Abstract
The aims of the present study were to develop and validate a new obesity-specific, parent-proxy measure of health-related quality of life (HRQOL), Sizing Them Up. Participants included 220 obese youth (Mage = 11.6 years, 68% female, 53% African American, MBMI = 36.7) and their primary caregivers (88% mothers). Primary caregivers completed a demographics questionnaire and two HRQOL measures: Sizing Them Up (obesity-specific) and PedsQL (generic). Youth height and weight were measured. Psychometric evaluation of Sizing Them Up was completed by conducting a factor analysis and determining internal consistency coefficients, test–retest reliability, convergent and discriminant validity, predictive validity, responsiveness to change, and minimal clinically important difference (MCID) scores. Sizing Them Up is a 22-item measure with six scales (i.e., Emotional Functioning, Physical Functioning, Teasing/Marginalization, Positive Social Attributes, Mealtime Challenges, and School Functioning) that account for 66% of the variance. The measure also includes an Adolescent Developmental Adaptation module. Sizing Them Up had internal consistency coefficients ranging from 0.59 to 0.91 and test–retest reliabilities ranging from 0.57 to 0.80. Validity was demonstrated by significant relations between a majority of Sizing Them Up scales and BMI z-scores. Sizing Them Up also demonstrated good convergent validity with other HRQOL measures and responsiveness to change related to weight loss for adolescents who had undergone bariatric surgery. Overall, Sizing Them Up is a reliable and valid parent-proxy measure of obesity-specific HRQOL that can be used in both clinical and research settings.
INTRODUCTION
The measurement of pediatric health-related quality of life (HRQOL) has gained significant attention in the past decade (1) with rigorous standards developed regarding the development and psychometric validation of HRQOL measures (2,3). HRQOL is defined as a multidimensional construct broadly assessing both physical and psychosocial functioning (4). It has been recognized as an important patient-reported outcome by agencies such as the Food and Drug Administration (5) and Centers for Disease Control and Prevention (6). HRQOL measures are now widely used for several reasons: (i) to describe the impact of an illness or condition on a patient’s daily functioning, (ii) as primary and secondary endpoints in clinical trials, (iii) evaluation of new pharmaceutical and surgical treatments, (iv) as an aid in clinical decision making, and (v) evaluation of clinical care and outcome. Tremendous growth has occurred in the development of both generic and disease-specific measures of HRQOL for children in the past ten years (1). While generic measures allow for cross-disease comparison, disease-specific measures identify issues that are most salient for a particular group of patients. However, there are several pediatric conditions for which disease-specific instruments are lacking, including obesity.
Why is it important to measure obesity-specific HRQOL? First, overweight and obesity affect 16% of children and adolescents in the United States (7), with an estimated 4% of children and adolescents meeting criteria for extreme obesity (BMI ≥ 40 kg/m2) (8). There is overwhelming literature to suggest that both the negative medical and psychosocial consequences of obesity are substantial. This warrants the need for reliable and valid patient- and parent-proxy-reported outcome measures, such as HRQOL. Second, new treatments have been developed for obesity that require further evaluation, including both pharmacological medications, such as sibutramine and orlistat (9), and surgical interventions (10,11). Third, obesity is one of the few pediatric conditions associated with significant medical comorbidities (e.g., endocrine, pulmonary, cardiac, reproductive, and skeletal disorders) that may cumulatively negatively affect the daily functioning for youth with these conditions. Finally, HRQOL measures go beyond conventional indices such as BMI. Although BMI represents an important medical indicator of health, it does not adequately capture the patient’s ability to function in his or her daily life. Overall, there is a need to develop and validate an obesity-specific measure of HRQOL.
To date, there is only one weight-specific HRQOL measure for adolescents (12) but no parallel forms for younger school-age children or parent-proxy measures. Parent-proxy measures, in conjunction with self-report measures, provide a broader viewpoint of the child’s HRQOL (1,13). For example, Ingerski and colleagues found discrepancies between child and parent-proxy reports, with parents reporting significantly worse generic HRQOL (14). Because parents play a key role in the initiation of both medical and psychosocial services, their vantage point is both informative and critical (15–17).
Previous studies examining HRQOL in obese youth utilizing generic measures (e.g., PedsQL; (18)) have found that overweight and obese children suffer from poor HRQOL across several domains of functioning compared to other chronic illness groups and normative values (14,19–23). For example, Schwimmer and colleagues (19) found that overweight and obese youth demonstrate HRQOL similar to children with cancer. These studies highlight the primary strength of generic measures, which is cross-disease comparison. However, generic measures lack understanding of the issues that are most salient to obese youth, such as weight-related stigmatization, body esteem, and physical discomfort related to their weight. For example, researchers have found that relative to a generic measure, an adult weight–specific measure was more sensitive to change and better represented HRQOL (24–26).
The aims of the present study were to describe the development and validation of a parent-proxy, obesity-specific HRQOL measure for parents of children 5–18 years of age called Sizing Them Up. The primary objective was to assess the reliability and validity of Sizing Them Up. Specifically, it was expected that Sizing Them Up would have (i) internally consistent factors (e.g., Cronbach’s α >0.70), (ii) good test–retest reliability, (iii) strong associations with BMI (construct validity), (iv) good agreement with similar scales on generic HRQOL measures (convergent validity), and (v) responsiveness to change. Other secondary study objectives included calculating the minimal clinically important difference (MCID) scores and examining age, gender, and race differences on Sizing Them Up.
METHODS AND PROCEDURES
Participants and procedures
Study participants included 220 obese children and their parents seeking treatment through hospital-based pediatric weight management programs, including a behavioral (n = 204) and bariatric surgery (n = 16) program. The behavioral treatment program requires a BMI ≥95th percentile and excludes youth with genetic syndromes associated with obesity and developmental disabilities. The bariatric surgery program adheres to adolescent patient selection guidelines as previously described (10). Study inclusion criteria included (i) patients 5–18 years of age (behavioral treatment) or 13–18 years of age (bariatric surgery), (ii) absence of developmental disability, and (iii) willingness to comply with study procedures and provision of written informed consent/assent.
Phase 1—scale development and validation
All participants who attended a prescreening visit for the behavioral treatment program between August 2004 and January 2007 received information letters and brochures describing the study about HRQOL in youth presenting for weight management. These participants were subsequently approached for recruitment and participation during this medical screening visit at the General Clinical Research Center or initial clinical assessment at Cincinnati Children’s Hospital Medical Center. Candidates approved for bariatric surgery were approached prior to surgery and data were collected during the week prior to surgery. Follow-up data were collected ~6 months after surgery during a scheduled study visit. Of the 239 potential participants, 19 eligible participants were not included for the following reasons: (i) eight parents declined to participate (seven behavioral treatment, one bariatric surgery), (ii) six participants were one of two siblings, (iii) one participant became sick during questionnaire administration, (iv) two participants had behavioral issues making administration difficult and invalid, and (v) two participants had difficulty understanding the questionnaires due to reading difficulties and English being a second language. A summary of the demographic characteristics of participants are presented in Table 1.
Table 1.
