Abstract
Objectives. The purpose of our study was to more accurately characterize people reporting influenza-like illness (ILI) and evaluate trends in health care seeking and influenza diagnosis and treatment during the 2009 influenza pandemic.
Methods. From September 2009 to March 2010, we ascertained ILI (fever with cough or sore throat), health care seeking, and clinical diagnosis and treatment of influenza with influenza antiviral drugs among adults in 51 jurisdictions, and ILI and health care seeking among children in 41 jurisdictions.
Results. Among 216 431 adults and 43 511 children, 8.1% and 28.4% reported ILI, respectively. ILI peaked during November interviews and was higher among young people and American Indian/Alaska Natives. Of those with ILI, 40% of adults and 56% of children reported seeking health care; 26% of adults who sought care reported receiving a diagnosis of influenza. Of adults reporting an influenza diagnosis, 36% were treated with influenza antiviral drugs; treatment was highest among adults aged 18 to 49 years.
Conclusions. Analysis of ILI data from the Behavioral Risk Factor Surveillance System enabled a better understanding of the factors associated with self-reported ILI, health care seeking, and clinical influenza diagnosis and treatment, and will help inform year-to-year influenza trends.
The influenza A (H1N1) pdm09 virus (pH1N1) caused an estimated 61 million infections, 274 000 hospitalizations, and 12 470 deaths in the United States from April 2009 to April 2010.1 Surveillance systems in place at the start of the pandemic provided data describing patient visits to health care providers for influenza-like illness (ILI) and reports of influenza-associated hospitalizations and deaths.2 However, no existing influenza surveillance system monitored influenza among community-dwelling individuals outside of the health care system. Community-level surveillance for influenza is important for accurate estimation of the total influenza disease burden, which includes medically attended laboratory-confirmed cases reported to public health, medically attended cases for which diagnostic testing is not performed, and cases for which medical attention is not sought.3
To better characterize people reporting ILI in the United States and to evaluate trends in health care–seeking behavior and clinical diagnosis and treatment of influenza during the pH1N1 pandemic, the Centers for Disease Control and Prevention used the Behavioral Risk Factor Surveillance System (BRFSS) to collect information on ILI. Although identification of laboratory-confirmed cases of infection would best estimate true influenza burden, community-level surveillance does not routinely include this information. Moreover, because diagnostic testing is not always performed for patients presenting with symptoms of influenza virus infection, ILI has traditionally been used to monitor influenza activity. Temporally, ILI correlates well with the weekly number of positive influenza test results and is a good predictor of infection among patients when influenza is circulating.4–7 In this article, we describe the design and implementation of a community survey administered via the BRFSS and present surveillance data collected from September 2009 to March 2010 in the United States.
METHODS
The BRFSS is a state-based surveillance system that measures health behaviors in the United States. The BRFSS is a random-digit-dialed telephone survey of the noninstitutionalized US population aged 18 years or older. It is the largest continuously conducted telephone survey in the world with more than 400 000 adult interviews completed each year. This system is the main source for states of data on the prevalence of health-risk behaviors, chronic health conditions, and preventive health services related to chronic disease and injury.8 BRFSS survey methodology is described elsewhere.9
From September 1, 2009, to March 31, 2010, BRFSS respondents in 49 states (excluding Vermont), the District of Columbia, and Puerto Rico were interviewed using a new module for ILI; in 41 of the 51 states and territories (excluding Alabama, Arkansas, Colorado, Florida, Minnesota, Missouri, New Hampshire, North Carolina, South Carolina, and Tennessee), the respondent's child was also eligible to participate through a proxy interview with an adult. Those who reported fever with cough or sore throat in the 30 days preceding the interview were defined as having ILI. To determine the presence of ILI among adult respondents, 2 questions were asked: “During the past month, were you ill with a fever?” If respondents answered yes, they were asked, “Did you also have a cough and/or sore throat?” Answering “yes” to both questions was classified as ILI. To determine the presence of ILI among children, adult respondents were asked 1 question about their child: “Has the child had a fever with cough and/or sore throat during the past month?” A “yes” answer was classified as ILI. To determine whether medical care was sought, respondents with ILI were asked, “Did you [or your child] visit a doctor, nurse, or other health professional for this illness?” Adults with ILI who sought medical care for their illness were asked, “What did the doctor, nurse, or other health professional tell you? Did they say …” and given the choice of 3 responses: (1) “You had regular influenza or the flu,” (2) “You had swine flu, also known as H1N1 or novel H1N1,” or (3) “You had some other illness, but not the flu.” A clinical diagnosis of influenza was defined as either the first or the second response. To determine whether antiviral treatment was given for the illness, adults were also asked, “Did you receive Tamiflu® or oseltamivir or an inhaled medicine called Relenza® or zanamivir to treat this illness?” Clinical diagnosis and receipt of influenza antiviral drug treatment were not ascertained for children.
