Abstract
Objectives. We evaluated whether sexual compulsivity fits into a syndemic framework, in which sexual compulsivity is one of a number of co-occurring psychosocial health problems that increase HIV risk among men who have sex with men (MSM).
Methods. In 2003 and 2004, we conducted an anonymous cross-sectional survey of MSM in New York City (n = 669) by approaching attendees at gay, lesbian, and bisexual community events. We analyzed data by bivariate and multivariate logistic regression.
Results. We found strong positive interrelationships among syndemic factors including sexual compulsivity, depression, childhood sexual abuse, intimate partner violence, and polydrug use. In bivariate analyses, all syndemic health problems except for childhood sexual abuse were positively related to HIV seropositivity and high-risk sexual behavior. Our multivariate models revealed an array of interrelationships among psychosocial health problems. We found amplified effects of these problems on HIV seropositivity and on the likelihood of engaging in high-risk sexual behavior.
Conclusions. Our findings support the conclusion that sexual compulsivity is a component of a syndemic framework for HIV risk among MSM. HIV prevention interventions should consider the overlapping and compounding effects of psychosocial problems, including sexual compulsivity.
In 2001, researchers suggested that the United States was likely to experience a resurgence in HIV infections among men who have sex with men (MSM) in the wake of increases in sexual risk practices.1 This prediction appears to have been valid because the number of HIV/AIDS diagnoses among MSM increased 8.6% from 2001 to 2006,2 and MSM remain disproportionately affected by HIV, accounting for 53% of new HIV cases in 2006.3 Although questions remain regarding the statistical significance of these increases in HIV incidence among MSM, the mean incidence rate of HIV among MSM in the United States is 2.39%, which, if sustained, will result in 40% of MSM being HIV positive by age 40.4
A syndemic occurs when multiple epidemics and risk factors interact and connect with one another, synergistically compounding the risk and consequences of disease.5–8 These epidemics and risk factors develop in conditions of health and social disparities, often within specific marginalized groups, such as MSM. Researchers have applied the syndemic framework to HIV risk among MSM, finding considerable empirical support for a model in which co-occurring psychosocial health problems (e.g., childhood sexual abuse, depression, substance use, intimate partner violence) compound the risk of HIV among MSM.9–11 For example, in their Urban Men's Health Study of MSM in 4 US cities Stall et al. found that as the number of psychosocial health problems among MSM increased, the odds of reporting HIV sexual risk behavior and HIV prevalence increased.9 Mustanski et al.11 found the same association among psychosocial health problems and increased HIV risk among young urban MSM. Together, these studies indicate that problems such as sexual abuse, depression, polydrug use, and partner violence have an additive effect on sexual risk practices and the HIV epidemic.
Too little research has been conducted on the potential mechanisms of action that drive these co-occurring syndemic factors among MSM. Mustanski et al.11 posited that sensation seeking and impulsivity, reliance on gay bars and sexually charged venues, and stigma and victimization could have an effect on multiple risk factors, resulting in a syndemic among MSM. Minority stress may also contribute to the co-occurrence of syndemic health problems.12 For example, chronic stress resulting from stigmatization as a sexual minority may lead MSM to experience depression, enter into violence-prone partnerships, or use illicit drugs to alleviate stress and stigma. A limitation of the minority stress model, however, is that it does not include childhood sexual abuse as a syndemic factor in most analyses.
Another factor that has frequently been associated with HIV sexual risk behaviors among MSM is sexual compulsivity. For men and women, sexual compulsivity is characterized by sexual fantasies and behaviors that increase in intensity and frequency over time so as to interfere with personal, interpersonal, or vocational pursuits.13–16 Compared with MSM who lack this characteristic, MSM with sexual compulsivity experience higher rates of unprotected anal intercourse, greater numbers of sexual partners (including HIV-serodiscordant partners), more sexual intercourse under the influence of drugs, higher incidence of HIV and sexually transmitted infections, increased identification as a barebacker (one who has intercourse without condoms), less disclosure of HIV status to sexual partners, and lower condom use self-efficacy.14,17–23
Researchers have demonstrated individual connections between sexual compulsivity and many of the psychosocial problems that have also been identified as syndemic factors related to HIV risk among MSM, such as childhood sexual abuse, depression, and substance use.17,24–26 The minority stress model suggests that engagement in compulsive sexual behaviors among MSM may stem, in part, from their stress and stigmatization as a sexual minority. However, studies have not focused specifically on sexual compulsivity as a potential syndemic factor related to HIV sexual risk and HIV prevalence among MSM. We examined the co-occurrence of sexual compulsivity with other psychosocial health problems previously identified as syndemic factors in an urban sample of MSM. We aimed to assess whether and how sexual compulsivity fits into the syndemic framework.
METHODS
In 2003 to 2004, we adapted a cross-sectional street-intercept method27 to anonymously survey 2361 gay and bisexual men at a series of gay, lesbian, and bisexual community events in New York City through the Sex and Love Study version 2.0.28–30 This approach to collecting data has been used in numerous studies,31–34 some of which focused on MSM.35,36 It has been shown to provide data that are comparable to those obtained from more methodologically rigorous approaches,37 such as time–space sampling.
