Abstract
Objectives. We evaluated the impact of revised national treatment recommendations on fluoroquinolone use for gonorrhea in selected states.
Methods. We evaluated gonorrhea cases reported through the Sexually Transmitted Disease Surveillance Network as treated between July 1, 2006 and May 31, 2008, using interrupted time series analysis. Outcomes were fluoroquinolone treatment overall, by area, and by practice setting.
Results. Of 16 126 cases with treatment dates in this period, 15 669 noted the medication used. After revised recommendations were released, fluoroquinolone use decreased abruptly overall (21.5%; 95% confidence interval [CI] = 15.9%, 27.2%), in most geographic areas evaluated, and in sexually transmitted disease clinics (28.5%; 95% CI = 19.0%, 37.9%). More gradual decreases were seen in primary care (8.6%; 95% CI = 2.6%, 14.6%), and in emergency departments, urgent care, and hospitals (2.7%; 95% CI = 1.7%, 3.7%).
Conclusions. Fluoroquinolone use decreased after the publication of revised national guidelines, particularly in sexually transmitted disease clinics. Additional mechanisms are needed to increase the speed and magnitude of changes in prescribing in primary care, emergency departments, urgent care, and hospitals.
More than 700 000 gonorrhea infections are estimated to occur in the United States each year.1 In 2008, 112 cases per 100 000 population were reported2—well above the Healthy People 2010 target of 19 cases per 100 000 population.3 Infection can cause pelvic inflammatory disease with long-term consequences including ectopic pregnancy, infertility, and chronic pelvic pain and may increase HIV transmission.4 Effective treatment is critical both to prevent sequelae in affected patients and to prevent the spread of infection to others. Treatment is challenging because of the ease with which Neisseria gonorrhoeae develops resistance to antimicrobials and the increased frequency of N. gonorrhoeae infections that are resistant to multiple classes of antimicrobials, including sulfanilamides, penicillin, tetracyclines, and, most recently, fluoroquinolones.5,6
The World Health Organization and the Centers for Disease Control and Prevention (CDC) have suggested that an antibiotic should no longer be routinely recommended for treatment of an infection when prevalence of infections resistant to that antibiotic exceeds 5%.7 Because of the increasing prevalence of fluoroquinolone-resistant N. gonorrhoeae above this threshold in specific areas and populations, fluoroquinolones were no longer recommended for treatment of gonococcal infections in Hawaii in 2000,8 in California in 2002,9 and for men who have sex with men in 2004.10 Prevalence of ciprofloxacin-resistant N. gonorrhoeae among heterosexual men in the Gonococcal Isolate Surveillance Project increased from 0.6% in 2001 to 6.7% in the first 6 months of 2006.11 Because of this increase, revised CDC guidelines that no longer recommended fluoroquinolones for the treatment of gonorrhea were published in Morbidity and Mortality Weekly Report on April 13, 2007, leaving cephalosporins as the only class of antimicrobials available in the United States recommended for gonorrhea treatment.11 These recommendations updating the CDC's STD Treatment Guidelines were sent to state and local health departments in a dear colleague letter and were announced at a national press conference timed to correspond with the Morbidity and Mortality Weekly Report article. This announcement received extensive media attention.12–16 It is not known how many providers were reached or how providers responded to the revised recommendations.
Previous studies have found that 78% of physicians either owned a copy of the CDC's STD Treatment Guidelines or knew how to access the guidelines17 and that adherence to sexually transmitted disease (STD) care guidelines was greater in STD clinics than in general medical clinics.18 However, little is known about practice changes after guideline revisions. To evaluate the impact of revised CDC guidelines on fluoroquinolone use, we used data from the STD Surveillance Network (SSuN). We employed interrupted time series analysis to evaluate the impact of revised guidelines on fluoroquinolone use and to determine whether impact varied by geographic area or by practice setting.
METHODS
Health providers and laboratories in the United States are legally mandated to report gonorrhea cases to state or local health departments.19 State and local health departments report cases to the CDC, but treatment is not reported at a national level. Health departments participating in SSuN—a national network of state and local health departments conducting enhanced STD surveillance following common protocols—contribute case report information, including treatment used and treatment date, for all gonorrhea cases reported in selected jurisdictions. For this analysis, 5 collaborating health departments participating in SSuN contributed data from the following jurisdictions: Adams, Arapahoe, and Denver counties, Colorado (the Colorado Department of Public Health and Environment); Hennepin County, Minnesota (the Minnesota Department of Health); the city of Richmond and Chesterfield and Henrico counties, Virginia (the Virginia Department of Health); the city of Baltimore, Maryland (the Baltimore City Health Department); and Hartford and New Haven counties, Connecticut (the Connecticut Department of Public Health). We did not include SSuN sites in geographic areas for which the CDC had no longer recommended fluoroquinolones,9 for which local health departments had previously issued recommendations against fluoroquinolone use in their jurisdictions,20–22 or that did not routinely collect treatment information. We refer to the geographic areas by the name of the relevant city.