ILI, health care seeking, clinical diagnosis, and influenza antiviral drug receipt among those diagnosed with influenza were evaluated by month of illness onset, gender, age group in years (0–4, 5–11, 12–17, 18–49, 50–64, and ≥ 65), racial/ethnic group, and census region. Unknown, missing, or refused responses were excluded from analysis. We grouped BRFSS respondents into 5 racial/ethnic categories: non-Hispanic (NH) White, NH Black (NH Black), Hispanic, American Indian/Alaska Native (AI/AN), and other race NH (including Asians, Native Hawaiians, and other Pacific Islanders; people of other races; and people who identified more than 1 race). Because the age distributions of racial/ethnic groups differed, we age adjusted prevalence estimates by race/ethnicity using the standard year 2000 projected US population.10 We used SAS-callable SUDAAN Version 10 statistical software (Research Triangle Institute, Research Triangle Park, NC) to calculate population-weighted estimates and corresponding standard errors, 95% confidence intervals, and P values, taking into account the design of the BRFSS sampling plan. We used the χ2 test to evaluate differences by interview month and census region and linear contrasts to evaluate differences in age group, sex, and racial/ethnic categories in self-reported ILI, health care–seeking behavior, influenza diagnosis, and antiviral drug receipt. Statistical significance was set at α ≤ .05.
RESULTS
From September 2009 through March 2010, between 27 000 and 33 000 adult interviews and 5000 and 7000 child interviews were conducted each month; this report includes responses obtained from 216 431 adult interviews and 43 511 child interviews. Response rates for BRFSS were calculated using Council of American Survey and Research Organizations guidelines. Median survey response rates were 55% (state range = 24%–74%), calculated as the percentage of people who completed interviews among all eligible people, including those who were not contacted. Median cooperation rates were 75% (state range = 55%–95%), calculated as the percentage of people who completed interviews among all eligible people who were contacted.
Reported Influenza-Like Illness Among Adults and Children
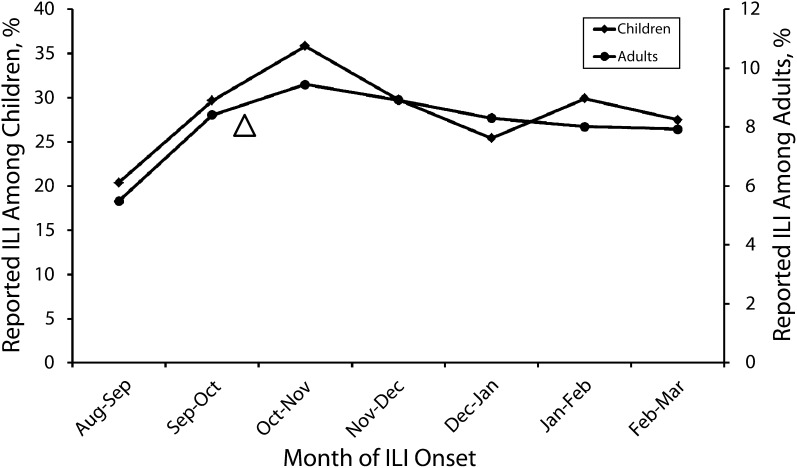
From September 2009 through March 2010, the average monthly percentage of adults reporting ILI was 8.1%, and the percentage of children with reported ILI was 28% (Tables 1 and 2). Reported ILI for both groups varied by month (P < .01 for both comparisons). ILI peaked among adults (9.5%) and children (36%) during November interviews, which corresponds with illness in October or November, and was lowest among adults (5.5%) and children (20%) during September interviews, which corresponds with illness in August or September (Figure 1).
