Abstract
Conclusion
IgG4-related disease involves nasal manifestations with chronic rhinosinusitis (CRS). This type of sinusitis is a new clinical entity of nasal disease associated with a high level of serum IgG4 for which steroid therapy is effective.
Objectives.
To confirm whether IgG4-related disease has distinctive chronic rhinosinusitis.
Methods:
We compared serum IgG4 levels as well as nasal computed tomography (CT) and clinicopathological findings before and after glucocorticoid treatment in 31 patients diagnosed as having IgG4-related disease with nasal manifestations. To evaluate immunohistochemical findings of nasal mucosa, we compared them with IgG4-related CRS and common CRS.
Results:
All patients had levels of high serum IgG4. Ten of the 31 patients had nasal obstruction, nasal discharge, postnasal discharge, hyposmia, and dull headache. They also demonstrated sinus lesions on radiological findings. After glucocorticoid treatment, serum IgG and IgG4 levels were markedly decreased and along with improvement of the symptoms, nasal sinus CT findings also revealed improvement of the sinus opacification. In immunohistochemical examination, the magnitude of IgG4-positive plasma cell infiltration in common CRS was almost the same as in the IgG4-related CRS group. Therefore, in nasal mucosa immunocytochemical positive staining for IgG4 is not specific for definition of IgG4-related disease.
Keywords: IgG4-related disease, high serum IgG4, steroids
Introduction
The first report of IgG4-related disease was of chronic pancreatitis characterized by high serum immunoglobulin G4 (IgG4) concentrations and abundant IgG4-bearing plasma cell infiltration in the pancreatic lesion [1]. This was categorized as autoimmune pancreatitis (AIP), and it has been reported to be associated with a variety of extrapancreatic lesions including sclerosing sialadenitis, sclerosing cholangitis, retroperitoneal fibrosis, tubulointerstitial nephritis [2], hilar lymphadenopathy, lung nodules [3], interstitial pneumonia [4], central airway stenosis [5], and prostatitis [6]. Since it has been reported that IgG4-related diseases other than AIP involve widespread inflammatory lesions similar to AIP, and that the lesions do not always occur simultaneously [7], it has been thought that there is possibly a systemic disease, which has been variously termed multifocal fibrosclerosis [8,9], IgG4-related sclerosing disease [10], or IgG4-associated multifocal fibrosis [11]. Most of the multiple organ lesions seem to show a favorable response to glucocorticoid treatment [1–10].
Formerly, in the otorinolaryngological field, Mikulicz disease (MD) has been considered one of the manifestations of Sjögren syndrome [12]. However, more recently, MD has been reported to be associated with elevated IgG4 concentrations in the serum and prominent infiltrations of plasmacytes expressing IgG4 into the lacrimal and salivary glands. Thus MD is now considered one of the manifestations of IgG4-related diseases rather than Sjögren syndrome [13]. Steroid therapy tends to be effective for reduction of the lacrimal and salivary gland size and serum IgG4 levels.
Meanwhile, through our follow-up of AIP and MD as IgG4-related disease patients, several had nasal problems, including nasal obstruction or nasal discharge and were diagnosed as having allergic rhinitis and/or chronic rhinosinusitis (CRS).
In this study, we compared 1) computed tomography (CT) findings, 2) clinicopathological findings, 3) serum IgG4 levels, and 4) immunohistochemical findings in IgG4-related AIP and MD patients who also had CRS before and after glucocorticoid treatment.
Material and methods
Patients
We recruited 31 patients (23 men and 8 women, 50–83 years of age, mean age 61.1 years) who were diagnosed with AIP and/or MD and who also had other IgG4-related disease and were admitted to the Departments of Internal Medicine or Otorhinolaryngology, Shinshu University Hospital between January 2008 and December 2009. Clinical manifestations of 31 patients who participated in this study are summarized in Table I.
Table I.
Clinical manifestations of IgG4-related disease.