To determine the effect of revised recommendations on the proportion of gonorrhea cases prescribed fluoroquinolones, we reviewed all gonorrhea cases reported from these sites with a treatment date from July 1, 2006 to May 31, 2008. We excluded cases if they were missing medication used or if they were recorded as not treated. We excluded cases from analysis by practice setting if they were missing practice setting information.
Study Outcomes
The primary outcome was absolute change in percentage of gonorrhea cases treated with fluoroquinolones after revised guidelines were announced that removed fluoroquinolones from recommended treatments for gonorrhea. We determined changes in prescribing for the proportion of cases treated with fluoroquinolones overall, by geographic area, and by practice setting. We divided the study period into fifty 14-day intervals (20 intervals before and 30 intervals after revised guidelines were released at the 21st interval on April 13, 2007). On the basis of reported treatment date, we determined the percentage of cases treated with fluoroquinolones among all cases treated with antimicrobials for each 14-day interval. In addition, we calculated the proportion of cases treated with fluoroquinolones by practice setting within each geographic area. For this stratified evaluation, we used monthly rather than 14-day intervals to reduce instability associated with small numbers of cases per interval.
We considered cases to have been treated with a fluoroquinolone if ciprofloxacin, levofloxacin, ofloxacin, gatifloxicin, norfloxacin, lomefloxacin, or gemifloxacin was prescribed. We counted cases treated with both a fluoroquinolone and a recommended treatment for gonorrhea (ceftriaxone or cefixime) as not treated with a fluoroquinolone. We evaluated each health jurisdiction and the most common practice settings for changes in prescribing after revised guidelines were released. Because of a relatively small number of cases reported from emergency departments, urgent care settings, and hospitals, and because in some cases “hospital” referred to an emergency department or urgent care setting, we combined cases from these practice settings into 1 category.
Statistical Analysis
We used autoregressive integrated moving average (ARIMA) interrupted time series analysis techniques23,24 to determine the effect of revised recommendations on prescribing fluoroquinolones for gonorrhea overall, by geographic area, and by practice setting. Briefly, ARIMA interrupted time series analysis is a quasiexperimental approach for evaluating longitudinal effects of an intervention. It has 2 components: an ARIMA noise component (Nt) and an intervention component (f (It)); Yt = Nt + f (It), where Yt is the outcome at time t. Nt accounts for the possible sources of noise that time series data may have; once the sources of noise are modeled, the impact of an intervention can be determined by testing a selected intervention component. The details of ARIMA time series analysis can be found elsewhere.24,25 We used a 3-stage approach including model identification, model estimation, and model evaluation to obtain an adequate ARIMA component model. We selected estimated parameters of the ARIMA component that were parsimonious (contained the fewest parameters allowing the model to effectively fit the data), were statistically significant, and satisfied conditions of stationarity and of invertibility. We evaluated the model residuals by residual autocorrelation function plot and the Ljung–Box Q test26 up to 24 interval lags. The residuals of all ARIMA models reported here corresponded to white noise.
We used 2 models to test the impact of revised recommendations on fluoroquinolone prescribing over time. One model assumed an abrupt and permanent pattern of impact (i.e., a sudden shift in the time series followed by maintenance at a new level consistent with an immediate effect of the intervention). The second model assumed a gradual and permanent pattern (i.e., a gradual change followed by a long-term effect on the time series). We modeled each of these 2 intervention patterns for all outcome time series, and we selected the pattern with the better fit for each series. An abrupt and temporary pattern of impact (i.e., a sudden shift followed by the disappearance of the change within a short period) did not seem plausible on the basis of visual inspection of the time series, and we did not model it. For both modeled patterns of impact, we determined the absolute change in fluoroquinolone prescribing immediately after the intervention (during the subsequent 2-week period). For series consistent with gradual and permanent patterns, which are consistent with a delayed effect of the intervention, we also determined shift rates (δ) ranging from 0 to 1, with higher values indicating a longer time before full realization of an effect.
We used the SAS-ARIMA procedure with maximum likelihood estimation to construct the ARIMA models.27,28 We performed all statistical analyses using SAS 9.1 for Windows (SAS Institute, Cary, NC). We considered P values < .05 to be statistically significant. All statistical tests were 2-tailed.
