Abstract
Public health arguments for collecting hemoglobin A1c (HbA1c) data, particularly in clinical settings, should be reframed to place more emphasis on nonmedical determinants of population health. We compare individual- with population-level interpretations of HbA1c titers. This comparison reveals that public health researchers need to pay close attention to diagnostic tests and their uses, including rhetorical uses. We also synthesize historical and current evidence to map out 2 possible scenarios for the future. In the first scenario, prevention efforts emphasize primary care and focus almost entirely downstream. The second scenario anticipates downstream interventions but also upstream interventions targeting environments. Our analysis adapts actor–network theory to strategic planning and forecasting in public health.
In the past few years, prominent international bodies have been agitating for hemoglobin A1c (HbA1c) levels to become the criterion for diagnosing type 2 diabetes mellitus. HbA1c is a glycoprotein formed by a direct reaction between blood glucose and hemoglobin. HbA1c titers are significantly higher in patients with prolonged periods of hyperglycemia. For this reason, HbA1c monitoring has been used routinely for many years in clinical research and in clinical practice to measure diabetes control in patients. This protein is present in all humans, and variation occurs within and between populations. Indeed, HbA1c has been used occasionally in social epidemiology as a measure of population health. How and the extent to which the increased use of the HbA1c test to measure individual health in clinical settings translates into increased use of aggregated HbA1c results to measure population health will eventually have consequences for health policy, resource allocation, and modes of intervention. We have adapted actor–network theory to explore the public health implications of reorganizing type 2 diabetes diagnosis around HbA1c assays. In particular, we examined how HbA1c levels in patients and populations are being used to promote particular views about physiology and behavior, without discussion of the potential significance of HbA1c data as a measure of population health and an indicator of upstream causes of morbidity and mortality.
The move toward HbA1c-based diagnosis has generated controversy.1 Proponents have offered several justifications for this substantial shift in clinical practice: (1) the failure of current diagnostic standards to halt the progression of secondary macrovascular disease, (2) the stability of the HbA1c molecule as a measure of average blood glucose levels over a period of weeks, and (3) an increasing trust in the reliability of HbA1c measurements.2,3 Proponents believe the HbA1c test has tremendous potential to identify prediabetic individuals before the onset of irreversible damage.4 Yet changing the criteria by which type 2 diabetes is diagnosed is not only a move to prevent the onset of disease and disability. Knowledge about the properties and significance of the HbA1c molecule is framed by other information about at-risk individuals, early targeted treatments, and comparable diabetic and nondiabetic populations.5 Changing the way prediabetic individuals are identified and classified will likely reorient the way patients, care providers, and institutions understand and respond to the escalating incidence and risks of diabetes in many different populations.6
STRESSORS AND SOCIAL ENVIRONMENTS
Stressors (i.e., negative events, chronic strains, and traumas) have consistently been shown to negatively affect human health across the life span when measured comprehensively and cumulatively.7,8 Furthermore, a key way that gender, race/ethnicity, and socioeconomic disparities contribute to health inequalities appears to be through differential environmental exposure to stressors.7,8 The social dimensions of an environment influence health not only by influencing behavior, but also by mechanisms that are still poorly understood.
Nevertheless, long-running debate has focused on the extent to which popular notions and some scientific operationalizations of stress reflect middle-class, adult, and male experiences.9,10 Reviews of research involving animals, in both laboratory and field settings, temper such critiques. Animal studies provide support for the view that negative experiences affect biological processes and are associated with poorer health across the life span.8,11 The importance of bonding and supportive relationships for resiliency is also suggested by animal studies.8,10 Although many questions remain about the significance of stressors for the health of human populations, current conceptions revolve around a social gradient of disease. Researchers posit that biological responses to stressors, which arise to varying degrees in different social environments, ultimately influence health outcomes.8,12,13
Because HbA1c provides an index of a person's exposure to hyperglycemia, and because glycemic levels are implicated in the biological response to stressors, social epidemiologists have turned to HbA1c as a potential biological marker of exposure to stressors in different social environments.13,14 Studies of HbA1c found that modest increases in the level of this glycoprotein correlated with psychological measures of job stress,15,16 increased risk of heart disease in men,17 and other chronic morbidities in nondiabetic populations.18–20 Although the mechanisms are not well characterized, an independent and inverse association with HbA1c levels was associated with employment grade in the Whitehall Study.21 A large body of cross-sectional data held by the National Health and Nutrition Examination Survey in the United States showed that HbA1c levels were significantly associated with key measures of socioeconomic status and stress in both men and women.22 Nevertheless, important limitations still exist in knowledge about HbA1c, stressors, social environments, and the health of human populations. One important concern is that the existing research evidence is almost entirely derived from cross-sectional studies.
The use of a biological measure such as HbA1c to assess relative health and exposure to stressors in different populations has important implications in health policy formation and the allocation of scarce resources. It is increasingly clear that human behavior and individual genetic inheritance account for only some of the individual variation in health status; biological measures such as HbA1c levels might therefore usefully serve as a means to identify and monitor populations at risk of increased burdens of disease.13,14 In the aggregate, databases containing HbA1c measures could be used in research on stressors, social environments, and the health of human populations. For example, a research group recently used HbA1c measures in an administrative database in a cross-sectional study of whether neighborhood characteristics were associated with type 2 diabetes control. Black veterans who had been previously diagnosed with type 2 diabetes and who lived in neighborhoods with high scores on a “working together to improve the neighborhood” survey item tended to have lower HbA1c levels.23(p519)
More research on links between stressors, social environments, and HbA1c levels is warranted, but it will heavily depend on the inclusion of HbA1c measures in surveys and in administrative databases. Should HbA1c levels become a routine screening and diagnostic tool for type 2 diabetes, the potential value of administrative databases in social epidemiology and intervention research would expand. Such data sets would contain information on more people over longer periods, and the impact on HbA1c levels from, for example, community interventions to increase social cohesion, could be studied. Large administrative databases with longitudinal HbA1c data could assist in moving beyond the limitations of cross-sectional studies in providing research evidence for translation into policy and programming initiatives.