At each 2-day-long community event, the research team hosted a booth, and a member of the team actively approached each person who passed the booth. The response rate was high, with 82.9% of those approached consenting. The survey required 15 to 20 minutes to complete, and we handed participants the survey on a clipboard so they could step away from others to complete the questionnaire privately. Participants deposited their own completed survey into a secure box at the booth. As an incentive, participants received a voucher for free admission to a movie. We entered survey data into a database in SPSS version 17.0 (SPSS Inc, Chicago, IL) and checked them for accuracy.
Of the 2361 men surveyed, 669 completed a version of the survey that included the complete set of measures we analyzed for this study. We found no significant differences in demographic characteristics among participants completing different survey versions.
Measures
Participant characteristics.
Participants indicated their age (in years), sexual identity, education (in ordinal categories), HIV status, and race/ethnicity. High-risk sexual behavior was defined as recent (< 90 days) unprotected anal intercourse with a nonprimary partner who was of known discordant or unknown HIV status (1 = yes, 0 = no).
Psychosocial health problems.
We adopted standard measures, such as those Stall et al. used in the Urban Men's Health Study,9 to measure psychosocial health problems. We defined polydrug use as the use of 3 or more recreational drugs in the past 90 days (methamphetamine, cocaine, crack, MDMA [ecstasy], ketamine, marijuana, or nitrate inhalants [poppers]). We used the Center for Epidemiological Studies Depression Scale to evaluate depression,38 and we defined scores higher than 22 as indicating depression symptomatology (α = 0.87; mean = 22.22; SD = 10.36), consistent with previous research.9,39–42
Partner violence was the experience of any form of violence in the past 5 years at the hands of a primary partner, both symbolic (e.g., “verbally threatened you,” “stalked you”) and physical (e.g., “hit you,” “kicked you”).43 Consistent with the Urban Men's Health Study,9 we defined childhood sexual abuse as the experience of being “forced or frightened by someone into doing something sexually” with a partner more than 10 years older than the respondent when the respondent was aged 16 years or younger.44 Finally, although no official diagnostic criteria for sexual compulsivity existed at the time of our study, we used the Sexual Compulsivity Scale (α = 0.90), the most widely published measure of sexual compulsivity among MSM.45 Consistent with existing literature,17,25,46–49 we defined scores of 24 and above as indicating sexual compulsivity (mean = 17.50; SD = 6.56; range = 10–40).
Analyses
We undertook analyses in 4 steps. First, we computed the prevalence of each psychosocial health problem. Second, similar to Mustanski et al.,11 we calculated bivariate odds ratios for each pair of variables to determine whether the 5 psychosocial health problems clustered together. We also included odds ratios for each psychosocial health problem and for HIV status and high-risk sexual behavior. Third, and consistent with Stall et al.,9 we used a set of multivariate logistic regression models to create separate profiles of MSM who reported high levels of polydrug use, depression, childhood sexual abuse, partner violence, and sexual compulsivity.
Each of these models used the same set of demographic and behavioral independent variables. We ran the same logistic model for each of the health problems (polydrug use, depression, childhood sexual abuse, partner violence, sexual compulsivity) but excluded measures of a given problem from the logistic regression models of that problem. Finally, we calculated the prevalence of HIV seropositivity and high-risk sexual behavior for each possible count score of psychosocial health problems. We used the Mantel–Haenszel χ2 test for linear association and γ to test the strength and direction of this association.
RESULTS
Table 1 shows characteristics of the sample (n = 669). Participant age ranged from 18 to 77 years (mean = 37.7; SD = 11.3), and 38% were persons of color. Most men identified as gay (88.8%) or bisexual (8.5%); the rest failed to disclose their sexual orientation but reported having sexual intercourse with men. Most men (87.4%) were HIV negative, 10.8% were HIV positive, and 1.8% failed to report their status or were untested. A total of 11.5% of men reported high-risk sexual behavior in the past 90 days. The data revealed a high prevalence of psychosocial health problems: 47.4% of men displayed depression symptoms, 21.5% had experienced partner violence in the previous 5 years, 19.3% indicated symptoms of sexual compulsivity, 10.2% had experienced sexual abuse as a child, and 8.4% had engaged in polydrug use in the past 90 days.
