Summary
Of 175 patients with 181 aneurysms initially treated with Guglielmi Detachable Coils (GDC), 25 were retreated. All retreatments except one were performed on previously ruptured aneurysms. Thirteen aneurysms were retreated because of recurrence, and 12 aneurysms were retreated to complete initial insufficient embolization. Sixteen patients underwent re-embolization and 9 patients were operated upon surgically. No complications related to the retreatment were experienced. We consider that repeat embolization should be attempted before considering surgical treatment in case that additional therapy is required. However, it is difficult to retreat aneurysms having wide necks. In regard to surgical clipping, aneurysms without a coil in the neck are easier to treat with primary clipping, whereas aneurysms with a coil mass in the neck are difficult to surgical clip. We have never used temporary clipping and coil extraction if the distance between the coil and the parent artery was wider than 2 mm. Emerging new embolic agents or devices and technical improvement might decrease the need for retreatment and increase long-term efficacy after endovascular treatment.
Key words: Cerebral aneurysm, Guglielmi detachable coil, embolization, retreatment
Introduction
A number of publications have documented the favorable results of endovascular treatments of cerebral aneurysms using the Guglielmi Detachable Coil (GDC) system 1-4. Furthermore, a randomized study comparing endovascular and surgical managements of ruptured aneurysms has shown significantly improved outcomes in patients treated with the GDC system 5. However, we often encounter recurrences of aneurysms or incomplete initial treatments after GDC embolization, which require repeats of surgical or endovascular treatment 6. We report cases which had been initially treated using the GDC system and retreated by embolization or surgical clipping.
Material and Methods
Between 1997 and 2001, 181 cerebral aneu rysms which includes 131 ruptured and 50 unruptured ones in 175 patients were treated by endosaccular coil placement using the GDC system at the Department of Neurosurgery, Mito National Hospital and the University of Tsukuba. Seventy of the patients were men and 105 were women, with a mean age of 58.9 years (range, 30-93 years). In each patient who has residual or recurrent aneurysms, the respective indications for neurosurgical or endovascular retreatment were discussed, taking into consideration the patient’s age and the morphological and topographical features of the aneurysm. Consequently, 25 patients (14%) were retreated after GDC embolization during the same period. We analyzed these cases retrospectively.
Results
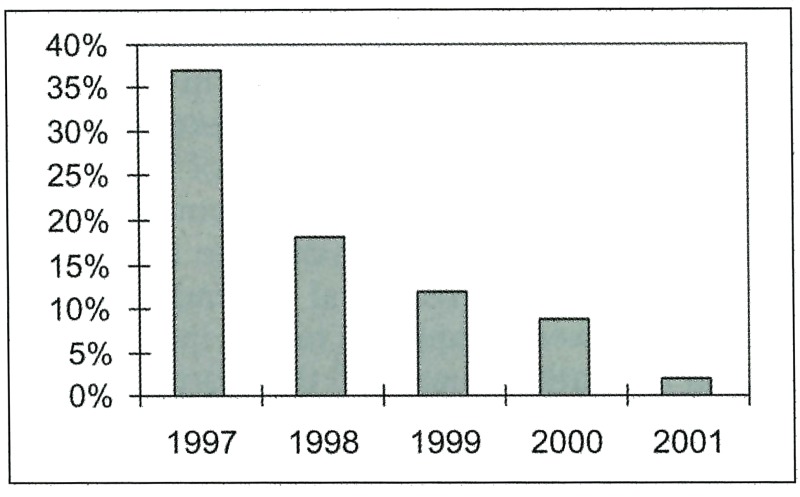
Twelve patients were men and 13 were women, with a mean age of 52.7 years (range, 31-73 years). Mean duration between initial treatment and retreatment was 4.4 months (range, 1 week-19 months). Table 1 shows the yearly transition of the incidence of retreatment, indicating a decrease over the years. Concerning the condition of aneurysms at the initial treatment, 24 aneurysms were ruptured and one was unruptured. Thirteen aneurysms were retreated because of recurrence, which showed that sufficient occlusion in the initial treatment subsequently led to aneurysmal opacification due to coil compaction, coil migration, recanalization of intraaneurysmal clot, or aneurysmal enlargement. Twelve aneurysms were retreated to complete the initial insufficient embolization. Sixteen patients underwent reembolization and nine patients were operated upon surgically. All retreated aneurysms were totally or near totally obliterated. No complications related to the retreatment were experienced.
Table 1.
