Abstract
Background
The study was conducted to examine the effectiveness of two different interventions on oral contraception (OC) adherence and condom use.
Study Design
A total of 1,155 women 16–24 years of age requesting OC were randomized to receive either face-to-face behavioral counseling and education at their baseline clinic visit (C group; n=383) or this same intervention followed by monthly phone calls for 6 months (C+P group; n=384) or standard care (S group; n=388). Phone interviews at 3, 6, and 12 months after the initial visit as well as a medical record review assessed OC continuation, condom use, and several other secondary and clinically meaningful outcomes such as pregnancy and sexually transmitted infection (STI) rates, and correct use of pills.
Results
The interventions did not have a significant effect on OC continuation after 3 (C+P: 58%; C: 50%; S: 55%), 6 (39%; 32%; 37%) or 12 months (20%; 18%; 20%) (p>.05). Condom use at last sexual intercourse did not differ by intervention methods (p>.05). Moreover, no effect was observed on pregnancy [S=48 (12.4%), C=63 (16.5%), C+P=52 (13.5%); p=.22) and STI [S=18 (4.6%), C=12 (3.1%), C+P=13 (3.4%); p=.50) rates, and mean number of correctly used pill packs (p=.06). However, those randomized to C+P were more likely than C and S patients to identify a cue and report that the cue worked as a reminder to take their OC on time based on 3 and 6 months follow-up information (p<.01 for all relationships).
Conclusions
Neither intervention in this study improved OC adherence among young women.
CLINICAL TRIAL REGISTRATION
ClinicalTrials.gov, www.ClinicalTrials.gov, NCT00584038.
1. Introduction
Many young women experience difficulty using oral contraception (OC) consistently or correctly. Moreover, among young users, almost half discontinue its use within 6 months of obtaining a prescription [1, 2]. These young women are at high risk of an unintended pregnancy because they often fail to use another contraceptive method after discontinuing their birth control pills. In one study of women, 33% of those 13 to 19 years of age and 18% of 20 to 22 year olds reported that they did not use any contraception for at least 1 month after stopping their birth control pills, even though they did not wish to become pregnant [3].
Further compounding the problem is that among those who continue to use OC for at least 6 months, a large proportion fail to take it correctly. In one nationwide study of 943 women (mean age 25 years), 47% of OC users missed ≥1 pill per cycle and 22% missed ≥2. Increased odds of missing ≥2 pills was associated with lacking an established pill-taking routine, not reading or understanding the informational material accompanying the pill package, or experiencing side effects [4]. Difficulty with adherence is even more pronounced among high school and college age women. In one study, only 52% of university students who were prescribed OC took all their active birth control pills during the first 3 months [5]. A prior study on 211 teens seen at our institution reported that nearly 60% of OC users missed one or more pills within the last 3 months and 10% missed at least three pills in the last cycle [1].
From these data, it is apparent that interventions must be developed to improve the consistency and correctness of OC use among young women. Suggestions on how to address this problem were made in 2003 by an interdisciplinary group of researchers and service providers, following a National Institutes of Health (NIH) funded meeting on this topic [6]. They noted that the current system used by most clinics of providing oral contraception at a single brief visit is not effective as providers can spend only a few minutes on education [7], which is not sufficient to meet the needs of younger women. This problem is compounded by the fact that the next follow-up visit does not occur until several months later. To address this, they suggested adding health educators to clinic staff or phone call interactions between visits [6]. Others have suggested that providers give OC users a toll-free number they could call if they missed pills, experienced breakthrough bleeding, or were confused about when to start a new package [8].
An examination of the literature, however, demonstrates that few studies have actually evaluated the effectiveness of additional educational or behavioral counseling on contraceptive adherence. Furthermore, most of those that have been published are limited in their usefulness because they did not measure clinically meaningful outcomes, such as unintended pregnancy rates [9–11]. A recent Cochrane review based on randomized controlled trials (RCTs) also emphasized the need for a high quality RCT as the RCTs included in the review had several limitations [12]. The purpose of the present study was to fill this gap in knowledge by testing two comprehensive educational and behavioral interventions designed to increase contraceptive adherence among young low income women. Furthermore, the efficacy of these interventions in increasing dual method use (joint use of a condom for protection from STIs and a highly effective contraceptive method) and decreasing rates of STI and unintended pregnancy was assessed.
2. Methods
A randomized, controlled trial was conducted to examine the effect of clinic-based intervention (C) and a clinic-based plus telephone (C+P) intervention on contraceptive adherence among young women initiating use of OC at one of five publicly funded reproductive health clinics in Southeast Texas. These clinics serve low income women, of which 80% have an annual income below US$ 30,000/yr. After obtaining approval from the University of Texas Medical Branch (UTMB) Institutional Review Board, sexually active, non-pregnant females 16 to 24 years old who requested initiation of OC between July 2006 and January 2010 were invited to participate. Exclusion criteria included a desire to become pregnant in the next year, a medical contraindication to OC, and current or prior (>1 month) OC use.
After obtaining, informed consent, patients were randomized into 3 groups to receive standard clinical care alone or one of two interventions. A fully documented randomization scheme developed by the UTMB Office of Biostatistics using the PLAN procedure (SAS Institute, Cary, NC) was followed for allocation. This was a single-blinded study as staff who made assessment phone calls were blinded to the intervention group. However, we could not mask our participants due to the nature of the interventions.