HEMOGLOBIN A1C AND TYPE 2 DIABETES MELLITUS
Although the apparent association between social stress and HbA1c is of increasing interest to population health researchers, elevations in this glycoprotein also occur in individuals with diabetes, of which the most prevalent form is type 2. This condition is characterized by hyperglycemia and disturbed lipid, protein, and carbohydrate metabolism. Unlike type 1 diabetes, type 2 is considered to be preventable. Because high blood glucose is the metabolic hallmark of a diabetic state, past efforts to identify the condition have focused on glucose determination—usually through a standardized protocol of blood glucose measurements.24 The validation of the HbA1c test in diabetes-related discourse is a relatively recent event.25 Endocrinologists and pharmaceutical companies were looking for a new hyperglycemic biomarker to track during drug safety and efficacy evaluations in the 1970s. The HbA1c glycoprotein was attractive because it reliably indexes the level of blood glucose in an individual over 6 weeks, unlike snapshot glucose measurements.
In the 1990s, the 2 most influential large-scale clinical trials of diabetic therapeutic regimens—the Diabetes Control and Complications Trial and the United Kingdom Prospective Diabetes Study—established changes in the titer of HbA1c molecules as an effective means to monitor glucose control in individual diabetic patients.26,27 These studies promoted wholesale changes in the treatment of diabetic patients because they also confirmed that the HbA1c glycoprotein is a reliable index of the risk of both microvascular and macrovascular complications. Many health care providers changed their clinical routines in response to these findings. They continued to definitively diagnose diabetic individuals through snapshot blood glucose determinations, but they began to use HbA1c rather than fasting plasma glucose levels to monitor diabetes control and plan treatments. HbA1c has thus become a crucial tool for health professionals to measure and address the adherence of individuals to prescribed therapies (diet, exercise, and medication),25,28 as well as to prescribe additional therapies, notably medication. People with diabetes are advised to strive for diabetes control, partly by regularly measuring plasma glucose values (i.e., self-managed blood glucose monitoring), but also through vigilance about eating and exercising. This emphasis on self-control predates the use of HbA1c in diabetes treatment; the widespread adoption of HbA1c as a measure of diabetic control reinforced and amplified a familiar way of thinking, by means of a novel technology.29,30
Yet the practice of attaining tight glucose control through self-monitoring is slowly falling out of favor. In follow-up studies, aggressive glucose-specific measures have been found to be inadequate for achieving the stated goals of reducing the incidence of macrovascular fatalities in people diagnosed with type 2 diabetes.31,32 Although these results are contested, the weight of opinion is that disciplined glucose regulation is insufficient to halt the development of diabetic complications. When the diagnosis of type 2 diabetes is delayed—no matter how tight the subsequent glucose control—onset of other chronic diseases seems to be inevitable. Because existing systems of diagnosis fail to detect a significant proportion of people who subsequently develop type 2 diabetes, many diabetologists now believe that earlier intervention is necessary. Because diabetes onset is subtle and gradual—and it is often difficult to pinpoint when someone with type 2 diabetes has truly become a diabetic—a concerted effort is being mounted to base diabetes diagnosis as well as diabetes treatment on HbA1c measurement. Because HbA1c accurately predicts both microvascular and macrovascular disease, proponents propose that an HbA1c blood level greater than 6.5 millimoles per liter should become the diagnostic gold standard for all forms of diabetes2–4 and that 6 millimoles per liter be accepted provisionally as a positive screen for type 2.2,33,34
Clearly, the evidentiary basis of type 2 diabetes diagnosis, care, and prevention is in transition. Many authors have noted that changes in how medical evidence, such as diagnostic tests, epidemiological databases, and clinical trials, is produced and appraised can have many and varied political, personal, and structural effects.35,36 Not all of these are anticipated by the proponents of change. Attempts to standardize clinical practice around the best available evidence may not only direct individual treatments but also mandate changes in public policy and agreed-upon evidentiary forms, thereby reformulating the legitimacy of claims to authority.37
ACTOR–NETWORK INSIGHTS
Our analysis of potential public health implications of changing the evidentiary status of HbA1c and recommendations is informed by scholarship in the interdisciplinary field of science and technology studies. Actor–network theory is a theoretical resource that provides a comprehensive and empirically grounded framework for understanding innovations within systems. Actor–network scholarship has generated important insights about links as well as gaps between clinical practice, epidemiological research, and programs within and outside the health care sector that can influence health and disease in entire populations.38,39 Nevertheless, this scholarship has yet to be applied extensively in public health.40–42