RESULTS
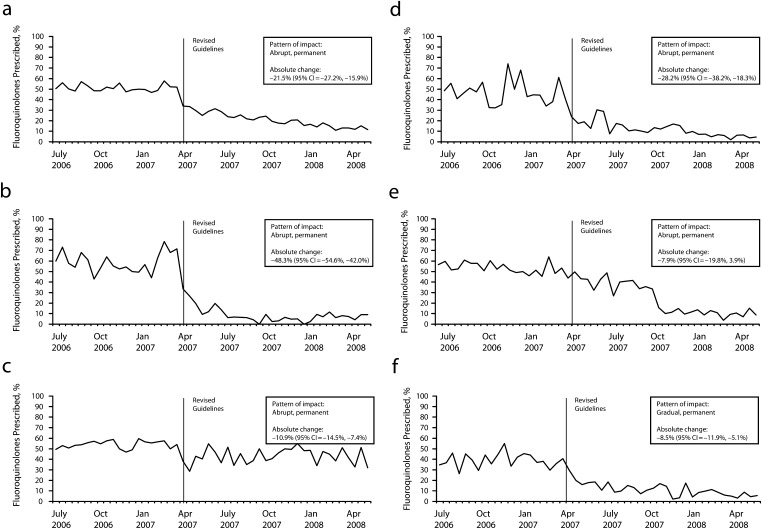
Of 16 126 cases reported as treated from the included SSuN sites between July 1, 2006 and May 31, 2008, 457 (2.8%) did not include information on the treatment used, and we excluded them, leaving 15 669 cases in the analysis. Overall, changes in prescribing were consistent with an abrupt and permanent pattern for effect of revised guidelines (data available as a supplement to the online version of this article at http://www.ajph.org). The proportion of gonorrhea cases treated with fluoroquinolones decreased 21.5% (95% confidence interval [CI] = 15.9%, 27.2%) by 2 weeks after revised guidelines were released (Figure 1).
FIGURE 1—
Fluoroquinolones prescribed for gonorrhea during biweekly intervals in (a) all 5 areas, (b) Denver, CO, (c) Minneapolis, MN, (d) Richmond, VA, (e) Baltimore, MD, and (f) Hartford and New Haven, CT: STD Surveillance Network, July 2006–May 2008.
Note. CI = confidence interval.
Fluoroquinolone Prescribing by Geographic Area
In Denver, Minneapolis, Richmond, and Baltimore, changes in prescribing were consistent with an abrupt and permanent pattern after revised guidelines were released (Figure 1). By 2 weeks after new guidelines were released, the proportion of gonorrhea cases treated with fluoroquinolones decreased by variable amounts in different areas (Figure 1): 48.3% (95% CI = 42.0%, 54.6%) in Denver, 10.9% (95% CI = 7.4%, 14.5%) in Minneapolis, and 28.2% (95% CI = 18.3%, 38.2%) in Richmond. Fluoroquinolone prescribing decreased nonsignificantly in Baltimore (7.9%; 95% CI = −3.9%, 19.8%). In Connecticut, changes in prescribing were consistent with a gradual and permanent pattern for effect of revised guidelines (Figure 1). The proportion of cases treated with fluoroquinolones decreased 8.5% (95% CI = 5.1%, 11.9%) by 2 weeks after the release of revised guidelines, then decreased at a shift rate of 0.72 (data available as a supplement to the online version of this article at http://www.ajph.org), indicating a relatively longer time before full realization of the effect of the revised recommendations.