TABLE 1—
Average Monthly Percentage of Reported ILI in the Month Preceding Interview, Health Care Seeking, Influenza Diagnosis, and Antiviral Treatment Among Adults, by Selected Demographics: BRFSS, United States, September 1, 2009–March 31, 2010
| Reported ILI |
Sought Health Care for ILI |
Clinical Diagnosis of Influenza Among Those Who Sought Health Care for ILI |
Antiviral Treatment Among Those Clinically Diagnosed With Influenza |
|||||
| Demographics | Sample Size, No. | % (95% CI) | Sample Size, No. | % (95% CI) | Sample Size, No. | % (95% CI) | Sample Size, No. | % (95% CI) |
| Total | 216 431 | 8.1 (7.8, 8.4) | 14 601 | 40 (38, 42) | 6148 | 26 (23, 29) | 1258 | 36 (31, 41) |
| Sex | ||||||||
| Male | 81 931 | 7.1 (6.7, 7.6) | 4609 | 33 (30, 36) | 1567 | 27 (22, 32) | 360 | 34 (26, 44) |
| Female | 134 500 | 9.0* (8.6, 9.4) | 9992 | 45* (43, 47) | 4581 | 26 (23, 28) | 898 | 37 (31, 43) |
| Race/ethnicity | ||||||||
| White, non-Hispanic | 169 376 | 8.4 (8.1, 8.7) | 11 126 | 42 (40, 44) | 4600 | 21 (19, 24) | 862 | 36 (31, 42) |
| Black, non-Hispanic | 17 129 | 7.2** (6.3, 8.2) | 1061 | 45 (38, 51) | 504 | 30 (20, 41) | 93 | 31a (19, 45) |
| Hispanic | 14 508 | 7.5 (6.7, 8.4) | 1128 | 43 (37, 48) | 472 | 39** (30, 47) | 160 | 33a (22, 46) |
| American Indian/Alaska Native | 2916 | 16** (12, 22) | 370 | 39 (29, 51) | 172 | 25 (14, 40) | 44 | 29a (12, 54) |
| Other race, Non-Hispanic | 8618 | 9.1 (7.8, 11) | 708 | 40 (34, 47) | 306 | 38** (28, 49) | 81 | 37a (23, 55) |
| Age group, y | ||||||||
| 18–49 | 71 684 | 10*** (10, 11) | 7051 | 37*** (35, 40) | 2708 | 29*** (26, 33) | 667 | 39*** (33, 46) |
| 50–64 | 72 167 | 6.8*** (6.4 ,7.2) | 5053 | 43*** (40, 46) | 2178 | 20 (17, 23) | 403 | 27 (21, 35) |
| ≥ 65 | 70 880 | 3.2 (3.0, 3.5) | 2418 | 56 (53, 60) | 1224 | 17 (14, 22) | 179 | 22 (14, 34) |
| Census Region | ||||||||
| Northeast | 33 440 | 7.7 (7.0, 8.4) | 1983 | 44† (40, 49) | 809 | 28† (22, 34) | 194 | 37a (26, 50) |
| Midwest | 51 872 | 7.8 (7.3, 8.3) | 3279 | 39† (36, 43) | 1307 | 22† (18, 27) | 268 | 30 (21, 40) |
| South | 74 424 | 8.4 (8.0, 8.9) | 5369 | 42† (39, 45) | 2564 | 23† (19, 28) | 428 | 45 (36, 54) |
| West | 54 423 | 8.2 (7.5, 8.8) | 3847 | 33† (30, 37) | 1384 | 34† (28, 41) | 347 | 29 (20, 40) |
Note. BRFSS = Behavioral Risk Factor Surveillance System; CI = confidence interval; ILI = influenza-like illness.
Estimate might be unreliable because the unweighted sample size is > 50 or the CI half width is > 10. Caution should be used when interpreting this estimate.
*P < .05, with men as reference group.
**P < .05, with non-Hispanic White as reference group.
***P < .05, with respondents aged ≥ 65 years as reference group.
†P < .05, χ2 test among census region.