| Case no. | Age/gender | Autoimmune pancreatitis | Sclerosing cholangitis | Retroperitoneal fibrosis | Mikulicz's disease | Lung lesions | Others | Chronic rhinosinusitis | Serum IgG (mg/dl) | Serum IgG4 (mg/dl) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 55/M | + | + | + | + | + | + | 5545 | 2970 | |
| 2 | 56/M | + | + | + | + | 2377 | 387 | |||
| 3 | 50/M | + | + | + | + | + | 2001 | 773 | ||
| 4 | 51/M | + | + | + | + | + | 2741 | 1610 | ||
| 5 | 60/M | + | + | + | + | + | + | 3767 | 1910 | |
| 6 | 68/M | + | + | + | + | 2112 | 209 | |||
| 7 | 74/M | + | + | + | + | *1 | + | 3092 | 1550 | |
| 8 | 59/F | + | + | 1159 | 364 | |||||
| 9 | 63/F | + | + | + | 2759 | 1500 | ||||
| 10 | 65/M | + | + | + | 2631 | 1570 | ||||
| 11 | 59/M | + | 1590 | 158 | ||||||
| 12 | 81/F | + | + | 1982 | 697 | |||||
| 13 | 60/F | + | + | *2 | 2734 | 1800 | ||||
| 14 | 74/M | + | + | + | 5831 | 3460 | ||||
| 15 | 71/M | + | 2455 | 294 | ||||||
| 16 | 71/M | + | + | 2347 | 1720 | |||||
| 17 | 59/M | + | 1709 | 387 | ||||||
| 18 | 83/M | + | + | 1764 | 252 | |||||
| 19 | 80/M | + | 4533 | 1890 | ||||||
| 20 | 59/M | + | + | + | 2006 | 352 | ||||
| 21 | 78/F | + | + | + | + | + | 3118 | 1980 | ||
| 22 | 79/F | + | + | + | 1754 | 555 | ||||
| 23 | 57/M | + | 1659 | 196 | ||||||
| 24 | 73/M | + | + | 1552 | 303 | |||||
| 25 | 64/F | + | + | + | 1903 | 692 | ||||
| 26 | 71/M | + | + | + | 1236 | 244 | ||||
| 27 | 71/M | + | + | + | + | 4661 | 1950 | |||
| 28 | 74/F | + | 1410 | 154 | ||||||
| 29 | 56/M | + | 1026 | 162 | ||||||
| 30 | 70/M | + | + | + | + | 2420 | 688 | |||
| 31 | 66/M | + | + | + | + | 3196 | 1300 |
*1, inflammatory pseudotumor (liver); 2, pericardial pseudotumor.
Diagnosis of CRS
CRS was diagnosed by two different otolaryngologists using endoscopic examination and nasal CT scanning, according to the following definition: 12 weeks or longer of two or more of the following symptoms: mucopurulent drainage, nasal obstruction, facial pain-pressure-fullness, or decreased sense of smell; and findings of purulent mucus or edema in the middle meatus or ethmoid region, polyps in the nasal cavity or the middle meatus, and/or radiographic imaging showing inflammation of the paranasal sinuses [14].
Oral prednisolone treatment for AIP patients with IgG4-related CRS
Seven of 10 IgG4-related patients who had CRS manifestations were treated with oral prednisolone. Three patients were not treated, because of unstable diabetes mellitus, because priority was given to surgical treatment for thyroid papillary carcinoma, and because symptoms were light with only MD, respectively.
Prednisolone administration was started at 40 mg per day and continued for 4 weeks, followed by a gradual reduction of 5 mg per week over a period of 7 weeks until a daily dose of 5 mg was reached [1].
CT scans
To evaluate therapeutic efficacy, comparison of pretreatment CT findings was made with findings from CT performed after approximately 3 months of prednisolone administration, i.e. at the point when it was possible to reduce the dosage to 5–15 mg/day.
CT data were obtained using a standard clinical protocol; 3–5 mm contiguous scans were obtained in the axial plane and reconstructed in the coronal plane. Each sinus CT scan was then scored in a blinded fashion by three otolaryngologists using the Zinreich method [15] and the average scores were calculated. In brief, the extent of sinus opacification was computed based on the sum of the scores for the five major right and left sinuses, each scored on a five-point opacification scale as follows: 0, 0%; 1, 1–25%; 2, 26–50%; 3, 51–75%; 4, 76–99%; 5, 100%.
Histological evaluation
Nasal mucosa was examined immunocytochemically for IgG4 antibody in five patients. As a control group, five other patients with clinically diagnosed common CRS were used. None of the patients in the control group had any findings characteristic of AIP or MD. Other autoimmune diseases, such as sarcoidosis or Wegener's granulomatosis were also ruled out in the control group.
Samples were obtained from the IgG4-related patients who had CRS manifestations by middle turbinate nasal mucosa biopsy (case nos 1–5). Histological specimens from the control group were taken from near the middle turbinate, excluding the polyp and mucosa during sinus surgery. Tissue samples from each surgically resected specimen were fixed in neutral formalin and embedded in paraffin. Sections were stained with hematoxylin and eosin (H&E), and immunostained with sheep polyclonal anti-human IgG4 antibody (Binding Site, Birmingham, UK).
Immunohistochemistry was carried out using the avidin-biotin-peroxidase complex method. We then counted the number of immunohistochemically identified IgG4-positive plasma cells in each specimen. The number of IgG4-positive plasma cells identified per high power field (HPF) was scored as previously described by Kamisawa et al. (severe, more than 30 per HPF; moderate, 30–10 per HPF; slight, 10–5 per HPF; or few, fewer than 5 per HPF) [16].
