thrombus formation and atherosclerotic plaques in animal models (22, 23), no PET imaging of TF has been reported to date. The goal of this proof-of-principle study was to investigate whether ALT-836 can be used for PET imaging of TF in preclinical pancreatic cancer models, using 64Cu as the radiolabel, which can open up new avenues for future patient selection/stratification in TF-related clinical trials, as well as monitoring the therapeutic response. To validate the PET findings, various in vitro/in vivo/ex vivo studies were carried out to confirm TF specificity of 64Cu-labeled ALT-836.
Materials and Methods
Chemicals
ALT-836 was provided by Altor Bioscience Corporation (Miramar, FL). AlexaFluor488- and Cy3-labeled secondary antibodies were purchased from Jackson Immunoresearch Laboratories, Inc. (West Grove, CA). S-2-(4-isothiocyanatobenzyl)-1, 4, 7-triazacyclononane-1, 4, 7-triacetic acid (p-SCN-Bn-NOTA) and Chelex 100 resin (50-100 mesh) were purchased from Macrocyclics, Inc. (Dallas, TX) and Sigma-Aldrich (St. Louis, MO), respectively. 64Cu was produced using the 64Ni(p,n)64Cu reaction with a cyclotron. Water and all buffers were of Millipore grade and pre-treated with Chelex 100 resin to ensure that the aqueous solution was heavy metal-free. All other reaction buffers and chemicals were from Thermo Fisher Scientific (Fair Lawn, NJ).
Cell Lines and Animal Models
BXPC-3, ASPC-1, and PANC-1 pancreatic cancer cell lines were purchased from the American Type Culture Collection (ATCC, Manassas, VA) and cultured according to the supplier's instructions. Cells were used for in vitro and in vivo experiments when they reached ∼75% confluence. All animal studies were conducted under a protocol approved by the University of Wisconsin Institutional Animal Care and Use Committee. Four- to five-week-old female athymic nude mice were purchased from Harlan (Indianapolis, IN) and tumors were established by subcutaneously injecting 5 × 106 cells, suspended in 100 μL of 1:1 mixture of culture medium and Matrigel (BD Biosciences, Franklin lakes, NJ), into the front flank of mice. Mice were used for in vivo experiments when the diameter of tumors reached 5-8 mm (4∼6 weeks after inoculation).
Antibody Conjugation and Radiolabeling
NOTA-ALT-836 was prepared similar as previously described (24), with the reaction ratio of p-SCN-Bn-NOTA:ALT-836 being 25:1. 64Cu-labeling and purification was also performed similar as previously described (24), with 37 MBq of 64Cu per 25 μg of NOTA-ALT-836.
Flow Cytometry
The TF binding activities of ALT-836 and NOTA-ALT-836 to BXPC-3/ASPC-1/PANC-1 cells was evaluated by flow cytometry. Briefly, cells were harvested and suspended in cold phosphate-buffered saline (PBS) with 2% bovine serum albumin at a concentration of 5 × 106 cells/mL. The cells were incubated with ALT-836 or NOTA-ALT-836 (1 or 5 μg/mL) for 30 min at room temperature (RT), washed three times with cold PBS, and centrifuged at 1,000 rpm for 5 min. The cells were then incubated with AlexaFluor488-labeled goat anti-human IgG for 30 min at RT. Afterwards, the cells were washed and analyzed using a BD FACSCalibur 4-color analysis cytometer (Becton-Dickinson, San Jose, CA) with FlowJo analysis software (Tree Star, Inc., Ashland, OR).
PET/CT Imaging and Biodistribution Studies
PET and CT scans, image reconstruction, and region-of-interest (ROI) analysis of the PET data were performed using an Inveon microPET/microCT rodent model scanner (Siemens Medical Solutions USA, Inc.) as described earlier (24, 25). Each tumor-bearing mouse was injected with 5-10 MBq of 64Cu-NOTA-ALT-836 via tail vein and 5-10 minute static PET scans were performed at various time points post-injection (p.i.). Tracer uptake was presented as percentage injected dose per gram of tissue (%ID/g) (mean ± SD; 4 mice per group). Another group of four BXPC-3 tumor-bearing mice was each injected with 1 mg of unlabeled ALT-836 at 2 h before 64Cu-NOTA-ALT-836 administration to evaluate the TF specificity of the tracer in vivo (i.e. blocking experiment). Biodistribution studies were carried out after the last PET scans at 48 h p.i. to validate the PET data. The BXPC-3/ASPC-1/PANC-1 tumors, liver, spleen (i.e. tissues with significant uptake of 64Cu-NOTA-ALT-836), and muscle were also frozen and cryo-sectioned for histological analysis.
Histology
Frozen tissue slices of 5 μm thickness were fixed with cold acetone for 10 min and dried in the air for 30 min. After rinsing with PBS and blocking with 10% donkey serum for 30 min at RT, the slices were incubated with ALT-836 (2 μg/mL) for 1 h at 4 °C and visualized using AlexaFluor488-labeled goat anti-human IgG. The tissue slices were also stained for endothelial marker CD31 as described previously (26, 27). After washing with PBS, the slices were incubated with rat anti-mouse CD31 antibody (2 μg/mL) for 1 h, followed by Cy3-labeled donkey anti-rat IgG for 30 min. All images were acquired with a Nikon Eclipse Ti microscope.