TABLE 2—
Average Monthly Percentage of Reported ILI in the Month Preceding Interview and Health Care Seeking Among Children, by Selected Demographics: BRFSS, September 1, 2009–March 31, 2010
| Reported ILI |
Sought health care for ILI |
|||
| Demographic | Sample Size, No. | % (95% CI) | Sample Size, No. | % (95% CI) |
| Total | 43 511 | 28 (28, 29) | 12 628 | 56 (55, 58) |
| Sex | ||||
| Male | 21 619 | 28 (27, 29) | 6098 | 55 (53, 57) |
| Female | 19 821 | 29 (28, 30) | 5950 | 57 (55, 60) |
| Race/ethnicity | ||||
| Non-Hispanic White | 28 930 | 30 (29, 31) | 8632 | 52 (50, 54) |
| Non-Hispanic Black | 3756 | 23* (21, 26) | 905 | 61* (55, 66) |
| Hispanic | 6112 | 28 (26, 30) | 1736 | 64* (59, 67) |
| American Indian/Alaska Native | 960 | 41* (31, 51) | 324 | 82* (73, 88) |
| Other race, non-Hispanic | 3127 | 29 (26, 32) | 890 | 51 (45, 56) |
| Age group, y | ||||
| 0–4 | 9985 | 33** (31, 35) | 3262 | 67** (64, 70) |
| 5–11 | 15 506 | 29** (28, 31) | 4697 | 52 (50, 55) |
| 12–17 | 17 944 | 24 (23, 25) | 4648 | 51 (48, 54) |
| Census region | ||||
| Northeast | 6812 | 26*** (24, 28) | 1040 | 58*** (54, 62) |
| Midwest | 11 604 | 29*** (28, 31) | 1648 | 48*** (45, 51) |
| Southa | 11 259 | 30*** (28, 31) | 2161 | 66*** (63, 68) |
| West | 13 288 | 28*** (26, 30) | 1849 | 50*** (47, 53) |
Note. BRFSS = Behavioral Risk Factor Surveillance System; CI = confidence interval; ILI = influenza-like illness.
Of 17 jurisdictions in this census region, 6 (Alabama, Arkansas, Florida, North Carolina, South Carolina, and Tennessee) did not administer the child portion of the survey and are not included in these results.
*P < .05, with non-Hispanic White as the reference group.
**P < .05, with respondents aged 12–17 years as reference group.
***P < .05, χ2 test among census region.
FIGURE 1—
Reported influenza-like illness (ILI) among adults and children, by onset period: Behavioral Risk Factor Surveillance System, United States, September 1, 2009–March 31, 2010.
Note. ILI = influenza-like illness. Triangle indicates peak of ILI visits to outpatient providers and peak in the weekly number of positive influenza test results.2
Among adults, more women (9.0%) reported ILI than men (7.1%; P < .01), but no statistically significant difference by sex was observed among children. Reported ILI decreased with increasing age for both groups. A higher percentage of adults aged 18 to 49 years (10%) and 50 to 64 years (6.8%) reported ILI than of adults aged 65 years or older (3.2%; P < .01 for both comparisons), and a higher percentage of children aged 0 to 4 years (33%) and 5 to 11 years (29%) were reported to have ILI than of children aged 12 to 17 years (24%; P < .01 for both comparisons). AI/AN adults (16%) and children (41%) reported more ILI than did NH White adults (8.4%; P < .01) and children (30%; P = .03); NH Black adults (7.2%) and children (23%), however, reported less ILI than did NH White adults (P = .02) and children (P < .01). Adults in different census regions reported similar ILI prevalence, but reported ILI among children varied by census region (P = .03) and ranged from 30% in the South census region to 26% in the Northeast census region. Reported ILI also varied by state and ranged from 5.3% among adults from Delaware to 12% among adults from Arkansas and from 21% among children from the District of Columbia to 33% among children from Arizona, Nebraska, Oklahoma, Utah, and West Virginia.