Demographic data on youth with obesity (n = 220)
| N | Mean (s.d.) | % | |
|---|---|---|---|
| Age | 11.6 (3.3) | ||
| Sex | |||
| Girls | 150 | 68 | |
| Boys | 70 | 32 | |
| Race | |||
| White | 92 | 42 | |
| African American | 117 | 53 | |
| Biracial/other | 10 | 4 | |
| Native American | 1 | 1 | |
| Anthropometric data | |||
| BMI | 36.7 (11.6) | ||
| Standardized BMI (zBMI) | 2.6 (0.37) | ||
| Participating caregiver | |||
| Mother | 194 | 88 | |
| Father | 6 | 3 | |
| Grandmother | 14 | 6 | |
| Other | 6 | 3 | |
| Marital status | |||
| Married | 80 | 37 | |
| Separated/divorced | 51 | 23 | |
| Single/never married | 82 | 37 | |
| Widowed | 7 | 3 | |
| Duncan scorea | 37.8 (20.1) |
Based upon Duncan TSEI2 for head of household, a measure of occupational attainment. The mean TSEI2 score reflects occupations such as metal workers, truck drivers, food services supervisors, sales worker.
All personnel were trained to recruit and screen participants, administer consent forms, and instruct or administer questionnaires to both children and their parents. Parents of participants were asked to complete several questionnaires. For the purpose of the current study, they completed a demographic form, parent-proxy PedsQL, and newly developed Sizing Them Up questionnaire (described below). Children completed one of two obesity-specific HRQOL measures: (i) Sizing Me Up for school-aged children (5–13 years of age), which is currently being validated and not reported in the current paper; or (ii) Impact of Weight on QOL-Kids (IWQOL-Kids) for adolescents (aged 14 years and older). Instructions for each measure were read to each child and parent; however, in general, the measures were each completed individually. The child’s weight and height were also obtained. All participants were compensated for their time. The protocols were approved by the Cincinnati Children’s Hospital Medical Center Institutional Review Board.
Phase 2—test–retest reliability
Participants recruited from August 2005 to January 2007 were approached for phase 2 of the study. In order to assess test–retest reliability, they were asked to complete Sizing Them Up questionnaire in ~2–4 weeks time after completing the first set of questionnaires. Research assistants administered questionnaires at the family’s home or a mutually agreed upon location. Parents completed Sizing Them Up questionnaire and children completed either Sizing Me Up (ages 5–13 years) or the IWQOL-Kids (ages 14–18 years). Height and weight measurements were taken at this time to ensure no significant changes occurred in BMI from phase 1, which would compromise stability over time. Overall, 118 children were approached for phase 2, of which 18 potential participants either declined (n = 9) or consented but had difficulties scheduling (n = 9). In addition, 3 participants had significant changes in zBMI (standardized BMI) (zBMI change of >0.10) between phase 1 and phase 2, resulting in a final phase 2 sample of 97 participants.
Responsiveness to change
Most parents of adolescents undergoing bariatric surgery (n = 14 of 16) completed Sizing Them Up questionnaire within 14 days prior to surgery as well as 6-months after surgery to determine the responsiveness of the measure to weight loss.
Measures
Demographic background questionnaire
Mothers completed a background questionnaire documenting the child’s race/ethnicity, parental marital status, and parental level of education. Adequate data were available to calculate the Revised Duncan (TSEI2; (27)) for each family, which is an occupation-based measure of socioeconomic status (28).
Sizing Them Up
This instrument was developed by the current investigators to assess parent-proxy reports of obesity-specific HRQOL for youth aged 5–18 years. Item content for the original 35-item measure was based on the published child/adolescent obesity and HRQOL literature, as well as expert advice from three independent pediatric obesity clinicians and researchers. All items used phrasing to orient parents to respond to questions in the context of child’s weight/shape/size (e.g., “…because of their weight/shape/size”). There were a core set of items that included physical functioning and discomfort, school functioning, emotional functioning, peer relations and victimization, and social withdrawal. In addition, there were a separate set of developmentally appropriate items (seven items) for parents of adolescents aged 14–18 years. These items were also created based on the obesity literature and expert opinion. All response items ranged from “never” (1) to “always” (4). Parents of children and adolescents between 5 and 18 years of age completed the measure.
PedsQL
The PedsQL is a 23-item generic HRQOL measure designed for parents of children between 2 and 18 years of age and for children between 5 and 18 years of age (18). For the current study, the PedsQL Parent Report of Young Children (ages 5–7), PedsQL Parent Report of Children (ages 8–12), and PedsQL Parent Report of Adolescents (ages 13–18) were used. The PedsQL assesses several domains of functioning, including Physical (eight items), Emotional (five items), Social (five items), and School (five items) and utilizes a 5-point Likert scale (0 = never a problem to 4 = almost always a problem). The PedsQL has been found to be valid and reliable for the different versions (Cronbach’s α = 0.89–0.90) (18). It is important to note that items on the three versions of the parent-proxy PedsQL were identical in content and scoring, and thus the data were pooled together.
IWQOL-Kids
The IWQOL-Kids is a weight-specific HRQOL measure for adolescents, which was validated on youth aged 11 years and older (12). For the purposes of this study, the IWQOL-Kids was assessed only in adolescents aged 14 years and older. It is comprised of four subscales (Physical Comfort, Body Esteem, Social Life, and Family Life), as well as a Total Score. The Physical Comfort scale (6 items) examines the impact of weight on an individual’s physical mobility and comfort. The Body Esteem scale (9 items) assesses how individuals feel about themselves and their body in context of their weight. The Social Life scale (6 items) reflects the impact of weight on how an individual is treated in their social environment and peer relations. The Family Life scale (6 items) examines the individual’s perception of what family members may think and feel about them and their weight. The IWQOL-Kids has been shown to have excellent reliability (Cronbach’s α = 0.88–0.95) and validity (12).
Weight and height
For phase 1, General Clinical Research Center or clinic nurses trained in methods of obtaining accurate anthropometric measures obtained height and weight from obese youth. Weight was measured (0.1 kg) on a digital Scaletronix scale (Wheaton, IL). Standing height was measured with a Holtain stadiometer (Holtain, Crymych, UK). For phase 2, research assistants completing data collection were trained in methods of obtaining accurate weight and height measurements. Weight was measured (0.1 kg) on a portable SECA digital scale (SECA, Hamburg, Germany). Standing height was measured with a calibrated custom portable stadiometer (Creative Health Products, Plymouth, MI). Weight and height measurements were taken in triplicate, and the mean was used in analyses. Participants were weighed and measured in street clothing without shoes.
These data were used to calculate BMI (kg/m2). BMI z-score values (zBMI) were calculated for participants using age- (to the nearest month) and sex-specific median, standard deviation, and power of the Box-Cox transformation (LMS method) based on national norms from the Centers for Disease Control and Prevention (29).