Statistical analysis
Quantitative data were expressed as mean ± SD. Means were compared using Student's t-test. P values < 0.05 were considered statistically significant.
Results
Characterization of NOTA-ALT-836
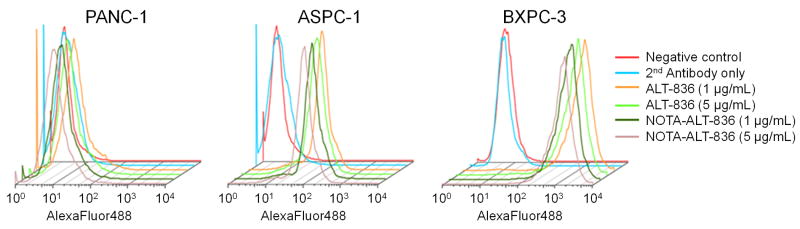
Based on flow cytometry analysis of both BXPC-3 and ASPC-1 cells (high and medium TF expression, respectively (15)), there were no observable differences between ALT-836 and NOTA-ALT-836 at 1 μg/mL or 5 μg/mL (Figure 1). For PANC-1 cells which are TF-negative (15), neither ALT-836 nor NOTA-ALT-836 bound to the cells at these concentrations. Together, these results indicated that NOTA conjugation did not alter the antigen binding affinity or specificity of ALT-836, with little non-specific binding in cell culture. Furthermore, the binding level of ALT-836 and NOTA-ALT-836 to the three cell lines is in accordance with TF expression level in these cells (BXPC-3 > ASPC-1 > PANC-1).
Figure 1.
Flow cytometry analysis of various concentrations of ALT-836 and NOTA-ALT-836 in three pancreatic cancer cell lines: PANC-1 (TF-negative), ASPC-1 (medium TF expression), and BXPC-3 (high TF expression).
Radiochemistry
64Cu-labeling, including final purification using PD-10 columns, took 70 ± 10 min (n = 6). The decay-corrected radiochemical yield was 79.6 ± 5.4 %, based on 25 μg of NOTA-ALT-836 per 37 MBq of 64Cu, with radiochemical purity of > 95%. The ratio of 64Cu activity to antibody mass was 1.2 GBq/mg (4.86 Ci/μmol), assuming complete antibody recovery after size exclusion chromatography.
PET Imaging
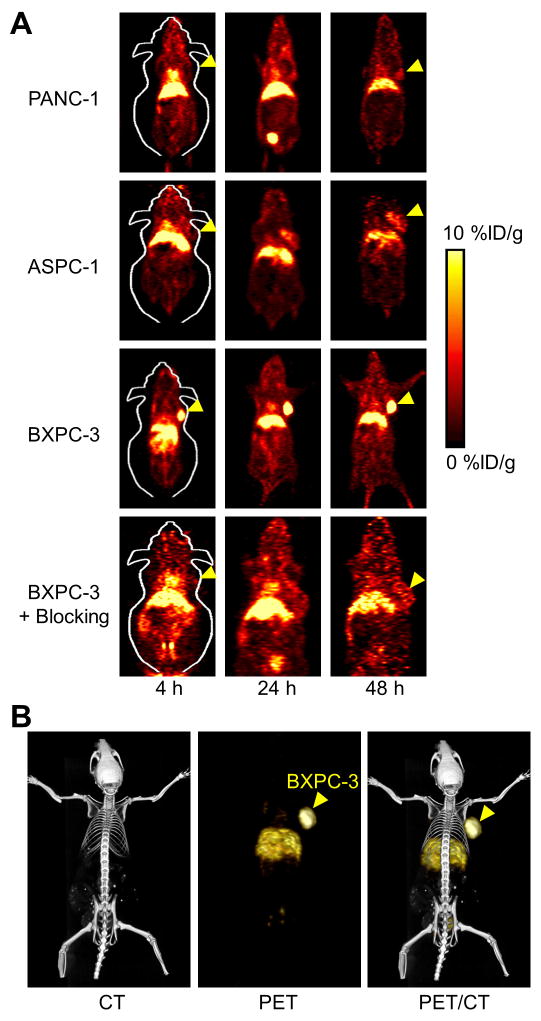
Based on the half-life of 64Cu (12.7 h), the time points of 4, 24, and 48 h p.i. were chosen for serial PET scans after intravenous injection of 64Cu-NOTA-ALT-836 into tumor-bearing mice. The coronal slices that contained the BXPC-3/ASPC-1/PANC-1 tumors are shown in Figure 2A and representative PET/CT fused images of a BXPC-3 tumor-bearing mouse at 24 h p.i. are shown in Figure 2B. The quantitative data obtained from ROI analysis are shown in Figure 3.
Figure 2.
Small animal PET imaging of tissue factor in pancreatic tumor-bearing mice. A. Serial coronal PET images at 4, 24, and 48 h post-injection of 64Cu-NOTA-ALT-836 (all three tumor models) or 1 mg of ALT-836 before 64Cu-NOTA-ALT-836 (i.e. blocking, BXPC-3 only). Tumors are indicated by arrowheads. B. Representative PET/CT images of 64Cu-NOTA-ALT-836 in BXPC-3 tumor-bearing mice at 24 h post-injection.