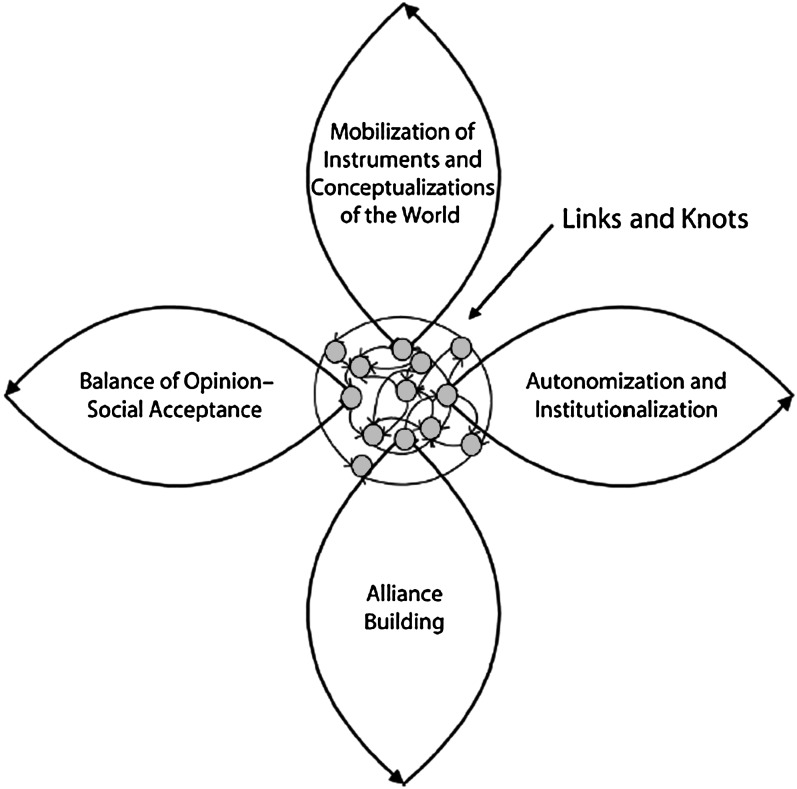
Actor–network theorists emphasize that ideas and things, the semiotic and material elements that compose any system, inevitably and continually shape one another. Research informed by this theoretical tradition has, for example, highlighted that physical dimensions of environments, such as automobiles and traffic patterns, are socially mediated and entwined with the history of medicine in unexpected ways.43 As expertly demonstrated by Young et al. in their analysis, informed by actor–network theory, of the history of smoke-free public spaces,41 when ideas and things are part of highly complex systems, they are typically limited by a repertoire of established responses. Changing the evidentiary status of HbA1c from a useful measure of control and risk to a diagnostic criterion and screening technology is therefore a significant step that will reshape the network of concepts, values, practices, and actors that drives efforts to prevent, diagnose, and effectively treat type 2 diabetes. Young et al. illustrate in a diagram how an established network responds to fundamental change and reform where heterogeneous elements (links and knots) such as people, research evidence, technologies, and financial resources interact and consolidate to realize a goal—such as diabetes prevention—that in turn ends up restructuring many aspects of everyday reality (Figure 1).
FIGURE 1—
Innovations in systems according to actor–network theory.
Source. Young et al.41(p1297)
Representing the relationships between people, institutions, technologies, and evidence through an actor–network approach illuminates how problems emerge in a system and how a system is reshuffled in response to bring about a solution. Young et al. describe 4 loops that reach out from a central reorganizing network (Figure 1) and that
represent activities designed to link the core with 4 interdependent sources of power: scientific evidence and the technologies or techniques that depend on it, professional or political authority, allies, and public opinion.41(p1209)
These loops then provide the means for network stabilization, such as the mobilization of science, technology, and theory to frame the issue; alliance building to solidify and defend the new network vis-à-vis alternative concepts and technologies; processes and interests that shape the social acceptance of the new system; and institutionalization or authoritative systematic acceptance of the new equilibrium. These loops or steps do not necessarily occur in sequence, nor are they determined by the weight of verified evidence. The institutionalization and social acceptance of the new system equilibrium is shaped, at least in part, by the relative success of the innovators in marshaling resources, evidence, and allies to support and manage the new network.
CURRENT SITUATION
Because diagnostic tests also provide the underlying structure to diagnostic categories, test results propel patients down systematized clinical pathways and into new social groups and, potentially, motivate them and their close kin to reorient themselves within a new way of living.30,44 Diagnostic tests give biomarkers, cell lines, genes, infectious agents, and other entities their prognostic and social significance. Changing what is perceived as the definitive test for a specific condition, therefore, can ultimately change disease definitions and classifications and, indeed, patient identity, social support, and status. Past studies indicated that the choice of diagnostic criterion for diabetes is also implicitly a choice of which particular phenomenon associated with the disease—sugar or glycoprotein, patient or population—will be the central articulation around which efforts will be made to characterize, identify, and manage its effects.6,29
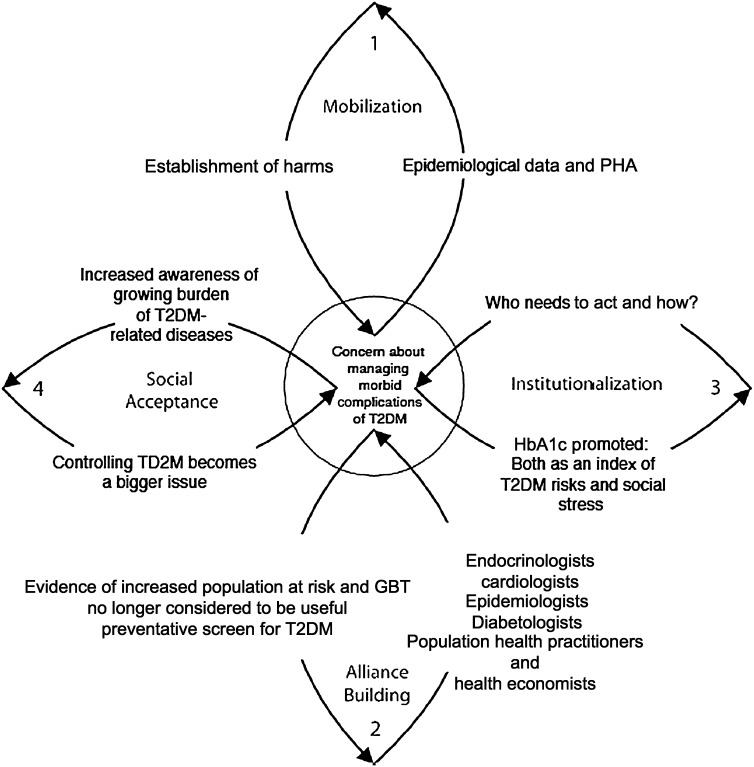
Adapting the Young et al. actor–network analysis of evidence-based innovation41 to the current debate about using HbA1c to screen for and to diagnose type 2 diabetes shows how the accumulation of epidemiological data can translate into treating type 2 diabetes as a pressing social and public health problem in clinical settings and in primary care policymaking (Figure 2). These loops represent 4 key processes: (1) HbA1c assays and population health data are being mobilized to establish the harms associated with chronic hyperglycemia; (2) alliances are being formed and repositioned between professional groups to organize a coordinated response to the growing significance of current and future burdens of chronic diseases, notably type 2 diabetes, microvascular disease, and macrovascular disease; (3) institutionalization is occurring as more actors accept the significance of the HbA1c molecule as evidence of populations at elevated risk for cardiometabolic disease and as an index of health risks for individuals; and (4) expert opinion is beginning to cohere around a perceived need to use HbA1c data to respond to the social implications and future disease burdens associated with higher rates of type 2 diabetes in healthy, at-risk, and clinically treated populations, and such an approach appears to be socially acceptable. Once the importance of this issue is established, the problem facing all those in the network is deciding on the most appropriate response: the best target and the most effective method or strategy of intervention.