Pilot testing of the interventions was conducted among 18 clinic patients who met all inclusion and exclusion criteria. For the pilot study, each subject was contacted approximately 2 weeks after the clinic-based intervention (for C subjects) or after two phone calls (for C+P subjects) to assess the subject’s experience, including her opinions and perceptions of the relevance of the intervention material and her ability to apply the information. Overall, the interventions were highly rated at both sites. The length of time spent with the health educator was rated as appropriate by all but one subject. Eighty-seven percent stated that instructions on how to initiate OC were extremely clear and 96% stated the instructions were clear about what to do if they missed a pill. In addition, almost all participants found the health educator to be personable, trustworthy, concerned, and helpful. Due to the large percentage of women who responded positively, it was determined that the intervention was ready for implementation and recruitment for the main study began.
Patients randomized to standard care (S) received all of their contraceptive services from a nurse provider who followed a written protocol for new OC users. Patients were given oral and written instructions and dispensed a 4-month supply of OCs. As was standard of care in these clinics at the time of the study (2006–2010), all patients were instructed to initiate OC within 7 days of starting their next menstrual cycle. A supply of 24 condoms was given to all patients free of charge and a follow-up appointment was made for 3 months. At the second visit, 9 additional months of OC were dispensed.
Participants randomized to the clinic-based (C) group also met one-on-one with a contraceptive counselor for approximately 45 min after completing their visit with the practitioner. The intervention was delivered by experienced research assistants trained in contraceptive counseling by the first author. Standardization of counseling techniques was tested by audio recording several sessions conducted by each research assistant, which were reviewed to confirm that all key points had been addressed. All counseling was provided in Spanish or English, depending on the patient’s preference.
The counselor used educational and behavioral techniques based on the health belief model and geared toward lower health literacy. The different components of the intervention included 1) distributing handouts with simple, concrete, written instructions for birth control pills and condoms; 2) reviewing instructions verbally using visual aids, in language easily understood by the patient; 3) helping the patient develop a cue, based on her daily routine that would assist her in remembering to take her pill; 4) discussing the risk of pregnancy if contraception was not used correctly and the impact this would have on her life; 5) discussing the noncontraceptive benefits of birth control pills; 6) discussing how to deal with the most common side effects, should they occur, and developing a specific plan for handling them; 7) discussing STIs, and need for condom use; and 8) practicing condom application on a plastic model and discussing condom negotiation skills they could use with their partner.
Subjects randomized to the clinic-based plus telephone (C+P) intervention group received the same treatment at their clinic visit as those randomized to the C group. In addition, they were contacted weekly until they began their OC and then monthly for 6 months by a contraceptive counselor following their baseline visit. Phone calls were made to the number provided by the patient at a time that she indicated would be convenient. Calls were placed weekly until the patient began taking her OC, then monthly. During these phone calls, the counselor reviewed how to take their OC correctly, what to do when doses were missed, strategies to address side effects, and the importance of condom use. In addition, participants were given a toll-free number they could call 24 h a day, if they needed additional assistance.
At the initial visit, patients were asked to report their age, race/ethnicity, marital status, employment, education level, grade levels repeated in school, number of sexual partners in the past year and in their lifetime, parity, prior history of an STI and current condom use. Factors associated with contraceptive adherence in the literature were also assessed. Since women who do not understand the written instructions for OCs are at high risk for poor adherence [13], we measured their health literacy with the short Test of Functional Health Literacy in Adults (S-TOFHLA) [14]. This instrument was derived from the longer, well-established TOFHLA and is available in English and Spanish [15, 16]. In addition, participants were assessed at baseline to examine their attitude toward as well as perceived risk and susceptibility of pregnancy as these factors may alter contraceptive adherence behaviors. Attitudes toward pregnancy were assessed using two items from the Add Health project [17] which used a five point agree–disagree scale. The first item was “Getting pregnant at this time in my life is one of the worst things that could happen to me” (strongly disagree 5 to strongly agree 1) and the second item was “It would not be all that bad if I got pregnant at this time in my life” (strongly disagree 1 to strongly agree 5). Scores of the two items were then averaged with higher scores indicating a more positive attitude toward pregnancy. Perceived risk of becoming pregnant was also assessed using a five-point “strongly disagree” (1) to “strongly agree” (5) rating scale with the statements: “It is likely that I will get pregnant,” “My chances of getting pregnant in the next few years are great,” and “I feel I will get pregnant sometime during my life” [18–20]. Average score of these 3 items ranged from 1 to 5 with higher scores indicating a higher perceived risk for pregnancy. Perceived susceptibility to pregnancy was assessed with the question: “Imagine that you were to have sexual intercourse with someone just once, but were unable to use any method of birth control for some reason. What is the chance that you would get pregnant?” [21]. The response options included the following: “almost no chance (1),” “some chance, but probably not (2),” “a 50–50 chance (3),” “a good chance (4),” and “almost certain (5)” with higher scores indicating higher perceived susceptibility.
Outcomes were assessed among women assigned to each intervention group and the standard care group at 3, 6, and 12 months using data obtained from phone interviews and medical record review. Research participants were reimbursed $20 for the baseline visit and each assessment phone call. At each call, subjects were asked if they were still using OC. They were then asked to retrieve their empty pill packs so they could more accurately remember when they had missed pills. Specific questions were asked regarding number of missed pills, delayed starting of the pill packs and what was done when pills were missed. Correct use of OCs was defined as starting each pack on time and not missing any doses or correctly making up any pills missed.
Use of condoms in addition to OC was assessed at 3, 6, and 12 months. Consistent condom use was documented for individuals who reported using a condom every time they had sex. Those who used OC correctly and condoms consistently were considered dual users. Those who reported inconsistent condom use were also asked: “The last time you had sexual intercourse, did your partner use a condom?”