Statistical and data analyses
Descriptive statistics (means and standard deviations) were used to characterize demographic variables. Exploratory factor analyses using principal axis factoring with promax rotation were performed on the 35-item pool. Items were deleted for several reasons, including high cross loadings (i.e., loadings of >0.30 on three or more scales when the original loading was below 0.60), redundancy in content, or low factor loadings (≤0.40; (30)). After determination of a meaningful factor structure, internal consistency coefficients using Cronbach’s α were calculated for each scale. Although coefficients of r > 0.70 are recommended (31), Ware and colleagues (1980) have suggested that α coefficients ≥0.60 are considered acceptable for newly developed scales (32). Next, test–retest reliability was determined using intraclass correlation coefficients. An intraclass correlation coefficient of ≥0.80 suggests excellent agreement, between 0.61 and 0.80 moderate agreement, and between 0.41 and 0.60 fair agreement (33). Regarding the adolescent module, factor analyses were not conducted due to the items only being applicable to a subset of the sample (e.g., adolescents). However, Cronbach’s α was calculated for this scale, and items were deleted if internal consistency improved. Test–retest reliability was also assessed for this module.
To examine construct validity for all scales and the adolescent module, Pearson’s product moment correlation coefficients were calculated to determine the relationship between zBMI and Sizing Them Up subscales. Pearson correlations were also calculated between similar scales on Sizing Them Up and scales on (i) PedsQL-Parent Proxy Report and (ii) IWQOL-Kids (adolescent report). Responsiveness to change was determined using a one-sample paired Student’s t test on a subsample of bariatric patients. Effect sizes were estimated by first creating difference scores for each participant and then dividing the mean of these difference scores by the standard deviation. Relative to statistically meaningful differences, the MCID score refers to the smallest change that patients themselves perceive to be beneficial. MCID scores are considered an important aspect of HRQOL measures when evaluating the effects of intervention (34). MCID scores were calculated for each scale using the standard error of measurement and is calculated in the following way: s.e.m. = s.d. √[1-α], s.d. = standard deviation of mean baseline Sizing Them Up scores for each scale (0–100 scores); α = scale reliability (35). One s.e.m. has been shown to be highly correlated with an established MCID on a disease-specific HRQOL measure (36). Pearson correlations were calculated to examine the relationship between age and Sizing Them Up scales. Finally, multivariate ANOVA were conducted to examine race and gender differences in parent-proxy obesity-specific HRQOL, after controlling for zBMI. Analyses were performed using SPSS statistical software (version 14.0, 2006; Chicago, IL).
RESULTS
Factor analysis
An exploratory factor analysis was conducted to examine 35 items on the Sizing Them Up measure for 220 participants. Eigenvalues over one and scree plot data supported the use of a five- to eight-factor solution. Each of these solutions was examined with respect to the pattern of item loadings, cross loadings, and conceptual meaning. A six-factor solution was chosen because it separated a moderate number of items into factors that were statistically distinct and interpretable. Initial items were removed if item loadings were <0.40 or significant cross loadings occurred across three scales. This resulted in a final instrument with 22 items for parents of children 5–18 years of age. (See Supplementary Data online for final Sizing Them Up measure.)
Sizing Them Up scales and items
Sizing Them Up is a 22-item measure consisting of six scales: Emotional Functioning (seven items), Physical Functioning (five items), Teasing/Marginalization (three items), Positive Attributes (four items), Mealtime Challenges (two items), and School Functioning (one item). These six scales make up a summary score or Total QOL scale. The scales, corresponding items, and item loadings of the factor analysis are presented in Table 2. The percentage variance accounted for by the 22-item measure was 66%. In addition, an adolescent module, which originally consisted of seven items was tested. One item was removed due to improvement in internal consistency without the item. Internal consistency coefficients (e.g., Cronbach’s α) for each scale were strong and are presented in Table 3. Internal consistency was lowest for the Positive Social Attributes Scale (α = 0.59) and highest for Emotional Functioning (α = 0.91). Factor intercorrelations were positive and ranged from 0.08 to 0.68 (see Table 4).
Table 2.
Sizing Them Up: exploratory factor loadings
| Item | Mean | s.d. | Emotional Functioning |
Physical Functioning |
Teasing/ Marginalization |
Positive Social Attributes |
Mealtime Challenges |
School Functioning |
|---|---|---|---|---|---|---|---|---|
| Felt frustrated | 2.71 | 0.96 | 0.89 | 0.56 | 0.60 | 0.37 | 0.40 | 0.23 |
| Felt worried | 2.81 | 0.92 | 0.84 | 0.46 | 0.51 | 0.28 | 0.33 | 0.29 |
| Felt mad | 2.96 | 0.91 | 0.83 | 0.43 | 0.53 | 0.39 | 0.41 | 0.29 |
| Felt sad | 2.81 | 0.92 | 0.82 | 0.54 | 0.62 | 0.34 | 0.38 | 0.37 |
| Felt concerned | 2.58 | 0.95 | 0.72 | 0.40 | 0.38 | 0.07 | 0.22 | 0.22 |
| Had low self-esteem | 2.82 | 0.99 | 0.68 | 0.38 | 0.60 | 0.47 | 0.36 | 0.38 |
| Avoided dressing in front of others | 2.70 | 1.10 | 0.61 | 0.46 | 0.50 | 0.35 | 0.25 | 0.35 |
| Difficulty participating in physical activity | 2.96 | 0.90 | 0.46 | 0.82 | 0.55 | 0.38 | 0.27 | 0.09 |
| Difficulty keeping up with other children | 2.90 | 0.87 | 0.43 | 0.77 | 0.57 | 0.33 | 0.34 | −0.01 |
| Became out of breath | 2.48 | 0.85 | 0.45 | 0.68 | 0.65 | 0.36 | 0.37 | 0.06 |
| Changes to physical surroundings | 3.59 | 0.69 | 0.43 | 0.57 | 0.23 | 0.17 | 0.18 | 0.31 |
| Chose not to participate in gym | 3.59 | 0.75 | 0.36 | 0.46 | 0.30 | 0.19 | 0.06 | 0.16 |
| Teased when physically active | 3.15 | 0.83 | 0.56 | 0.47 | 0.74 | 0.35 | 0.31 | 0.26 |
| Felt left out | 3.25 | 0.83 | 0.64 | 0.55 | 0.72 | 0.47 | 0.34 | 0.27 |
| Teased by peers | 2.80 | 0.95 | 0.48 | 0.41 | 0.72 | 0.28 | 0.26 | 0.27 |
| Felt successful in daily activities | 2.60 | 0.81 | 0.31 | 0.29 | 0.31 | 0.72 | 0.28 | 0.13 |
| Good sense of humor | 3.20 | 0.81 | 0.16 | 0.07 | 0.23 | 0.54 | 0.19 | 0.10 |
| Perceived as healthy | 2.17 | 0.90 | 0.21 | 0.30 | 0.32 | 0.52 | 0.17 | −0.03 |
| Kept body clean | 3.35 | 0.95 | −0.05 | 0.13 | 0.06 | 0.35 | 0.03 | 0.01 |
| Upset at mealtimes | 3.25 | 0.85 | 0.37 | 0.23 | 0.32 | 0.33 | 0.91 | 0.27 |
| Argued about eating | 2.62 | 0.98 | 0.32 | 0.25 | 0.33 | 0.24 | 0.69 | 0.20 |
| Chose not to go to school | 3.78 | 0.55 | 0.32 | 0.18 | 0.32 | 0.17 | 0.28 | 0.72 |
Boldface represents the factor loading of the item on its intended scale.
Table 3.