The ethics committee of Shinshu University Hospital approved the study and informed consent for invasive tests such as nasal mucosa biopsy was obtained from all subjects.
Statistics
All data are expressed as means ± standard error (SEM). The data were evaluated for significance by an ANOVA. If the variance was parametric, the difference was evaluated by Student's t test. Significance was determined at p < 0.05 (two-tailed test).
Results
Clinical findings
All 31 patients had a high serum IgG4 levels (cut-off, 135 mg/dl) [1]. Patients presenting with submandibular and/or lacrimal gland swelling were diagnosed by gland biopsy.
Clinical findings of the 10 out of the 31 patients who had CRS manifestations (bilateral, 8; unilateral, 2) are summarized in Table II. Nutritional conditions of all were relatively normal, and they had a variety of complaints such as lacrimal and submandibular gland swelling, loss of appetite, and abdominal symptoms.
Table II.
Clinical findings and symptoms of IgG4-related patients who had CRS manifestations.
| Case no. | Age/ gender |
Nasal symptoms |
Allergic involvement |
Laboratory tests |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Rhinorrhea | Nasal obstruction | Postnasal drip | Anosmia | Allergic rhinitis | Asthma | Serum IgE (IU/ml) | Blood eosinophils (%) | Nasal smear eosinophils | ||
| 1 | 55/M | + | + | 288 | 15 | + | ||||
| 2 | 56/M | + | 129 | 2 | ||||||
| 3 | 50/M | + | + | + | 482 | 5 | + | |||
| 4 | 51/M | + | + | + | + | + | 246 | 5 | + | |
| 5 | 60/M | + | + | + | 298 | 5 | + | |||
| 6 | 68/M | + | + | 75 | 5 | |||||
| 7 | 74/M | + | + | + | 1669 | 4 | + | |||
| 8 | 59/F | + | + | 152 | 6 | + | ||||
| 9 | 63/F | + | + | 197 | 0 | |||||
| 10 | 65/M | + | + | + | + | 452 | 9 | + | ||
| Total cases | 70% | 30% | 80% | 10% | 70% | 10% | ||||
Serum IgE: normal range, <360 IU/ml; blood eosinophils: normal range, <10.0%.
The 10 patients who had CRS manifestations had rhinorrhea, nasal obstruction, postnasal drip, anosmia, and so on. These cases tended to have symptoms correlated with secretion such as rhinorrhea (70%) and postnasal drip (80%). Local findings and CT images of all CRS cases are summarized in Figure 1. Endoscopic findings demonstrated that not all cases had polyp formation, and those that did showed multiple small polyps. There were many cases of allergic rhinitis (70%), but bronchial asthma was not seen as often (10%) as allergic diseases. The peripheral blood eosinophil counts were almost normal in the 10 patients except in case no. 1, and serum IgE presented with a high level in 3 patients (case nos 3, 7, and 10). Biochemistry examination implied pancreatic or biliary system disorder in some patients.
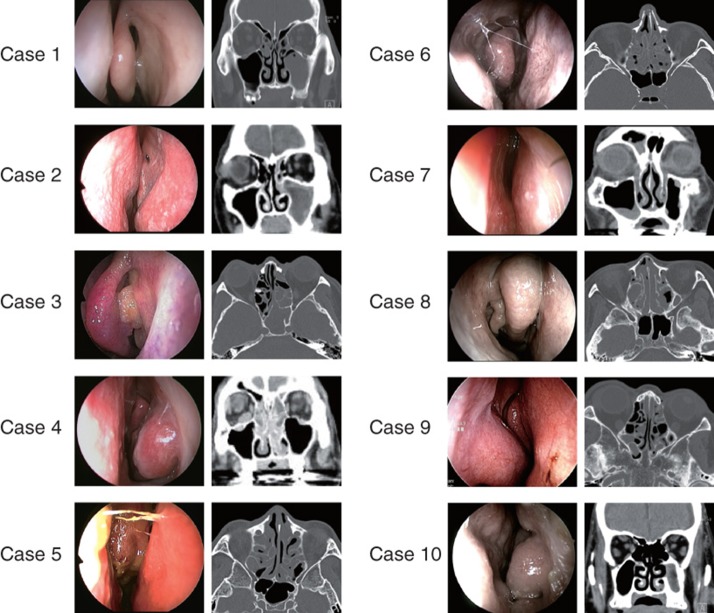
Figure 1.
Endoscopic findings and CT images in all cases. These cases presented various nasal cavity views such as swelling, polyps, and rhinorrhea. Case nos 1 and 2 exhibited unilateral maxillary sinus lesion with bony thickness. The other cases had diffuse mucous lesions mainly in the ethmoid sinuses.