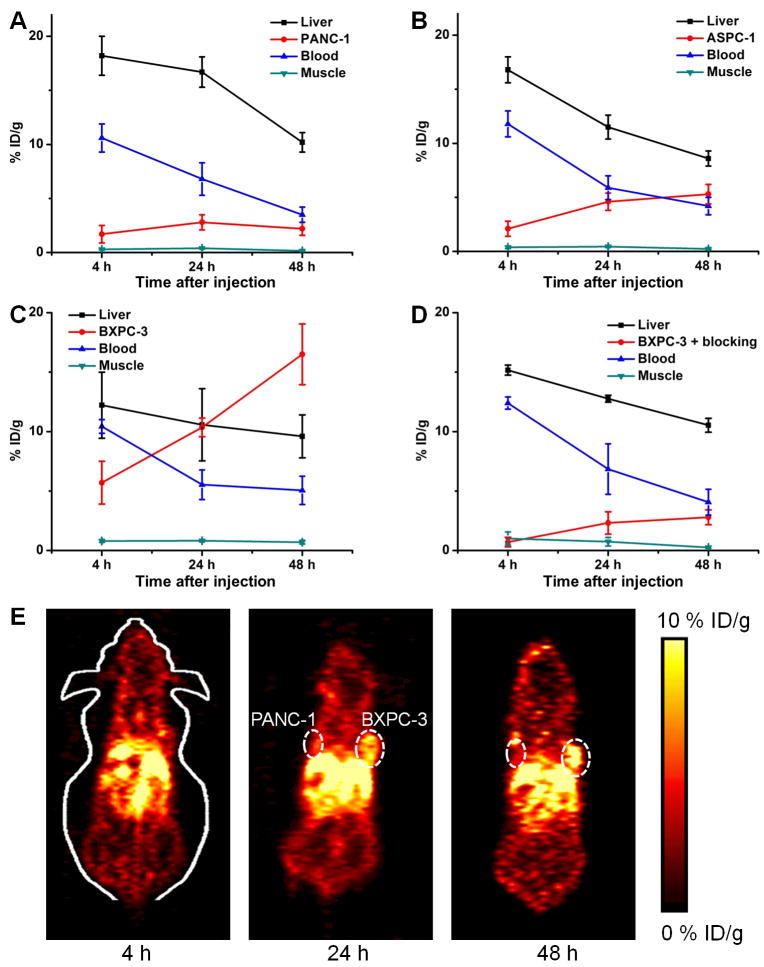
Figure 3.
Quantitative analysis of the PET data. A. Time-activity curves of the PANC-1 tumor, liver, blood, and muscle after intravenous injection of 64Cu-NOTA-ALT-836 (n = 4). B. Time-activity curves of the ASPC-1 tumor, liver, blood, and muscle after intravenous injection of 64Cu-NOTA-ALT-836 (n = 4). C. Time-activity curves of the BXPC-3 tumor, liver, blood, and muscle after intravenous injection of 64Cu-NOTA-ALT-836 (n = 4). D. Time-activity curves of the BXPC-3 tumor, liver, blood, and muscle after intravenous injection of 64Cu-NOTA-ALT-836 with a pre-injected blocking dose of ALT-836 (n = 4). E. Representative serial coronal PET images at 4, 24, and 48 h post-injection of 64Cu-NOTA-ALT-836 in mice bearing both PANC-1 and BXPC-3 tumors.
Liver uptake and blood pool activity of 64Cu-NOTA-ALT-836 were prominent at early time points, which gradually declined over time, similar to other radiolabeled antibodies reported in the literature. In the PANC-1 tumor which does not express detectable level of TF, the uptake of 64Cu-NOTA-ALT-836 was very low (1.7 ± 0.8, 2.8 ± 0.7, and 2.2 ± 0.6 %ID/g at 4, 24, and 48 h p.i. respectively; n = 4; Figure 2A, 3A). The liver uptake (18.2 ± 1.8, 16.7 ± 1.4, and 10.2 ± 0.9 %ID/g at 4, 24, and 48 h p.i. respectively) and blood radioactivity (10.6 ± 1.3, 6.8 ± 1.5, and 3.5 ± 0.7 %ID/g at 4, 24, and 48 h p.i. respectively; n = 4; Figure 2A, 3A) were similar to those in the other two tumor models. Uptake of 64Cu-NOTA-ALT-836 in the ASPC-1 tumors (medium TF expression) was higher than that in the PANC-1 tumors, at 2.1 ± 0.7, 4.6 ± 0.8, and 5.3 ± 0.9 %ID/g at 4, 24, and 48 h p.i. respectively (n = 4; Figure 2A, 3B). In BXPC-3 tumor-bearing mice, tumor uptake of 64Cu-NOTA-ALT-836 was clearly visible as early as 4 h p.i. and increased over time (5.8 ± 1.8, 10.4 ± 0.8, and 16.5 ± 2.6 %ID/g at 4, 24, and 48 h p.i. respectively; n = 4; Figure 2A, 3C). These values were significantly higher than those of the PANC-1 and ASPC-1 tumors at all time points (P < 0.05), indicating TF specificity of the tracer.