Sizing Them Up: means (s.d.) and reliability coefficients
| Scale | Mean (s.d.) | Cronbach’s α |
Test–retest reliability (n = 97) |
|---|---|---|---|
| Emotional Functioning | 58.89 (25.8) | 0.91 | 0.78 |
| Physical Functioning | 70.15 (20.1) | 0.80 | 0.73 |
| Teasing/Marginalization | 68.79 (24.1) | 0.78 | 0.67 |
| Positive Social Attributes | 60.98 (19.4) | 0.59 | 0.60 |
| Mealtime Challenges | 64.70 (27.7) | 0.77 | 0.70 |
| School Functioninga | 92.85 (18.2) | – | 0.57 |
| Adolescent Developmental Adaptation | 64.65 (18.5) | 0.61 | 0.74 (n = 19) |
| Total Quality of Life | 65.26 (17.0) | 0.91 | 0.80 |
Scale contains only one item.
Table 4.
Sizing Them Up: scale intercorrelations
| Sizing Them Up scales | ||||||||
|---|---|---|---|---|---|---|---|---|
| Emotion Functioning |
Physical Functioning |
Teasing/ Marginalization |
Positive Social Attributes |
Mealtime Challenges |
School Functioning |
Adolescent Developmental Adaptationa |
Total QOL |
|
| Sizing Them Up | ||||||||
| Emotional Functioning | ||||||||
| Physical Functioning | 0.59* | |||||||
| Teasing/Marginalization | 0.68* | 0.59* | ||||||
| Positive Social Attributes | 0.24* | 0.29* | 0.29* | |||||
| Mealtime Challenges | 0.38* | 0.29* | 0.32* | 0.20* | ||||
| School Functioning | 0.33* | 0.21* | 0.33* | 0.08 | 0.28* | |||
| Adolescent Developmental Adaptation | 0.55* | 0.44* | 0.51* | 0.14 | 0.25 | 0.43* | ||
| Total QOL | 0.90* | 0.78* | 0.80* | 0.49* | 0.53* | 0.39* | 0.59* | |
QOL, Quality of Life.
n = 61 for this scale,
P < 0.01.
The Emotional Functioning scale assessed parents’ perceptions of the impact of body weight/size on their child’s feelings and self-esteem. The Physical Functioning scale assessed parents’ perceptions of the impact of body weight/size on their child’s ability to keep up with physical activities. The Teasing/Marginalization scale assessed parents’ perceptions of how often their children were teased or left out due to their weight. The Mealtime Challenges scale assessed parents’ perceptions of difficulty around mealtimes. The Positive Social Attributes scale assessed parents’ perceptions of positive qualities and strengths they perceive their child to possess in context of their weight. The School Functioning scale is comprised of one item which assessed the parents’ perception of whether their child refuses to go to school as a result of their weight. The Adolescent Developmental Adaptation module assessed parent’s perceptions of the impact of body weight/size on their adolescents’ engagement in developmentally appropriate activities (e.g., dating, participating in activities) and concerns related to these activities. Finally, the Total QOL scale is a compilation of the six core scales. All scaled scores were calculated by summing the items and then transforming them to a score ranging from 0 to 100, with 100 representing the best HRQOL. For example, the following computation could be used to calculate the total score (Emotional Functioning = ((emotional functioning_raw score − 7)/21) × 100). Scaled scores allow for better interpretability across scales. The total score was calculated by summing the core 22 items and then similarly transforming to a 0 to 100 scale. The Adolescent Developmental Adaptation module is calculated similarly and can be used with parents of obese adolescents (14–18 years of age).
Test–retest reliability
Test–retest reliability was calculated for 97 participants. The average time between phase 1 and phase 2 visits was 17.3 days (s.d. = 7.6). There was no significant change in zBMI from phase 1 to 2 for these participants (paired t test t(94) = 1.7; P = n.s.) with the exception of three participants who were excluded from these analyses. Test–retest reliability was strong for a majority of scales, ranging from 0.57 to 0.80 (see Table 3).
Construct validity
Regarding the relation between Sizing Them Up and zBMI, a significant association was found for the Physical Functioning scale. Specifically, higher zBMI was associated with poorer HRQOL for Physical Functioning (r = −0.34, P < 0.0001). No significant relations were found between zBMI and other Sizing Them Up scales.
Convergent validity
As expected, correlations were small/moderate to high for similar domains of Sizing Them Up and the PedsQL (see Table 5): Physical Functioning scales = 0.68, Emotional Functioning scales = 0.56, School Functioning scales = 0.31, Sizing Them Up Teasing/Marginalization scale and PedsQL Social scale = 0.73, and Total QOL scales = 0.70. Similarly, correlations between similar scales on Sizing Them Up and the IWQOL-Kids were examined. Correlations were small/moderate between similar constructs: Sizing Them Up Physical Functioning and IWQOL-Kids Physical Comfort scales = 0.35, Sizing Them Up Teasing/Marginalization scale and PedsQL Social scale = 0.24, and Total QOL scales = 0.22 (see Table 5).
Table 5.
Convergence between Sizing Them Up, PedsQL, and IWQOL-Kids scales
| Sizing Them Up scales | ||||||||
|---|---|---|---|---|---|---|---|---|
| Emotion Functioning |
Physical Functioning |
Teasing/ Marginalization |
Positive Social Attributes |
Mealtime Challenges |
School Functioning |
Adolescent Developmental Adaptationa |
Total QOL | |
| PedsQL | ||||||||
| Physical | 0.44** | 0.68** | 0.42** | 0.33** | 0.28** | 0.18** | 0.30* | 0.60** |
| Emotion | 0.56** | 0.44** | 0.49** | 0.29** | 0.40** | 0.32** | 0.43** | 0.62** |
| Social | 0.59** | 0.65** | 0.73** | 0.31** | 0.37** | 0.29** | 0.42* | 0.73** |
| School | 0.28** | 0.36** | 0.27** | 0.23** | 0.22** | 0.31** | 0.29* | 0.38** |
| Psychosocial total | 0.57** | 0.59a,** | 0.60** | 0.33** | 0.40** | 0.37** | 0.48** | 0.70** |
| Total QOL | 0.56** | 0.67** | 0.57** | 0.36** | 0.38** | 0.31** | 0.45** | 0.70** |
| IWQOL-Kids | ||||||||
| Physical Comfort | 0.18 | 0.35** | 0.23** | −0.04 | −0.07 | −0.02 | 0.09 | 0.22* |
| Body Esteem | 0.34** | 0.17 | 0.33** | 0.09 | 0.01 | 0.10 | 0.24 | 0.31** |
| Social Life | 0.07 | 0.09 | 0.24* | 0.10 | 0.06 | −0.03 | −0.03 | 0.13 |
| Family Relations | 0.01 | 0.04 | 0.12 | 0.07 | 0.02 | −0.02 | −0.14 | 0.05 |
| Total QOL | 0.18 | 0.19 | 0.28** | 0.07 | 0.01 | 0.02 | 0.05 | 0.22* |
IWQOL, Impact of Weight on Quality of Life.
Boldface numbers represent domains for which convergence was expected based on similarity of constructs.
n = 61 for this scale,
P < 0.05,
P < 0.01.