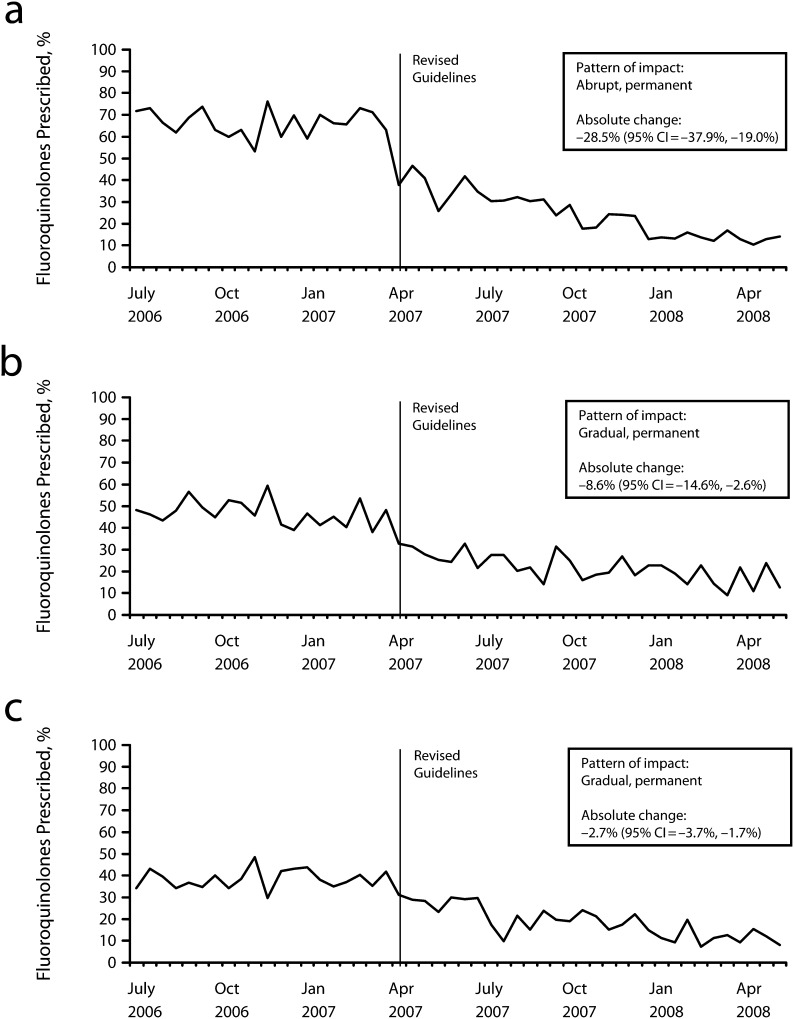
Fluoroquinolone Prescribing by Practice Setting
Of the 15 669 cases with treatment information from the included SSuN sites in the overall analysis, 13 846 (88.4%) included information on practice setting. Of these, 34.6% were treated in an STD clinic, 25.8% in a primary care setting, and 28.1% in an emergency department, urgent care setting, or hospital (Table 1). Changes in prescribing in STD clinics were consistent with an abrupt and permanent pattern for effect of revised guidelines (Figure 2). The proportion of gonorrhea cases treated with fluoroquinolones in STD clinics decreased 28.5% (95% CI = 19.0%, 37.9%) after revised guidelines were released (Figure 2).
TABLE 1—
Distribution of Gonorrhea Cases by Practice Setting: STD Surveillance Network, July 2006–May 2008
| Practice Settinga | Denver, CO, No. (%) | Minneapolis, MN, No. (%) | Hartford and New Haven, CT, No. (%) | Baltimore, MD, No. (%) | Richmond, VA, No. (%) | Total, No. (%) |
| STD clinic | 1058 (38.8) | 876 (30.5) | 424 (20.4) | 1455 (37.3) | 972 (42.9) | 4785 (34.6) |
| Primary care | 641 (23.5) | 944 (32.9) | 672 (32.3) | 694 (17.8) | 626 (27.6) | 3577 (25.8) |
| Emergency department or urgent care | 180 (6.6) | 657 (22.9) | 530 (25.5) | 308 (7.9) | 544 (24.0) | 2219 (16.0) |
| Hospital | 439 (16.1) | 0 (0.0) | 1 (0.0) | 1228 (31.5) | 5 (0.2) | 1673 (12.1) |
| Family planning | 144 (5.3) | 182 (6.3) | 345 (16.6) | 219 (5.6) | 69 (3.0) | 959 (6.9) |
| Jail or prison | 105 (3.9) | 33 (1.1) | 51 (2.5) | 0 (0.0) | 12 (0.5) | 201 (1.5) |
| Otherb | 159 (5.9) | 180 (6.3) | 55 (2.6) | 0 (0.0) | 38 (1.6) | 432 (3.1) |
| Total with practice setting information | 2726 (100.0) | 2872 (100.0) | 2078 (100.0) | 3904 (100.0) | 2266 (100.0) | 13 846 (100.0) |
Note. STD = sexually transmitted disease.
Of those with a known practice setting.
Includes HIV care center, prenatal, school, military, obstetrics and gynecology, and outreach.
FIGURE 2—
Fluoroquinolones prescribed for gonorrhea during biweekly intervals in (a) sexually transmitted disease clinics, (b) primary care, and (c) emergency rooms, urgent care, and hospitals: Sexually Transmitted Disease Surveillance Network, July 2006–May 2008.
Note. CI = confidence interval.
For patients seen in primary care and for those seen in emergency departments, urgent care, and hospitals, changes in prescribing were most consistent with a gradual and permanent pattern for effect of revised guidelines (Figure 2). At 2 weeks after the release of revised national treatment guidelines, the proportion of cases treated with fluoroquinolones decreased 8.6% (95% CI = 2.6%, 14.6%) in primary care settings and just 2.7% (95% CI = 1.7%, 3.7%) in emergency departments, urgent care clinics, and hospitals, then decreased at gradual shift rates of 0.62 for primary care settings and 0.90 for emergency departments, urgent care clinics, and hospitals (data available as a supplement to the online version of this article at http://www.ajph.org).
