Summary
We introduce our training tools and system of neurovascular intervention. An in vitro cerebral vascular model was used for the young residents to understand the basic interventional techniques and devices.
The model included several vascular lesions such as cerebral aneurysm, dural arterio-venous fistula, or carotid artery stenosis. Endovascular procedures in the model were performed under fluoroscopic or direct visual control, and consecutive haemodynamic changes were visualized by using digital subtraction angiography and direct observation. Thus, traineess could have an easy understanding of clinical conditions. New medical devices, such as platinum coils, were successfully implanted in the model under stable conditions.
After the initial training using vascular model, the residents had started clinical experiences under the control of senior surgeons. Although it is difficult to describe usefulness of our clinical training, we believe that we provide enough good quality and quantity of clinical cases to the residents. Because our endovascular team has recently had150-200 interventional procedures every year, one resident can have experienced more than 100 cases per year. The qualification of a Board Certified Specialist of the Japanese Society of Intravascular Neurosurgery (JSIN) requires that the applicant must have experienced more than 100 cases for four years. So our residents can have enough case materials to qualify the board examination.
Key words: cerebral aneurysm, dural arterio-venous malformation, carotid artery stenosis, endovascular treatment, in vitro model, medical training
Introduction
Recently, neurovascular intervention has rapidly become widespread. This procedure is less invasive, safe, useful, and developing with various devices such as Guglielmi detachable coil (GDC) 1.
The endovascular treatment requires manual skill that develops with technical experience and surgeons are best trained under the careful supervision of senior staff. However, this therapeutic field is relatively new, and the training system of the neurovascular intervention has not yet established in Japan. The Japanese Society of Intravascular Neurosurgery (JSIN) started the board certification system from 2000 to avoid unnecessary complications, which are caused by improper techniques and immature experiences 2. We introduce our training system for young neurosurgeons using in vitro vascular model as a basic understanding of techniques and devices, and daily clinical practice. We hope that this paper may help other endovascular team for establishing endovascular training system.