In addition, pregnancy and STI rates were assessed by self-report and medical record review after 3, 6, and 12 months. During the phone assessments, each subject was asked whether she had become pregnant or been diagnosed with a STI. At the conclusion of the study, the entire UTMB medical record of each subject since beginning the study was reviewed to detect any additional unreported STIs or pregnancies over the 12-month interval. Participants’ satisfaction was assessed by asking, “Overall, how satisfied are you with your current method of birth control?” to which subjects responded using a Likert-type scale. In addition, participants were asked whether they would recommend using OC to a friend.
We based our sample size using our previous study estimations which showed adherence rates for OC users were approximately 87% at 3 months, 76% at 6 months, and 63% at 12 months (22) and assumed that the parameters would be similar to OC adherence of C+P group in this study. We also assumed that an odds ratio of 2 for the C+P group compared to “C” or “S” groups would be clinically meaningful. Using a two-group continuity corrected chi-square test of equal proportions with a 0.05 two-sided significance level, we calculated that 190 women would be required in each group (570 in total after 12 months) to have 90% power to detect odds ratio (OR) with a magnitude of 2.0 for OC continuation after 12 months (C + P vs. S or C).
2.1. Statistical analysis
We used an intent-to-treat approach to test our hypothesis that one or both interventions would increase OC continuation. OC adherence variables, such as OC continuation, dual method use, and condom use at last sexual intercourse, measured at 3, 6 and 12 months were considered as primary outcomes. Proportions of these ends points were compared between randomized groups using 2-sided χ2 tests.
We conducted additional analyses based on other adherence variables such as discontinuation of the study, identification of a cue, method satisfaction, recommending the method to friends and clinically meaningful outcomes which include pregnancy and STI rates, and correct use of pills. Analysis of variance, chi-square, or Fisher’s exact tests were conducted, as appropriate, for the comparisons between randomized groups. We also used generalized estimating equations (GEE) procedures [23] to examine the association of interventions with contraceptive adherence variables after adjusting for age and race/ethnicity which are known confounders. Besides Cox proportional hazards models were also used to examine the association of intervention methods with the incidence of pregnancy and STI. Any variables that were unevenly distributed across study groups were controlled for in the multivariate statistical models. All analyses were performed using STATA 11 (Stata Corp, College Station, TX).
3. Results
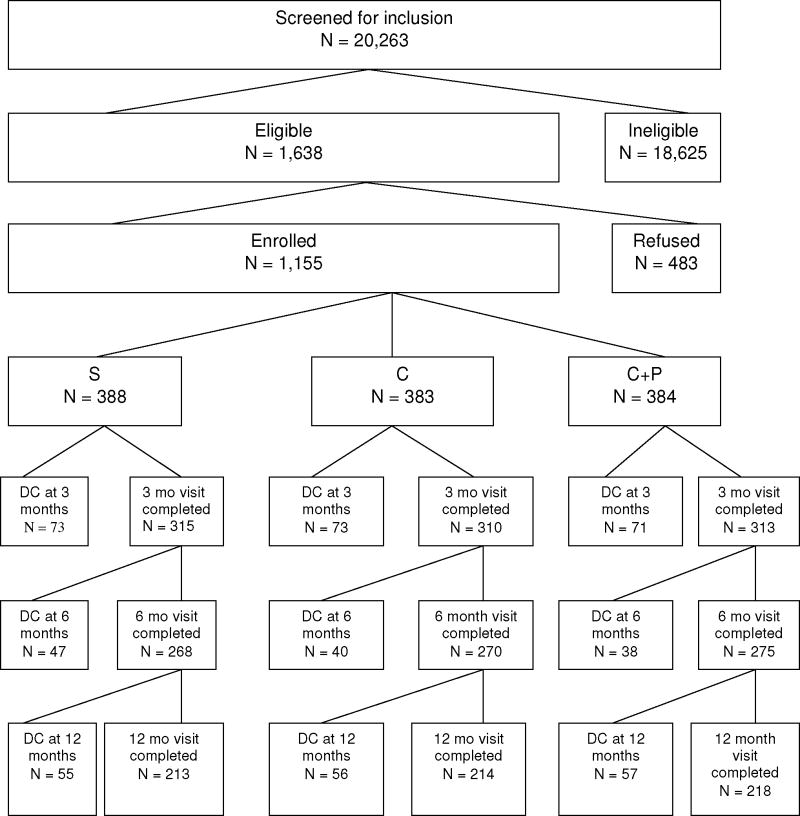
A total of 20,263 women were approached to determine if they were eligible for this study, of which 1,638 women were eligible (Fig. 1). The most common reasons for ineligibility were that they did not want to use OC (57.2%), were already using OC (9.3%), had previously used OC for >1 month (22.7%) or planned to become pregnant within 12 months (3.2%). Of those eligible, 483 (30%) declined to participate, usually due to time constraints that day. Thus, 1155 women met all inclusion/exclusion criteria and agree to be enrolled in the study. No differences were observed between those who refused and those who enrolled with regard to desire for a pregnancy within the next year (p= .26) or having ever had sex (p = .09). However, those who refused participation were significantly older (mean age of those who refused 20.2 ± 2.4 compared to 19.9 ± 2.4 years among those enrolled; p<.001). Although statistically significant, this age difference was felt to be too small to be clinically meaningful. Additionally, Hispanic women were significantly less likely to agree to participate than white and African-American women (65% of Hispanic women vs. 80% of white and African-American women; p<.001).
Fig. 1. Total number of women recruited and followed at 3, 6, and 12 months by intervention group.
DC=Discontinued; mo=month; S=Standard clinic practice; C=Clinic-based intervention; C+P= Clinic-based intervention with phone reinforcement.
