Summary
We have been using the Guglielmi detachable coils (GDC) since 1997 as one choice of cerebral aneurysm treatment. We have, at the present time, two effective radical treatment methods for acutely ruptured cerebral aneurysms, GDC embolization and conventional surgical aneurysmal neck clipping. There ensued questions about the cost and efficacy of the two strategies. Retrospective analysis was done on a GDC group and a clipping group, with each twenty consecutive patients. The features of the GDC group patients were higher age, and poorer Hunt and Kosnik grades than the other group. All MCA aneurysms were treated with surgical neck clipping, while all the posterior circulation aneurysms were embolized with GDC.
Based on the Japanese Medical Insurance and Payment System, 477,890 points (1 point = ¥10) as a mean was required with the GDC group, and 456,084 points with the neck clipping group, showing no significant difference between the two groups. In the GDC group, the cost of the implanted medical device seemed to raise the total medical expense.
At present, the GDC embolization is the preferred choice of strategies in acutely ruptured cerebral aneurysms, and its preference increases in the surgically difficult cases, very old, or poor grade patients, and in various complicated cases. And, the GDC embolization seems to be satisfactory from the medico-financial viewpoint.
Key words: GDC, ruptured cerebral aneurysm, medical insurance, medical expenses
Introduction
Since 1997, we have been able to use Guglielmi detachable coils (GDC) for treatment in Japan. This has changed our therapeutic strategy for ruptured cerebral aneurysms. Surgical neck clipping had been the only method of radical treatment before the appearance of GDC. But now we can choose the appropriate treatment for acutely ruptured aneurysms from two therapeutic methods in accordance with the condition of patients and their cerebral aneurysms.
Until now, many studies have emphasized the merits and efficacy of GDC embolization compared with surgical neck clipping from a medical point of view. Some studies have pointed out weak the points of GDC embolization compared with surgical neck clipping, such as indistinctness of long-term results, requiring several angiographical follow-ups and others. The ISAT study made an impact on these discussions in 2002, and GDC embolization became known to a wide public on equal terms with surgical neck clipping 1.
We propose that a widely-used treatment should be evaluated not only in clinical aspects but also in medico-financial aspects. However, few studies have discussed the cost and efficacy of GDC embolization for cerebral aneurysms from a medico-financial view point 2-4.
In this study, we surveyed the cost and efficacy of GDC embolization for acutely ruptured cerebral aneurysms in comparison with surgical neck clipping from a medico-financial viewpoint.
Patients and Methods
The subjects in this investigation were forty patients with acutely ruptured cerebral aneurysms who were treated within seventy two hours from onset in our hospital before June, 2002. The GDC group contained twenty patients with acutely ruptured cerebral aneurysm treated with GDC. Likewise, the clipping group included twenty patients treated by surgical neck clipping. We excluded from the study two patients who had multiple cerebral aneurysms and who were treated by both therapeutic methods. We also excluded one patient treated with GDC who moved to another hospital soon after embolization. We compared the two groups on the basis of their clinical backgrounds (age, Hunt and Kosnik grade, location of aneurysms, and other medical conditions) and the medical expenses incurred for medical treatment fees and hospital charges, based on the Japanese medical insurance and payment system.
Standard Policy for the Choice of Treatment
During the research period, our first choice of treatment for acutely ruptured cerebral aneurysms was surgical neck clipping. The reasons for the choice of GDC embolization were advanced aged patients, poor grade patients, locations of aneurysms and their medical conditions such as severe liver dysfunction, severe renal failure, heart failure and neurogenic lung edema.
Standard Supportive Therapy
To several patients in the GDC group, lumbar and/or ventricular drainage was introduced, and urokinase was intrathecally administrated. To almost all patients in the clipping group, cisternal and ventricular drainage were introduced, continuous irrigation using artificial cerebrospinal fluid with ascorbic acid was performed. External decompression was done to some patients in the latter group. Also for some patients in each group, a V-P shunt operation was performed.