FIGURE 2—
Network mapping the rising prominence of HbA1c data and the coemergence of type 2 diabetes mellitus complications as a pressing public health issue.
Note. GBT = glucose-based test; HbA1c = hemoglobin A1c; PHA = population health assessments; S&PE = social and physical environments; T2DM = type 2 diabetes mellitus.
DOWNSTREAM AND UPSTREAM APPROACHES TO PREVENTION
Of increasing importance is whether to continue to direct almost all available resources toward individual cases or to invest in interventions targeting entire populations as well. A focus on individual cases emphasizes downstream, or proximal, causes, particularly individual behavior (following recommendations for diet, exercise, and medication); a focus on populations emphasizes upstream, environmental causes. The likely consequences of both strategies for the US health care system were simulated by Jones et al. at the National Center for Chronic Disease Prevention, Centers for Disease Control and Prevention, and were published in this journal.45 Their complex population dynamics model predicts that a mixture of individual- and population-focused measures that address type 2 diabetes as a heterogeneous system is the most appropriate long-term strategy.
The use of actor–network scholarship in formulating policy prescriptions with the intent of promoting a favored outcome has faced long-standing resistance.46,47 Nonetheless, tentative steps are being taken toward drawing on actor–network scholarship to map out the implications of current events and, more significantly, provide action-oriented evidence.48,49
We do not oppose the use of HbA1c data to manage type 2 diabetes or to identify prediabetic individuals. The advantages of reorganizing clinical practices around the blood level of this molecule are compelling. The HbA1c test represents the level of blood glucose over months rather than minutes and provides an index to determine differences in morbid risks between patients. It produces a continuum from the hyperglycemic past to future health, replacing freeze-frame diagnosis and surveillance. Because the HbA1c test is thought to have greater sensitivity for marginally hyperglycemic individuals, and therefore identifies a larger cohort of patients who have the early subclinical stages of poor glucose regulation, it is possible that over time, diabetes—like hypertension and high cholesterol—will be mainly perceived as a risk factor for other chronic diseases and premature death. As evidence of the cardiovascular impact of this metabolic problem mounts,20,50 momentum within this new network is building around the notion that “the comprehensive care of diabetes involves the treatment of all vascular risk factors—not just hyperglycaemia.”51(p355)
Exposure to stressors in social environments are known to have adverse health effects; therefore, steps that promote the reduction of disparities within and between populations—such as facilitating healthy diets, regular exercise, and safer neighborhoods—could have a profound impact on diabetes incidence, HbA1c levels, and associated human suffering.45,52 The current situation (Figure 2) could evolve such that stressors, which vary across environments and which seem to influence HbA1c in populations, remain overlooked and consequently ignored.