Among the 1155 participants, 644 (56%) were between 16 and 19 years of age and 511 (44%) were 20–24 years old. Distribution among racial/ethnic groups was representative of the clinics’ patient bases: 54% were Hispanic (N=626); 19% were black (N=215); 25% were white (N=287); and 2% were other (N=27). Most women were single/never married (78%), and about a quarter worked >20 h per week.
Analyses of baseline characteristics revealed no significant differences between the three study groups with regard to mean age, race, marital status, education, employment, or school performance (Table 1). Furthermore, there were no significant differences at baseline between study groups in history of a prior STI, condom use at last intercourse, number of sexual partners in the last year and lifetime, mean number of prior pregnancies or scores obtained on pregnancy attitudes, perceived risk and susceptibility, and standardized measures of health literacy (Table 1).
Table 1.
Characteristics at baseline by assigned intervention group (N=1155)
| S (N = 388) |
C (N = 383) |
C+P (N = 384) |
p value | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age, mean (±SD) | 20.0 (2.4) | 19.8 (2.3) | 19.9 (2.4) | .47 |
| Race, (%) | .76 | |||
| White | 96 (24.7) | 105 (27.4) | 86 (22.4) | |
| Black | 73 (18.8) | 68 (17.8) | 74 (19.3) | |
| Hispanic | 212 (54.6) | 200 (52.2) | 214 (55.7) | |
| Other | 7 (1.8) | 10 (2.6) | 10 (2.6) | |
| Marital status, (%) | .61 | |||
| Never married | 298 (77.2) | 302 (79.1) | 306 (80.1) | |
| Married, divorced, or separated | 88 (22.8) | 80 (20.9) | 76 (19.9) | |
| Education, (%) | .13 | |||
| Did not complete HS or get GED | 173 (44.9) | 198 (52.2) | 188 (49.3) | |
| At least HS graduate | 212 (55.1) | 181 (47.8) | 193 (50.7) | |
| Employment status, (%) | .32 | |||
| Does not work | 238 (61.3) | 243 (63.4) | 227 (59.1) | |
| Employed ≤ 20 h/wk | 35 (9.0) | 38 (9.9) | 51 (13.3) | |
| Employed > 20 h/wk | 113 (29.1) | 102 (26.6) | 104 (27.1) | |
| Ever repeated a grade in school, (%) | 84 (21.9) | 72 (18.9) | 88 (23) | .35 |
| Reproductive characteristic | ||||
| No. sexual partners in the last year, mean (±SD) | 1.64 (1.4) | 1.63 (1.3) | 1.59 (1.1) | .76 |
| No. lifetime sexual partners, mean (±SD) | 3.9 (5.8) | 3.9 (5.1) | 3.6 (3.3) | .52 |
| Mean number of prior pregnancies, mean (±SD) | 1.4 (0.7) | 1.6 (0.8) | 1.6 (0.8) | .59 |
| History of STI (%) | 102 (26.5) | 102 (26.8) | 97 (25.4) | .89 |
| Condom use at last intercourse (%) | 187 (48.2) | 180 (47.0) | 195 (50.8) | .56 |
| Other possible confounders | ||||
| Attitude toward pregnancy, mean (±SD)a | 2.8 (1.1) | 2.7 (1.1) | 2.6 (1.1) | .14 |
| Perceived risk for pregnancy, mean (±SD)b | 2.9 (0.8) | 2.9 (0.8) | 3.0 (0.8) | .86 |
| Susceptibility for pregnancy, mean (±SD)c | 3.2 (1.0) | 3.2 (1.0) | 3.2 (0.9) | .63 |
| Health literacy, mean (±SD)d | 33.2 (4.6) | 33.4 (3.6) | 33.8 (3.4) | .15 |
S.D.=Standard deviation; S=Standard care; C=Clinic-based intervention with educational information and counseling; C+P=Clinic-based intervention with phone reinforcement.
Numbers vary in some categories due to missing data.
Range of values 1–5; higher values indicate more positive attitude toward pregnancy.
Range of values 1–5; higher values indicate greater perceived risk.
Range of values 1–5; higher values indicate greater perceived susceptibility of pregnancy after unprotected sex.
Range of values 0–36; higher numbers indicate better literacy.
One-way analysis of variance with Bonferroni correction was used for continuous variables and chi-square tests were used for categorical variables. To identify specific pairwise differences for categorical variables, we created separate 2×2 tables for each of the pairs and used chi square tests. To adjust for multiple comparisons, p<.017 (.05/3) was used to indicate statistical significance.
Neither of the interventions (S=19.8%, C=18.0%, C+P=19.8%; p=.77) had a significant effect on OC continuation after 12 months (Table 2). Significant differences were also not seen with regard to dual use of condom and OC, and condom use at last sexual intercourse at any point of follow-up.
Table 2.
OC adherence, dual use of OC and condom, and condom use at last sexual intercourse by intervention group (primary analysis)
| S (N=388) | C (N=383) | C+P (N=384) | p value | |
|---|---|---|---|---|
| Used OC | ||||
| 3 mo | 214 (55.2) | 191 (49.9) | 224 (58.3) | .06 |
| 6 mo | 145 (37.4) | 122 (31.9) | 151 (39.3) | .08 |
| 12 mo | 77 (19.8) | 69 (18.0) | 76 (19.8) | .77 |
| Dual use of OC and condoms, (%) | ||||
| 3 mo | 45 (11.6) | 36 (9.4) | 48 (12.5) | .37 |
| 6 mo | 28 (7.2) | 22 (5.7) | 32 (8.3) | .38 |
| 12 mo | 24 (6.2) | 18 (4.7) | 18 (4.7) | .56 |
| Partner used condom at last sex, (%) | ||||
| 3 mo | 82 (21.1) | 75 (19.6) | 100 (26.0) | .08 |
| 6 mo | 51 (13.1) | 46 (12.0) | 58 (15.1) | .45 |
| 12 mo | 31 (8.0) | 31 (8.1) | 29 (7.6) | .96 |
OC=Oral contraception; S=Standard care; C=Clinic-based intervention with educational information and counseling; C+P=Clinic-based intervention with phone reinforcement.