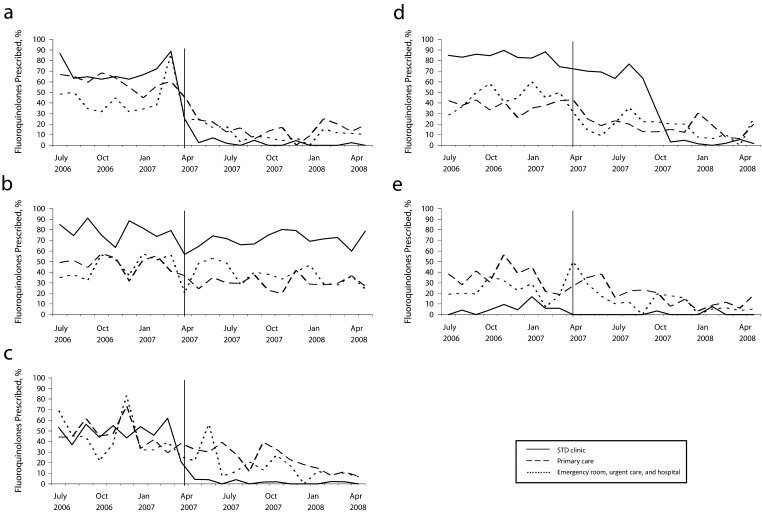
Fluoroquinolone Prescribing by Practice Setting Within Geographic Areas
Numbers of cases prescribed fluoroquinolones by practice setting were insufficient for ARIMA time series analysis when stratified by geographic area. Evaluation of monthly trends over time revealed 3 patterns of fluoroquinolone prescribing in STD clinics. In Denver, Richmond, and Hartford and New Haven, fluoroquinolone prescribing in STD clinics decreased to nearly zero around the time of the revised treatment recommendations (Figure 3). In Minneapolis, fluoroquinolone prescribing in STD clinics did not appear to decrease substantially (Figure 3). In Baltimore, fluoroquinolone prescribing decreased to nearly zero several months after revised recommendations were released (Figure 3). In all areas, fluoroquinolone prescribing decreased in primary care and in emergency department, urgent care, and hospital settings. In most areas, these decreases were not as substantial as was the decrease in STD clinics.
FIGURE 3—
Fluoroquinolones as percentage of all antimicrobials prescribed for gonorrhea during monthly intervals in (a) Denver, CO, (b) Minneapolis, MN, (c) Richmond, VA, (d) Baltimore, MD, and (e) Hartford and New Haven, CT, by area and practice setting: STD Surveillance Network, July 2006–May 2008.
Note. STD = sexually transmitted disease.
DISCUSSION
We used SSuN—a sentinel surveillance system containing enhanced data, including treatment information on all reported gonorrhea cases from selected jurisdictions—to evaluate the effect of revised national guidelines for the treatment of gonorrhea. We found overall fluoroquinolone use decreased more than 20% after publication and dissemination of revised national guidelines that removed fluoroquinolones from recommended treatments for gonorrhea. Fluoroquinolone prescribing decreased significantly and by large magnitudes in Denver and Richmond, decreased significantly but by smaller magnitudes in Hartford and New Haven and in Minneapolis, and decreased nonsignificantly in Baltimore. In most areas, fluoroquinolone prescribing decreased to nearly zero in STD clinics but did not decrease as substantially in primary care and in emergency department, urgent care, and hospital settings.
Fluoroquinolone prescribing decreased significantly in all practice settings but more quickly and by a greater magnitude in STD clinics. STD clinics were the only practice setting where prescribing fit an abrupt and permanent rather than a gradual and permanent pattern of change, reflecting the greater speed with which prescribing changed in STD clinics. Although the Interagency Task Force on Antimicrobial Resistance, cochaired by the CDC, the Food and Drug Administration, and the National Institutes of Health, recommended monitoring antimicrobial use as a “Top Priority Action Item to Combat Antimicrobial Resistance,”29 there are limited data available on antibiotic prescribing practices for infections with potential for increased antibiotic resistance, including N. gonorrhoeae. These findings add to our understanding of how providers respond to guidelines by identifying differences in prescribing practices among different provider specialties in selected areas of the United States.