Health Care Seeking for Influenza-Like Illness
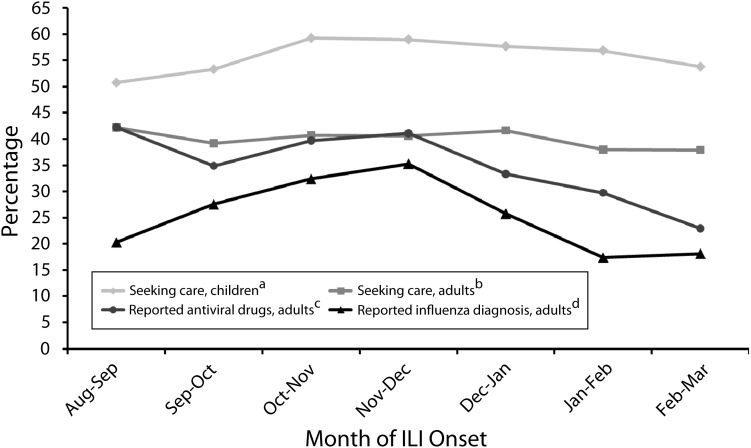
A total of 40% of adults and 56% of children reported seeking health care for their ILI episode (Tables 1 and 2); this proportion did not vary significantly by interview month for either group (Figure 2). Among adults, more women (45%) reported seeking health care than men (33%; P < .01), but no statistically significant difference by sex was observed among children. A lower percentage of adults aged 18 to 49 years (37%) and 50 to 64 years (43%) reported seeking health care than of adults aged 65 years or older (56%; P < .01 for both comparisons), and a higher percentage of children aged 0 to 4 years (67%) were reported to have sought health care than of children aged 12 to 17 years (51%; P < .01).
FIGURE 2—
Monthly percentage of health care seeking among children and health care seeking, influenza diagnosis, and antiviral treatment among adults, by onset period: Behavioral Risk Factor Surveillance System, United States, September 1, 2009–March 31, 2010.
Note. ILI = influenza-like illness.
aAmong children with ILI.
bAmong adults with ILI.
cAmong adults with ILI who sought care and recalled an influenza diagnosis.
dAmong adults with ILI who sought care.
No statistically significant difference by race/ethnicity was observed among adults in health care seeking, but NH Black (61%), Hispanic (64%), and AI/AN (82%) children were reported to have sought health care more often than NH White children (52%; P < .01 for all 3 comparisons). Health care seeking among adults and children varied by census region (P < .01 for both comparisons) and ranged from 44% among adults from the Northeast census region to 33% among adults from the West region and from 66% among children from the South census region to 48% among children from the Midwest census region.
Reported Clinical Influenza Diagnosis Among Adults
Of adults who sought health care for their ILI episode, 26% reported being given an influenza diagnosis (Table 1). Reporting an influenza diagnosis varied by interview month (P < .01) and peaked during November interviews (27%), which corresponds with illness in October or November, and was lowest during February interviews (17%), which corresponds with illness in January or February (Figure 2).
No statistical difference was noted by sex, but reporting an influenza diagnosis varied by age. A higher percentage of adults aged 18 to 49 years (29%) reported an influenza diagnosis than of adults aged 65 years or older (17%; P < .01). Compared with NH White adults (21%), Hispanic (39%) and other NH (38%) adults reported a clinical influenza diagnosis more often (P < .01 for both comparisons). Reporting an influenza diagnosis also varied by census region (P = .01) and ranged from 34% among adults in the West census region to 22% among adults in the Midwest census region.
Reported Influenza Antiviral Drug Receipt Among Adults
Of adults who sought health care and who recalled an influenza diagnosis, 36% reported receipt of an influenza antiviral drug (Table 1). Receipt of an influenza antiviral drug ranged from 42% during September interviews to 23% during March interviews, but this difference was not statistically significant (Figure 2).
Respondents aged 50 to 64 years (27%) and 65 years or older (22%) reported similar percentages of antiviral drug receipt, whereas respondents aged 18 to 49 years reported receiving antiviral drugs more often (39%; P < .01). Antiviral drug receipt did not vary significantly by gender, race/ethnicity, or census region.
DISCUSSION
During the pH1N1 influenza pandemic, the Centers for Disease Control and Prevention quickly implemented state-based surveillance to monitor influenza outcomes not captured by other surveillance systems. Results from this national surveillance indicate that ILI prevalence, health care–seeking practices, and receipt of an influenza diagnosis and influenza antiviral drug treatment varied significantly by respondents’ sex, age group, race/ethnicity, and geographic location.