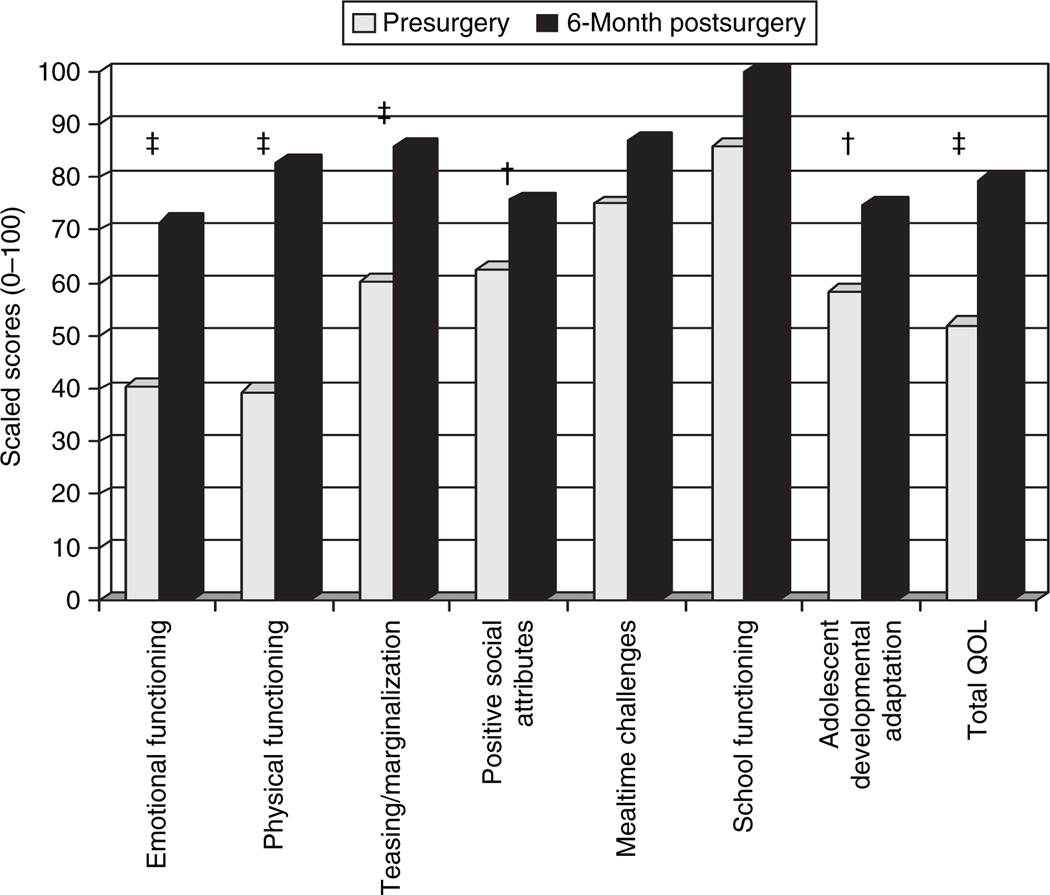
Responsiveness to weight change
Mean BMI change for adolescents who underwent bariatric surgery over a 6-month period was a reduction of 20.3 BMI points (s.d. = 3.1). Significant improvements were observed on several scales of Sizing Them Up, including Emotional Functioning (t(13) = −6.9; P < 0.001), Physical Functioning (t(13) = −9.1; P < 0.001), Teasing/Marginalization (t(13) = −4.9; P < 0.001), Positive Attributes (t(13) = −3.2; P < 0.01), Total QOL (t(13) = −10.1; P < 0.001), and Adolescent Developmental Adaptation (t(13) = −3.6; P < 0.01) (see Figure 1). Effect sizes for pre- to 6-month postsurgery were as follows: Emotional Functioning = 1.86, Physical Functioning = 2.42, Teasing/Marginalization = 1.32, Positive Attributes = 0.86, Mealtime Challenges = 0.47, School Functioning = 0.50, Total QOL = 2.69, and Adolescent Developmental Adaptation = 0.96.
Figure 1.
Changes in Sizing Them Up scores after bariatric surgery intervention. Significant differences between pre- and postsurgery (†P < 0.01, ‡P < 0.001). QOL, Quality of Life.
MCID
Standard errors of measurement were as follows for each scale: Emotional Functioning = 7.74, Physical Functioning = 9.05, Teasing/Marginalization = 11.09, Positive Attributes = 12.42, Mealtime Challenges = 13.29, School Functioning = not applicable because this is a one-item scale, Total QOL = 5.10, Adolescent Developmental Adaptation = 11.55.
Age, gender, and race differences
There were significant negative correlations between age and a majority of Sizing Them Up scales, including Emotional Functioning (r = −0.26, P < 0.0001), Physical Functioning (r = −0.26, P < 0.0001), Positive Attributes (r = −0.14, P < 0.05), School Functioning (r = −0.13, P < 0.05), and Total QOL (r = −0.23, P < 0.001). These data suggest that obesity-specific HRQOL decreases as children grow older. However, age was significantly positively correlated with Mealtime Challenges (r = 0.18, P < 0.01), suggesting that parents perceive older children to have less mealtime challenges. No significant relations were found between Teasing/Marginalization scale and Adolescent Developmental Adaptation module and age.
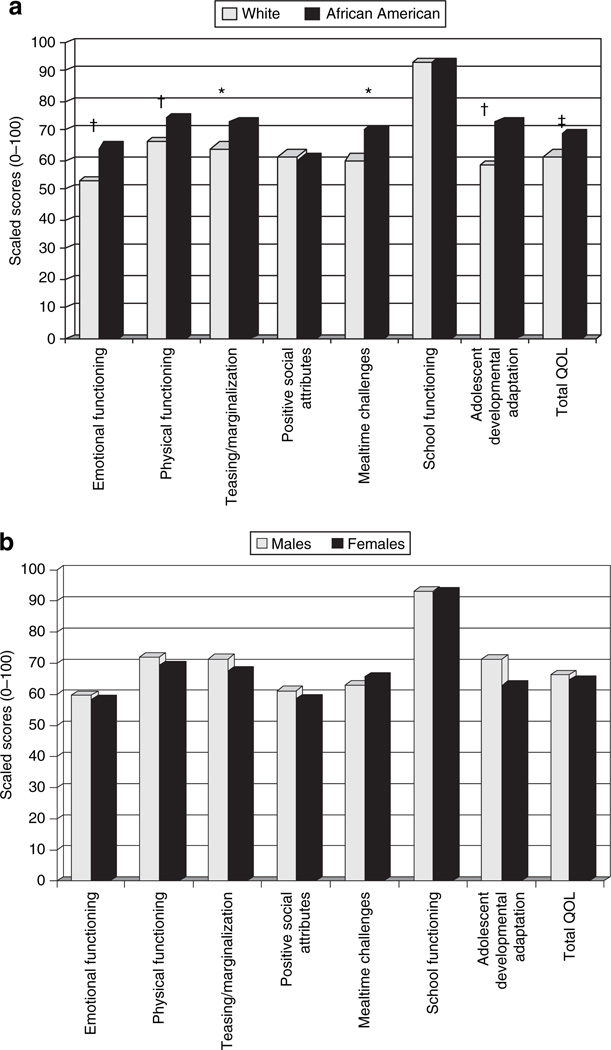
Race differences were also examined on Sizing Them Up scales, adjusting for zBMI scores. Given the large proportion of white and African-American youth in the current sample, analyses were limited to these two groups. The overall multivariate ANOVA suggested significant race differences on Sizing Them Up scales (Hotelling’s T = 0.08, F (6, 200) = 2.65, P < 0.05). Specifically, parents of African-American youth reported better Emotional Functioning (F(1, 205) = 9.7, P < 0.01), Physical Functioning (F(1, 205) = 10.3, P < 0.01), Teasing/Marginalization (F(1, 205) = 6.3, P < 0.05), Mealtime Challenges (F(1, 205) = 6.4, P < 0.05), Total QOL scores (F(1, 206) = 11.4, P < 0.001), and Adolescents Developmental Adaptation (F(1, 56) = 9.4, P < 0.01) compared to parents of white youth (see Figure 2). No significant differences were found on the Positive Attributes and School scales. In addition, no significant differences were found on Sizing Them Up scales by gender, after adjusting for zBMI (Hotelling’s T = 0.01, F (6, 211) = 0.47, P = n.s.) (see Figure 2).