TABLE 1—
Characteristics of Men Who Have Sex With Men: Sex and Love Study Version 2.0, New York City, 2003–2004
| Characteristic | No. (%) |
| Education | |
| ≤ high school | 52 (7.7) |
| Some college | 180 (26.9) |
| College degree | 216 (32.3) |
| Graduate school | 215 (32.2) |
| Race | |
| African American | 69 (10.3) |
| Asian/Pacific Islander | 40 (6.0) |
| White/European | 413 (61.7) |
| Latino | 96 (14.3) |
| Other/multiracial | 47 (7.0) |
| Income, $ | |
| < 19 999 | 115 (17.2) |
| 20 000–39 999 | 155 (23.2) |
| 40 000–59 999 | 166 (24.8) |
| 60 000–99 999 | 156 (23.2) |
| ≥ 100 000 | 64 (9.6) |
| Age, y | |
| 18–29 | 171 (25.6) |
| 30–39 | 229 (34.2) |
| 40–49 | 159 (23.8) |
| ≥ 50 | 108 (16.1) |
| Sexual identitya | |
| Gay | 594 (88.8) |
| Bisexual | 57 (8.5) |
| HIV status | |
| Negative | 585 (87.4) |
| Positive | 72 (10.8) |
| Unknown/undisclosed | 12 (1.8) |
| Unprotected anal intercourse with HIV-serodiscordant or unknown-status partner in past 90 db | |
| No | 470 (70.3) |
| Yes | 77 (11.5) |
| Syndemic health problemsc | |
| Polydrug use (valid n = 652) | 56 (8.4) |
| Depressiond (valid n = 660) | 317 (47.4) |
| Childhood sexual abuse (valid n = 669) | 68 (10.2) |
| Partner violence (valid n = 649) | 144 (21.5) |
| Sexual compulsivitye (valid n = 666) | 129 (19.3) |
Note. The sample size was n = 669.
Percentages do not add up to 100% because the additional men did not report this information.
Some participants (18.2%; n = 122) did not provide a response to this question. Men who were in monogamous relationships were excluded (n = 198).
Percentages reported for syndemic health problems are out of the total sample. Valid n corresponds to the portion of participants for whom complete data are available.
Center for Epidemiological Studies Depression Scale score > 22.
Sexual Compulsivity Scale score ≥ 24.
Bivariate Associations and Odds Ratios
Table 2 presents bivariate associations and odds ratios of psychosocial health problems, high-risk sexual behavior, and HIV status. Associations among psychosocial health problems were striking: of the 10 odds ratios calculated among psychosocial health problems, 7 were significant and positive. For example, men who were experiencing symptoms of sexual compulsivity had 3.95 higher odds of being depressed, 2.20 higher odds of experiencing childhood sexual abuse, and 2.56 higher odds of experiencing intimate partner violence in the past 5 years compared with participants who were not sexually compulsive.
TABLE 2—
Bivariate Associations Among Psychosocial Health Problems, Sexual Risk Behavior, and HIV Status Among Men Who Have Sex With Men: Sex and Love Study Version 2.0, New York City, 2003–2004
| Polydrug Use | Depression |
Childhood Sexual Abuse |
Partner Violence |
Sexual Compulsivity |
HIV Positive |
High-Risk Sexual Behavior |
|||||||
| Valid No. | OR (95% CI) | Valid No. | OR (95% CI) | Valid No. | OR (95% CI) | Valid No. | OR (95% CI) | Valid No. | OR (95% CI) | Valid No. | OR (95% CI) | ||
| Polydrug use | 643 | 1.54 (0.87, 2.72) | 652 | 0.80 (0.33, 2.24) | 633 | 1.91** (1.05, 3.49) | 649 | 1.49 (0.78, 2.82) | 652 | 2.18** (1.07, 4.45) | 534 | 5.89† (3.05, 11.38) | |
| Depressiona | 660 | 2.00*** (1.19, 3.53) | 647 | 1.58*** (1.08, 2.29) | 659 | 3.95† (2.56, 6.08) | 660 | 1.77** (1.07, 2.92) | 491 | 2.04*** (1.23, 3.37) | |||
| Childhood sexual abuse | 649 | 2.44† (1.43, 4.19) | 666 | 2.20*** (1.27, 3.80) | 669 | 1.30 (0.62, 2.75) | 547 | 0.69 (0.29, 1.68) | |||||
| Partner violence | 648 | 2.56† (1.67, 3.91) | 649 | 3.06† (1.83, 5.12) | 533 | 2.11*** (1.26, 3.53) | |||||||
| Sexual compulsivityb | 666 | 2.05*** (1.19, 3.53) | 546 | 2.25*** (1.31, 3.86) | |||||||||
| HIV positive | 547 | 5.97† (3.34, 10.65) | |||||||||||
Note. CI= confidence interval; OR = odds ratio. Valid no. is portion of participants for whom complete data are available.
Center for Epidemiological Studies Depression Scale score > 22.
Sexual Compulsivity Scale score ≥ 24.
**P < .05; ***P < .01; †P < .001.
Polydrug use was generally unrelated to other psychosocial health problems, except for intimate partner violence. Except for childhood sexual abuse, psychosocial health problems were all significantly and positively related to HIV seropositivity and high-risk sexual behavior. For example, those who had engaged in high-risk sexual intercourse had 2.25 higher odds of reporting symptoms of sexual compulsivity and 2.11 higher odds of experiencing partner violence than did other respondents. HIV-positive individuals had 3.06 higher odds of reporting partner violence, 2.18 higher odds of reporting polydrug use, 2.05 higher odds of reporting symptoms of sexual compulsivity, and 1.77 higher odds of being depressed than did other respondents.