Frequency of Retreatments
 |
Case 1
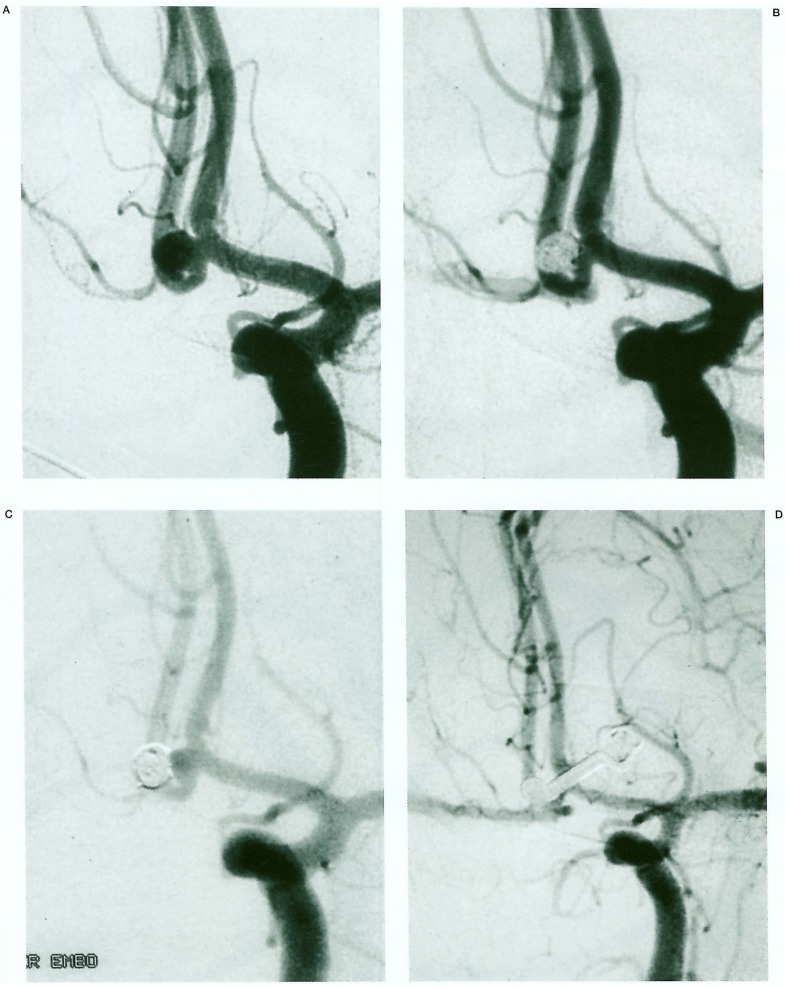
A 41-year-old man presented with a Hunt and Hess Grade II subarachnoid haemorrhage due to a rupture of a 4 mm anterior communicating artery aneurysm (figure 1A). GDC embolization was performed on day 1. The aneurysm was occluded sufficiently with 3 GDC 10 coils whose total length was 24 cm (figure 1B). The patient suffered no significant neurological sequelae. Follow-up angiography performed three months later revealed coil compaction with a small amount of fundal opacification considered to be difficult for reembolization because the neck was relatively large (figure 1C). The residual neck of the aneurysm was clipped easily without coil extraction (figure 1D).
Figure 1.
Left internal carotid injection demonstrates an anterior communicating artery aneurysm (A). The aneurysm was occluded using the GDC 10 system on day 1 (B). Follow-up angiogram performed three months later reveals aneurysmal recurrence (C). Surgical clipping was performed on the residual aneurysmal neck (D).