Methods
We have started neurovascular intervention procedure at our department of neurological surgery on 1980’s. From that time, our basic training system for young neurosurgeons was almost same. We set three-year period for the residents to be trained as a endovascular neurosurgeon after general neurosurgical training for at least three years. So one could join our endovascular team with enough knowledge of general neurosurgical field 3.
During this three-year period, young neurosurgeons made experimental studies, which were related to neurovascular intervention as a basic research. In the same time, they started clinical experiences in the endovascular team.
Recently, we could have good in vitro vascular model 4-7, and applied it for the initial training. After understandings of the basic endovascular techniques and devices using the model, they started clinical practice under the careful supervision of senior staff.
In-vitro Vascular Model
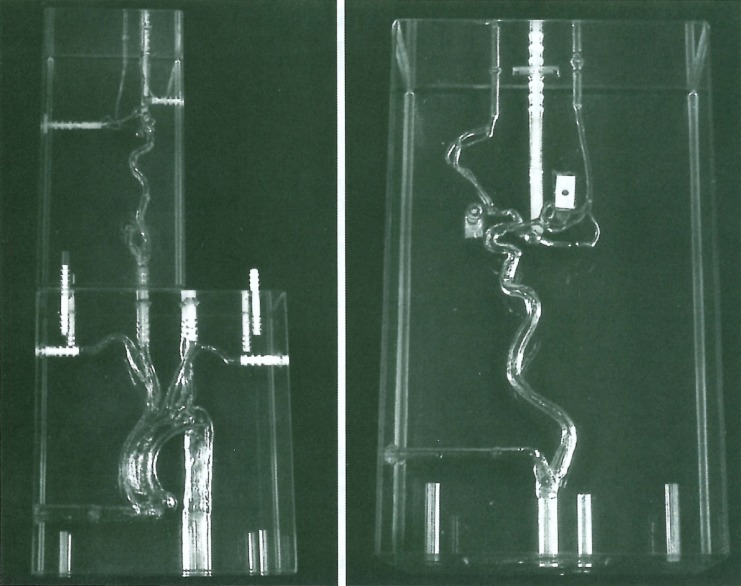
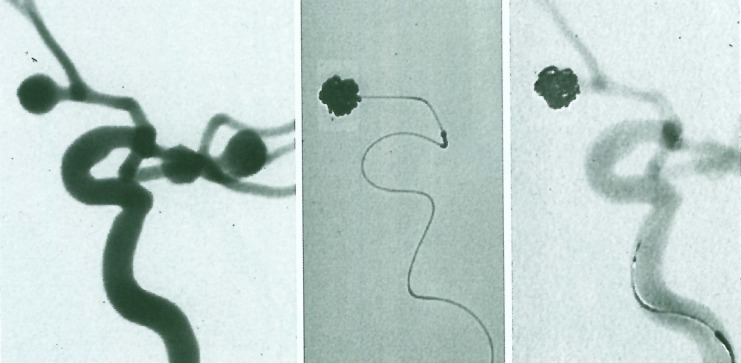
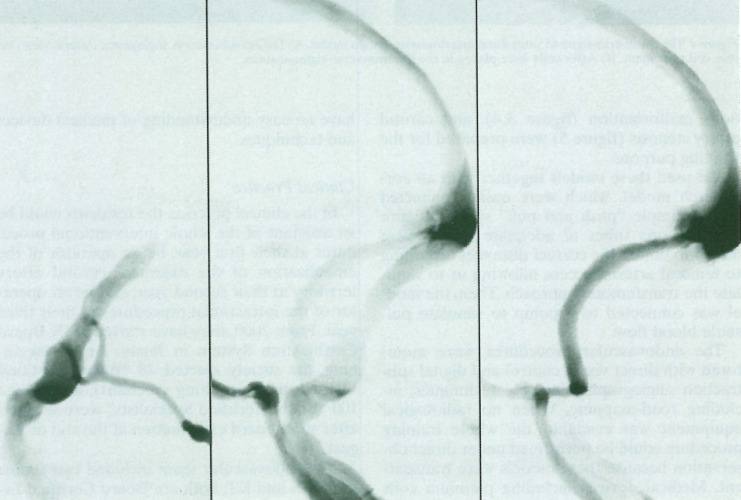
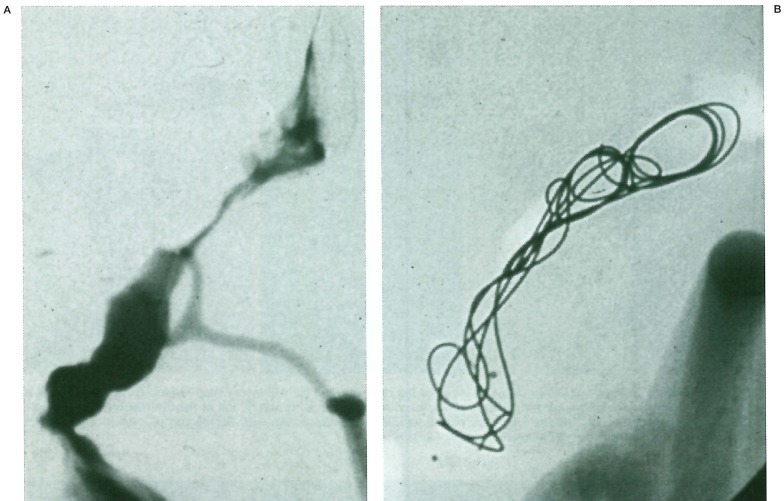
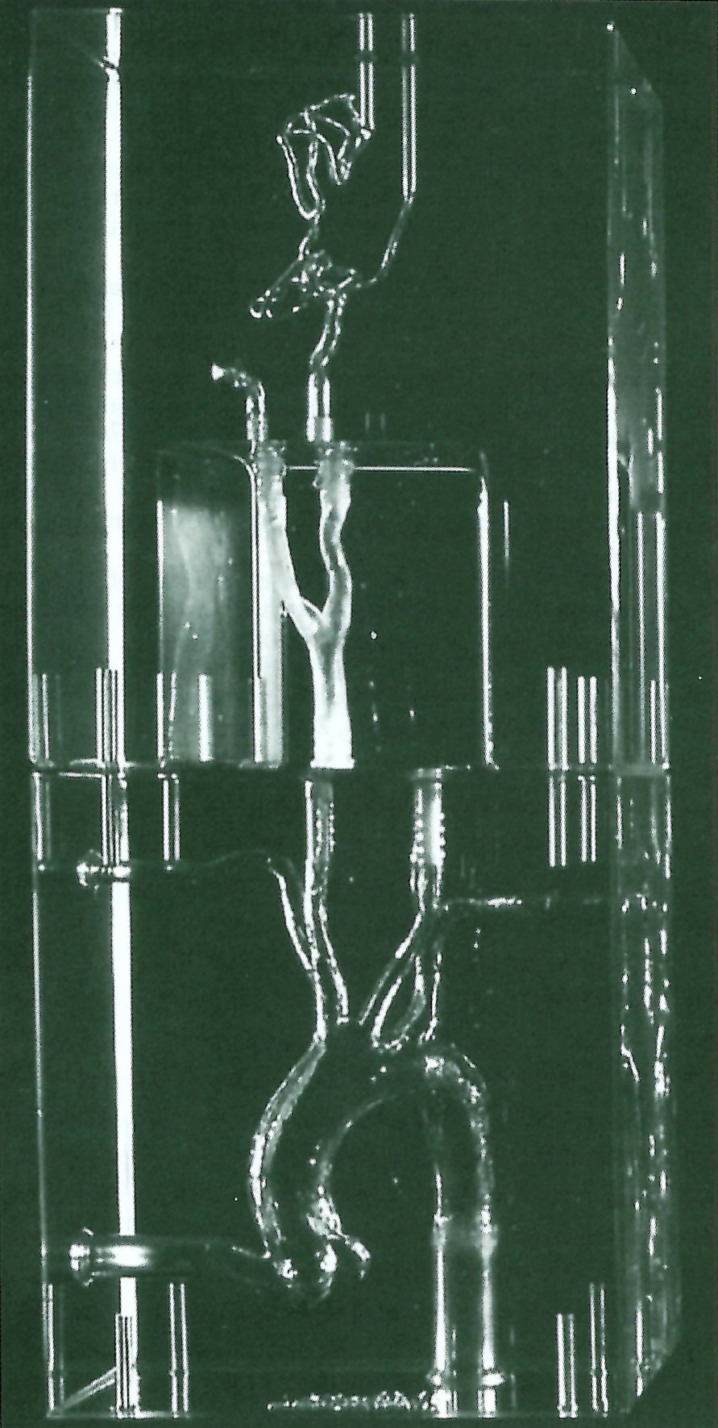
A description of making vascular models using "lost wax" technique has been reported 4-8. The transparent silicone models were anatomically accurate and reproducible copies of human vascular casts. Flow conditions could be simulated through a circuit by using the electric pump. Several vascular lesions including cerebral aneurysm (figure 1,2), dural arteriovenous malformation (figure 3,4), and carotid artery stenosis (figure 5) were prepared for the training purpose.
Figure 1.
The right carotid artery rigid model with three aneurysms (at the origin of the posterior communicating artery, in the anterior communicating artery, and at the bifurcation of the middle cerebral artery). This silicone block can be connected to an aortic arch silicone block with a simple "push and pull" connection system. White obturators connected to each aneurysmal cavity are seen. left) A-P view with the aortic arch. right) Lateral view of the right carotid artery block.
Figure 2.