Multivariate Logistic Regression Analyses
Table 3 shows the multivariate logistic regression models for separate profiles of MSM who reported high levels of polydrug use, depression, childhood sexual abuse, partner violence, and sexual compulsivity. We also report models regressed separately on HIV seropositivity and high-risk sexual behavior. In the multivariate model regressed on polydrug use, only high-risk sexual intercourse (adjusted odds ratio [AOR] = 4.59) and age (AOR = 0.96) revealed significant associations. In the 4 models regressed on psychosocial syndemic factors, sexual compulsivity (AOR = 3.42) and having attended some college (AOR = 1.58) were significantly associated with depression; partner violence (AOR = 2.47) was significantly associated with childhood sexual abuse; sexual compulsivity (AOR = 2.14), childhood sexual abuse (AOR = 2.49), and HIV seropositivity (AOR = 2.81) were significantly associated with partner violence; and depression (AOR = 3.38) and partner violence (AOR = 2.12) were significantly associated with sexual compulsivity.
TABLE 3—
Multivariable Logistic Regressions Among Intersecting Health Problems Among Men Who Have Sex With Men: Sex and Love Study Version 2.0, New York City, 2003–2004
| Dependent Variables |
|||||||
| Independent Variables | Polydrug Use, AOR (95% CI) | Depression, AOR (95% CI) | Childhood Sexual Abuse, AOR (95% CI) | Partner Violence, AOR (95% CI) | Sexual Compulsivity, AOR (95% CI) | HIV Seropositivity, AOR (95% CI) | High-Risk Sexual Behavior, AOR (95% CI) |
| Age, y | 0.96** (0.92, 0.99) | 0.99 (0.97, 1.00) | 0.99 (0.96, 1.02) | 0.99 (0.97, 1.01) | 1.01 (0.99, 1.04) | 1.05† (1.02, 1.08) | 1.00 (0.98, 1.03) |
| Education | |||||||
| ≤ high school | 1.63 (0.47, 5.70) | 1.37 (0.60, 3.15) | 1.56 (0.52, 4.67) | 1.84 (0.77, 4.42) | 1.35 (0.52, 3.49) | 1.63 (0.54, 4.97) | 1.87 (0.64, 5.40) |
| Some college | 0.80 (0.35, 1.83) | 1.58** (1.02, 2.46) | 1.05 (0.52, 2.10) | 1.32 (0.80, 2.18) | 1.03 (0.60, 1.79) | 1.60 (0.82, 3.13) | 1.09 (0.57, 2.08) |
| College degree (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Race | |||||||
| African-American | 1.39 (0.49, 3.95) | 0.63 (0.32, 1.22) | 1.53 (0.56, 4.20) | 0.72 (0.32, 1.60) | 0.88 (0.36, 2.15) | 3.57*** (1.47, 8.68) | 2.25* (0.97, 5.20) |
| Latino | 0.47 (0.13, 1.74) | 0.83 (0.46, 1.49) | 1.51 (0.63, 3.59) | 1.07 (0.55, 2.06) | 1.32 (0.64, 2.70) | 2.85** (1.23, 6.62) | 0.63 (0.24, 1.70) |
| Other | 1.05 (0.38, 2.89) | 0.58* (0.33, 1.04) | 1.69 (0.72, 3.94) | 1.09 (0.57, 2.07) | 1.78* (0.90, 3.52) | 1.15 (0.44, 3.03) | 1.75 (0.79, 3.87) |
| White (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Income, $ | |||||||
| 0–39 999 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ≥ 40 000 | 1.57 (0.74, 3.47) | 0.74 (0.49, 1.11) | 0.97 (0.50, 1.86) | 0.85 (0.53, 1.37) | 1.09 (0.65, 1.84) | 0.91 (0.47, 1.76) | 1.34 (0.71, 2.50) |
| HIV serostatus | |||||||
| Negative/unknown (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | … | 1.00 |
| Positive | 1.33 (0.50, 3.53) | 1.33 (0.71, 2.50) | 1.15 (0.46, 2.91) | 2.81† (1.49, 5.30) | 1.05 (0.51, 2.17) | … | 5.27† (2.66, 10.44) |
| High-risk sexual behavior | 4.59† (2.07, 10.16) | 1.54 (0.86, 2.77) | 0.52 (0.19, 1.44) | 1.41 (0.75, 2.67) | 1.61 (0.83, 3.13) | 5.70† (2.88, 11.28) | … |
| Psychosocial health problems | |||||||
| Polydrug use | … | 1.72 (0.83, 3.55) | 1.17 (0.40, 3.41) | 1.19 (0.54, 2.61) | 1.19 (0.52, 2.75) | 1.23 (0.45, 3.34) | 4.49† (2.06, 9.75) |
| Depressiona | 1.77 (0.80, 3.72) | … | 1.73* (0.92, 3.26) | 0.96 (0.61, 1.51) | 3.38† (2.03, 5.66) | 1.39 (0.73, 2.66) | 1.62 (0.89, 2.96) |
| Childhood sexual abuse | 1.07 (0.35, 3.24) | 1.76* (0.93, 3.36) | … | 2.49*** (1.32, 4.72) | 1.40 (0.69, 2.84) | 1.09 (0.43, 2.75) | 0.51 (0.18, 1.42) |
| Partner violence | 1.17 (0.54, 2.56) | 0.95 (0.60, 1.50) | 2.47*** (1.31, 4.66) | … | 2.12*** (1.25, 3.58) | 3.01† (1.59, 5.69) | 1.48 (0.79, 2.79) |
| Sexual compulsivityb | 1.17 (0.51, 2.71) | 3.42† (2.04, 5.72) | 1.42 (0.71, 2.88) | 2.14*** (1.27, 3.61) | … | 1.02 (0.49, 2.13) | 1.51 (0.77, 2.96) |
| Model statistics | |||||||
| Model r2 (Nagelkerke) | 0.16† | 0.13† | 0.09** | 0.13† | 0.15† | 0.26† | 0.23† |
Note. AOR = adjusted odds ratio; CI = confidence interval. Valid n = 509.