Results
1) Age
The mean age of the patients in the GDC group was 62.0 year-old (range; 42-81 year-old, SD; 11.1). The mean age of the patients in the clipping group was 55.2 year-old (range; 31-68 year-old, SD; 8.31). It is thus significant that the patients in the GDC group were older than those in the other group. Six patients (30%) in the GDC group were more than seventy-year-old.
2) Hunt and Kosnik Grade
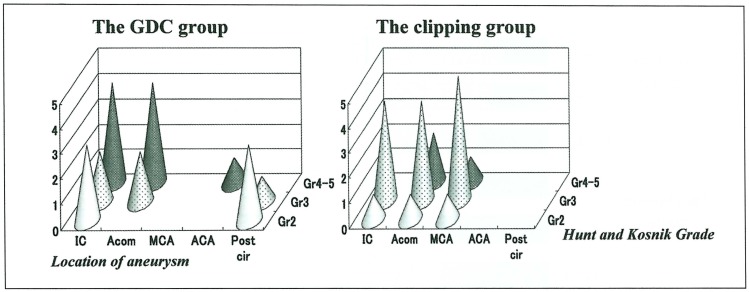
Nine patients in the GDC group (45%) fell under grade 4 and 5 of the Hunt and Kosnik grades. However, only three patients in the clipping group (15%) fell under Hunt and Kosnik grade 4. The patients in the GDC group were clearly more serious than the patients in the clipping group (figure 1).
Figure 1.
Patients' clinical back ground; Hunt and Kosnik grade. The GDC group included poor-grade patients (nine of twenty, 45%).
3) Location of Aneurysms
Figure 2 shows that all aneurysms existing in the posterior circulation were treated by GDC embolization. All middle cerebral artery aneurysms were treated by surgical neck clipping. In the other anterior circulation aneurysms, poor grade patients were treated by GDC embolization (figure 2).
Figure 2.
Patients' clinical background; Locations of ruptured cerebral aneurysms and Hunt and Kosnik grades. All posterior circulation aneurysms were treated with GDC. All middle cerebral artery aneurysms were treated by surgical neck clipping. The other cerebral aneurysms were treated by one of two methods because of age, severity, medical conditions, and other reasons.
4) Other Medical Conditions
Two patients (10%) in the GDC group suffered severe renal failure undergoing artificial haemodialysis.
5) Medical Expenses
A comparison of the total medical expenses was calculated by the accounts of medical treatment based on the Japanese medical insurance and payment system. The mean value of the GDC group was 477,890 points (1 point equals ¥ 10). The mean value of the clipping group was 456,084 points. Thus, there was no significant difference between the two groups. The technical fee for operations in the clipping group was more expensive. Medical devices used in operations such as GDC, microcatheters and others raised total medical expenses in the GDC group (figure 3).
Figure 3.
Medical expenses based on the Japanese medical insurance and payment system. There was no significant difference between the two groups in the total medical expenses. In the GDC group, the cost of medical devices was marked. The technical fees of procedures were more expensive in the clipping group.
In the correlations between the total medical expenses and the Hunt and Kosnik grades, the total medical expenses increased proportionally with the severity of the condition of the patients. However, the total medical expenses increased more gradually in the GDC group.
In patients belonging to Hunt and Kosnik grades 2 and 3, the medical devices, especially GDC, increased the medical expenses which were accompanied with the size of cerebral aneurysm in the GDC group. This occurred regardless of location of the cerebral aneurysm or severity of the patient. But in patients belonging to Hunt and Kosnik grades 4 and 5, primary brain damage and operative invasions increased the medical expenses especially in the clipping group (figure 4).
Figure 4.
Correlations between the medical expenses and the Hunt and Kosnik grades. The total medical expenses increased proportionally with the severity of the condition of patients. But, those of the GDC group increased more gradually than those of the clipping
6) Hospitalized Days
With regard to the days of hospitalization required, the GDC group was better than the clipping group in any grade of Hunt and Kosnik grade. This was especially true in patients with poor Hunt and Kosnik grades (figure 5).
Figure 5.
Hospitalized days. The GDC group was better than the clipping group in any grade of Hunt and Kosnik grade.