Digital subtraction angiograms (lateral view) of the right internal carotid artery rigid model. Three aneurysms (at the origin of the posterior communicating artery, in the anterior communicating artery, and at the bifurcation of the middle cerebral artery) are seen. left) Before coils were placed. middle) non-subtraction view during coil placement. right) After coils were placed in the anterior communicating artery aneurysm.
Figure 3.
Digital subtraction angiograms (lateral view) of the transverse-sigmoid sinus dural arteriovenous fistula model. The occipital artery was directly connected into the transverse-sigmoid sinus junction, and both anterograde-flow to jugular vein and retrograde-flow to the superior sagittal sinus were seen.
Figure 4.
The transverse-sigmoid sinus dural arteriovenous fistula model. A) Digital subtraction angiograms (lateral view) before coil placement. B) After coils were placed in the the transverse-sigmoid sinus.
Figure 5.
The right carotid artery stenosis model with an aortic arch block. A stent can be placed into the stenotic portion. The implanted stent can be easily removed, and the model can be reused.
We used these models together with an aortic arch model, which were easily connected with a simple "push and pull" system (figure 1,5). Silicone tubes of adequate length were added to obtain the correct distances according to femoral arterial access, allowing us to simulate the transfemoral approach. Then, the model was connected to a pump to simulate pulsatile blood flow.
The endovascular procedures were monitored with direct visual control and digital subtraction angiographic imaging techniques, including road-mapping. When no radiological equipment was available, the whole training procedure could be performed under direct observation because these models were transparent. Medical devices including platinum coils and stents were successfully implanted in the model under stable conditions (figure 2,4). Through these procedures, the traineess could have an easy understanding of medical devices and techniques.
Clinical Practice
In the clinical practice, the residents could be an assistant of the whole interventional procedures at their first year, be an operator of the embolization of the exteranal carotid artery territory at their second year, and be an operator of the intracranial procedures at their third year. From 2000, they have started JSIN Board Certification System in Japan. At the beginning, the society elected 48 "Board Certified Instructors" (consulting specialist), and almost 100 "Board Certified Specialists" were selected after strict board examination at the end of August 2002.