Differences in fluoroquinolone use by area may be partly explained by local health department communications to providers. We reviewed local and state health department communications regarding fluoroquinolones for the areas and periods studied. The Colorado Department of Public Health and Environment announced the CDC's revised recommendations through a press release on April 13, 2007.30 Denver's STD clinic changed its prescribing policy and sent updates to all providers in Denver Health, the largest provider for inner-city Denver. Because local resistance rates among heterosexuals were low, on September 25, 2007, the Minnesota Department of Health recommended “the continued cautious use of [fluoroquinolones] for … gonorrhea in heterosexuals.”31 The Minnesota Department of Health subsequently reevaluated fluoroquinolone resistance to N. gonorrhoeae among heterosexuals in Minnesota, found resistance had increased from 0.8% in 2006 to 4.5% by December 2007, and released a dear colleague letter on June 4, 2008 stating that fluoroquinolones were no longer recommended for gonorrhea treatment in Minnesota.32 Our analysis does not cover the period after this 2008 announcement. The Virginia Department of Health mailed an article about the CDC's revised guidelines to local health departments and to each licensed physician in the state in May 2007. The Baltimore City Health Department sent a letter to providers in April 2007 stating that ceftriaxone was now the preferred treatment for gonorrhea but that because local data showed low prevalence of ciprofloxacin-resistant N. gonorrhoeae (2.0% in 200733), alternative treatment with fluoroquinolones could be used if there was no history of travel in the past 2 months and no reported male same-sex contact or sexual contact with partners in these groups. In addition, because resistance to fluoroquinolones was known to be very low among heterosexual males in Baltimore, STD clinics continued to dispense fluoroquinolones to heterosexuals while waiting for stocks of formulary medications to be depleted. They then changed to cephalosporins several months later as standard gonorrhea treatment (informal communication, Emily Erbelding, March 25, 2008). The lack of detection by interrupted time series analysis of a significant decrease in fluoroquinolone prescribing for treatment of gonorrhea in Baltimore is most likely because the substantial local decreases in fluoroquinolone prescribing followed the release of revised national guidelines by several months and therefore could not be attributed to this intervention. There was no formal health department dissemination effort in Connecticut. Our findings suggest that local communications may have amplified or moderated national messages about fluoroquinolone prescribing.
Several factors may explain differential changes in fluoroquinolone use by practice setting. Primary care providers may find it difficult to prescribe intramuscular antibiotics. For most of the study period (through April 2008),34 cefixime tablets were unavailable. Providers in STD clinics commonly follow protocols and may prescribe medications from a set formulary. Changes made by STD clinic directors may, therefore, have a larger, more coordinated impact than do changes made by individual clinicians in more generalist settings. In addition, STD clinics tend to receive state or county funding, which provides a direct relationship with governmental STD programs and additional sources of communication regarding revised treatment guidelines.
Our analysis is subject to several limitations. It is difficult to determine on the basis of observational data whether changes in prescribing were the result of revised guidelines. Still, the rapidity of decreases in fluoroquinolone use after the release of the revised guidelines overall and in most areas supports the conclusion that changes in prescribing were related to this intervention. Although we were able to stratify by practice setting given enhanced data in SSuN, the provider data in SSuN still consist of crude categories, and it is difficult to standardize across sites (e.g., medicine clinics in hospitals might be recorded as “hospital” at 1 site and “primary care” at another). In addition, we could not examine several practice settings (e.g., family planning, prisons) because of relatively few cases. Because we selected cases by treatment date to classify cases into the appropriate time interval in relationship to revised guidelines, we were unable to evaluate cases missing the treatment date. A review of cases by report date (the date that the case was reported to a public health department, which may not be the same as the treatment date) from July 1, 2006 to May 31, 2008 revealed varying completeness of the treatment date. By excluding cases without the treatment date (and all unreported cases), we may have overestimated adherence to guidelines because there may be a correlation between providers who report more complete information and those who are aware of and follow treatment recommendations. Whether changes in prescribing were related to awareness of guidelines, perceptions of the importance of following guidelines, or other factors is unknown. Finally, our sample cannot be considered nationally representative. However, the sites were in 5 geographically diverse areas, and cases reported within the selected jurisdictions provided a comprehensive picture of gonorrhea morbidity reported to public health departments.