The pH1N1 pandemic in the United States has been characterized since its beginning by a limited impact on older adults but a substantial impact on children and young adults.4 A telephone survey was used to monitor illness and health care–seeking behavior at the beginning of the pandemic in 10 states.11 Similar to results seen in this survey, the reported incidence of ILI was lowest in people aged 65 years or older and highest in people younger than 5 years. Additionally, overall trends and the percentage of respondents seeking health care for ILI were similar and ranged from 70% among children younger than 5 years to 45.9% among adult household members.11
Standard surveillance for influenza in the United States involves health care providers describing patient visits for ILI and submitting respiratory specimens for influenza diagnostic testing. The results from such health care–based surveillance conducted during the pH1N1 pandemic, including ILI visits to outpatient providers and the weekly number of positive influenza test results, indicate that activity peaked in late October 2009, which corresponds with the peak of ILI presented in this analysis.2,4 However, a majority of adults and almost half of children with ILI in this survey reported that they did not visit a health care provider for their illness and would not have been captured by health care–based influenza surveillance. Additionally, children, women, the oldest adult respondents, and adults in the Northeast and children in the South census regions were more likely to seek health care, suggesting that the epidemiology of ILI ascertained through routine influenza surveillance systems may differ substantially from that of cases identified using community surveillance. Understanding and accounting for the differential health care–seeking patterns identified in this report would allow for more accurate burden estimation and disease characterization when conducting health care–based surveillance for influenza.
Older respondents were less likely to report receipt of influenza antiviral drugs than were younger respondents. Although disproportionately more illness and infection with pH1N1 among young respondents was noted during the pandemic, severe outcomes occurred more often among older adults infected with pH1N1.1–4,12 An analysis of patients who were hospitalized with or died of pH1N1 virus in California found that people aged 50 years or older had the highest influenza mortality rate once hospitalized, and the presence of underlying chronic diseases in this population increased the mortality risk.13 Although recommendations published before the pH1N1 pandemic indicated that antiviral treatment be initiated within 48 hours of symptom onset for all people with suspected influenza virus infection who either were 65 years old or older or were at high risk for complications,14 few of the respondents in this age group received them. Continued exploration is needed to determine the nature of this gap in treatment among older adults and identify appropriate intervention strategies, which may include physician education or reducing barriers to health care access.
Self-reported ILI among AI/AN adults was 2 times higher than among all other racial/ethnic groups in the study. Moreover, AI/AN children reported substantially more ILI and sought health care much more often than other children in the study. Reasons for these differences among racial/ethnic groups are not clear and are being investigated, but higher incidence and more severe outcomes among AI/AN and other minorities have previously been reported for seasonal and pandemic influenza as well as other respiratory infections and may be related to a higher prevalence of chronic conditions or reduced access to quality health care.15–18 Findings from surveillance for invasive pneumococcal disease found incidences of the disease among NH Blacks to be 2 times higher, among Alaska Natives to be 4 times higher, and among White Mountain Apache Indians to be 8 times higher than among NH Whites.15 In a study examining health outcomes associated with respiratory syncytial virus, seasonal influenza virus, and parainfluenza viruses in the 2000–2001 season, higher hospitalization rates were identified among NH Black and Hispanic children than among NH White children for all 3 viruses.16 Elevated rates of hospitalization resulting from pH1N1 infection among minorities were also noted in a report from Chicago, Illinois, where enhanced surveillance methods found elevated hospitalization rates among NH Black, Asian/Pacific Islanders, and Hispanics.17 Elevated rates of hospitalization and death from pH1N1 among AI/ANs were found in a report from 12 states in which one half of the AI/AN population of the United States resides.18
This study is subject to at least 4 limitations. First, ILI data were self-reported or reported by parents for their children, and the accuracy of 1-month recall of illness is unclear. However, self-report of infectious illness, including respiratory illness, has shown high congruence with physician documentation in the medical record during patient interviews conducted as many as 3 months after a health care visit.19 Nonetheless, people with severe symptoms or those who sought care for their illness may have been more likely to remember and report an episode of ILI than were those with milder illness; therefore, the prevalence of ILI among those who did not seek medical care may have been underestimated. Second, because we did not include standard criteria to diagnose influenza or include a diagnostic testing component, reported ILI and recalling a clinical diagnosis of influenza cannot be interpreted to represent laboratory-confirmed influenza activity in the population. Illnesses meeting the ILI criteria can be caused by pathogens other than influenza (e.g., respiratory syncytial virus); conversely, influenza infections may cause illness that would not meet our ILI case definition. Studies have indicated that 12% to 31% of all respiratory illnesses occurring during periods when influenza viruses are known to be circulating are actually laboratory-confirmed influenza;20–22 this proportion has exceeded 50% during the peak of influenza transmission.22 Moreover, requiring fever as part of the case definition has been shown to increase the specificity of ILI for influenza illness.5–7