To identify specific pairwise differences for categorical variables, we created separate 2×2 tables for each of the pairs and used chi square tests. To adjust for multiple comparisons, p<.017 (.05/3) was used to indicate statistical significance.
Secondary analyses based on clinically meaningful outcomes, showed that, of 1155 women, 163 women [overall= 163 (14.1%), S=48 (12.4%), C=63 (16.5%), C+P=52 (13.5%)] became pregnant and 43 (overall = 43 (3.7%), S=18 (4.6%), C=12 (3.1%), C+P=13 (3.4%)] had at least one STI over 12 months. However, the pregnancy (p=.22) and STI (p=.50) rates did not differ between study groups.
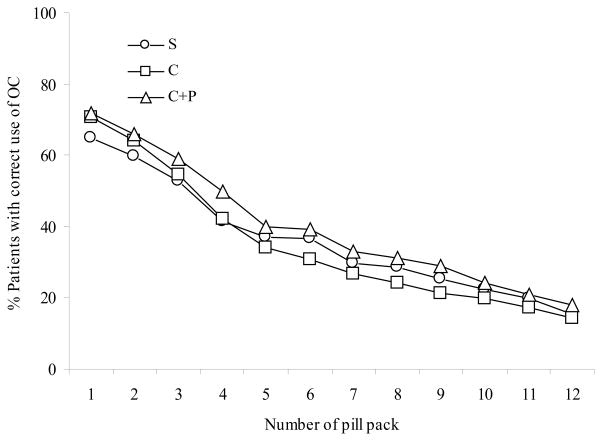
We also observed that the mean number of correctly used pill packs was 5.2 in women randomized to the S group, 5.3 in the C group and 5.9 in the C+P group (p=.064), suggesting that neither intervention significantly increased the duration of correct OC use over standard care. Correct use of each individual pill pack number also did not differ between the two interventions and standard care (Fig. 2). However, a few notable differences were observed. Women in the C+P group were significantly more likely than those in C and S groups to identify a cue at 3 and 6 months (Table 3). The same was also true for the effectiveness of the cue as a reminder to take their OC. Other contraceptive adherence variables such as switching the method, not using any method, or study discontinuation did not differ by study group at any follow-up intervals. There were also no differences between women in the standard care group and those in the two intervention groups with regard to pattern of missed pills (Table 4). We did not observe a differential effect of attitude toward pregnancy, perceived susceptibility or perceived risk scores on OC adherence.
Fig. 2. Participants with correct oral contraceptive use by intervention.
Based on initial number of participants in each intervention group
S=Standard clinic practice (n=388); C=Clinic-based intervention (n=383); C+P=Clinic-based intervention with phone reinforcement (n=384).
Table 3.
Effects of interventions on secondary oral contraceptive adherence variables
| S | C | C+P | p value | |
|---|---|---|---|---|
| Identified a cue, (%) e | ||||
| 3 mo | 141 (44.8) | 149 (48.1) | 205 (65.5)a | <.01 |
| 6 mo | 93 (34.7) | 100 (37.0) | 137 (49.8)a | <.01 |
| 12 mo | 50 (23.5) | 50 (23.4) | 65 (29.8) | .21 |
| Cue served as reminder for pill-taking, (%)e | ||||
| 3 mo | 135 (42.9) | 146 (47.1) | 202 (64.5)a | <.01 |
| 6 mo | 93 (34.7) | 97 (35.9) | 136 (49.5)a | <.01 |
| 12 mo | 50 (23.5) | 49 (22.9) | 63 (28.9) | .28 |
| Satisfaction with method, (%)d,e | ||||
| 3 mo | 171 (54.3) | 152 (49.0) | 187 (59.7)b | .03 |
| 6 mo | 122 (45.5) | 102 (37.8) | 138 (50.2)b | .01 |
| 12 mo | 76 (35.7) | 68 (31.8) | 75 (34.4) | .69 |
| Recommend the method to a friend, (%)e | ||||
| 3 mo | 174 (55.2) | 152 (49.0) | 186 (59.4)b | .03 |
| 6 mo | 131 (48.9) | 103 (38.1) | 140 (50.9)bc | <.01 |
| 12 mo | 77 (36.2) | 68 (31.8) | 75 (34.4) | .63 |
| Switched to method other than OCf | ||||
| 3 mo | 52 (13.4) | 62 (16.2) | 59 (15.4) | .54 |
| 6 mo | 64 (16.5) | 76 (19.8) | 70 (18.2) | .48 |
| 12 mo | 66 (17.0) | 66 (17.2) | 78 (20.3) | .41 |
| Not using any contraceptive methodf | ||||
| 3 mo | 33 (8.5) | 42 (11.0) | 23 (6.0) | .05b |
| 6 mo | 52 (13.4) | 64 (16.7) | 49 (12.8) | .25 |
| 12 mo | 66 (17.0) | 74 (19.3) | 58 (15.1) | .30 |
| Discontinued the studyf | ||||
| 3 mo | 73 (18.8) | 73 (19.1) | 71 (18.5) | .98 |
| 6 mo | 120 (30.9) | 113 (29.5) | 109 (28.4) | .74 |
| 12 mo | 175 (45.1) | 169 (44.1) | 166 (43.2) | .87 |
S=Standard care; C=Clinic-based intervention with educational information and counseling; C+P=Clinic-based intervention with phone reinforcement; OC=Oral contraception.