TWO POSSIBLE FUTURES AND THEIR PUBLIC HEALTH IMPLICATIONS
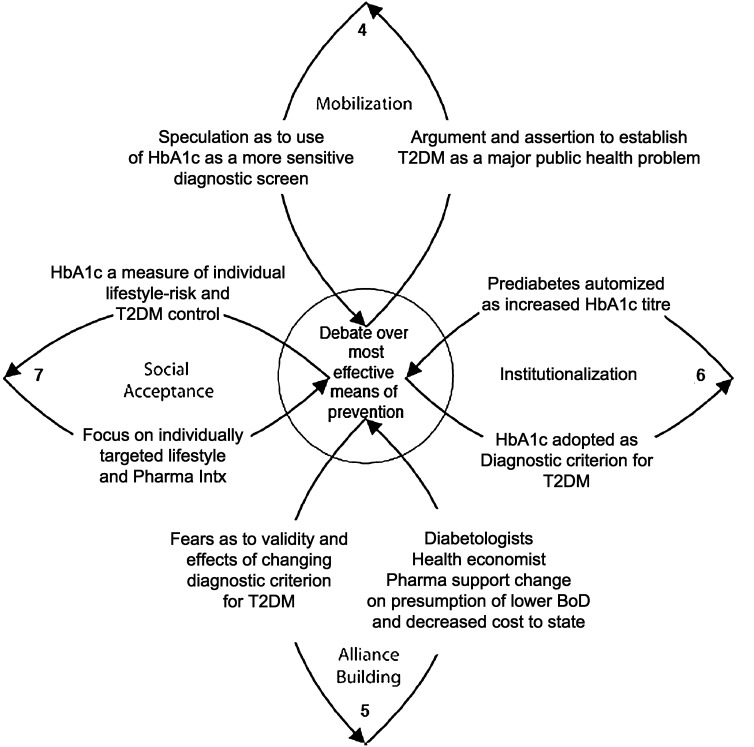
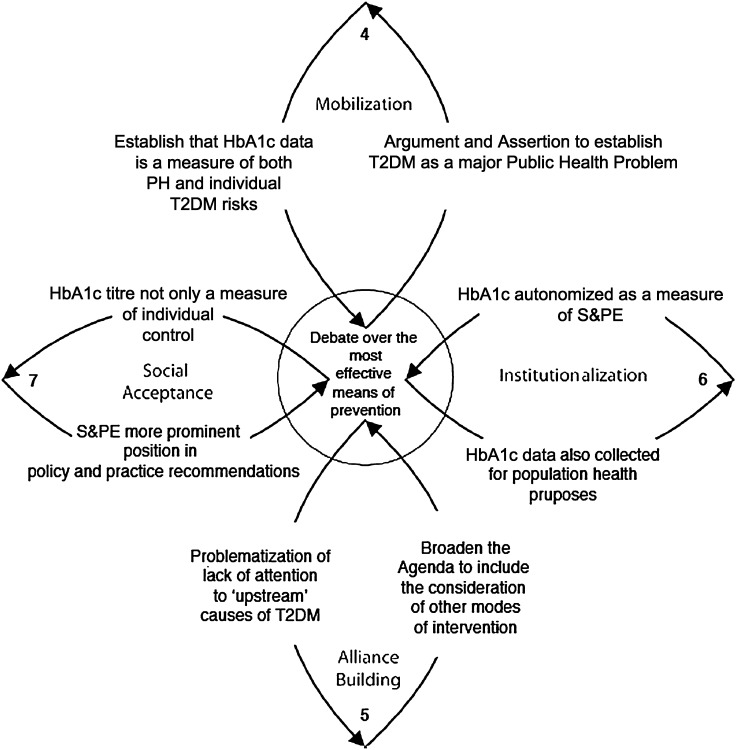
In much the same way as Jones et al. compared the future consequences of individual versus mixed type 2 diabetes intervention strategies,45 we anticipated 2 future configurations by applying an adaptation of actor–network theory prospectively to the current focus on reducing the burdens of diabetes complications through self-management and clinical interventions hinging on HbA1c (Figure 2). Both scenarios presume that HbA1c would be used to screen for and diagnose type 2 diabetes, but aggregated HbA1c data would be mobilized in distinct ways. In the first scenario, the focus would remain almost entirely on primary care and individual self-management, with a view to averting or at least delaying the downstream consequences of type 2 diabetes mellitus (Figure 3). In the second scenario, a focus on overall population health and upstream interventions would parallel treatment efforts (Figure 4).
FIGURE 3—
Prospective network with HbA1c data used only in primary care to prevent type 2 diabetes mellitus and related complications.
Note. BoD = burden of disease; HbA1c = hemoglobin A1c; Intx = interventions; T2DM = type 2 diabetes mellitus.
FIGURE 4—
Alternative network after mobilization of HbA1c as a resource for primary care and for promoting the physical and mental health of populations.
Note. HbA1c = hemoglobin A1c; PH = population health; S&PE = social and physical environments; T2DM = type 2 diabetes mellitus.
In our first projected network (Figure 3), the evidentiary significance of HbA1c data would become completely enmeshed with the concerns of primary care. As a consequence, HbA1c titers would only be construed as a measure of lifestyle risks, diabetic control, and quality of individuals’ treatment. The potential relevance of HbA1c measurements to population health as a tool to monitor and better target population-level interventions would be subsumed by efforts to identify and ameliorate type 2 diabetes in particular people before they head further downstream.
DOWNSTREAM AND UPSTREAM INTERVENTIONS FOR OBESITY
Evidence suggests that interventions focused on weight loss—whether through lifestyle changes, new medications, or bariatric surgery—are the most effective early treatment and preventive measures for type 2 diabetes.53,54 Although the rising incidence of weight-related health problems in many populations worldwide stems, in all likelihood, from the interplay of social, cultural, demographic, and economic trends, intervention research to address the root causes has not found much favor among diabetes experts.55,56 When issues relating to the increasing incidence of health risks in populations are framed alongside the positive attributes of the HbA1c test, professional opinion leaders are comfortable claiming that now is the time to evaluate “the public health, economic and practical implications of redefining the diagnostic criteria for diabetes.”4(p2247) However, despite the acknowledgment that diabetes is a public health issue related to interactions between food, activity levels, and environment, the HbA1c test is being used strategically to frame this population-wide problem as amenable to clinical management and, ultimately, self-management through adherence to professional advice regarding diet, exercise, and medication.2
Some practitioners and researchers, looking beyond the scientific evidence, also hope that deploying HbA1c as a diagnostic screen will have an explicit rhetorical impact, drawing the focus of people, their caregivers, regulators, and planners to preventive actions.34,57 Yet despite the evident potential for a broader public health focus, high HbA1c levels in distinct groups of people are not stimulating recognition of the need for population-level interventions. Instead, the HbA1c test is only being used as an explicit link between asymptomatic states in individuals and their risk of future disease, thereby permitting earlier interventions and a coherent flow of clinically mediated actions and future evaluations. With the widespread adoption of HbA1c-based diagnosis, it is likely that a larger proportion of the population will find themselves among the ranks of prediabetic patients who are encouraged to regulate their lives and lifestyles—as individuals.58 The success of these activities—and patients' adherence—will be measured against their HbA1c levels, if current trends continue, under the direct supervision of primary health care providers.