The ability of ILI to predict influenza illness can, however, vary substantially and is highest when influenza virus is circulating. Because this is the 1st year of the surveillance program and we did not have data from summer months when influenza activity is expected to be limited, we were unable to adjust for a background level of noninfluenza ILI in our estimates. Therefore, estimating the burden of pandemic influenza from these findings would be inappropriate because ILI prevalence may remain elevated even in the absence of influenza activity. However, because the peak in this report occurred at the same time as the peaks in other established health care–based influenza surveillance systems, the peak of ILI in this report likely reflects a peak in influenza activity during the surveillance period.2,4 Third, BRFSS data were collected only from households with a landline telephone. Selection bias related to exclusion of households with only cellular phones is possible, especially among younger adults, Hispanics, or residents of the South or Midwest census regions, who are more likely to be living in households with only cellular phones.23 Finally, only respondents from 39 states were included in the pediatric analysis, and 6 (54%) of the 11 missing sites were in the South census region. Therefore, results from the pediatric analysis may not be generalizable to the South census region or the entire United States.
Our study represents the only national information describing people with ILI who did not seek medical care during the 2009 pandemic. It also characterizes people who reported seeking care for ILI and who received an influenza diagnosis and antiviral treatment during their health care encounter. We found statistically significant differences among community-dwelling individuals in reported ILI, health care–seeking, and influenza diagnosis and antiviral drug treatment along geographic location and several demographic factors. Although ILI was found among all respondents during this period, reported ILI was 2 times higher among adults identified as AI/AN than among all other racial/ethnic groups. Treatment with influenza antiviral drugs was also common among adults who sought health care and who were clinically diagnosed with influenza. However, receipt of antiviral drugs was lowest among those aged 65 years or older, despite treatment recommendations during the pandemic that encouraged use of antiviral medications for all people aged 65 years or older with suspected influenza. The gaps in health care seeking and antiviral treatment identified in this report merit additional investigation, and the Centers for Disease Control and Prevention implemented a modified supplementary ILI module during the 2010–2011 influenza season, including a question to ascertain the duration between illness onset and first health care encounter, to further describe these inconsistencies. Continued analysis of ILI data from the BRFSS will help inform year-to-year influenza trends and better understand factors associated with self-reported ILI, health care seeking, and clinical influenza diagnosis and treatment using data that are not available in other surveillance systems.
Acknowledgments
All authors declare no conflicts of interest with the publication of this article.
Human Participant Protection
This investigation was determined to be part of the public health response to the pH1N1 pandemic and was not considered to be human subjects research in accordance with federal human subjects protection regulations. Thus, approval from an institutional review board was not required.
References
- 1.Shrestha SS, Swerdlow DL, Borse RHet al. Estimating the burden of 2009 pandemic influenza A (H1N1) in the United States (April 2009–January 2010). Clin Infect Dis. 2011;52(suppl 1):S75–S82 [DOI] [PubMed] [Google Scholar]
- 2.Brammer L, Blanton L, Epperson Set al. Surveillance for influenza during the 2009 Influenza A (H1N1) pandemic- United States, April 2009–March 2010. Clin Infect Dis. 2011;52(suppl 1):S27–S35 [DOI] [PubMed] [Google Scholar]
- 3.Reed C, Angulo F, Swerdlow Det al. Estimates of the prevalence of pandemic (H1N1) 2009, United States, April–July 2009. Emerg Infect Dis. 2009;15(12):2004–2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jhung MA, Swerdlow D, Olsen SJet al. Epidemiology of 2009 pandemic influenza A (H1N1) in the United States. Clin Infect Dis. 2011;52(suppl 1):S13–S26 [DOI] [PubMed] [Google Scholar]
- 5.Monto AS, Gravenstein S, Elliott M, Colopy M, Schweinle J. Clinical signs and symptoms predicting influenza infection. Arch Intern Med. 2000;160(21):3243–3247 [DOI] [PubMed] [Google Scholar]
- 6.Ong AK, Chen MI, Lin Let al. Improving the clinical diagnosis of influenza—a comparative analysis of new influenza A cases. PLoS ONE. 2009;4:e8453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Call SA, Vollenweider MA, Hornung CAet al. Does this patient have influenza? JAMA. 2005;293(8):987–997 [DOI] [PubMed] [Google Scholar]
- 8.Chowdhury P, Balluz L, Town M Centers for Disease Control and Prevention. Surveillance of certain health behaviors among states and selected local areas—Behavioral Risk Factor Surveillance System, United States. MMWR Surveill Summ. 2007;59(1):1–220. [PubMed]
- 9. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Operational and User's Guide. Available at: ftp://ftp.cdc.gov/pub/Data/Brfss/userguide.pdf. Accessed August 5, 2010.