Our endovascular team included two senior staff (KS and KT; both are Board Certified Instructor) and three residents (trainee). Recently, we have had150-200 interventional procedures every year. Thus one resident can expect about 100 cases per year. The qualification of a Board Certified Specialist requires that the applicant must have experienced more than 100 cases for four years. So our residents can have enough case materials to qualify the board examination.
Discussion
Recently, neurovascular intervention has rapidly become widespread. For example, endovascular treatment for cerebral aneurysms has played an important roll in the neurosurgical field in a only few years since the introduction of the Guglielmi detachable coil (GDC) 1. Training in this technique requires a steep learning curve, with the most improvement seen during the first 50-100 cases 6,9. Similar observations have been made in the other fields of neurovascular intervention. However, there are fewer interventional cases that one can have in Japanese institutes comparing with that of in the State’s or Europian centers. Thus, systematic training of young endovascular neurosurgeons is very important issue. Adequate training can help for inexperienced surgeons to decrease the learning curve. As above mentioned, we had kept our training system for the young neurosurgeons from 1980’s. Recently, in addition to the daily clinical practice, we introduced in vitro vascular model as an initial training tool. Becouse even for experienced endovascular neurosurgeons, stable in vitro conditions in accurate anatomical structures provide a good opportunity for training colleagues or testing new devices 4-7.
In vitro vascular models are also useful for the preclinical evaluation of medical devices and implants. The models are anatomically accurate and provide various vascular lesions for the trainees. The use of models allows the simulation of a stable endovascular environment and the introduction of circulation circuits allows the simulation of variable flow conditions. The possibility of controlling these parameters can optimize preclinical evaluation by engineers and medical doctors, consequently limiting the use of animal models, in which the simulation of biological aspects is mandatory. The transparency of the models allows for direct visual control of endovascular procedures and for insight into the mechanics of medical device implantation. Trainees quickly understand the influence of manipulating such devices 4-7.
Conclusions
We introduced our training tools and system of neurovascular intervention. We believe that our training system using in vitro vascular model as an initial training and clinical practice is very useful for the residents who are going to be a Board Certified Specialist of JSIN. We hope that this paper may help other endovascular team for establishing good endovascular training system.
References
- 1.Guglielmi G, Vinuela F, et al. Electrothrombosis of saccular aneurysms via endovascular approach. Part 2: Preliminary clinical experience. J Neurosurg. 1991;75:8–14. doi: 10.3171/jns.1991.75.1.0008. [DOI] [PubMed] [Google Scholar]
- 2.Taki W, Gotoh K, et al. The first specialist qualification examination of the Japanese Society of Intravascular Neurosurgery (JSIN) Interventional Neuroradiology. 2002;8:343–345. doi: 10.1177/159101990200800403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sugiu K, Tokunaga K, et al. Training in neurovascular intervention. [Article in Japanese] No Shinkei Geka. 2002;30:1231–1237. [PubMed] [Google Scholar]
- 4.Gailloud P, Pray JR, et al. An in vitro anatomic model of the human cerebral arteries with saccular arterial aneurysms. Surg Radiol Anat. 1997;19:119–121. [PubMed] [Google Scholar]
- 5.Gailloud P, Muster M, et al. In vitro models of intracranial arteriovenous fistulas for evaluation of new endovascular treatment materials. Am J Neuroradiol. 1999;20:291–295. [PMC free article] [PubMed] [Google Scholar]
- 6.Piotin M, Mandai S, et al. Dense packing of cerebral aneurysms: An in vitro study with detachable platinum coils. Am J Neuroradiol. 2000;21:757–760. [PMC free article] [PubMed] [Google Scholar]
- 7.Sugiu K, Martin JB, et al. Artificial cerebral aneurysm model for medical testing, training, and research. Neurol Med Chir (Tokyo) 2003;43:69–73. doi: 10.2176/nmc.43.69. [DOI] [PubMed] [Google Scholar]
- 8.Kerber CW, Heilman CB. Flow dynamics in the human carotid artery: 1. Preliminary observations using a transparent elastic model. Am J Neuroradiol. 1992;13:173–180. [PMC free article] [PubMed] [Google Scholar]
- 9.Malisch TW, Guglielmi G, et al. Intracranial aneurysms treated with the Guglielmi detachable coil: Midterm clinical results in a consecutive series of 100 patients. J Neurosurg. 1997;87:176–183. doi: 10.3171/jns.1997.87.2.0176. [DOI] [PubMed] [Google Scholar]