Figure 2.
Differences on obesity-specific health-related quality of life (HRQOL) by (a) race and (b) gender, after controlling for standardized BMI *P < 0.05, †P < 0.01, ‡P < 0.001.
DISCUSSION
Sizing Them Up is the first parent-proxy, obesity-specific HRQOL measure that assesses domains of functioning that are most relevant and important to obese children. Preliminary results demonstrate that Sizing Them Up has strong psychometric properties, including good internal consistency among scales, test–retest reliability, construct validity with zBMI, convergent validity with similar HRQOL scales, and responsiveness to change following bariatric surgery treatment. Preliminary MCID data were also established and suggest changes of 5 to 13 points, depending on the scale, represent important perceived change by parents of obese youth. Thus, Sizing Them Up likely has both clinical and research utility in a variety of settings, including obesity treatment programs, medical specialty clinics that work with obese children, and primary care offices.
Sizing Them Up is comprised of six core scales, including Emotional Functioning, Physical Functioning, Teasing/Marginalization, Positive Social Attributes, Mealtime Challenges, and School Functioning, as well as a module for parents of adolescents, Adolescent Developmental Adaptation. Several parent-proxy measures of HRQOL (e.g., PedsQL) include broad scales such as Physical and Emotional functioning; however, Sizing Them Up considers these areas in the context of obesity (e.g., questions that attribute difficulties to weight/shape/size). Scales such as Teasing/Marginalization and Mealtime Challenges were developed to assess for areas that are problematic for obese youth (37–41). For example, mothers of obese youth reported difficulties with child behavior at mealtimes compared to mothers of nonoverweight youth (41). Similarly, obese children and adolescents, relative to nonoverweight peers, reported more name-calling and teasing about their appearance (40). Unique to this measure are the Positive Social Attributes scale and Adolescent Developmental Adaptation module. The Positive Social Attributes scale assesses the perceived strengths of obese youth (e.g., humor, healthiness, success) and may enable clinicians to understand the child’s strengths, as well as areas that they may want to improve. Having an HRQOL scale focused on identifying positive attributes of a child is quite unique but critical in obtaining a more balanced view of obese youth. Further, the Adolescent Developmental Adaptation module assesses aspects of HRQOL that are known to be most relevant during the adolescent developmental period, including dating, participation in hobbies and school-based extracurricular activities, and employment. Data from the current study suggest that adolescents with obesity have poor developmental adaptation as demonstrated by their low-scaled scores on the Adolescent Developmental Adapatation module on Sizing Them Up. Age-salient tasks, which are assessed on this module, are known to serve as “benchmarks” for successful adaptation in adulthood while failing these tasks is predictive of poorer adaptation (42,43). Given that obesity during adolescence and young adulthood has been strongly associated with lower education attainment, family income, and rates of marriage (44), it is important to measure this aspect of HRQOL.
Additional analyses considered whether parent-proxy, obesity-specific HRQOL varied by age, race, or gender. Obesity-specific HRQOL decreased with age for a majority of the scales. This is consistent with prior research that demonstrates a negative association between generic HRQOL and age for overweight and obese children and adolescents (22,45), as well as other chronic conditions, including diabetes, cardiac disorders, cancer, and rheumatology disorders (46). One potential reason for these findings could be drawn from the few longitudinal studies in pediatric obesity which suggest that self-esteem worsens with increasing age (47,48), which likely influences HRQOL. Interestingly, Mealtime Challenges improved with age, which is likely due to the fact that mealtime challenges tend to occur when children are younger and exhibit more behavioral issues around eating. In addition, significant race differences were also observed for Sizing Them Up scales. Similar to research conducted by Kolotkin and colleagues (2006), parents of African-American obese youth reported better HRQOL than parents of white obese youth. This may be attributed to African-American youth and adults preferring a heavier ideal body size and potentially being less affected by their weight compared to their white counterparts (49–51). In contrast to the adult and adolescent weight-specific HRQOL literature (12,52), we found no significant differences by gender on Sizing Them Up scales. One potential reason for lack of gender differences is the proxy reporting of HRQOL compared to self-report in those studies. In addition, scales from the weight-specific measures in which differences were found may not be relevant to children (e.g., Sexual life) or are not present in Sizing Them Up (e.g., Body Esteem).
Within a given clinical setting, Sizing Them Up can be utilized in a number of ways to inform clinical care. For example, the measure is brief (e.g., 22 items) and allows a caregiver to describe the impact of their child or adolescent’s obesity on daily functioning. This may serve to not only guide clinical decision making but also provide a tool to improve caregiver/patient–provider communication around current patient concerns. Given its demonstrated sensitivity to weight change and preliminary establishment of MCIDs, Sizing Them Up may also be used to assess clinical care outcomes. For example, if a patient loses some weight but reports improvement in their physical functioning, this could be used as a motivator to continue with weight loss efforts. Further, from a provider perspective, Sizing Them Up is of low cost, easy to score and interpret, and, therefore, presents minimal burden for use within a clinical setting.
Although Sizing Them Up represents the first parent-proxy HRQOL measure developed and validated for parents of children and adolescents with obesity, the study has some limitations. First, the sample may not be generalizable because (i) children and families were treatment seeking, (ii) data collection occurred at one site, and (iii) children represented primarily two ethnic groups (e.g., white and black). It is possible that obese youth within the community who are not seeking treatment have different HRQOL compared to those who do seek treatment. Furthermore, HRQOL may differ for other ethnic groups, including Hispanic, Native American, and Asian youth. It is also important to note that this measure was developed for parents of obese, not overweight, children and adolescents. Future research needs to evaluate the factor structure and psychometric properties in an overweight population. Finally, it is important to note that this study represents preliminary psychometric evaluation of Sizing Them Up. Potential limitations of the measure include a relatively lower α for the Positive Attribute Scale (α = 0.59), as well as a one-item scale (e.g., School Functioning). Although the School Functioning scale is not comprehensive, it was retained due to its high factor loading and clinical utility. In addition, we present an initial demonstration of the salience and clinical utility of a module assessing adolescent developmental adaptation; however, this module would benefit from further psychometric evaluation with larger adolescent samples.