Case 2
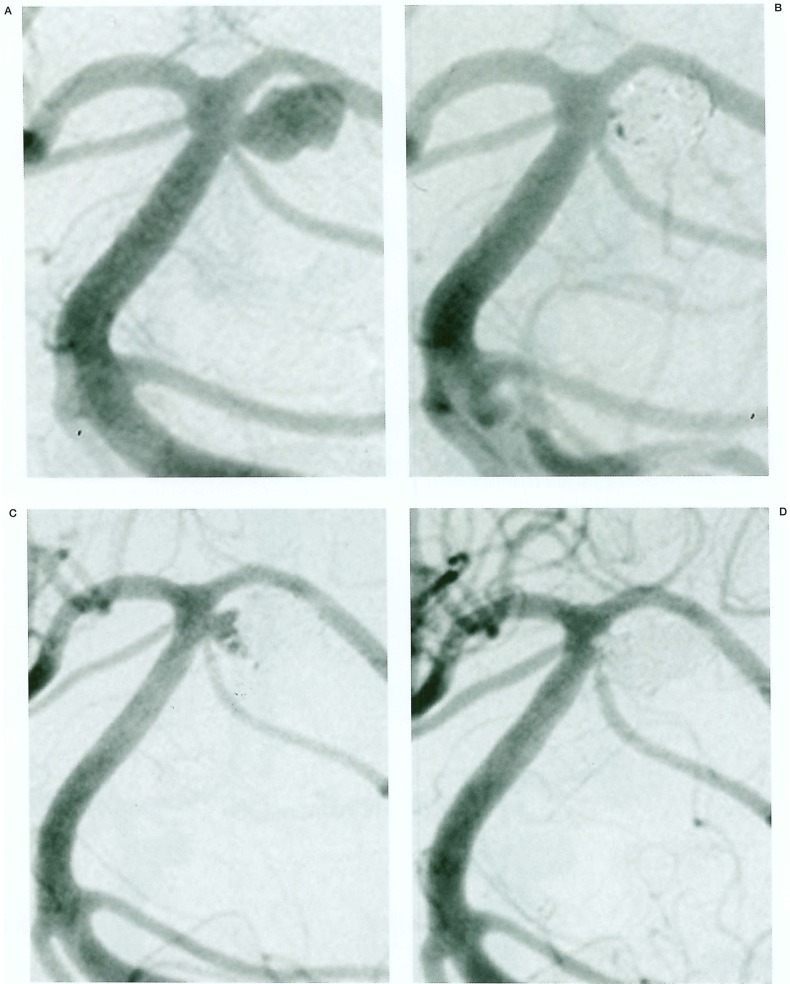
A 63-year-old woman presented with a Hunt and Hess Grade IV subarachnoid haemorrhage secondary to a 6 mm left superior cerebellar artery aneurysm (figure 2A). The patient underwent GDC embolization on day 5. A small residual neck was evident after the embolization using 6 GDC10 coils whose total length was 46 cm (figure 2B). Post embolization course was uneventful and the patient’s neurological condition recovered completely. Angiographic follow-up six months later demonstrated significant recurrent aneurysm due to coil compaction (figure 2C). Repeat embolization was performed, resulting in complete occlusion using small 2 GDC10 coils (figure 2D).
Figure 2.
Left vertebral artery injection demonstrates left superior cerebellar artery aneurysm (A). The aneurysm was occluded using GDC10 coils on day 5 (B). Follow-up angiogram obtained 6 months later shows aneurysmal recurrence (C). Reembolization was performed. The additional GDC coils occluded the residual aneurysm (D).
Discussion
Residual filling of the lumen or neck region is more frequent after coil embolization, even after complete initial occlusion, than after surgical clipping. Byrne et Al reported from their experience of coil embolization for 317 patients presenting with aneurysmal subarachnoid haemorrhage that the incidences of rebleeding in patients with unstable aneurysms after coil embolization was 7.9% and those of stable occlusions was 0.4%3. This data provides reassurance that complete occlusion is protective, and does not suggest that regrowth and rebleeding are inevitable consequences of incomplete occlusion. Therefore, aneurysm recurrences or incomplete initial treatments require retreatment to prevent the rupture of unruptured aneurysms and the rerupture of ruptured ones.
The incidence of retreatment after embolization varies. Byrne et Al reported 13 retreatments within 317 aneurysms (4.1%) including 11 reembolizations and two surgical clippings 3. Horowitz et Al reported nine aneurysms requiring additional therapy of 125 aneurysms that underwent embolization (6.4%) including four reembolizations and five surgical clippings 7. Asgari et Al described 17 retreatments of 130 aneurysms (13%) including 12 reembolizations and five surgical clippings 8. In our series, we have retreated 25 aneurysms of 181 initially embolized aneurysms (14%) by means of 16 reembolizations and 9 surgical clipping. The incidence of retreatment decreased over the years because of technical improvements and new devices such as the balloon assisted technique 9 and 3D GDCs. In our cases, all retreated aneurysms except one were ruptured aneurysms. Reymond et Al also mentioned that angiographic recurrence after the endovascular treatment of aneurysms were more common in large, ruptured lesions with suboptimal initial results and will be detected more frequently with long-term follow-up studies 6.