HbA1c entered mainstream diabetic discourse through pharmaceutical trials and not through social epidemiology or population health interventions. Although it is not construed this way, the HbA1c test offers not only a record of patients’ hyperglycemia and behavioral history, but also a précis of their exposure to stressors. Although the promotion of the HbA1c test implicitly acknowledges that conditions that promote hyperglycemia are widespread, the link between elevated levels of this molecule and different populations’ environments remains underemphasized. At this time, the HbA1c test is only being promoted as a means to enable population-level change through small increments in individuals, often to be achieved only by resisting trends in physical and social environments.58 It is arguable that when positioned alongside the current emphasis on weight and the health risks of obesity, the HbA1c test is being deployed as a rhetorical resource to try to monitor and intervene in the individual lives and lifestyles of a larger proportion of the population. This approach ignores the potential for improving population health through primary prevention via interventions in sectors other than health care, such as the food industry, transportation, and urban planning.
MOVING UPSTREAM TO AMELIORATE ENVIRONMENTAL STRESSORS
Other configurations of knowledge and practice are possible. For example, HbA1c data collected in the course of identifying and treating individual patients with type 2 diabetes can also tell us about the average levels of HbA1c in distinct populations. Secondary analysis could create further evidence that could encourage population-based interventions for obesity and other socially mediated health risks and diseases. As Young et al. point out, the credibility of this alternative network of evidence, theories, and values depends not only on its internal coherence, but also on its generalizability and ability to engage diverse sectors.41
As diabetes and its morbid complications are increasingly recognized to be a pressing and significant population health problem, the collation of HbA1c data as a measure of the diabetic risk of specific populations could highlight—and possibly reverse—the lack of attention to upstream causes of this condition. In our second prospective network, HbA1c titers would be not only a measure of the health, diabetic risks, and self-management by individuals, but also an index of underlying health disparities and a means to identify and monitor populations at risk of increased burdens of disease. Alliances between planners and population health researchers could broaden the agenda to gain public support for and ultimately institutionalize alternative modes of intervention focusing on physical and social dimensions of environments.
If epidemiological data from population-based testing is to be used to better manage morbid risks in individual patients, we need to pay closer attention to technologies of primary care. When clinicians use a test during diagnostic determinations, the audiences—patients, their caregivers, and health professionals—are being furnished with a set of perspectives, interpretations, and explanations. In turn, the results of diagnostic tests populate databases and can inform the formulation and implementation of policies of many different kinds and in many different settings. In each circumstance, what is being communicated is not just a set of facts or a causal story that can be fitted into an archetypical illness script or the likely prognosis. What is being transferred or translated also includes a disciplinary perspective and its supporting sociotechnical network—in essence, a way of knowing.59,60
If nothing else, the potential use of HbA1c to represent and index the relative health and well-being of populations—rather than healthy, diseased, or at-risk individuals only—could assist in the future prevention and management of type 2 diabetes and many other chronic health problems. As illustrated by Figure 4, it is conceivable that HbA1c administrative data could be mobilized through research to assess the impact of different environments. Current practice, however, is indicative of how we are attempting to deal with weight-related dysfunctions without explicitly addressing the health inequities produced by obesogenic and stressful environments.18,56,61
CONCLUSIONS
The distribution of HbA1c in individuals and in populations is being proposed to serve as a resource that substantiates specific clinical practices. This is a narrow perspective that ignores many plausible venues for intervention outside health care to address the burgeoning prevalence of type 2 diabetes and related health problems. International advisory bodies and expert consensus groups are using epidemiological data and improved levels of standardization across diagnostic laboratories to bolster arguments for a change in diagnostic criteria.62 The impetus behind retooling HbA1c level as the diagnostic criterion for type 2 diabetes is to address “individuals within the collective” without acknowledgement of the health gains that could stem from recognizing the existence of “collectives of interacting individuals.”63(p242)
The journey of the HbA1c test toward becoming the accepted diagnostic tool for type 2 diabetes highlights why public health researchers need to pay close attention to diagnostic tests and their uses, including rhetorical uses. We see a need to reframe public health arguments for collecting HBA1c data, in clinical as well as nonclinical settings, to place more emphasis on the determinants of population health and on population health intervention research.
Acknowledgments
C. Degeling received support from Alberta Innovates—Health Solutions Establishment and Incentive Grants to Melanie Rock and a University of Calgary Veterinary Medicine Postdoctoral Entrance Award. M. Rock holds a Population Health Investigator award from Alberta Innovates—Health Solutions, which is funded by the Alberta Heritage Foundation for Medical Research Endowment. She also holds a New Investigator in Societal and Cultural Dimensions of Health Award from the Canadian Institutes of Health Research.
We thank our anonymous reviewers and Kenneth R. McLeroy for the depth of their insights and for their clarifying comments and suggestions.
Human Participant Protection
No protocol approval needed for this study because no human participants were involved.