Effect of oral prednisolone treatment
All of the patients who had swelling of the submandibular gland (case nos 1–5 and 7) had significantly reduced swelling within 3–4 days after starting prednisolone administration. After approximately 3 months of prednisolone administration, at the point when it was possible to reduce the dosage to 5–15 mg/day, the characteristic findings of AIP were improved in six patients, except case no. 6, with the enlargement of the pancreas and the irregular narrowing of the main pancreatic duct improved. Serum IgG and IgG4 levels were also markedly decreased. Nose, nasal discharge, and obstruction symptoms were also improved.
Endoscopic findings were improved in six of seven cases treated with prednisolone (Figure 2). After oral prednisolone treatment, along with improvement of the symptoms, nasal sinus CTs also revealed improvement of the sinus opacification in six of seven patients. In these patients, serum IgG4 levels were markedly decreased. In case no. 6 only, there was no significant improvement of CT findings, the score was exacerbated, and the serum IgG4 level was only slightly decreased (Table III).
Figure 2.
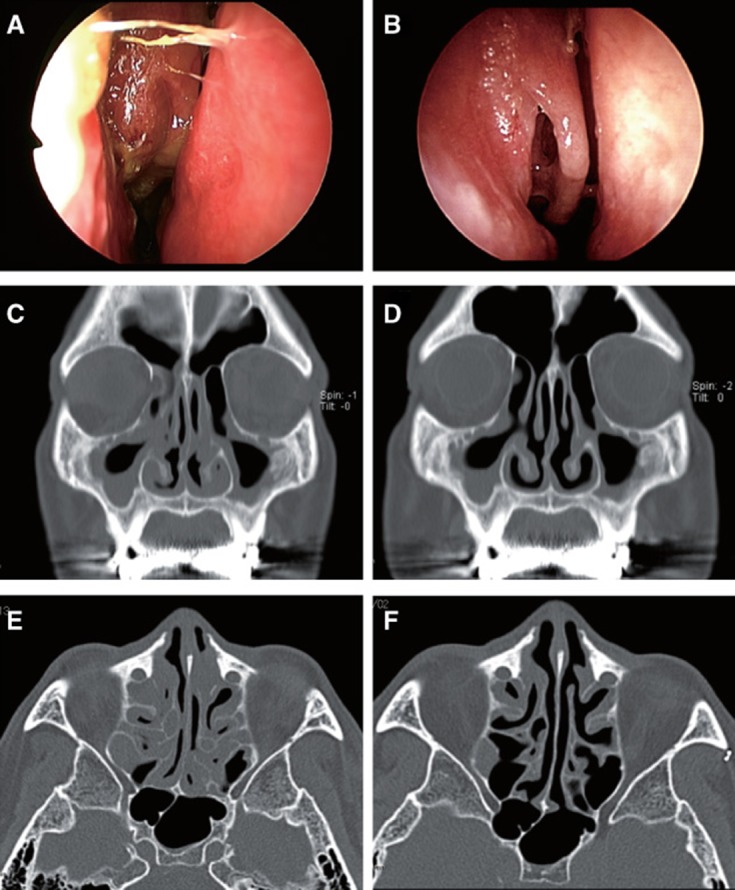
Endoscopic findings of right side nose and CT (coronal and axial) images in case no. 5. (A), (C), and (E) show status before steroid therapy. CT showed bilateral opaque areas located in maxillary and ethmoid sinus with a diffuse liquid pattern. Nasal discharge and nasal crusting were observed. (B), (D), and (F) show status after steroid therapy; these finding showed improvement of sinusitis, respectively.
Table III.
Clinical effects of prednisolone treatment for IgG4-related CRS.