Administration of a blocking dose of ALT-836 at 2 h before 64Cu-NOTA-ALT-836 injection reduced the tumor uptake to 0.7 ± 0.4, 2.3 ± 0.9, and 2.8 ± 0.7 %ID/g at 4, 24, and 48 h p.i. respectively (n = 4; Figure 2A, 3D), which was significantly different from that of mice injected with 64Cu-NOTA-ALT-836 alone (P < 0.05 at all three time points). Slightly higher radioactivity in the blood was observed at early time points (12.4 ± 0.5 and 6.9 ± 2.1 %ID/g at 4 and 24 h p.i. respectively; n = 4; Figure 3D) in the blocking group, whereas liver uptake of 64Cu-NOTA-ALT-836 (15.6 ± 0.4, 12.8 ± 0.3, and 10.5 ± 0.6 %ID/g at 4, 24, and 48 h p.i. respectively; n = 4; Figure 3D) was comparable to that of mice injected with 64Cu-NOTA-ALT-836 alone. Overall, tracer uptake in all major organs was similar between the two groups yet the BXPC-3 tumor uptake was significantly higher in the 64Cu-NOTA-ALT-836 dosed mice than in the blocking group, which confirmed TF specificity of the tracer in vivo.
An additional group of three mice were each injected with PANC-1 cells on the left flank and BXPC-3 cells on the right flank and subjected to serial 64Cu-NOTA-ALT-836 PET scans. Since BXPC-3 tumors grow faster than PANC-1, the tumor diameters at the time of PET scans were ∼7 mm for BXPC-3 and ∼4 mm for PANC-1, respectively. Significant uptake of 64Cu-NOTA-ALT-836 in the BXPC-3 tumors could be observed at 24 h p.i. while tracer uptake in the PANC-1 tumors was at the background level (Figure 3E). Non-invasive detection of TF-positive tumors but not TF-negative tumors in the same mice further validated that 64Cu-NOTA-ALT-836 can specifically target TF in vivo.
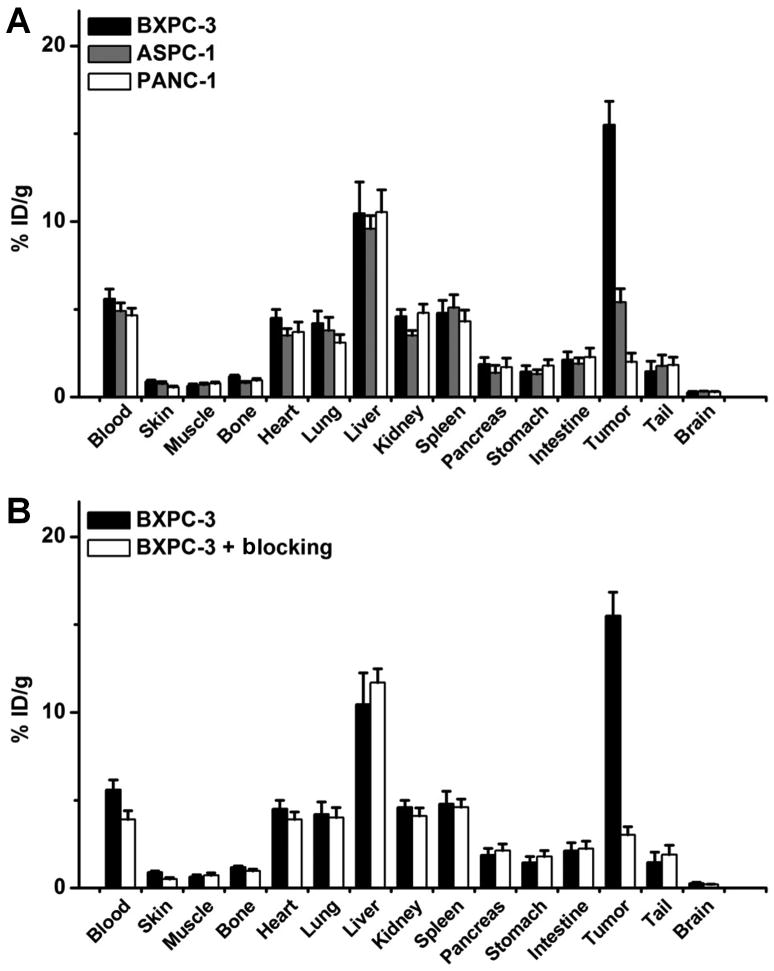
Biodistribution Studies
All mice were euthanized after the terminal PET scans at 48 h p.i. for biodistribution and histology studies to validate the in vivo PET data. Besides the tumors, blood, liver, and spleen also had significant radioactivity accumulation at 48 h p.i., as expected for a radiolabeled antibody which typically has long circulation half-life and hepatic clearance (Figure 4A). Appreciable kidney uptake (∼5 %ID/g) was also observed, likely due to a small fraction of 64Cu detaching from NOTA-ALT-836 and degradation of the tracer over time (lower molecular weight species can undergo renal clearance). 64Cu-NOTA-ALT-836 showed similar biodistribution profile in BXPC-3/ASPC-1/PANC-1 tumor-bearing mice in all the major organs/tissues except the tumor. When compared with all major organs in mice, BXPC-3 tumor uptake of 64Cu-NOTA-ALT-836 was the highest, which provided excellent tumor contrast with a tumor/muscle ratio of 24.2 ± 2.1 at 48 h p.i. (n = 4).
Figure 4.