References
- 1.James C, Bullard KM, Rolka DBet al. Implications of alternative definitions of prediabetes for prevalence in U.S. adults. Diabetes Care. 2011;34(2):387–391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Expert Committee International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32(7):1327–1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cox ME, Edelman D. Tests for screening and diagnosis of type 2 diabetes. Clin Diabetes. 2009;27(4):132–138 [Google Scholar]
- 4.Borch-Johnsen K, Colagiuri S. Diagnosing diabetes—time for a change? Diabetologia. 2009;52(11):2247–2250 [DOI] [PubMed] [Google Scholar]
- 5.Rock M. Classifying diabetes; or, commensurating bodies of unequal experience. Public Cult. 2005;17(3):467–486 [Google Scholar]
- 6.Rock M. Reconstituting populations through evidence-based medicine: an ethnographic account of recommending procedures for diagnosing type 2 diabetes in clinical practice guidelines. Health (London). 2005;9(2):241–266 [DOI] [PubMed] [Google Scholar]
- 7.Thoits PA. Stress and health: major findings and policy implications. J Health Soc Behav. 2010;51(Suppl):S41–S53 [DOI] [PubMed] [Google Scholar]
- 8.Hertzman C, Boyce T. How experience gets under the skin to create gradients in developmental health. Annu Rev Public Health. 2010;31:329–347 [DOI] [PubMed] [Google Scholar]
- 9.Young A. The discourse on stress and the reproduction of conventional knowledge. Soc Sci Med Med Anthropol. 1980;14B(3):133–146 [DOI] [PubMed] [Google Scholar]
- 10.Taylor SE, Klein LC, Lewis BP, Gruenewald TL, Gurung RA, Updegraff JA. Biobehavioral responses to stress in females: tend-and-befriend, not fight-or-flight. Psychol Rev. 2000;107(3):411–429 [DOI] [PubMed] [Google Scholar]
- 11.Sapolsky RM. Social status and health in humans and other animals. Annu Rev Anthropol. 2004;33:393–418 [Google Scholar]
- 12.Brunner EJ, Marmot M. Social organization, stress, and health. : Marmot M, Wilkinson R, Social Determinants of Health. 2nd ed Oxford, UK: Oxford University Press; 2006:6–30 [Google Scholar]
- 13.Kelly S, Hertzman C, Daniels M. Searching for the biological pathway between stress and health. Annu Rev Public Health. 1997;18:437–462 [DOI] [PubMed] [Google Scholar]
- 14.Daniel M, Dea K, Rowley KG, McDermott R, Kelly S. Glycated hemoglobin as an indicator of social environmental stress among indigenous versus westernized populations. Prev Med. 1999;29(5):405–413 [DOI] [PubMed] [Google Scholar]
- 15.Cesana G, Panza G, Ferrario M, Zanettini R, Arnoldi M, Grieco A. Can glycosylated hemoglobin be a job stress parameter? J Occup Med. 1985;27(5):357–360 [DOI] [PubMed] [Google Scholar]
- 16.Kawakami N, Araki S, Hayashi T, Masumoto T. Relationship between perceived job-stress and glycosylated hemoglobin in white-collar workers. Ind Health. 1989;27(4):149–154 [DOI] [PubMed] [Google Scholar]
- 17.Khaw KT, Wareham N, Luben Ret al. Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of European prospective investigation of cancer and nutrition (EPIC-Norfolk). BMJ. 2001;322(7277):15–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kawakami N, Akachi K, Shimizu Het al. Job strain, social support in the workplace, and haemoglobin A1c in Japanese men. Occup Environ Med. 2000;57(12):805–809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jørgensen L, Jenssen T, Joakimsen O, Heuch I, Ingebretsen OC, Jacobsen BK. Glycated hemoglobin level is strongly related to the prevalence of carotid artery plaques with high echogenicity in nondiabetic individuals: the Trømso Study. Circulation. 2004;110(4):466–470 [DOI] [PubMed] [Google Scholar]
- 20.Selvin E, Steffes MW, Zhu Het al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 2010;362(9):800–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feldman PJ, Steptoe A. Psychosocial and socioeconomic factors associated with glycated hemoglobin in nondiabetic middle-aged men and women. Health Psychol. 2003;22(4):398–405 [DOI] [PubMed] [Google Scholar]
- 22.Kelly SJ, Stedman J, Leonardi-Bee J. Is hemoglobin A1c level associated with measures of socio-economic status in non-diabetics after controlling for known explanatory factors? Stress Health. 2005;21(3):185–192 [Google Scholar]
- 23.Long JA, Field S, Armstrong K, Chang VW, Metlay JP. Social capital and glucose control. J Community Health. 2010;35(5):519–526 [DOI] [PubMed] [Google Scholar]
- 24.Goldstein DE, Little RR, Lorenz RAet al. Tests of glycemia in diabetes. Diabetes Care. 2004;27(Suppl 1):S91–S93 [DOI] [PubMed] [Google Scholar]
- 25.Sinding C. Une molécule espion pour les diabétologues, l'innovation en médicine entre science et morale [A molecular spy for diabetologists, medical innovation between science and morality]. Sci Soc Sante. 1999;18(2):95–120 [Google Scholar]
- 26.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986 [DOI] [PubMed] [Google Scholar]
- 27.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998(9131);352:837–853 [PubMed] [Google Scholar]
- 28.Broom D, Whittaker A. Controlling diabetes, controlling diabetics: moral language in the management of diabetes type 2. Soc Sci Med. 2004;58(11):2371–2382 [DOI] [PubMed] [Google Scholar]
- 29.Feudtner C. The want of control: ideas, innovations, and ideals in the modern management of diabetes mellitus. Bull Hist Med. 1995;69(1):66–90 [PubMed] [Google Scholar]
- 30.Ferzacca S. “Actually, I don't feel that bad”: managing diabetes and the clinical encounter. Med Anthropol Q. 2000;14(1):28–50 [DOI] [PubMed] [Google Scholar]