| Case no. | Age/gender | Pretreatment |
Treatment |
Post-treatment |
Recovery ratio |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IgG (mg/dl) | IgG4 (mg/dl) | CT score | PSL | IgG (mg/dl) | IgG4 (mg/dl) | CT score | IgG (%) | IgG4(%) | CT score (%) | ||
| 1 | 55/M | 5545 | 2970 | 11.0 | + | 1579 | 969 | 1.0 | 71.5 | 67.4 | 90.9 |
| 2 | 56/M | 2377 | 387 | 11.0 | + | 912 | 81 | 1.7 | 61.6 | 79.1 | 84.5 |
| 3 | 50/M | 2001 | 773 | 32.3 | + | 1132 | 190 | 11.0 | 43.4 | 75.4 | 65.9 |
| 4 | 51/M | 2741 | 1610 | 16.3 | + | 955 | 319 | 7.3 | 65.2 | 80.2 | 55.2 |
| 5 | 60/M | 3767 | 1910 | 16.3 | + | 1076 | 202 | 6.7 | 71.4 | 89.4 | 58.9 |
| 6 | 68/M | 2112 | 209 | 17.0 | + | 1185 | 174 | 21.0 | 43.9 | 16.7 | −23.5 |
| 7 | 74/M | 3092 | 1550 | 11.7 | + | 1028 | 383 | 3.0 | 66.8 | 75.3 | 74.4 |
| 8 | 59/F | 1159 | 364 | 22.7 | None | 1132 | 384 | 22.7 | 2.3 | −5.5 | 0 |
| 9 | 63/F | 2759 | 1500 | 4.3 | None | 2680 | 1850 | 4.0 | 2.9 | −23.3 | 6.97 |
| 10 | 65/M | 2631 | 1570 | 2.7 | None | 2697 | 1460 | 2.7 | −2.5 | 7.0 | 0 |
| Average of treatment cases | |||||||||||
| Nos 1–7 | 59.8 | 2681.7 | 1073.2 | 17.4 | + | 1048.0 | 224.8 | 8.5 | 58.7 | 69.4 | 52.6* |
| Average of nontreatment cases | |||||||||||
| Nos 8–10 | 62.3 | 2183.0 | 1144.7 | 9.9 | None | 2169.7 | 1231.3 | 9.8 | 0.9 | −7.3 | 2.3* |
CRS, chronic rhinosinusitis; AIP, autoimmune pancreatitis; MD, Mikulicz disease; PSL, prednisolone treatment. Recovery ratio: 1 – (post-treatment score ÷ pretreatment score) ×100.
*p = 0.008 (t test).
The recovery ratio clearly showed the effectiveness of oral prednisolone treatment (Table III). Comparison between treated cases and non-treated cases identified significant differences in CT scores with recovery ratio.
Histological evaluation
With regard to histological and immunohistochemical findings, serum IgG4 in IgG4-related patients who had CRS manifestations was significantly higher than serum IgG4 in the control group (p < 0.05; 1530 ± 1012.9 mg/dl, 46.8 ± 39.2 mg/dl, respectively) (Table IV).
Table IV.
Pathological findings in IgG4-related CRS and common CRS cases.
| Case nos | Age/gender | Nasal manifestations | Serum IgG4 (mg/dl) | IgG4-positive plasma cell infiltration in nasal mucosa |
|---|---|---|---|---|
| IgG4-related CRS | ||||
| 1 | 55/M | NC, AR | 2970 | Severe |
| 2 | 56/M | NC | 387 | Severe |
| 3 | 50/M | NP, AR | 773 | Severe |
| 4 | 51/M | NP, AR | 1610 | Moderate |
| 5 | 60/M | NP, AR | 1910 | Severe |
| Controls | ||||
| 1 | 41/M | NP | 64 | Severe |
| 2 | 64/M | AR, NC | 22 | Mild |
| 3 | 60/F | NP | 15 | Severe |
| 4 | 58/F | NP, AR | 108 | Severe |
| 5 | 33M | NP | 25 | Moderate |
AR, allergic rhinitis; NC, nasal crusting; NP, nasal polyposis.
Histological findings of nasal mucosa revealed diffuse inflammatory changes with plasma cells, and scattered eosinophil infiltration in the IgG4-related patient group and control group, with no significant differences (Figure 3).
Figure 3.
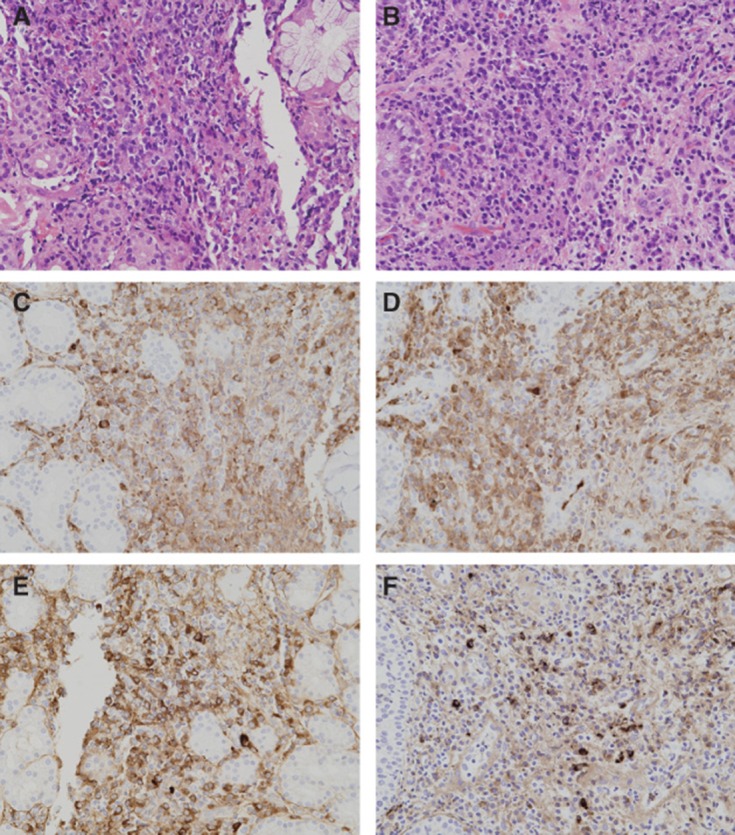
H&E staining of nasal mucosa specimens of patient with IgG4-related CRS (A) and common CRS (B) (original magnification ×100). Numerous lymphoplasmacytic and scattered eosinophil infiltrations with fibrosis are shown in both (A) and (B). There are no significant differences in the degree of infiltrations in each nasal mucosa. IgG and IgG4 immunostaining of nasal mucosa of patient with IgG4-related CRS (C and E) and common CRS (D and F). (C) and (D), (E) and (F) were shown to be infiltrated with IgG-positive and IgG4-positive plasma cells, respectively.