Research has strongly advocated for multi-informant reporting of HRQOL to assess both the child and parent’s vantage point. Parents and children have unique perspectives regarding the child’s HRQOL and several studies have shown discrepancies based on child self-report and parent-proxy reports (53,54). For example, even with the current study, IWQOL-Kids scores have low-to-moderate correlations with Sizing Them Up scale. Both self-report and parent-proxy reports are important because parents typically initiate both medical and psychological treatment (15–17) while children/adolescents may more accurately report on their own thoughts and feelings. We are currently working on the validation of the parallel obesity-specific, child self-report HRQOL measure, Sizing Me Up. Having the child’s perspective is key in treatment, both to understand the outcome of treatment and to facilitate dialogue when parents and children disagree about how obesity is affecting life. Using Sizing Them Up and Sizing Me Up together in both research and clinical practice will provide further insight into the impact of obesity on children and their families.
Supplementary Material
ACKNOWLEDGMENTS
This research was funded by grants from the National Institutes of Health through a postdoctoral training grant from the National Institutes of Health (T32 DK063929) awarded to the first author and K23-DK60031 (Exploring Barriers to Treatment: Pediatric Obesity) and R03DK0788901 (Bariatric Surgery in Adolescence: Psychosocial Outcomes) grants awarded to the second author. Additional resources were provided by the Cincinnati Children’s Hospital Medical Center–General Clinical Research Center, which is supported in part by USPHS Grant #M01 RR 08084 from the General Clinical Research Centers Program, National Center for Research Resources/NIH. We extend our deepest appreciation to children and adolescents and their families who participated in this study. We also thank the research assistants and summer students who were instrumental in recruiting participants and collecting data, including Christina Ramey, Lindsay Wilson, Carrie Piazza-Waggoner, Julie Koumoutsos, Sarah Valentine, Stephanie Ridel, Kate Grampp, Ambica Tumkur, Rachel Jordan, Matt Flanigan, and Neha Godiwala.
Footnotes
SUPPLEMENTARY MATERIAL
Supplementary material is linked to the online version of the paper at http://www.nature.com/oby
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1.Quittner AL, Davis MA, Modi AC. Health-related quality of life in pediatric populations. In: Roberts MC, editor. Handbook of Pediatric Psychology. 2nd edn. New York: Guilford Publications; 2003. pp. 696–709. [Google Scholar]
- 2.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 3.Juniper EF, Guyatt GH, Jaeschke R. How to develop and validate a new health-related quality of life instrument. In: Spilker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. 2nd edn. Philadelphia, PA: Lippincott Williams & Wilkins; 1996. pp. 49–56. [Google Scholar]
- 4.Schipper H, Clinch JL, Olweny LM. Quality of life studies: definitions and conceptual issues. In: Spilker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. 2nd edn. Philadelphia, PA: Lippincott-Raven; 1996. pp. 11–24. [Google Scholar]
- 5.U.S.-Food-and-Drug-Administration. Guidance for industry patient reported outcome measures: use in medical product development to support labeling claims (Draft Guidance) 2006 doi: 10.1186/1477-7525-4-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zahran HS, Kobau R, Moriarty DG, et al. Health-related quality of life surveillance—United States, 1993–2002. MMWR Surveill Summ. 2005;54:1–35. [PubMed] [Google Scholar]
- 7.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 8.Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity (Silver Spring) 2006;14:301–308. doi: 10.1038/oby.2006.39. [DOI] [PubMed] [Google Scholar]
- 9.Berkowitz RI, Fujioka K, Daniels SR, et al. Effects of sibutramine treatment in obese adolescents: a randomized trial. Ann Intern Med. 2006;145:81–90. doi: 10.7326/0003-4819-145-2-200607180-00005. [DOI] [PubMed] [Google Scholar]
- 10.Inge TH, Krebs NF, Garcia VF, et al. Bariatric surgery for severely overweight adolescents: concerns and recommendations. Pediatrics. 2004;114:217–223. doi: 10.1542/peds.114.1.217. [DOI] [PubMed] [Google Scholar]
- 11.Holterman AX, Browne A, Dillard BE, 3rd, et al. Short-term outcome in the first 10 morbidly obese adolescent patients in the FDA-approved trial for laparoscopic adjustable gastric banding. J Pediatr Gastroenterol Nutr. 2007;45:465–473. doi: 10.1097/MPG.0b013e318063eef6. [DOI] [PubMed] [Google Scholar]
- 12.Kolotkin RL, Zeller M, Modi AC, et al. Assessing weight-related quality of life in adolescents. Obesity (Silver Spring) 2006;14:448–457. doi: 10.1038/oby.2006.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eiser C, Morse R. Quality-of-life measures in chronic diseases of childhood. Health Technol Assess. 2001;5:1–157. doi: 10.3310/hta5040. [DOI] [PubMed] [Google Scholar]
- 14.Ingerski LM, Janicke DM, Silverstein JH. Brief report: quality of life in overweight youth-the role of multiple informants and perceived social support. J Pediatr Psychol. 2007;32:869–874. doi: 10.1093/jpepsy/jsm026. [DOI] [PubMed] [Google Scholar]
- 15.Janicke DM, Finney JW, Riley AW. Children’s health care use: a prospective investigation of factors related to care-seeking. Med Care. 2001;39:990–1001. doi: 10.1097/00005650-200109000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Seid M, Varni JW, Kurtin PS. Measuring quality of care for vulnerable children: challenges and conceptualization of a pediatric outcome measure of quality. Am J Med Qual. 2000;15:182–188. doi: 10.1177/106286060001500409. [DOI] [PubMed] [Google Scholar]
- 17.Campo JV, Comer DM, Jansen-Mcwilliams L, Gardner W, Kelleher KJ. Recurrent pain, emotional distress, and health service use in childhood. J Pediatr. 2002;141:76–83. doi: 10.1067/mpd.2002.125491. [DOI] [PubMed] [Google Scholar]
- 18.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289:1813–1819. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 20.Williams J, Wake M, Hesketh K, Maher E, Waters E. Health-related quality of life of overweight and obese children. JAMA. 2005;293:70–76. doi: 10.1001/jama.293.1.70. [DOI] [PubMed] [Google Scholar]
- 21.Swallen KC, Reither EN, Haas SA, Meier AM. Overweight, obesity, and health-related quality of life among adolescents: the National Longitudinal Study of Adolescent Health. Pediatrics. 2005;115:340–347. doi: 10.1542/peds.2004-0678. [DOI] [PubMed] [Google Scholar]