Biodistribution studies in pancreatic tumor-bearing mice. A. Biodistribution of 64Cu-NOTA-ALT-836 at 48 h post-injection in three pancreatic cancer models (n = 4). Tracer uptake in the BXPC-3 tumor was significantly higher than those in PANC-1 and ASPC-1 tumors. B. Biodistribution of 64Cu-NOTA-ALT-836 at 48 h post-injection in the BXPC-3 tumor model, with and without a blocking dose of ALT-836 (n = 4). Tumor uptake was significantly different between the two groups.
Pre-injection of a blocking dose of ALT-836 led to a significant decrease in BXPC-3 tumor uptake (P < 0.01; n = 4; Figure 4B) but not other normal tissues including the blood and liver, corroborating the PET findings. Overall, consistent quantitative data from ex vivo biodistribution studies and in vivo PET scans demonstrated that ROI analysis of non-invasive PET scans accurately reflected tracer distribution in vivo, as well as TF specificity of 64Cu-NOTA-ALT-836.
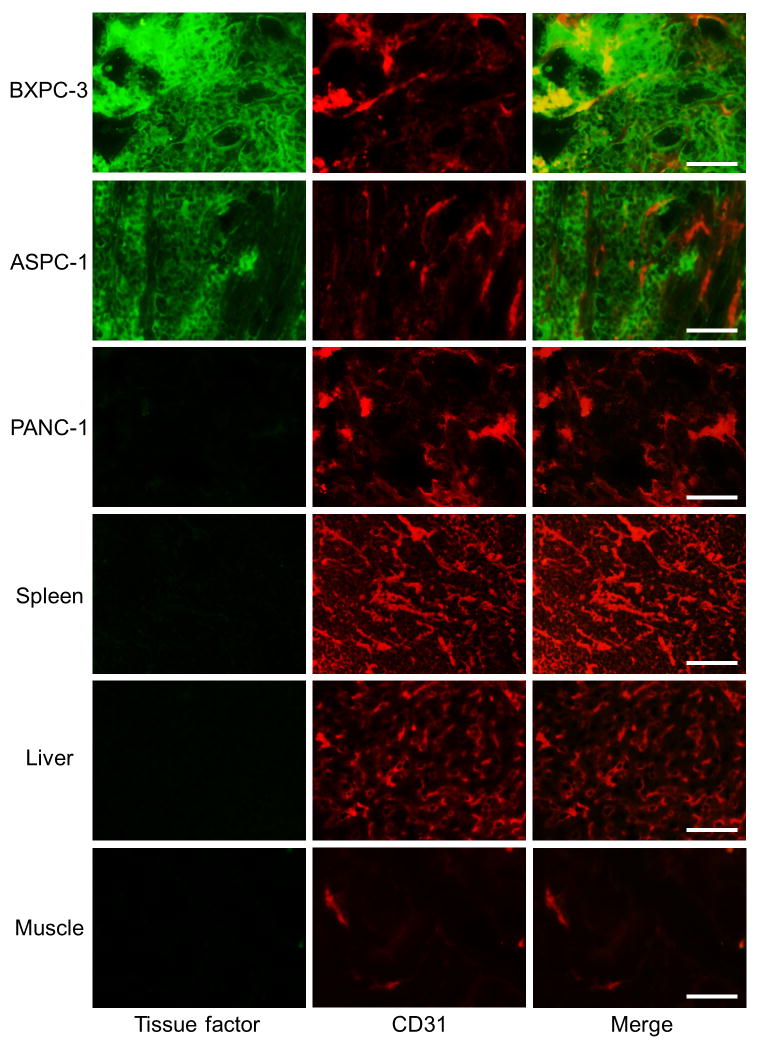
Histology
Immunofluorescence TF/CD31 staining revealed that TF expression was prominent on the BXPC-3/ASPC-1 tumor cells, but absent on the PANC-1 cells (Figure 5). TF staining of mouse liver/spleen/muscle all gave very low signal, since not only do these tissues not express TF at a high level, but also the binding affinity of ALT-836 to murine TF is low. Therefore, uptake of 64Cu-NOTA-ALT-836 in mouse liver/spleen was largely unrelated to TF binding and more likely related to non-specific capture by the reticuloendothelial system and hepatic clearance of the tracer.
Figure 5.
Immunofluorescence tissue factor/CD31 double-staining of the three pancreatic tumor tissues, spleen, liver, and muscle. ALT-836 and AlexaFluor488-labeled goat anti-human IgG were used for tissue factor staining (green). Afterwards, the tissue slices were stained with rat anti-mouse CD31 antibody and Cy3-labeled donkey anti-rat IgG (red). All images were acquired under the same condition and displayed at the same scale. Magnification: 200×. Scale bar: 50 μm.
Discussion
TF is over-expressed in most cancer types (28, 29). Mounting literature data have suggested a key role for TF in the development of cancer-associated thrombosis and tumor growth, angiogenesis, and metastasis. As a direct antagonist of TF, ALT-836 can be used to block TF signaling in cancer, thereby inhibiting cancer-associated venous thromboembolism and tumor development/metastasis. In pre-clinical studies including non-human primates, ALT-836 exhibited potent anti-thrombotic and anti-inflammatory activities with good safety profile (16). In patients with coronary artery disease (CAD) and ALI/ARDS, single dose administration of ALT-836 was found to be safe and exhibited anti-coagulant and anti-inflammatory effects (17). A phase II study using a multi-dose regimen of ALT-836 is being conducted in patients with ALI/ARDS.