The CDC has defined the appropriate prescribing of antimicrobials as the prescription of antimicrobial agents only when they are likely to benefit the patient and using agents that target the likely pathogens at the proper dose and duration.35 According to data from the National Ambulatory Medical Care Survey, more than 40% of antimicrobial prescriptions provided in physician offices in 1992 were inappropriate.36 Multiple methods to decrease inappropriate prescribing—including prescribing restrictions, reminders, printed materials, and feedback—have been evaluated, but it has been unclear which elements are most effective in influencing antimicrobial prescribing.37,38
Our results demonstrate that widely disseminated and publicized national recommendations did substantially affect prescribing behavior in most areas and all practice settings and suggest that local public health messages can also modify their impact. However, many cases of gonorrhea were still treated with fluoroquinolones a year after the release of revised guidelines that no longer recommended fluoroquinolones. It is critical to reach providers to ensure that patients are treated with effective therapy. Additional mechanisms are needed to encourage appropriate antimicrobial prescribing among primary care, emergency department, and hospital providers. Because we saw greater impact in STD clinics, where set formularies are often used, mechanisms to influence prescribing in other settings might include hospital and managed care formulary changes. In addition, the identification of effective oral antibiotic options for the treatment of gonorrhea should be encouraged to ensure that viable treatment options are available in primary care settings. Monitoring for antimicrobial resistance to N. gonorrhoeae continues to be critical because cephalosporins are the only remaining class of antimicrobials for gonorrhea treatment. Prompt changes in prescribing practices may become even more critical if resistance emerges to cephalosporins.
Acknowledgments
The authors thank Jennifer Bissette, BS, of the Virginia Department of Health and Darlene Davis of the Centers for Disease Control and Prevention for assistance with data acquisition and management. We also thank the STD Surveillance Network (SSuN) collaborators from state and local health departments, who were instrumental in development and implementation of SSuN.
Human Participant Protection
No protocol approval was needed because we obtained data from existing sources. The Centers for Disease Control and Prevention determined the STD Surveillance Network to be a nonresearch, public health activity to control disease and conduct surveillance.
References
- 1.Weinstock H, Berman S, Cates W., Jr Sexually transmitted diseases among American youth: incidence and prevalence estimates, 2000. Perspect Sex Reprod Health. 2004;36(1):6–10. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2008. Atlanta, GA: US Department of Health and Human Services; November 2009. [Google Scholar]
- 3.US Department of Health and Human Services. Healthy People 2010: Volume 2. 2nd ed Washington, DC: Government Printing Office; November 2000. [Google Scholar]
- 4.Fleming DT, Wasserheit JN. From epidemiologic synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75(1):3–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Workowski KA, Berman SM, Douglas JM. Emerging antimicrobial resistance in Neisseria gonorrhoeae: urgent need to strengthen prevention strategies. Ann Intern Med. 2008;148(8):606–613. [DOI] [PubMed] [Google Scholar]
- 6.Wang SA, Harvey AB, Conner SMet al. Antimicrobial resistance for Neisseria gonorrhoeae in the United States, 1988–2003: the spread of fluoroquinolone resistance. Ann Intern Med. 2007;147(2):81–88. [DOI] [PubMed] [Google Scholar]
- 7.Newman LM, Moran JS, Workowski KA. Update on the management of gonorrhea in adults in the United States. Clin Infect Dis. 2007;44(suppl 3):S84–S101. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Fluoroquinolone resistance in Neisseria gonorrhoeae, Hawaii, 1999, and decreased susceptibility to azithromycin in N. gonorrhoeae, Missouri, 1999. MMWR Morb Mortal Wkly Rep. 2000;49(37):833–837. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Increases in fluoroquinolone-resistant Neisseria gonorrhoeae—Hawaii and California, 2001. MMWR Morb Mortal Wkly Rep. 2002;51(46):1041–1044. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Increases in fluoroquinolone-resistant Neisseria gonorrhoeae among men who have sex with men—United States, 2003, and revised recommendations for gonorrhea treatment, 2004. MMWR Morb Mortal Wkly Rep. 2004;53(16):335–338. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Update to CDC's sexually transmitted diseases treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal infections. MMWR Morb Mortal Wkly Rep. 2007;56(14):332–336. [PubMed] [Google Scholar]
- 12.Altman LK. Agency urges a change in antibiotics for gonorrhea. New York Times. April 13, 2007. [Google Scholar]
- 13.Yee D. As Gonorrhea Joins List of “Superbugs,” CDC Says Old Drug Therapy No Longer Effective. Associated Press; April 13, 2007. Available at: http://www.aegis.com/news/ap/2007/AP070424.html. Accessed April 11, 2009. [Google Scholar]
- 14.Stein S. Drugs losing efficacy against gonorrhea; CDC tells doctors to change antibiotics. The Washington Post. April 13, 2007. [Google Scholar]
- 15.Robin R. Gonorrhea mutates to resist antibiotic treatment: development is a “public health wake-up call,” CDC official warns. USA Today. April 12, 2007. [Google Scholar]
- 16.Chong J. Drug-resistant gonorrhea spreading rapidly in U.S. Los Angeles Times. April 13, 2007. [Google Scholar]
- 17.Hogben M, Wimberly YH, Moore S. Estimating dissemination of Centers for Disease Control and Prevention Sexually Transmitted Disease Treatment Guidelines from a survey of physicians. Int J STD AIDS. 2007;18(5):318–320. [DOI] [PubMed] [Google Scholar]
- 18.Asch SM, Sa'adah MG, Lopez R, Kokkinis A, Richwald GA, Rhew DC. Comparing quality of care for sexually transmitted diseases in specialized and general clinics. Public Health Rep. 2002;117(2):157–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roush S, Birkhead G, Koo D, Cobb A, Fleming D. Mandatory reporting of diseases and conditions by health care professionals and laboratories. JAMA. 1999;282(2):164–170. [DOI] [PubMed] [Google Scholar]
- 20.Washington State Department of Health. “Dear Colleague” Letter; March 2, 2004 Available at: http://www.cdc.gov/std/Gonorrhea/arg/WAhealthalert.pdf. Accessed January 8, 2010.