Center for Epidemiological Studies Depression Scale score > 22.
Sexual Compulsivity Scale score ≥ 24.
*P < .10; **P < .05; ***P < .01; †P < .001.
In the model regressed on HIV seropositivity, partner violence (AOR = 3.01), high-risk sexual intercourse (AOR = 5.70), being African American (AOR = 3.57) or Latino (AOR = 2.85), and age (AOR = 1.05) emerged as significant correlates. Finally, in the model regressed on high-risk sexual behavior, polydrug use (AOR = 4.49) and being HIV positive (AOR = 5.27) showed significant correlations.
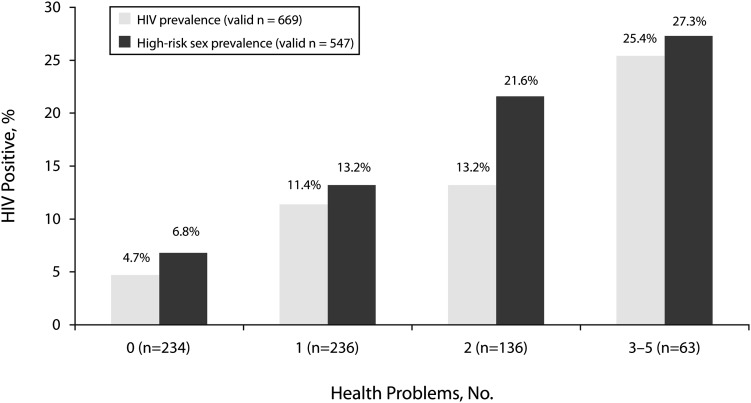
Additive Effects of Psychosocial Problems
Finally, we assessed for additive effects of the 5 psychosocial problems on HIV seropositivity and likelihood of engaging in high-risk sexual behavior. We computed a count score for number of psychosocial health problems (out of 5) reported by each participant. Thirty-five percent (n = 234) of participants reported experiencing no problems, 35.3% (n = 236) reported 1 problem, 20.3% (n = 136) reported 2 problems, and 9.4% (n = 63) reported 3 or more problems. Greater numbers of health problems were significantly and positively associated with HIV infection and current high-risk sexual behavior (Figure 1). For example, 4.7% of men experiencing no psychosocial health problems were HIV positive; 11.4% who reported 1 problem, 13.2% who reported 2 problems, and 25.4% who reported 3 or more problems were HIV positive. For both HIV seropositivity and high-risk sexual intercourse, the Mantel–Haenszel χ2 tests for linear-by-linear association were significant at P < .001 (γ HIV seropositivity = 0.41; γ high-risk sexual intercourse= 0.41). Approximately 41% of the variance in both HIV seropositivity and high-risk sexual behavior was explained by the number of psychosocial health problems.
FIGURE 1—
Number of psychosocial health problems by HIV-seropositive prevalence and by high-risk sexual behavior prevalence among men who have sex with men: New York City, 2003–2004.
Note. Psychosocial health problems were depression, childhood sexual abuse, partner violence, sexual compulsivity, and polydrug use.Source. Sex and Love Study version 2.0.28–30
We reran these analyses with a multivariate logistic regression model with controls for age, education, race, and income, and we obtained substantially the same findings. A greater number of psychosocial health problems was associated with ascending odds ratios (compared with participants who reported no psychosocial health problems) for high-risk sexual behavior (1 problem, AOR = 1.65; 95% confidence interval [CI] = 1.32, 2.07; 2 problems, AOR = 2.73; 95% CI = 1.74, 4.28; 3 problems, AOR = 4.51; 95% CI = 2.30, 8.86; 4 problems, AOR = 7.46; 95% CI = 3.04, 18.34; 5 problems, AOR = 12.33; 95% CI = 4.01, 37.95). The odds for prevalence of HIV seropositivity also rose with number of psychosocial health problems (1 problem, AOR = 1.63; 95% CI = 1.30, 2.05; 2 problems, AOR = 2.66; 95% CI = 1.68, 4.20; 3 problems, AOR = 4.33; 95% CI = 2.18, 8.61; 4 problems, AOR = 7.07, 95% CI = 2.83, 17.64; 5 problems, AOR = 11.52, 95% CI = 3.67, 36.14).