In immunohistochemical examination numerous IgG4-positive plasma cell infiltrations were observed in specimens of the IgG4-related patient group. Surprisingly, the magnitude of IgG4-positive plasma cell infiltration in the control group was almost the same as in the IgG4-related patient group (Table IV), and the IgG4-positive plasma cell/IgG-positive plasma cell ratios were not particularly different between the IgG4-related patient group and the control group. Immunohistochemical findings of IgG-4 and IgG are shown in Figure 3.
Discussion
Our study suggests the strong possibility of sinusitis as one of the complications of extrapancreatic lesions of AIP. This hypothesis is supported by the following findings: 1) 10 patients who were diagnosed with IgG4-related disease had sinusitis (10/31, 32%), 2) systemic glucocorticoid therapy for the treatment of AIP was also effective for the rhinosinus lesions, 3) the therapeutic efficacy for IgG4-related patients who had CRS correlated with the decreased serum IgG4 level, and the one recurrent AIP patient also demonstrated recurrent sinusitis during the tapering oral glucocorticoid therapy. We suggest IgG4-related CRS as a new clinical entity of nasal disease.
Following many reports regarding IgG4-related disease, it is now widely accepted that IgG4 has the possibility to affect various organs and cause diseases that present with inflammatory lesions [1–5]. Although many extrapancreatic lesions associated with AIP have been reported [1–5], all of those lesions had abundant IgG4-bearing plasma cell infiltrations. The concept of a spectrum of IgG4-related disease entities has expanded to the liver, lung, aortic aneurysms, and so on, even when there are no elevated serum IgG4 levels or conditions symptomatic of AIP. Recently, a single case report described unilateral sinusitis associated with IgG4-related disease [17]. Our series of IgG4-related cases had nasal symptoms and exhibited lesions in the sinonasal area on CT findings. In this study, CRS was seen at a high rate in patients with IgG4-related diseases (32%). This proportion seems to be quite a bit higher than that seen in the general population. Bousquet et al. have reported that CRS affects approximately 16% of the total population in the United States in the National Institute of Allergy and Infectious Diseases Fact Sheet [18]. Allergic rhinitis, diagnosed by nasal smear eosinophil and local findings, was present in 7/10 (70%) patients, and thus these results provide support for IgG4-related disease involving an allergic reaction. Characteristic findings of this condition were not observed in local findings and CT findings. CT findings exhibited broadly two patternings in opacification of nasal sinuses; unilateral maxillary sinus with solid-like lesion and bilateral ethmoid sinus diffuse liquid lesion. Previous reports suggested that there were some variations in imaging findings for IgG4-related disease involved in lung [4], indicating that there is adequate support for the CT findings in this study. On the other hand, many nasal symptoms were rhinorrhea and post nasal drip as compared with nasal obstruction and anosmia. These results indicate that symptoms with secretion from the sinonasal cavity were a well-characterized feature of IgG4-related CRS.
Previous reports described pulmonary manifestations of AIP such as interstitial pneumonia, inflammatory pseudotumor, and especially in central airway stenosis involvements, so it has been supposed that IgG4-related disease may involve sinonasal disease in view of the strong relation between sinonasal disease and lower airway disease. Interestingly, the present study showed that 6 of 10 patients (interstitial pneumonia, 2; central airway stenosis, 2; mediastinal lymphadenopathy, 4; each overlapping) with IgG4-related CRS had pulmonary manifestations (Table I), suggesting that CRS is closely associated with pulmonary lesions in IgG4-related disease as well. Nine of 10 patients had MD, also suggesting close association with MD (Table I), supporting a recent concept that MD is one of the IgG4-related diseases [13].