- 21.New York City Department of Health and Mental Hygiene. Health Department Issues Advisory on Gonorrhea in New York City; April 29, 2004. Available at: http://www.nyc.gov/html/doh/html/press_archive04/pr043-0429.shtml. Accessed January 8, 2010. [Google Scholar]
- 22.Philadelphia Department of Public Health. Health Advisory; April 12, 2007. Available at: https://hip.phila.gov/xv/Portals/0/HIP/Health_Alerts/2007/PDPH-HAN_Advisory_4_GC_Resistance_Combined_04132007.pdf. Accessed January 8, 2010. [Google Scholar]
- 23.Cook TD, Campbell DT. Quasi-experiments: Interrupted Time-Series Designs in Quasi-experimentation: Design and Analysis Issues for Field Settings. Boston: Houghton Mifflin Company; 1979. [Google Scholar]
- 24.McDowall D, McCleary R, Meidinger EE, Hay RA. Interrupted Time Series Analysis. Thousand Oaks, CA: Sage Publications; 1980. [Google Scholar]
- 25.Pankratz A. Forecasting With Dynamic Regression Models. New York: John Wiley and Sons; 1991. [Google Scholar]
- 26.Ljung GM, Box GEP. On a measure of lack of fit in time series models. Biometrika. 1978;65(2):297–303. [Google Scholar]
- 27.Brocklebank JC, Dickey DA. SAS for Forecasting Time Series. Cary, NC: SAS Institute; 2003. [Google Scholar]
- 28.SAS Institute, Inc. The ARIMA Procedure. Cary, NC; 2009. Available at: http://support.sas.com/documentation/cdl/en/etsug/60372/HTML/default/viewer.htm#arima_toc.htm. Accessed May 6, 2010. [Google Scholar]
- 29.Interagency Task Force on Antimicrobial Resistance. A Public Health Action Plan to Combat Antimicrobial Resistance. Part 1: Domestic Issues. 2001:1–43. Available at: http://www.cdc.gov/drugresistance/actionplan/aractionplan-archived.pdf. Accessed September 8, 2011. [Google Scholar]
- 30.Colorado Department of Public Health and Environment. Gonorrhea Treatment Changed Due to Current Treatment Resistance to Antibiotics; April 13, 2007. Available at: http://www.cdphe.state.co.us/release/2007/041307.html. Accessed May 28, 2010. [Google Scholar]
- 31.Minnesota Department of Health. “Dear Colleague” Letter; September 23, 2007. Available at: http://www.health.state.mn.us/divs/idepc/dtopics/stds/cdcguidelinesgctx.pdf. Accessed March 27, 2010.
- 32.Minnesota Department of Health. “Dear Colleague” Letter; June 4, 2008. Available at: http://www.health.state.mn.us/divs/idepc/dtopics/stds/DearColleague062008.pdf. Accessed February 28, 2011.
- 33.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2007 Supplement, Gonococcal Isolate Surveillance Project (GISP) Annual Report 2007. Atlanta, GA: US Department of Health and Human Services; March 2009. [Google Scholar]
- 34.Centers for Disease Control and Prevention. Availability of cefixime 400 mg tablets—United States, April 2008. MMWR Morb Mortal Wkly Rep. 2008;57(16):435. [PubMed] [Google Scholar]
- 35.Besser RE. Antimicrobial prescribing in the United States: good news, bad news. Ann Intern Med. 2003;138(7):605–606. [DOI] [PubMed] [Google Scholar]
- 36.Emmer CL, Besser RE. Combating antimicrobial resistance: intervention programs to promote appropriate antibiotic use. Infect Med. 2002;19(4):160–173. [Google Scholar]
- 37.Arnold SR, Straus SE. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev. 2005(4):CD003539 DOI:10.1002/14651858.CD003539.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Davey P, Brown E, Fenelon Let al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. 2005(4):CD003543 DOI:10.1002/14651858.CD003543.pub2. [DOI] [PubMed] [Google Scholar]