DISCUSSION
We found evidence supporting the inclusion of sexual compulsivity as a syndemic factor related to HIV seropositivity and high-risk sexual behavior among urban MSM. In bivariate analyses, sexual compulsivity was significantly related to 3 of the 4 other syndemic factors, and in multivariate models it was significantly associated with depression and partner violence. In addition, we found strong interrelationships among the psychosocial health problems assessed. When we treated sexual compulsivity as a syndemic factor, we found strong additive associations: the experience of multiple syndemic factors was significantly associated with high-risk sexual behavior and HIV seropositivity. Furthermore, sexual compulsivity was bivariately associated with being HIV positive and reporting unprotected anal intercourse, consistent with previous research.14,17–23
Ours is the first study, to our knowledge, to consider sexual compulsivity within the nexus of syndemic factors associated with HIV infection. Our findings provide empirical support for the inclusion of sexual compulsivity within the broader syndemic framework as applied to MSM; however, further evaluation would be needed to support its extension to other populations. Our results have clear implications for providers seeking to prevent HIV transmissions among MSM. Specifically, our data highlight the need to approach HIV transmission and high-risk sexual behavior within the context of overlapping health problems and to explore all the factors that may underlie these negative conditions. Further research would be well served by a consideration of the elements of the minority stress model12—such as internalized homophobia, expectation of stigma, and the experience of prejudicial events—and how these may play a role in syndemics among MSM. It is possible that interventions designed to alleviate the negative effects of stigma and minority stress could prove useful in ameliorating syndemic factors. Furthermore, mental health providers who treat sexual compulsivity would benefit from a broader consideration of co-occurring factors so that compulsive sexual behaviors are not treated in isolation.
The syndemics framework is an effective theoretical lens through which to view the ways in which multiple psychosocial health conditions may amplify HIV risk, but protective factors that keep men safe and resilient in the face of adversity would also be worth investigating. In our sample, men experiencing 3 or more psychosocial health problems were the most likely to be HIV positive and to report high-risk sexual behavior (compared with men with fewer psychosocial health conditions). Nevertheless, the majority of men experiencing 3 or more problems (72.7%) did not report high-risk sexual intercourse and were HIV negative (74.6%). Research into the protective factors that keep these men HIV negative and sexually safe is essential to developing well-rounded HIV prevention strategies, particularly for those facing multiple psychosocial health problems. The minority stress model could be useful here, because it may be that resilience is associated with better strategies for coping with the stress and stigma associated with being a sexual minority.
Limitations
Our sample comprised only men who attended large-scale gay, lesbian, and bisexual events in New York City; therefore, our data cannot be generalized to all MSM. We analyzed cross-sectional data, so causality between variables should not be inferred; nor do these analyses rule out the potential for confounding effects from other variables not assessed. However, this sampling approach may improve ecological validity for the types of individuals who attend large-scale gay, lesbian, and bisexual events and who compose a considerable (and accessible) portion of the gay, bisexual, and MSM communities in New York City. Although we tried to ensure confidentiality, some responses may have been biased by social desirability in the reporting of sensitive information, which may explain some of the missing data about sexual behavior. Further investigation of these data suggested that missing responses were not related to participants’ age, race, or HIV status (i.e., data were missing at random).
The survey instrument we used assessed a broad range of variables related to psychosocial and sexual health. Such an instrument provides a general perspective about a variety of characteristics but also has limitations. Consistent with the brief street-intercept survey method,27 many questions on our survey were quantitative and closed-ended. We had no information on the amount of time since HIV-positive men were diagnosed. In addition, although the Sexual Compulsivity Scale is among the most widely used and tested scales for detecting symptoms of sexual compulsivity among MSM, no formal diagnostic criteria for sexual compulsivity exist. Finally, all the limitations inherent to self-reported data are applicable.
Conclusions
Our data provide further evidence that multiple factors synergistically affect risky behavior in MSM. It is likely that an HIV prevention cocktail50 may be an effective strategy for working with MSM who demonstrate sexual compulsivity and other syndemic problems. Such a comprehensive approach to HIV risk reduction would necessitate the involvement of a variety of providers, such as clinicians offering therapy or pharmacological treatments for persons with sexual compulsivity or depression, counselors leading group-based approaches to address sexual risk reduction for MSM, and media campaigns focusing on minimizing stigma related to being a sexual minority. Further research in these areas would contribute to our understanding of how syndemic factors interrelate and amplify HIV risk, in addition to helping us determine how such problems may be ameliorated.
Acknowledgments
The Sex and Love version 2.0 project was supported by the Hunter College CHEST.
An earlier version of this article was presented at the 2009 meeting of the International Academy of Sex Research.
We acknowledge the contributions of other members of the CHEST Sex and Love version 2.0 project team: Michael R. Adams, David S. Bimbi, Gideon Feldstein, Catherine Holder, James Kelleher, and Juline A. Koken. We also thank the anonymous reviewers for their insightful feedback on earlier drafts of this article.
Human Participant Protection
All procedures were approved by the Hunter College institutional review board. Because the survey was anonymous, participants provided verbal consent to take part.