To identify specific pairwise differences for categorical variables, we created separate 2×2 tables for each of the pairs and used chi square tests. To adjust for multiple comparisons, p<.017 (.05/3) was used to indicate the statistical significance.
Difference between C+P and S, and C+P and C significant at p<.01 level.
Difference between C+P and C significant at p<.01 level.
Difference between S and C significant at p<.01 level.
Numerator was based on those who responded “satisfied” or ‘somewhat satisfied”.
Denominators are based on available individuals at 3, 6, and 12 months with phone call follow-up data.
Denominators are based on all participants recruited at baseline.
Table 4.
Reported missed pills by intervention groupa
| S | C | C+P | p value | |
|---|---|---|---|---|
| Missed active pill during the past week | ||||
| 3 mo | 12 (3.8) | 18 (5.8) | 15 (4.8) | .51 |
| 6 mo | 11 (4.1) | 11 (4.1) | 10 (3.6) | .95 |
| 12 mo | 4 (1.9) | 7 (3.3) | 5 (2.3) | .64 |
| Missed active pill during the past month | ||||
| 3 mo | 50 (15.9) | 52 (16.8) | 58 (18.5) | .67 |
| 6 mo | 29 (10.8) | 30 (11.1) | 38 (13.8) | .49 |
| 12 mo | 19 (8.9) | 25 (11.7) | 14 (6.4) | .16 |
| Missed active pill during the past 3 months | ||||
| 3 mo | 103 (32.7) | 89 (28.7) | 94 (30.0) | .54 |
| 6 mo | 50 (18.7) | 43 (15.9) | 50 (18.2) | .67 |
| 12 mo | 25 (11.7) | 24 (11.2) | 17 (7.8) | .34 |
S=Standard care; C=Clinic-based intervention with educational information and counseling; C+P=Clinic-based intervention with phone reinforcement.
Denominators are based on available individuals at 3, 6, and 12 months with phone call follow- up data.
To identify specific pairwise differences for categorical variables, we created separate 2×2 tables for each of the pairs and used chi square tests. To adjust for multiple comparisons, p<.017 (.05/3) was used to indicate statistical significance.
Estimates based on GEE models showed that women in C and C+P intervention groups did not differ from standard care after 12 months with regard to almost all contraceptive adherence variables (Table 5). However, several positive effects were observed. Women in the C+P group were more likely to report condom use at last sexual intercourse than those in the S group. Furthermore, women in the C+P and C groups were more likely than those randomized to S to identify a cue and report it as a reminder of pill-taking. Based on Cox proportional hazards regression models, we failed to observe a difference between the intervention groups and standard care with regard to pregnancy and STI risk over 12 months of follow-up.
Table 5.
Association of intervention type with primary (OC continuation, dual use of OC and condom, and condom use at last sexual intercourse) and secondary outcomes (other OC adherence variables, and pregnancy and STI rates)
| Contraceptive adherence characteristics | S [OR (95% CI)] | C [OR (95% CI)] | C+P [OR (95% CI)] |
|---|---|---|---|
| Continued to use OC | 1.00 | 0.80 (0.63–1.03) | 1.09 (0.86–1.40) |
| Dual use of OC and condoms | 1.00 | 1.01 (0.75–1.37) | 1.14 (0.85–1.53) |
| Partner used condom at last sex | 1.00 | 1.12 (0.87–1.45) | 1.32 (1.03–1.70) |
| Switched to method other than OC | 1.00 | 1.18 (0.89–1.57) | 1.18 (0.98–1.57) |
| Not using any contraceptive method | 1.00 | 1.26 (0.93–1.70) | 0.86 (0.62–1.19) |
| Discontinued the study | 1.00 | 0.93 (0.71–1.21) | 0.91 (0.70–1.96) |
| Identified a cue | 1.00 | 2.00 (1.48–2.71) | 4.64 (3.27–6.60) |
| Cue served as reminder for pill- taking | 1.00 | 1.71 (1.29–2.28) | 3.64 (2.66–5.00) |
| Satisfaction with method | 1.00 | 0.91 (0.70–1.18) | 1.23 (0.93–1.61) |
| Recommend OC to a friend | 1.00 | 0.79 (0.59–1.06) | 1.22 (0.89–1.66) |
| Pregnancya | 1.00 | 1.39 (0.95–2.03)b | 1.07 (0.72–1.59)b |
| STIa | 1.00 | 1.01 (0.46–2.21)b | 0.70 (0.31–1.59)b |
OC=Oral contraception; STI= Sexually transmitted infection; CI=Confidence intervals S=Standard care; C=Clinic-based intervention with educational information and counseling; C+P=Clinic-based intervention with phone reinforcement.
Adjusted by race (non-Hispanic whites, non-Hispanic black, Hispanics), age (16–19 yr vs. 20–24 yr) and follow-up visit as a categorical variable (3, 6, 12 month).
Cox proportional hazards models were used for pregnancy and STI and adjusted by age and race/ethnicity.
Hazard ratio.