- 10.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2010 Stat Notes. 2001;20:1–10 [PubMed] [Google Scholar]
- 11.Reed C, Angulo F, Biggerstaff M, Swerdlow D, Finelli L. Influenza-like illness in the community during the emergence of 2009 pandemic influenza A (H1N1)—Survey of 10 states, April 2009. Clin Infect Dis. 2011;52(suppl 1):S90–S93 [DOI] [PubMed] [Google Scholar]
- 12.Miller E, Hoschler K, Hardelid P, Stanford E, Andrews N, Zambon M. Incidence of 2009 pandemic influenza A H1N1 infection in England: a cross-sectional serological study. Lancet. 2010;375(9720):1100–1108 [DOI] [PubMed] [Google Scholar]
- 13.Louie JK, Acosta M, Winter Ket al. Factors associated with death or hospitalization due to pandemic 2009 influenza A (H1N1) infection in California. JAMA. 2009;302(17):1896–1902 [DOI] [PubMed] [Google Scholar]
- 14.Harper SA, Bradley JS, Englund JAet al. Seasonal influenza in adults and children—diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: clinical practice guidelines of the Infectious Disease Society of America. Clin Infect Dis. 2009;48(8):1003–1032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Brien KL, Santosham M. Potential impact of conjugate pneumococcal vaccines on pediatric pneumococcal diseases. Am J Epidemiol. 2004;159(7):634–644 [DOI] [PubMed] [Google Scholar]
- 16.Iwane MK, Edwards KM, Szilagyi PGet al. Population-based surveillance for hospitalizations associated with respiratory syncytial virus, influenza virus, and parainfluenza viruses among young children. Pediatrics. 2004;113(6):1758–1764 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention 2009 pandemic influenza A (H1N1) virus infections—Chicago, Illinois, April–July 2009. MMWR Morb Mortal Wkly Rep. 2009;58(33):913–918 [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention Deaths related to 2009 pandemic influenza A (H1N1) among American Indian/Alaska Natives—12 states, 2009. MMWR Morb Mortal Wkly Rep. 2009;58(48):1341–1344 [PubMed] [Google Scholar]
- 19.Orts K, Sheridan JF, Robinson-Whelen S, Glaser R, Malarkey WB, Kiecolt-Glaser JK. The reliability and validity of a structured interview for the assessment of infectious illness symptoms. J Behav Med. 1995;18(6):517–529 [DOI] [PubMed] [Google Scholar]
- 20.Monto AS, Ullman BM. Acute respiratory illness in an American community. JAMA. 1974;227(2):164–169 [PubMed] [Google Scholar]
- 21.Bridges CB, Thompson WW, Meltzer MIet al. Effectiveness and cost-benefit of influenza vaccination of healthy working adults: a randomized controlled trial. JAMA. 2000;284(13):1655–1663 [DOI] [PubMed] [Google Scholar]
- 22.Ren L, Gonzalez R, Wang Zet al. Prevalence of human respiratory viruses in adults with acute respiratory tract infections in Beijing, 2005–2007. Clin Microbiol Infect. 2009;15(12):1146–1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blumberg SJ, Luke JV. Wireless substitution: early release of estimates from the National Health Interview Survey, January–June 2009. Available at: http://www.cdc.gov/nchs/data/nhis/earlyrelease/wireless200912.pdf. Accessed December 28, 2010.