References
- 1.Wolitski RJ, Valdiserri RO, Denning PH, Levine WC. Are we headed for a resurgence of the HIV epidemic among men who have sex with men? Am J Public Health. 2001;91(6):883–888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Trends in HIV/AIDS diagnoses among men who have sex with men—33 states, 2001–2006. MMWR Morb Mortal Wkly Rep. 2008;57(25):681–686 [PubMed] [Google Scholar]
- 3.CDC Subpopulation estimates from the HIV incidence surveillance system—United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57(36):985–989 [PubMed] [Google Scholar]
- 4.Stall R, Duran L, Wisniewski SRet al. Running in place: implications of HIV incidence estimates among urban men who have sex with men in the United States and other industrialized countries. AIDS Behav. 2009;13(4):615–629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singer MC, Erickson PI, Badiane Let al. Syndemics, sex and the city: understanding sexually transmitted diseases in social and cultural context. Soc Sci Med. 2006;63(8):2010–2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singer MC, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17(4):423–441 [DOI] [PubMed] [Google Scholar]
- 7.Singer MC. Introduction to Syndemics: A Critical Systems Approach to Public and Community Health. San Francisco, CA: Jossey-Bass; 2009 [Google Scholar]
- 8.Senn TE, Carey MP, Vanable PA. The intersection of violence, substance use, depression, and STDs: testing of a syndemic pattern among patients attending an urban STD clinic. J Natl Med Assoc. 2010;102(7):614–620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stall R, Mills TC, Williamson Jet al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolitski RJ, Stall R, Valdiserri RO, Unequal Opportunities: Health Disparities Affecting Gay and Bisexual Men in the United States. New York, NY: Oxford University Press; 2008 [Google Scholar]
- 11.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parsons JT, Kelly BC, Bimbi DS, Muench F, Morgenstern J. Accounting for the social triggers of sexual compulsivity. J Addict Dis. 2007;26(3):5–16 [DOI] [PubMed] [Google Scholar]
- 14.Kalichman SC, Rompa D. Sexual sensation seeking and sexual compulsivity scales: reliability, validity, and predicting HIV risk behavior. J Pers Assess. 1995;65(3):586–601 [DOI] [PubMed] [Google Scholar]
- 15.Muench F, Parsons JT. Sexual compulsivity and HIV: identification and treatment. Focus. 2004;19(6):1–4 [PubMed] [Google Scholar]
- 16.Kafka MP. Hypersexual disorder: a proposed diagnosis for DSM-V. Arch Sex Behav. 2010;39(2):377–400 [DOI] [PubMed] [Google Scholar]
- 17.Grov C, Parsons JT, Bimbi DS. Sexual compulsivity and sexual risk in gay and bisexual men. Arch Sex Behav. 2010;39(4):940–949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O'Leary A, Wolitski RJ, Remien RHet al. Psychosocial correlates of transmission risk behavior among HIV-seropositive gay and bisexual men. AIDS. 2005;19(suppl 1):S67–S75 [DOI] [PubMed] [Google Scholar]
- 19.Reece M. Sexual compulsivity and HIV serostatus disclosure among men who have sex with men. Sex Addict Compulsivity. 2003;10(1):1–11 [Google Scholar]
- 20.Dilley JW, Loeb L, Marson Ket al. Sexual compulsiveness and change in unprotected anal intercourse: unexpected results from a randomized controlled HIV counseling intervention study. J Acquir Immune Defic Syndr. 2008;48(1):113–114 [DOI] [PubMed] [Google Scholar]
- 21.Semple SJ, Zians J, Grant I, Patterson TL. Sexual compulsivity in a sample of HIV-positive methamphetamine-using gay and bisexual men. AIDS Behav. 2006;10(5):587–598 [DOI] [PubMed] [Google Scholar]
- 22.Benotsch EG, Kalichman SC, Cage M. Men who have met sex partners via the Internet: prevalence, predictors, and implications for HIV prevention. Arch Sex Behav. 2002;31(2):177–183 [DOI] [PubMed] [Google Scholar]
- 23.Coleman E, Horvath KJ, Miner Met al. Compulsive sexual behavior and risk for unsafe sex among Internet using men who have sex with men. Arch Sex Behav. 2010;39(5):1045–1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bancroft J, Vukadinovic Z. Sexual addiction, sexual compulsivity, sexual impulsivity, or what? Toward a theoretical model. J Sex Res. 2004;41(3):225–234 [DOI] [PubMed] [Google Scholar]
- 25.Kalichman SC, Rompa D. The Sexual Compulsivity Scale: further development and use with HIV-positive persons. J Pers Assess. 2001;76(3):379–395 [DOI] [PubMed] [Google Scholar]
- 26.Parsons JT, Kelly BC, Bimbi DS, DiMaria L, Wainberg ML, Morgenstern J. Explanations for the origins of sexual compulsivity among gay and bisexual men. Arch Sex Behav. 2008;37(5):817–826 [DOI] [PubMed] [Google Scholar]