Although the optimal treatment of IgG4-related disease has not been established, several previous reports suggested good response to steroids based on evidence of AIP treatment [19]. However, in some cases of AIP treatment was likely to be ineffective or there was a relapse during steroid tapering [20]. In this study, the IgG4-related CRS cases showed response to steroid therapy; most cases (6/7, 86%) had improvement of symptoms and CT findings, which was relative to the decrease in their serum IgG4 levels. Case no. 6 showed AIP relapse during reduction of prednisolone dosage, and an unstable state with pancreatic and bile duct function in the laboratory data. Also the serum IgG4 level was not decreased to the same extent as in the other cases treated with oral steroids (Table III). So the prednisolone could not be reduced to a maintenance dosage, and was increased to 20 mg. It seems that IgG4-related disease has nasal manifestations reflected in the state of this disease.
Concerning diagnostic criteria, there are many reports of IgG4-related disease diagnosed pathologically with histological and immunohistological findings, which do not necessarily require involvement of AIP. In this study, we found a large amount of IgG4-bearing plasma cell infiltrations in the mucosal tissues of patients with sinusitis associated with IgG4-related disease. However the control group, i.e. common CRS patients, also had IgG4-bearing plasma cell infiltrations in their nasal mucosa, and there were no significant differences between the IgG4-related CRS and control groups (Figure 3). Immunostaining of IgG4 and IgG was used to evaluate the ratio of IgG4-positive plasma cells/IgG-positive plasma cells in detail, but no evidence discriminating the two groups was found. Therefore, in nasal mucosa positive staining of IgG4 is not specific for the definition of IgG4-related disease. Thus caution is required when diagnosing IgG4-related CRS. Ishida et al. reported it as ‘IgG4-related sclerosing lesions in the maxillary sinus’ in a patient with normal serum IgG4 levels [21]. This patient did not show any other IgG4-related clinical manifestations. It was uncertain by the diagnosis only for immunohistological evaluation. Together with the present results, immunohistochemical study of IgG4 can not be used for differential diagnosis of IgG4-related CRS. The result of serum IgG4 level is necessary for diagnosis of this disease.
One of the most common health issues, common CRS, can usually be successfully treated by traditional therapy and surgery but cases in which these are not effective are sometimes seen. Frequent complications of viral, fungal, or bacterial processes are seen but it must be noted that infection is not always present, as evidenced by the manifestation of CRS in systemic disorders such as Churg-Strauss syndrome, or Wegener's granulomatosis. CRS involved with IgG4-related disease should also be considered as systemic disease for which surgical treatment may not be effective. In patients showing signs and symptoms that may be AIP and/or MD, we should consider the possibility of a diagnosis of IgG4-related CRS. We conclude that sinus lesion as likely CRS is one of the extrapancreatic manifestations of AIP and/or MD. This type of sinusitis is a new clinical entity of nasal disease associated with high levels of serum IgG4, and is effectively treated by steroid therapy.
Acknowledgments
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- [1].Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001;344:732–8. doi: 10.1056/NEJM200103083441005. [DOI] [PubMed] [Google Scholar]
- [2].Kawa S, Hamano H. Clinical features of autoimmune pancreatitis. J Gastroenterol. 2007;42:9–14. doi: 10.1007/s00535-007-2044-x. [DOI] [PubMed] [Google Scholar]
- [3].Hamed G, Tsushima K, Yasuo M, Kubo K, Yamazaki S, Kawa S, et al. Inflammatory lesions of the lung, submandibular gland, bile duct and prostate in a patient with IgG4-associated multifocal sysytemic fibrosis. Respirology. 2007;12:455–7. doi: 10.1111/j.1440-1843.2007.01053.x. [DOI] [PubMed] [Google Scholar]