- 22.Ravens-Sieberer U, Redegeld M, Bullinger M. Quality of life after in-patient rehabilitation in children with obesity. Int J Obes Relat Metab Disord. 2001;25(Suppl 1):S63–S65. doi: 10.1038/sj.ijo.0801702. [DOI] [PubMed] [Google Scholar]
- 23.Janicke DM, Marciel KK, Ingerski LM, et al. Impact of psychosocial factors on quality of life in overweight youth. Obesity (Silver Spring) 2007;15:1799–1807. doi: 10.1038/oby.2007.214. [DOI] [PubMed] [Google Scholar]
- 24.Kolotkin RL, Crosby RD. Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (IWQOL-lite) in a community sample. Qual Life Res. 2002;11:157–171. doi: 10.1023/a:1015081805439. [DOI] [PubMed] [Google Scholar]
- 25.Le Pen C, Levy E, Loos F, Banzet MN, Basdevant A. “Specific” scale compared with “generic” scale: a double measurement of the quality of life in a French community sample of obese subjects. J Epidemiol Community Health. 1998;52:445–450. doi: 10.1136/jech.52.7.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dymek MP, Le Grange D, Neven K, Alverdy J. Quality of life after gastric bypass surgery: a cross-sectional study. Obes Res. 2002;10:1135–1142. doi: 10.1038/oby.2002.154. [DOI] [PubMed] [Google Scholar]
- 27.Stevens G, Featherman DL. A revised socioeconomic index of occupational status. Soc Sci Res. 1981;10:364–395. [Google Scholar]
- 28.Mueller CW, Parcel TL. Measures of socioeconomic status: alternatives and recommendations. Child Dev. 1981;52:13–20. [Google Scholar]
- 29.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;(314):1–27. [PubMed] [Google Scholar]
- 30.Bryant F, Yarnold P. Principal-components analysis and exploratory and confirmatory factor analysis. In: Grimm LG, Yarnold PR, editors. Reading and Understanding Multivariate Statistics. Washington, DC: American Psychological Association; 2001. pp. 99–136. [Google Scholar]
- 31.Nunnally J, Bernstein I. Psychometric Theory. 3rd edn. New York: McGraw-Hill; 1994. [Google Scholar]
- 32.Ware JE, Brook RH, Davies-Avery A, et al. Model of Health and Methodology (R-1987/1-HEW) Santa Monica, CA: RAND Corporation; 1980. [Google Scholar]
- 33.Shrout PE. Measurement reliability and agreement in psychiatry. Stat Methods Med Res. 1998;7:301–317. doi: 10.1177/096228029800700306. [DOI] [PubMed] [Google Scholar]
- 34.Terwee CB, Dekker FW, Wiersinga WM, Prummel MF, Bossuyt PM. On assessing responsiveness of health-related quality of life instruments: guidelines for instrument evaluation. Qual Life Res. 2003;12:349–362. doi: 10.1023/a:1023499322593. [DOI] [PubMed] [Google Scholar]
- 35.Wyrwich KW, Tierney WM, Wolinsky FD. Further evidence supporting an SEM-based criterion for identifying meaningful intra-individual changes in health-related quality of life. J Clin Epidemiol. 1999;52:861–873. doi: 10.1016/s0895-4356(99)00071-2. [DOI] [PubMed] [Google Scholar]
- 36.Wyrwich KW, Tierney WM, Wolinsky FD. Using the standard error of measurement to identify important changes on the Asthma Quality of Life Questionnaire. Qual Life Res. 2002;11:1–7. doi: 10.1023/a:1014485627744. [DOI] [PubMed] [Google Scholar]
- 37.Pearce MJ, Boergers J, Prinstein MJ. Adolescent obesity, overt and relational peer victimization, and romantic relationships. Obes Res. 2002;10:386–393. doi: 10.1038/oby.2002.53. [DOI] [PubMed] [Google Scholar]
- 38.Faith MS, Leone MA, Ayers TS, Heo M, Pietrobelli A. Weight criticism during physical activity, coping skills, and reported physical activity in children. Pediatrics. 2002;110(2 Pt 1):e23. doi: 10.1542/peds.110.2.e23. [DOI] [PubMed] [Google Scholar]
- 39.Israel AC, Shapiro LS. Behavior problems of obese children enrolling in a weight reduction program. J Pediatr Psychol. 1985;10:449–460. doi: 10.1093/jpepsy/10.4.449. [DOI] [PubMed] [Google Scholar]
- 40.Neumark-Sztainer D, Story M, Faibisch L. Perceived stigmatization among overweight African-American and Caucasian adolescent girls. J Adolesc Health. 1998;23:264–270. doi: 10.1016/s1054-139x(98)00044-5. [DOI] [PubMed] [Google Scholar]
- 41.Zeller MH, Reiter-Purtill J, Modi AC, et al. Controlled study of critical parent and family factors in the obesigenic environment. Obesity (Silver Spring) 2007;15:126–136. doi: 10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]
- 42.Masten AS, Coatsworth JD, Neemann J, et al. The structure and coherence of competence from childhood through adolescence. Child Dev. 1995;66:1635–1659. [PubMed] [Google Scholar]
- 43.Roisman GI, Masten AS, Coatsworth JD, Tellegen A. Salient and emerging developmental tasks in the transition to adulthood. Child Dev. 2004;75:123–133. doi: 10.1111/j.1467-8624.2004.00658.x. [DOI] [PubMed] [Google Scholar]
- 44.Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 1993;329:1008–1012. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 45.Zeller MH, Modi AC. Predictors of health-related quality of life in obese youth. Obesity (Silver Spring) 2006;14:122–130. doi: 10.1038/oby.2006.15. [DOI] [PubMed] [Google Scholar]
- 46.Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:43. doi: 10.1186/1477-7525-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brown KM, McMahon RP, Biro FM, et al. Changes in self-esteem in black and white girls between the ages of 9 and 14 years. The NHLBI Growth and Health Study. J Adolesc Health. 1998;23:7–19. doi: 10.1016/s1054-139x(97)00238-3. [DOI] [PubMed] [Google Scholar]
- 48.Strauss RS. Childhood obesity and self-esteem. Pediatrics. 2000;105:e15. doi: 10.1542/peds.105.1.e15. [DOI] [PubMed] [Google Scholar]
- 49.Neff LJ, Sargent RG, McKeown RE, Jackson KL, Valois RF. Black-white differences in body size perceptions and weight management practices among adolescent females. J Adolesc Health. 1997;20:459–465. doi: 10.1016/S1054-139X(96)00273-X. [DOI] [PubMed] [Google Scholar]
- 50.Fitzgibbon ML, Blackman LR, Avellone ME. The relationship between body image discrepancy and body mass index across ethnic groups. Obes Res. 2000;8:582–589. doi: 10.1038/oby.2000.75. [DOI] [PubMed] [Google Scholar]
- 51.Thompson JK, Heinberg LJ, Altable M, Tantleff-Dunn S. Exacting Beauty: Theory, Assessment, and Treatment of Body Image Disturbance. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- 52.Kolotkin RL, Crosby RD, Williams GR. Health-related quality of life varies among obese subgroups. Obes Res. 2002;10:748–756. doi: 10.1038/oby.2002.102. [DOI] [PubMed] [Google Scholar]
- 53.Modi AC, Quittner AL. Validation of a disease-specific measure of health-related quality of life for children with cystic fibrosis. J Pediatr Psychol. 2003;28:535–545. doi: 10.1093/jpepsy/jsg044. [DOI] [PubMed] [Google Scholar]
- 54.Theunissen NC, Vogels TG, Koopman HM, et al. The proxy problem: child report versus parent report in health-related quality of life research. Qual Life Res. 1998;7:387–397. doi: 10.1023/a:1008801802877. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.