- 27.Miller KW, Wilder LB, Stillman FA, Becker DM. The feasibility of a street-intercept survey method in an African-American community. Am J Public Health. 1997;87(4):655–658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grov C, Bimbi DS, Parsons JT, Nanín JE. Race, ethnicity, gender, and generational factors associated with the coming-out process among gay, lesbian, and bisexual individuals. J Sex Res. 2006;43(2):115–121 [DOI] [PubMed] [Google Scholar]
- 29.Koken JA, Parsons JT, Severino J, Bimbi DS. Exploring commercial sex encounters in an urban community sample of gay and bisexual men: a preliminary report. J Psychol Human Sex. 2005;17(1–2):197–213 [Google Scholar]
- 30.Grov C, Bimbi DS, Nanin JE, Parsons JT. Exploring racial and ethnic differences in recreational drug use among gay and bisexual men in New York City and Los Angeles. J Drug Educ. 2006;36(2):105–123 [DOI] [PubMed] [Google Scholar]
- 31.Kalichman SC, Simbaya L. Traditional beliefs about the cause of AIDS and AIDS-related stigma in South Africa. AIDS Care. 2004;16(5):572–580 [DOI] [PubMed] [Google Scholar]
- 32.Carey MP, Braaten LS, Jaworski BC, Durant LE, Forsyth AD. HIV and AIDS relative to other health, social, and relationship concerns among low-income urban women: a brief report. J Womens Health Gend Based Med. 1999;8(5):657–661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen JL, Kodagoda D, Lawrence AM, Kerndt PR. Rapid public health interventions in response to an outbreak of syphilis in Los Angeles. Sex Transm Dis. 2002;29(5):277–284 [DOI] [PubMed] [Google Scholar]
- 34.Rotheram-Borus MJ, Lee M, Zhou Set al. Variation in health and risk behavior among youth living with HIV. AIDS Educ Prev. 2001;13(1):42–54 [DOI] [PubMed] [Google Scholar]
- 35.Benotsch EG, Martin AM, Espil FMet al. Internet use, recreational travel, and HIV risk behaviors in men who have sex with men. J Community Health. 2011;36(3):398–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kalichman SC, Benotsch E, Rompa Det al. Unwanted sexual experiences and sexual risks in gay and bisexual men: associations among revictimization, substance use, and psychiatric symptoms. J Sex Res. 2001;38(1):1–9 [Google Scholar]
- 37.Halkitis PN, Parsons JT. Recreational drug use and HIV-risk sexual behavior among men frequenting gay social venues. J Gay Lesbian Soc Serv. 2002;14(4):19–38 [Google Scholar]
- 38.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401 [Google Scholar]
- 39.Centers for Disease Control and Prevention Impact of September 11 attacks on workers in the vicinity of the World Trade Center—New York City. MMWR Morb Mortal Wkly Rep. 2002;51(spec no.):8–10 [PubMed] [Google Scholar]
- 40.Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12(2):277–287 [DOI] [PubMed] [Google Scholar]
- 41.Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: a comparison of depression scales. J Am Acad Child Adolesc Psychiatry. 1991;30(1):58–66 [DOI] [PubMed] [Google Scholar]
- 42.Lyness JM, Noel TK, Cox C, King DA, Conwell Y, Caine ED. Screening for depression in elderly primary care patients. A comparison of the Center for Epidemiological Studies–Depression Scale and the Geriatric Depression Scale. Arch Intern Med. 1997;157(4):449–454 [PubMed] [Google Scholar]
- 43.Greenwood GL, Relf MV, Huang B, Pollack LM, Canchola JA, Catania JA. Battering victimization among a probability-based sample of men who have sex with men. Am J Public Health. 2002;92(12):1964–1969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paul JP, Catania J, Pollack L, Stall R. Understanding childhood sexual abuse as a predictor of sexual risk-taking among men who have sex with men: the Urban Men's Health Study. Child Abuse Negl. 2001;25(4):557–584 [DOI] [PubMed] [Google Scholar]
- 45.Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual sensation seeking: scale development and predicting AIDS-risk behavior among homosexually active men. J Pers Assess. 1994;62(3):385–397 [DOI] [PubMed] [Google Scholar]
- 46.Kalichman SC, Greenberg J, Abel GG. HIV-seropositive men who engage in high-risk sexual behavior: psychological characteristics and implications for prevention. AIDS Care. 1997;9(4):441–540 [DOI] [PubMed] [Google Scholar]
- 47.Parsons JT, Bimbi DS, Halkitis PN. Sexual compulsivity among gay/bisexual male escorts who advertise on the Internet. Sex Addict Compulsivity. 2001;8(2):101–112 [Google Scholar]
- 48.Benotsch EG, Kalichman SC, Pinkerton SD. Sexual compulsivity in HIV-positive men and women: prevalence, predictors, and consequences of high-risk behaviors. Sex Addict Compulsivity. 2001;8(2):83–99 [Google Scholar]
- 49.Cooper A, Delmonico DL, Burg R. Cybersex users, abusers, and compulsives: new findings and implications. Sex Addict Compulsivity. 2000;7(1–2):5–29 [Google Scholar]
- 50.Stall R, Herrick A, Guadamuz TE, Friedman MS. Updating HIV prevention with gay men: current challenges and opportunities to advance health among gay men. : Mayer KH, Pizer HF, HIV Prevention: A Comprehensive Approach. Cambridge, MA: Elsevier; 2009:267–280 [Google Scholar]