With these encouraging results, a phase I, open-label, multi-center, dose-escalation study of ALT-836 in combination with gemcitabine for locally advanced or metastatic solid tumors is currently ongoing, with the primary outcome measures being maximum tolerated dose (MTD) of ALT-836 in combination with gemcitabine, safety profile, number and severity of treatment related adverse effects, clinical benefit, progression free survival, etc. (ClinicalTrials.gov Identifier: NCT01325558). The development of a PET tracer based on ALT-836, which does not affect its binding affinity and specificity to TF, can play multiple roles in future clinical trials of ALT-836 such as patient selection, which can significantly improve the response rate in cancer patients. In addition, radiolabeled ALT-836 can also be used to more effectively study the pharmacokinetics of this antibody, as well as monitoring the therapeutic effect of drugs that act through modulation of TF signaling.
Pancreatic cancer is the fourth leading cause of cancer death in the United States (30). With a 5-year survival rate of ∼5% and a median survival of less than 6 months, the diagnosis of pancreatic cancer carries one of the most dismal prognoses. Due to the lack of specific symptoms and limitations in diagnostic methods, pancreatic cancer is nearly undetectable during its formative stages. Many pancreatic cancer cells are naturally resistant to current chemotherapy and radiation therapy and to date, most known pancreatic cancer antigens generated relatively weak immune response (30, 31). Early detection methods are under development but do not yet exist for pancreatic cancer. The correlation between TF and pancreatic cancer development and metastasis makes TF a useful marker for diagnosis (10), and the development of a PET tracer for TF imaging is of critical importance.
To the best of our knowledge, imaging of TF in cancer has not been reported to date. Over the last decade, a myriad of preclinical and clinical data suggested a promising future for immunoPET in the management of cancer patients (32). In this study, we have successfully developed and characterized 64Cu-labeled ALT-836 for PET imaging of tumor TF expression in vivo. Our data showed that 64Cu-NOTA-ALT-836 specifically bound to TF-positive BXPC-3 tumors but not to TF-negative PANC-1 tumors, and the tumor uptake of 64Cu-NOTA-ALT-836 was closely associated with TF expression level in the tumor. Even within the same mouse, 64Cu-NOTA-ALT-836 can delineate and differentiate tumors with different TF expression (BXPC-3 vs. PANC-1, Figure 3E). Such TF specificity in vivo makes 64Cu-NOTA-ALT-836 a PET tracer with broad potential applications in many clinical situations, not only in cancer but also in many other diseases (e.g. ALI/ARDS) where TF plays a key role.
The pancreas is of close proximity to the liver, thus tracer uptake may be masked by appreciable signal in the liver. Usually, pancreatic cancer is diagnosed with metastases (33), therefore we envision that 64Cu-NOTA-ALT-836 may be more useful in the metastatic setting rather than for initial primary tumor detection. Guiding surgery with molecularly targeted fluorescent agents has attracted enormous interest over the last decade (34). Future development of fluorescently labeled ALT-836, which emits in the near-infrared range (700-900 nm (24, 35)) hence has good signal penetration with low autofluorescence background, may be useful for surgical guidance of tumor removal.
The advantages of antibody-based tracers are that they are very antigen specific and have high binding affinity and absolute tumor uptake, which makes them suitable for internal radiotherapy applications and/or targeted delivery of anti-cancer drugs. To provide more insight about the long-term behavior of ALT-836 in vivo, other longer lived isotopes (e.g., 89Zr which has a decay half-life of 3.3 days (25)) can be explored in future studies. The major limitations of antibody-based imaging are slow tumor accumulation and high background signal in the reticuloendothelial system, which may be overcome by peptide, small molecule, or antibody fragment-based tracers (36, 37). For pancreatic cancer, since the primary metastasis site is also liver, development of TF-targeting PET probes with low liver uptake can be advantageous.
One of the key requirements for accurate PET imaging with 64Cu-labeled antibodies is that the tracer should be sufficiently stable during the imaging period, since the PET scanner detects the distribution of 64Cu rather than the antibody itself. It is now generally agreed that NOTA is one of the best chelators for 64Cu-labeling. A recent elegant study compared the effect of several bifunctional chelators on the biodistribution of a 64Cu-labeled antibody (38), which concluded that thermodynamic stability of 64Cu-chelator complexes did not significantly influence tumor uptake of the tracer but dramatically affected the normal tissue distribution. Consistent with this report, our own studies also showed that 64Cu-NOTA and 64Cu-DOTA (DOTA denotes 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid) based PET tracers behaved similarly in terms of tumor uptake yet the use of NOTA as the chelator resulted in significantly lower liver uptake (39, 40).
Conclusion
Herein we report the development, characterization, and in vivo investigation of a 64Cu-labeled antibody for PET imaging of TF expression in pancreatic cancer. Rapid, persistent, and TF-specific uptake of 64Cu-NOTA-ALT-836 in the BXPC-3 tumor was observed, which was further validated by various in vitro, in vivo, and ex vivo experiments. Furthermore, tumor uptake of 64Cu-NOTA-ALT-836 in various pancreatic tumors was related to their TF expression level. Upon further optimization and development, such TF-targeted PET tracers can be translated into the clinic for improving pancreatic cancer patient management. Lastly, these tracers can also play multiple roles in not only many other solid tumors types but also many other diseases where TF signaling is upregulated.