4. Discussion
In this study, we observed that women who received additional education on how to use OC were no more likely than those randomized to standard care to remain on this method or to do so correctly. This suggests that merely adding additional educational time to the clinic visit or immediately afterwards by telephone may not be sufficient to increase adherence with OC use among young, low income women at high risk of unintended pregnancy. These findings agree with two studies published in 2010 [10, 24] on this topic, one which used similar methodology to our investigation [24]. In that study of 805 adolescents 14–18 years of age, no differences were observed between those randomized to receive standard care vs those who received standard care plus nine follow-up phone calls over 12 months. Furthermore, the authors reported that clinic counselors were only able to complete 2.7 calls per patient and had to make 7.8 attempts for every completed call. Thus, this intervention was very time-consuming and expensive. The current investigation supports their conclusion that calling patients after their visit does not appear to be an effective method to improve compliance with OC use among adolescents.
Our interventions may have failed due to their reliance on improving the knowledge base of the women. It is possible that more sessions would have improved our results. Patients may, however, know what to do and still not remember to take their medication. In fact, one of the most common reasons cited by our participants for missing pills was an inability to remember taking them. To address this, all women in the intervention groups were taught to identify a cue, such as brushing their teeth, which they could associate with taking their medication. Our study demonstrated a relationship between C+P intervention and development of a cue, although did not have any impact on OC adherence. A recent randomized study of 683 young women demonstrated that text messaging was effective in increasing adherence with OC use [25], suggesting that helping patients to remember their medication may be the most important component of any intervention. Future studies should further explore how modern technology could best be used to address this important issue.
One concerning finding from this study is that almost 20% of women reported missing at least 1 active pill during the last month when interviewed at 3 months. It is likely that this number is actually an underestimate of the number of missed pills as a prior study noted that under-reporting of missed birth control pills was common when compared to recordings made by an electronic monitoring device [10]. In fact, that study showed that women actually missed an average of >4 pills per cycle. This high rate of missed doses places users at significant risk of unintended pregnancy and accounts for the large discrepancy between theoretical and actual user effectiveness of OC.
The high rate of missed doses and failure to switch to a method with which they could adhere were very likely factors in the high pregnancy rate we observed (14%), even though all had been prescribed effective birth control and stated that they did not wish to become pregnant during the following 12 months. This high pregnancy rate, irrespective of interventions, demonstrates the frequent inability of young women to adhere to the daily regimen required to use birth control pills. This was demonstrated in a recent study of 5,087 women 14 to 25 years of age which showed that those who used OC had a much higher discontinuation rate after 12 months than those who selected an intrauterine device (IUD) for birth control. Satisfaction was also higher among users of IUDs (80%) than OC (41%) [26]. Based on their findings, the authors suggested that long-acting contraception, such as IUDs or implants, may be easier for young women to use correctly because they are not user-dependent.
Furthermore, these interventions did not increase the percentage of women who practiced dual use. This is unfortunate as dual use not only offers protection against STIs, but also acts as a back-up method when OCs are not taken correctly. In fact, it has been estimated that if half of all women who used hormonal methods alone also used condoms, 40% of unplanned pregnancies among this population could be prevented [27]. Furthermore, those who use both condoms and a hormonal method report high sexual satisfaction scores, probably because they feel more protected against unwanted pregnancies and STIs [28].
One beneficial effect of both interventions was that more women in the C+P than the S group reported using condoms at last intercourse based on GEE analysis although did not achieve statistical significance based on primary analyses. This finding appears to have been driven by a higher likelihood to use condoms within the first 3 months after beginning the study. The 3-month follow-up interview was the closest time point to the actual intervention, when subjects practiced placing condoms on models and negotiating condom use with a partner. Thus, it is logical that they would be most comfortable with this practice when their training was more recent.
This study has several limitations. A number of the instruments relied on self-report and may have biased our findings. Also, a possibility exists that the assessment calls to the S group acted as an intervention, thus causing their outcomes to resemble that of the intervention groups. In addition, the number of women lost to follow-up was greater than anticipated. One reason for this was that many women lived in the region affected by Hurricane Ike which made landfall while the study was in progress. Many participants were relocated to other areas of Texas and could not be contacted.
Overall, we observed that additional education alone may not be sufficient to increase adherence with OC use among young, low income women at high risk of unintended pregnancy. However, extending contact between health care personnel and patients did result in development of a cue. Data from this large randomized study may be useful in developing more sophisticated interventions to increase OC compliance, such as those using text messaging. Furthermore, the use of similar interventions among adolescents using long-acting reversible contraception may result in more dual use and better health outcomes for young women.