In the literature, it has been recommended that repeat embolization should be attempted before considering surgical treatment in cases in which additional therapy was required because the surgical treatment of recurrent lesions is often difficult 7,8,10. We also prefer to reembolize residual aneurysms in cases of coil compaction with sufficient space for small additional coils and a compact neck.
In regard to surgical clipping, aneurysms without a coil in the neck are relatively easy to treat by means of primary clipping, whereas aneurysms with a coil mass in the neck are difficult to surgically clipping 10,11. Horowitz et Al assumed that coil extraction would be necessary in order to obliterate the lesion with the use of temporary occlusion 7. Meanwhile, Gurian et Al recommended that observation of such lesions might be preferable to allow for coil compaction and subsequent coiling or clip application 10. Asgari et Al reported that temporary clipping was not necessary in cases in which the patent portion at the aneurysm neck was sufficiently large (>2 mm) 8. We have never used temporary clipping and coil extraction if the distance between the coil and the parent artery was wider than 2 mm.
Retreatment is frequent after coil embolization as compared to surgical clipping. However, all retreatments including reembolizations and surgical clipping were performed without any adverse events in our cases. In the context of acutely ruptured lesions, endovascular treatment has proven to improve clinical outcome 1 year after treatment compared with surgical treatment 8. This benefit of the endovascular approach should not be negated. Furthermore, emerging new embolic agents or devices might increase long-term efficacy.
Conclusions
Residual or recurrent aneurysms after embolization require retreatments. We have performed 25 retreatments without any complications in 181 previously embolized aneurysms. Repeat embolizations should be attempted before considering surgical options. Surgical clipping could be performed if the neck was sufficiently large (>2 mm) without temporary occlusion or coil extraction.
References
- 1.Viñuela F, Duckwiler G, et al. Guglielmi detachable coil embolization of acute intracranial aneurysm: perioperative anatomical and clinical outcome in 403 patients. J Neurosurg. 1997;86:475–482. doi: 10.3171/jns.1997.86.3.0475. [DOI] [PubMed] [Google Scholar]
- 2.Raymond J, Roy D. Safety and efficacy of endovascular treatment of acutely ruptured aneurysms. Neurosurgery. 1997;41:1235–1245. doi: 10.1097/00006123-199712000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Byrne JV, Sohn MJ, et al. Five-year experience in using coil embolization for ruptured intracranial aneurysms: outcomes and incidence of late rebleeding. J Neurosurg. 1999;90:656–663. doi: 10.3171/jns.1999.90.4.0656. [DOI] [PubMed] [Google Scholar]
- 4.Murayama Y, Nien YL, et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years’ experience. J Neurosurg. 2003;98:959–966. doi: 10.3171/jns.2003.98.5.0959. [DOI] [PubMed] [Google Scholar]
- 5.Molyneux A. International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group: International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002;360:1267–1274. doi: 10.1016/s0140-6736(02)11314-6. [DOI] [PubMed] [Google Scholar]
- 6.Raymond J, Guilbert F, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34:1398–1403. doi: 10.1161/01.STR.0000073841.88563.E9. [DOI] [PubMed] [Google Scholar]
- 7.Horowitz M, Purdy P, et al. Aneurysm retreatment after Guglielmi detachable coil and nondetachable coil embolization: report of nine cases and review of the literature. Neurosurgery. 1999;44:712–719. doi: 10.1097/00006123-199904000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Asgari S, Doerfler A, et al. Complementary management of partially occluded aneurysms by using surgical or endovascular therapy. J Neurosurg. 2002;97:843–850. doi: 10.3171/jns.2002.97.4.0843. [DOI] [PubMed] [Google Scholar]
- 9.Moret J, Cognard C, et al. La technique de reconstruction dans le traitement des aneurisms intracraniens a collet large. Resultant angiographiques et cliniques a long terme. A propos de 56 cas. J Neuroradiol. 1997;24:30–44. [PubMed] [Google Scholar]
- 10.Gurian JH, Maratin NA, et al. Neurosurgical management of cerebral aneurysms following unsuccessful or incomplete endovascular embolization. J Neurosurg. 1995;83:843–853. doi: 10.3171/jns.1995.83.5.0843. [DOI] [PubMed] [Google Scholar]
- 11.Civit T, Auque J, et al. Aneurysm clipping after endovascular treatment with coils: a report of eight patients. Neurosurgery. 1996;38:955–960. doi: 10.1097/00006123-199605000-00021. [DOI] [PubMed] [Google Scholar]