Acknowledgments
This work was supported, in part, by the University of Wisconsin Carbone Cancer Center, the Department of Defense (W81XWH-11-1-0644), the National Center for Advancing Translational Sciences (NCATS) grant 9U54TR000021, and the Elsa U. Pardee Foundation.
References
- 1.Drake TA, Morrissey JH, Edgington TS. Selective cellular expression of tissue factor in human tissues. Implications for disorders of hemostasis and thrombosis. Am J Pathol. 1989;134:1087–1097. [PMC free article] [PubMed] [Google Scholar]
- 2.Nemerson Y. Tissue factor and hemostasis. Blood. 1988;71:1–8. [PubMed] [Google Scholar]
- 3.Hobbs JE, Zakarija A, Cundiff DL, et al. Alternatively spliced human tissue factor promotes tumor growth and angiogenesis in a pancreatic cancer tumor model. Thromb Res. 2007;120(2):S13–21. doi: 10.1016/S0049-3848(07)70126-3. [DOI] [PubMed] [Google Scholar]
- 4.Contrino J, Hair G, Kreutzer DL, Rickles FR. In situ detection of tissue factor in vascular endothelial cells: correlation with the malignant phenotype of human breast disease. Nat Med. 1996;2:209–215. doi: 10.1038/nm0296-209. [DOI] [PubMed] [Google Scholar]
- 5.Rickles FR, Falanga A. Molecular basis for the relationship between thrombosis and cancer. Thromb Res. 2001;102:V215–224. doi: 10.1016/s0049-3848(01)00285-7. [DOI] [PubMed] [Google Scholar]
- 6.Rickles FR, Levine MN. Epidemiology of thrombosis in cancer. Acta Haematol. 2001;106:6–12. doi: 10.1159/000046583. [DOI] [PubMed] [Google Scholar]
- 7.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: The impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 8.Khorana AA, Fine RL. Pancreatic cancer and thromboembolic disease. Lancet Oncol. 2004;5:655–663. doi: 10.1016/S1470-2045(04)01606-7. [DOI] [PubMed] [Google Scholar]
- 9.Hidalgo M. Pancreatic cancer. N Engl J Med. 2010;362:1605–1617. doi: 10.1056/NEJMra0901557. [DOI] [PubMed] [Google Scholar]
- 10.Haas SL, Jesnowski R, Steiner M, et al. Expression of tissue factor in pancreatic adenocarcinoma is associated with activation of coagulation. World J Gastroenterol. 2006;12:4843–4849. doi: 10.3748/wjg.v12.i30.4843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van den Berg YW, Osanto S, Reitsma PH, Versteeg HH. The relationship between tissue factor and cancer progression: insights from bench and bedside. Blood. 2012;119:924–932. doi: 10.1182/blood-2011-06-317685. [DOI] [PubMed] [Google Scholar]
- 12.Guan M, Jin J, Su B, Liu WW, Lu Y. Tissue factor expression and angiogenesis in human glioma. Clin Biochem. 2002;35:321–325. doi: 10.1016/s0009-9120(02)00312-0. [DOI] [PubMed] [Google Scholar]
- 13.Hair GA, Padula S, Zeff R, et al. Tissue factor expression in human leukemic cells. Leuk Res. 1996;20:1–11. doi: 10.1016/0145-2126(95)00107-7. [DOI] [PubMed] [Google Scholar]
- 14.Koomagi R, Volm M. Tissue-factor expression in human non-small-cell lung carcinoma measured by immunohistochemistry: correlation between tissue factor and angiogenesis. Int J Cancer. 1998;79:19–22. doi: 10.1002/(sici)1097-0215(19980220)79:1<19::aid-ijc4>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 15.Nitori N, Ino Y, Nakanishi Y, et al. Prognostic significance of tissue factor in pancreatic ductal adenocarcinoma. Clin Cancer Res. 2005;11:2531–2539. doi: 10.1158/1078-0432.CCR-04-0866. [DOI] [PubMed] [Google Scholar]
- 16.Jiao JA, Kelly AB, Marzec UM, et al. Inhibition of acute vascular thrombosis in chimpanzees by an anti-human tissue factor antibody targeting the factor X binding site. Thromb Haemost. 2010;103:224–233. doi: 10.1160/TH09-06-0400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morris PE, Steingrub JS, Huang BY, et al. A phase I study evaluating the pharmacokinetics, safety and tolerability of an antibody-based tissue factor antagonist in subjects with acute lung injury or acute respiratory distress syndrome. BMC Pulm Med. 2012;12:5. doi: 10.1186/1471-2466-12-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gambhir SS, Czernin J, Schwimmer J, Silverman DH, Coleman RE, Phelps ME. A tabulated summary of the FDG PET literature. J Nucl Med. 2001;42:1S–93S. [PubMed] [Google Scholar]
- 19.Alauddin MM. Positron emission tomography (PET) imaging with 18F-based radiotracers. Am J Nucl Med Mol Imaging. 2012;2:55–76. [PMC free article] [PubMed] [Google Scholar]
- 20.Vach W, Høilund-Carlsen PF, Fischer BM, Gerke O, Weber W. How to study optimal timing of PET/CT for monitoring of cancer treatment. Am J Nucl Med Mol Imaging. 2011;1:54–62. [PMC free article] [PubMed] [Google Scholar]