- 31.Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller MEet al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kelly TN, Bazzano LA, Fonseca VA, Thethi TK, Reynolds K, He J. Systematic review: glucose control and cardiovascular disease in type 2 diabetes. Ann Intern Med. 2009;151(6):394–403 [DOI] [PubMed] [Google Scholar]
- 33.Bennett CM, Guo M, Dharmage SC. HbA1c as a screening tool for detection of type 2 diabetes: a systematic review. Diabet Med. 2007;24(4):333–343 [DOI] [PubMed] [Google Scholar]
- 34.Saudek CD, Herman WH, Sacks DB, Bergenstal RM, Edelman D, Davidson MB. A new look at screening and diagnosing diabetes mellitus. J Clin Endocrinol Metab. 2008;93(7):2447–2453 [DOI] [PubMed] [Google Scholar]
- 35.Mykhalovskiy E, Weir L. The problem of evidence-based medicine: directions for social science. Soc Sci Med. 2004;59(5):1059–1069 [DOI] [PubMed] [Google Scholar]
- 36.Rogers WA. Evidence based medicine and justice: a framework for looking at the impact of EBM upon vulnerable or disadvantaged groups. J Med Ethics. 2004;30(2):141–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Timmermans S, Kolker ES. Evidence-based medicine and the reconfiguration of medical knowledge. J Health Soc Behav. 2004;45(Suppl):177–193 [PubMed] [Google Scholar]
- 38.Berg M, Mol A. Differences in medicine: an introduction. : Berg M, Mol A, Differences in Medicine: Unraveling Practices, Techniques, and Bodies. Durham, NC: Duke University Press; 1998:1–12 [Google Scholar]
- 39.Law J, Mol A. Complexities: Social Studies of Knowledge Practices. Durham, NC: Duke University Press; 2002 [Google Scholar]
- 40.Cummins S, Curtis S, Diez-Roux AV, Macintyre S. Understanding and representing ‘place’ in health research: a relational approach. Soc Sci Med. 2007;65(9):1825–1838 [DOI] [PubMed] [Google Scholar]
- 41.Young D, Borland R, Coghill K. An actor–network theory analysis of policy innovation for smoke-free places: understanding change in complex systems. Am J Public Health. 2010;100(7):1208–1217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hawe P, Shiell A, Riley T. Theorising interventions as events in systems. Am J Community Psychol. 2009;43(3–4):267–276 [DOI] [PubMed] [Google Scholar]
- 43.Schlich T. Trauma surgery and traffic policy in Germany in the 1930s: a case study in the coevolution of modern surgery and society. Bull Hist Med. 2006;80(1):73–94 [DOI] [PubMed] [Google Scholar]
- 44.Rosenberg CE. The tyranny of diagnosis: specific entities and individual experience. Milbank Q. 2002;80(2):237–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jones AP, Homer JB, Murphy DL, Essien JDK, Milstein B, Seville DA. Understanding diabetes population dynamics through simulation modeling and experimentation. Am J Public Health. 2006;96(3):488–494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jasanoff S. Breaking the waves in science studies: comment on H.M. Collins and Robert Evans, 'The Third Wave of Science Studies.' Soc Stud Sci. 2003;33(3):389–400 [Google Scholar]
- 47.Vikkelsø S. Description as intervention: engagement and resistance in actor–network analyses. Sci Cult. 2007;16(3):297–309 [Google Scholar]
- 48.Mol A. Proving or improving: on health care research as a form of self-reflection. Qual Health Res. 2006;16(3):405–414 [DOI] [PubMed] [Google Scholar]
- 49.Webster A. Crossing boundaries social science in the policy room. Sci Technol Human Values. 2007;32(4):458–478 [Google Scholar]
- 50.Buse JB, Ginsberg HN, Bakris GLet al. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Circulation. 2007;115(1):114–126 [DOI] [PubMed] [Google Scholar]
- 51.Skyler JS, Bergenstal R, Bonow ROet al. Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA diabetes trials: a position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. Circulation. 2009;119(2):351–357 [DOI] [PubMed] [Google Scholar]
- 52.Brown AF, Ettner SL, Piette Jet al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol Rev. 2004;26:63–77 [DOI] [PubMed] [Google Scholar]
- 53.Alberti KGMM, Zimmet P, Shaw J. International Diabetes Federation: a consensus on type 2 diabetes prevention. Diabet Med. 2007;24(5):451–463 [DOI] [PubMed] [Google Scholar]
- 54.Nathan DM. Navigating the choices for diabetes prevention. N Engl J Med. 2010;362(16):1533–1535 [DOI] [PubMed] [Google Scholar]
- 55.Crandall JP, Knowler WC, Kahn SEet al. The prevention of type 2 diabetes. Nat Clin Pract End Met. 2008;4(7):382–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Type 2 diabetes—time to change our approach [editorial]. Lancet. 2010;375(9733):2193. [DOI] [PubMed] [Google Scholar]
- 57.Droumaguet C, Balkau B, Simon Det al. Use of HbA1c in predicting progression to diabetes in French men and women: data from an Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care. 2006;29(7):1619–1625 [DOI] [PubMed] [Google Scholar]
- 58.Rose G. The Strategy of Preventative Medicine. Oxford, UK: Oxford University Press; 1992 [Google Scholar]
- 59.Pickstone JV. Ways of Knowing: A New History of Science, Technology, and Medicine. Chicago, IL: University of Chicago Press; 2001 [Google Scholar]
- 60.Hacking I. Styles of scientific reasoning. : Rajchman J, West C, Post-Analytic Philosophy. New York, NY: Columbia University Press; 1985:145–165 [Google Scholar]
- 61.McKinlay J, Marceau L. US public health and the 21st century: diabetes mellitus. Lancet. 2000;356(9231):757–761 [DOI] [PubMed] [Google Scholar]
- 62.Rose G. Sick individuals and sick populations. 1985. Bull World Health Organ. 2001;79(10):990–996 [PMC free article] [PubMed] [Google Scholar]
- 63.Arah OA. On the relationship between individual and population health. Med Health Care Philos. 2009;12(3):235–244 [DOI] [PMC free article] [PubMed] [Google Scholar]