Acknowledgments
This study was supported by an award from the Maternal and Child Health Bureau, Health Resources and Services Administration (R40MC06634, Berenson) and a midcareer investigator award in patient-oriented research (K24HD043659, Berenson), from the Eunice Kennedy Shriver National Institute of Child Health & Human Development, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the MCHB, HRSA, NICHD, or the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Berenson AB, Wiemann CM. Contraceptive use among adolescent mothers at 6 months postpartum. Obstet Gynecol. 1997;89:999–1005. doi: 10.1016/s0029-7844(97)00123-3. [DOI] [PubMed] [Google Scholar]
- 2.Wiemann CM, Berenson AB. An investigation into why adolescents may reject Norplant. Pediatrics. 1996;97:185–91. [PubMed] [Google Scholar]
- 3.Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: a prospective evaluation of frequency and reasons. Am J Obstet Gynecol. 1998;179:577–82. doi: 10.1016/s0002-9378(98)70047-x. [DOI] [PubMed] [Google Scholar]
- 4.Rosenberg MJ, Waugh MS, Burnhill MS. Compliance, counseling and satisfaction with oral contraceptives: a prospective evaluation. Fam Plann Perspect. 1998;30:89–92. 104. [PubMed] [Google Scholar]
- 5.Oakley D, Potter L, de Leon-Wong E, Visness C. Oral contraceptive use and protective behavior after missed pills. Fam Plann Perspect. 1997;29:277–9. 87. [PubMed] [Google Scholar]
- 6.Kalmuss D, Davidson A, Cohall A, Laraque D, Cassell C. Preventing sexual risk behaviors and pregnancy among teenagers: linking research and programs. Perspect Sex Reprod Health. 2003;35:87–93. doi: 10.1363/3508703. [DOI] [PubMed] [Google Scholar]
- 7.Lipkin M., Jr Physician-patient interaction in reproductive counseling. Obstet Gynecol. 1996;88:31S–40S. doi: 10.1016/0029-7844(96)00247-5. [DOI] [PubMed] [Google Scholar]
- 8.Cramer JA. Compliance with contraceptives and other treatments. Obstet Gynecol. 1996;88:4S–12S. doi: 10.1016/0029-7844(96)00248-7. [DOI] [PubMed] [Google Scholar]
- 9.Gilliam M, Knight S, McCarthy M., Jr Success with oral contraceptives: a pilot study. Contraception. 2004;69:413–8. doi: 10.1016/j.contraception.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Hou MY, Hurwitz S, Kavanagh E, Fortin J, Goldberg A. Using daily text-message reminders to improve adherence with oral contraceptives: a randomized controlled trial. Obstet Gynecol. 2010;116:633–40. doi: 10.1097/AOG.0b013e3181eb6b0f. [DOI] [PubMed] [Google Scholar]
- 11.Jay MS, DuRant RH, Shoffitt T, Linder CW, Litt IF. Effect of peer counselors on adolescent compliance in use of oral contraceptives. Pediatrics. 1984;73:126–31. [PubMed] [Google Scholar]
- 12.Halpern V, Lopez LM, Grimes DA, Gallo MF. Strategies to improve adherence and acceptability of hormonalmethods of contraception. Cochrane Database of Systematic Reviews. 2011;(4):Art. No.: CD004317. doi: 10.1002/14651858.CD004317.pub3. [DOI] [PubMed] [Google Scholar]
- 13.Rosenberg MJ, Waugh MS, Meehan TE. Use and misuse of oral contraceptives: risk indicators for poor pill-taking and discontinuation. Contraception. 1995;51:283–88. doi: 10.1016/0010-7824(95)00074-k. [DOI] [PubMed] [Google Scholar]
- 14.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 15.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 16.Nurss JR, Parker R, Williams M, Baker D. TOFHLA: Test of Functional Health Literacy in Adults. Snow Camp, NC: Peppercorn Books & Press; 2001. [Google Scholar]
- 17.Jaccard J, Dodge T, Dittus P. Do adolescents want to avoid pregnancy? Attitudes toward pregnancy as predictors of pregnancy. J Adolesc Health. 2003;33:79–83. doi: 10.1016/s1054-139x(03)00134-4. [DOI] [PubMed] [Google Scholar]
- 18.Stanton BF, Li X, Galbraith J, Feigelman S, Kaljee L. Sexually transmitted diseases, human immunodeficiency virus, and pregnancy prevention: Combined contraceptive practices among urban African-American early adolescents. Arch Pediatr Adolesc Med. 1996;150:17–24. doi: 10.1001/archpedi.1996.02170260021003. [DOI] [PubMed] [Google Scholar]
- 19.Hester NR, Macrina DM. The health belief model and the contraceptive behavior of college women: implications for health education. J Am Coll Health. 1985;33:245–52. doi: 10.1080/07448481.1985.9935034. [DOI] [PubMed] [Google Scholar]
- 20.Champion VL, Skinner CS, Foster JL. The effects of standard care counseling or telephone/in-person counseling on beliefs, knowledge, and behavior related to mammography screening. Oncol Nurs Forum. 2000;27:1565–71. [PubMed] [Google Scholar]
- 21.Jaccard J, Helbig DW, Wan CK, Gutman MA, Kritz-Silverstein DC. The prediction of accurate contraceptive use from attitudes and knowledge. Health Educ Q. 1996;23:17–33. doi: 10.1177/109019819602300102. [DOI] [PubMed] [Google Scholar]
- 22.Berenson AB, Rahman M, Radecki Breitkopf C, Bi Lian X. A prospective cohort study, controlled study on the effects of depot medroxyprogesterone acetate 20 μg birth control pills on bone mineral density. Obstetrics & Gynecology. 2008;112:788–99. doi: 10.1097/AOG.0b013e3181875b78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liang K, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 24.Kirby D, Raine T, Thrush G, Yuen C, Sokoloff A, Potter SC. Impact of an intervention to improve contraceptive use through follow-up phone calls to female adolescent clinic patients. Perspect Sex Reprod Health. 2010;42:251–7. doi: 10.1363/4225110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Castaño PM, Bynum JY, Andrés R, Lara M, Westhoff C. Effect of daily text messages on oral contraceptive continuation: a randomized controlled trial. Obstet Gynecol. 2012;119:14–20. doi: 10.1097/AOG.0b013e31823d4167. [DOI] [PubMed] [Google Scholar]
- 26.Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117:1105–13. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pazol K, Kramer MR, Hogue CJ. Condoms for dual protection: patterns of use with highly effective contraceptive methods. Public Health Rep. 2010;125:208–17. doi: 10.1177/003335491012500209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Higgins JA, Hoffman S, Graham CA, Sanders SA. Relationships between condoms, hormonal methods, and sexual pleasure and satisfaction: an exploratory analysis from the Women’s Well Being and Sexuality Study. Sex Health. 2008;5:321–30. doi: 10.1071/sh08021. [DOI] [PMC free article] [PubMed] [Google Scholar]