- 21.Grassi I, Nanni C, Allegri V, et al. The clinical use of PET with 11C-acetate. Am J Nucl Med Mol Imaging. 2012;2:33–47. [PMC free article] [PubMed] [Google Scholar]
- 22.Falati S, Gross P, Merrill-Skoloff G, Furie BC, Furie B. Real-time in vivo imaging of platelets, tissue factor and fibrin during arterial thrombus formation in the mouse. Nat Med. 2002;8:1175–1181. doi: 10.1038/nm782. [DOI] [PubMed] [Google Scholar]
- 23.Temma T, Ogawa Y, Kuge Y, et al. Tissue factor detection for selectively discriminating unstable plaques in an atherosclerotic rabbit model. J Nucl Med. 2010;51:1979–1986. doi: 10.2967/jnumed.110.081216. [DOI] [PubMed] [Google Scholar]
- 24.Zhang Y, Hong H, Engle JW, Yang Y, Barnhart TE, Cai W. Positron emission tomography and near-infrared fluorescence imaging of vascular endothelial growth factor with dual-labeled bevacizumab. Am J Nucl Med Mol Imaging. 2012;2:1–13. [PMC free article] [PubMed] [Google Scholar]
- 25.Hong H, Severin GW, Yang Y, et al. Positron emission tomography imaging of CD105 expression with 89Zr-Df-TRC105. Eur J Nucl Med Mol Imaging. 2012;39:138–148. doi: 10.1007/s00259-011-1930-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cai W, Chen K, Mohamedali KA, et al. PET of vascular endothelial growth factor receptor expression. J Nucl Med. 2006;47:2048–2056. [PubMed] [Google Scholar]
- 27.Cai W, Wu Y, Chen K, Cao Q, Tice DA, Chen X. In vitro and in vivo characterization of 64Cu-labeled Abegrin™, a humanized monoclonal antibody against integrin αvβ3. Cancer Res. 2006;66:9673–9681. doi: 10.1158/0008-5472.CAN-06-1480. [DOI] [PubMed] [Google Scholar]
- 28.Milsom C, Magnus N, Meehan B, Al-Nedawi K, Garnier D, Rak J. Tissue factor and cancer stem cells: is there a linkage? Arterioscler Thromb Vasc Biol. 2009;29:2005–2014. doi: 10.1161/ATVBAHA.108.177444. [DOI] [PubMed] [Google Scholar]
- 29.Kasthuri RS, Taubman MB, Mackman N. Role of tissue factor in cancer. J Clin Oncol. 2009;27:4834–4838. doi: 10.1200/JCO.2009.22.6324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bardeesy N, DePinho RA. Pancreatic cancer biology and genetics. Nat Rev Cancer. 2002;2:897–909. doi: 10.1038/nrc949. [DOI] [PubMed] [Google Scholar]
- 31.Laheru D, Jaffee EM. Immunotherapy for pancreatic cancer - science driving clinical progress. Nat Rev Cancer. 2005;5:459–467. doi: 10.1038/nrc1630. [DOI] [PubMed] [Google Scholar]
- 32.Wu AM. Antibodies and antimatter: the resurgence of immuno-PET. J Nucl Med. 2009;50:2–5. doi: 10.2967/jnumed.108.056887. [DOI] [PubMed] [Google Scholar]
- 33.Asa SL. Pancreatic endocrine tumors. Mod Pathol. 2011;24(2):S66–77. doi: 10.1038/modpathol.2010.127. [DOI] [PubMed] [Google Scholar]
- 34.van Dam GM, Themelis G, Crane LM, et al. Intraoperative tumor-specific fluorescence imaging in ovarian cancer by folate receptor-alpha targeting: first in-human results. Nat Med. 2011;17:1315–1319. doi: 10.1038/nm.2472. [DOI] [PubMed] [Google Scholar]
- 35.Yang Y, Zhang Y, Hong H, Liu G, Leigh BR, Cai W. In vivo near-infrared fluorescence imaging of CD105 expression. Eur J Nucl Med Mol Imaging. 2011;38:2066–2076. doi: 10.1007/s00259-011-1886-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buckle T, van den Berg NS, Kuil J, et al. Non-invasive longitudinal imaging of tumor progression using an 111indium labeled CXCR4 peptide antagonist. Am J Nucl Med Mol Imaging. 2012;2:99–109. [PMC free article] [PubMed] [Google Scholar]
- 37.Hao G, Hajibeigi A, De León-Rodríguez LM, Öz OK, Sun X. Peptoid-based PET imaging of vascular endothelial growth factor receptor (VEGFR) expression. Am J Nucl Med Mol Imaging. 2011;1:65–75. [PMC free article] [PubMed] [Google Scholar]
- 38.Dearling JL, Voss SD, Dunning P, et al. Imaging cancer using PET--the effect of the bifunctional chelator on the biodistribution of a 64Cu-labeled antibody. Nucl Med Biol. 2011;38:29–38. doi: 10.1016/j.nucmedbio.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hong H, Benink HA, Zhang Y, et al. HaloTag: a novel reporter gene for positron emission tomography. Am J Transl Res. 2011;3:392–403. [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang Y, Hong H, Engle JW, et al. Positron emission tomography imaging of CD105 expression with a 64Cu-labeled monoclonal antibody: NOTA is superior to DOTA. PLoS One. 2011;6:e28005. doi: 10.1371/journal.pone.0028005. [DOI] [PMC free article] [PubMed] [Google Scholar]