Discussion
In this study, we chose GDC embolization for treatment of ruptured cerebral aneurysms for advanced-age patients, poor grade patients, and on the basis of locations of cerebral aneurysms, and other medical conditions. Therefore, the GDC group included aged patients over seventy (30%), patients with serious renal insufficiency who required hemodialysis (10%), patients with cerebral aneurysms located in the posterior circulation (20%), and poor-graded patients (45%). Regardless of the disadvantageous clinical backgrounds of the patients, the cost and efficacy of the GDC group was sufficiently favorable in comparison with the clipping group. This suggests that the GDC embolization should be the first choice of treatment for disadvantageous patients with ruptured cerebral aneurysms.
The medical environment of GDC embolization is changing every year. The report from the ISAT collaborative group shows that the outcomes of patients treated with GDC was better than that of patients treated by surgical neck clipping 1. New devices and new techniques for endovascular surgery are being developed regularly 5-7.
According to the revised medical fee schedule published in April, 2002 by the government, the technical fee for endovascular surgery has been raised from 31,200 points to 34,300 points. In addition, the technical fee for surgical neck clipping has been reduced substantially because of the institutional standard which is regulated by yearly numbers of the cases treated by surgical neck clipping in any institution. If the yearly number of surgical neck clippings in an institution is below fifty, the technical fee for surgical neck clipping reduces to 70% (from 77,100 points to 50,190 points). But, the institutional standard of endovascular surgery (not only aneurysmal embolization) was regulated ten procedures in a year.
These factors may increase the advantage of endovascular treatment for acutely ruptured cerebral aneurysms. It is expected that the medical and social environment surrounding GDC embolization may change rapidly. In the near future, therefore we must reevaluate the medicofinancial efficiency of both treatments for acutely ruptured cerebral aneurysms.
Conclusions
GDC embolization is approximately the same as surgical neck clipping in the total medical expenses of treatment for ruptured cerebral aneurysms. In this study, despite the disadvantageous clinical backgrounds of the patients, the cost and efficacy of GDC embolization is demonstrated favorably.
References
- 1.International Subarachnoid Aneurysm Trial (ISAT) Collaborate Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet. 2002;360:1267–1274. doi: 10.1016/s0140-6736(02)11314-6. [DOI] [PubMed] [Google Scholar]
- 2.Sturaitis MK, Rinne J, et al. Impact of Guglielmi detachable coils on outcomes of patients with intracranial aneurysms treated by a multidisciplinary team at a single institution. J Neurosurg. 2000;93(4):719–21. doi: 10.3171/jns.2000.93.4.0569. [DOI] [PubMed] [Google Scholar]
- 3.Murayama Y, Vinuela F, et al. Embolization of incidental cerebral aneurysms by using the Guglielmi detachable coil system. J Neurosurg. 1999;90(2):207–214. doi: 10.3171/jns.1999.90.2.0207. [DOI] [PubMed] [Google Scholar]
- 4.Kallmes DF, Kallmes MH, et al. Guglielmi detachable coil embolization for unruptured aneurysms in nonsurgical candidates: a cost-effectiveness exploration. Am J Neuroradiol. 1998;19(1):167–176. [PMC free article] [PubMed] [Google Scholar]
- 5.Sewa S, Onishi K, et al. The Development for Polymer Actuator Active Catheter System. Interventional Neuroradiology. 2001;7(Suppl 1):115–123. doi: 10.1177/15910199010070S117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Negoro M, Tanimoto M, et al. An Intelligent Catheter System Robotic Controlled Catheter System. Interventional Neuroradiology. 2001;7(Suppl 1):111–113. doi: 10.1177/15910199010070S116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shimozuru T, Kamezawa T, et al. Hydroxyapatite Coating of Detachable Coils for Endovascular Occlusion of Experimental Aneurysm. Interventional Neuroradiology. 2001;7(Suppl 1):105–110. doi: 10.1177/15910199010070S115. [DOI] [PMC free article] [PubMed] [Google Scholar]