- [4].Kobayashi H, Shimokawaji T, Kanoh S, Motoyoshi K, Aida S. IgG4-positive pulmonary disease. J Thorac Imaging. 2007;22:360–2. doi: 10.1097/RTI.0b013e31813fab9f. [DOI] [PubMed] [Google Scholar]
- [5].Ito M, Yasuo M, Yamamoto H, Tsushima K, Tanabe T, Yokoyama T, et al. Central airway stenosis in a patient with autoimmune pancreatitis. Eur Respir J. 2009;33:680–3. doi: 10.1183/09031936.00051408. [DOI] [PubMed] [Google Scholar]
- [6].Uehara T, Hamano H, Kawakami M, Koyama M, Kawa S, Sano K, et al. Autoimmune pancreatitis-associated prostatitis: distinct clinicopathological entity. Pathol Int. 2008;58:118–25. doi: 10.1111/j.1440-1827.2007.02199.x. [DOI] [PubMed] [Google Scholar]
- [7].Hamano H, Arakura N, Muraki T, Ozaki Y, Kiyosawa K, Kawa S. Prevalence and distribution of extrapancreatic lesions complicating autoimmune pancreatitis. J Gastroenterol. 2006;41:1197–205. doi: 10.1007/s00535-006-1908-9. [DOI] [PubMed] [Google Scholar]
- [8].Kawaguchi K, Koike M, Tsuruta K, Okamoto A, Tabata I, Fujita N. Lymphoplasmacytic sclerosing pancreatitis with cholangitis: a variant of primary sclerosing cholangitis extensively involving pancreas. Hum Pathol. 1991;22:387–95. doi: 10.1016/0046-8177(91)90087-6. [DOI] [PubMed] [Google Scholar]
- [9].Hamano H, Kawa S, Ochi Y, Unno H, Shiba N, Wajiki M, et al. Hydronephrosis associated with retroperitoneal fibrosis and sclerosing pancreatitis. Lancet. 2002;359:1403–4. doi: 10.1016/s0140-6736(02)08359-9. [DOI] [PubMed] [Google Scholar]
- [10].Kamisawa T, Okamoto A. IgG4-related sclerosing disease. World J Gastroenterol. 2008;14:3948–55. doi: 10.3748/wjg.14.3948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Van der Vliet HJ, Perenboom RM. Multiple pseudotumors in IgG4-associated multifocal systemic fibrosis. Ann Intern Med. 2004;141:896–7. doi: 10.7326/0003-4819-141-11-200412070-00033. [DOI] [PubMed] [Google Scholar]
- [12].Morgan WS, Castleman B. A clinicopathologic study of “Mikulicz's disease”. Am J Pathol. 1953;29:471–503. [PMC free article] [PubMed] [Google Scholar]
- [13].Geyer JT, Ferry JA, Harris NL, Stone JH, Zukerberg LR, Lauwers GY, et al. Chronic sclerosing sialadenitis (Küttner tumor) is an IgG4-associated disease. Am J Surg Pathol. 2010;34:202–10. doi: 10.1097/PAS.0b013e3181c811ad. [DOI] [PubMed] [Google Scholar]
- [14].Rosenfeld RM, Andes D, Bhattacharyya N, Cheung D, Eisenberg S, Ganiats TG, et al. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg. 2007;137:S1–S3. doi: 10.1016/j.otohns.2007.06.726. [DOI] [PubMed] [Google Scholar]
- [15].Kennedy DW, Kuhn FA, Hamilos DL, Zinreich SJ, Butler D, Warsi G, et al. Treatment of chronic rhinosinusitis with high-dose oral terbinafine: a double blind, placebo-controlled study. Laryngoscope. 2005;115:1793–9. doi: 10.1097/01.mlg.0000175683.81260.26. [DOI] [PubMed] [Google Scholar]
- [16].Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38:982–4. doi: 10.1007/s00535-003-1175-y. [DOI] [PubMed] [Google Scholar]
- [17].Ikeda R, Awataguchi T, Shoji F, Oshima T. A case of paranasal sinus lesion in IgG4-related sclerosing disease. Otolaryngol Head Neck Surg. 2010;142:458–9. doi: 10.1016/j.otohns.2009.09.019. [DOI] [PubMed] [Google Scholar]
- [18].Bousquet J, Bachert C, Canonica G, Casale T, Cruz A, Lockey R, et al. Unmet needs in severe chronic upper airway disease (SCUAD) J Allergy Clin Immunol. 2009;124:428–33. doi: 10.1016/j.jaci.2009.06.027. [DOI] [PubMed] [Google Scholar]
- [19].Ghazale A, Chari ST. Optimising corticosteroid treatment for autoimmune pancreatitis. Gut. 2007;56:1650–2. doi: 10.1136/gut.2007.129833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Kawa S, Hamano H, Ozaki Y, Ito T, Kodama R, Chou Y, et al. Long-term follow up of autoimmune pancreatitis: characteristics of chronic disease and recurrence. Clin Gastroenterol Hepatol. 2009;7:S18–S22. doi: 10.1016/j.cgh.2009.07.041. [DOI] [PubMed] [Google Scholar]
- [21].Ishida M, Hotta M, Kushima R, Shibayama M, Shimizu T, Okabe H. Multiple IgG4-related sclerosing lesions in the maxillary sinus, parotid gland and nasal septum. Pathol Int. 2009;59:670–5. doi: 10.1111/j.1440-1827.2009.02425.x. [DOI] [PubMed] [Google Scholar]