Abstract
Background
Multimorbidity is increasingly recognized as a major public health challenge of modern societies. However, knowledge about the size of the population suffering from multimorbidity and the type of multimorbidity is scarce. The objective of this study was to present an overview of the prevalence of multimorbidity and comorbidity of chronic diseases in the Dutch population and to explore disease clustering and common comorbidities.
Methods
We used 7 years data (2002–2008) of a large Dutch representative network of general practices (212,902 patients). Multimorbidity was defined as having two or more out of 29 chronic diseases. The prevalence of multimorbidity was calculated for the total population and by sex and age group. For 10 prevalent diseases among patients of 55 years and older (N = 52,014) logistic regressions analyses were used to study disease clustering and descriptive analyses to explore common comorbid diseases.
Results
Multimorbidity of chronic diseases was found among 13% of the Dutch population and in 37% of those older than 55 years. Among patients over 55 years with a specific chronic disease more than two-thirds also had one or more other chronic diseases. Most disease pairs occurred more frequently than would be expected if diseases had been independent. Comorbidity was not limited to specific combinations of diseases; about 70% of those with a disease had one or more extra chronic diseases recorded which were not included in the top five of most common diseases.
Conclusion
Multimorbidity is common at all ages though increasing with age, with over two-thirds of those with chronic diseases and aged 55 years and older being recorded with multimorbidity. Comorbidity encompassed many different combinations of chronic diseases. Given the ageing population, multimorbidity and its consequences should be taken into account in the organization of care in order to avoid fragmented care, in medical research and healthcare policy.
Keywords: Multimorbidity, Comorbidity, Chronic disease, Epidemiology, Prevalence
Background
The presence of multiple coexistent chronic diseases is increasingly recognized as a major public health challenge of modern societies [1,2]. Challenges include optimalization of individuals’ health despite multimorbidity and the organisation and provision of health care for multimorbid patients. A first step in meeting these challenges is to provide insight into the size of the population suffering from multimorbidity, and the type of multimorbidity. Several studies on these figures are now available, showing high prevalences of multimorbidity [3-7]. Until now however, the distribution and combination of specific diseases received very little attention [8]. Health care needs of patients with multiple chronic conditions not only depend on the number but also, and maybe even more so, on the type of co-occurring diseases. With the ageing population and the accompanying rise in multimorbidity, the burden of chronically ill on health service capacity and costs is high [9] and is expected to rise in the future. Insight into combinations of diseases which often co-occur may assist in planning and improving (the organization of) health care services.
In this paper we analyze the prevalence of multimorbidity of chronic diseases by age and sex and the clustering of chronic diseases on the basis of electronic medical records in a representative sample of Dutch general practices. For a selection of 10 specific diseases we also present a detailed picture of the comorbidity, i.e. the type and prevalence of additional diseases among that specific disease.
Methods
Study design & participants
We used a longitudinal dataset of electronic medical records of over 350,000 patients in a representative sample of 92 general practices that participate in the Netherlands Information Network of General Practice (LINH), covering circa 2% of the total Dutch population [10]. General practices within this network are evenly distributed across the Netherlands. The listed population and the general practices are representative for the Dutch population and the Dutch general practitioners, respectively. In the Netherlands, all individuals are obligatory listed in a general practice, with exception of a small, very old part of the Dutch population in nursing homes. Therefore, the listed population can be used as the denominator in population based epidemiological studies. The prevalence of multimorbidity was analysed using LINH data from 2002 to 2008. LINH is registered with the Dutch Data Protection Authority; data are handled according to the data protection guidelines of the authority. According to Dutch legislation, studies using this kind of observational data do not require medical ethical approval.
Dataset
LINH includes routinely recorded data on consultations, including drug prescriptions and referrals. Diagnostic codes were recorded with consultations, drug prescriptions, and referrals, according to the International Classification of Primary Care (ICPC) [11]. Episodes of care were constructed and included all patients contacts and drug prescriptions pertaining to a specific health problem [12]. Thus two consultations for the same health problem are grouped into one episode of care. Consider, for instance, a patient who visits the general practitioner with a chronic cough, and a few months later the same patient is diagnosed with COPD. Most likely, both diagnoses refer to the same health problem and to avoid double counting the two diagnoses were grouped into one episode of care named COPD. Another example is a patient with symptoms of breathlessness and a diagnosis of heart failure a few weeks later, these health problems were grouped into one episode of heart failure. These episodes were constructed by EPICON, an algorithm to group ICPC-coded contact records from electronic medical records in general practice into episodes of care [13,14].
For prevalence calculations the data from general practices should meet standards for completeness, i.e. for each general practice the percentage of valid ICPC codes should be 60% or more and the registration of morbidity and prescriptions must have occurred continuously over each year [10].
Multimorbidity and comobidity
Multimorbidity is defined as the co-occurrence of two or more chronic diseases within one person in a specific period of time [15]. Comorbidity refers to the presence of at least one extra chronic disease along with a chronic disease of interest [16]. Chronic diseases are defined as irreversible conditions without complete recovery or relatively long-lasting conditions. Diseases were selected based on high prevalence and a chronic and severe character from a standard list of chronic conditions for primary care [17]. This resulted in 29 chronic diseases, presented with ICPC codes in Table1[17]. Comorbidity was explored for 10 chronic diseases which are prevalent among older patients: diabetes mellitus, coronary heart disease, osteoarthritis, chronic obstructive pulmonary disease (COPD), chronic neck- or back disorders, cancer, stroke, depression, heart failure, and anxiety disorders.
Table 1.
Selection of 29 chronic diseases with ICPC-1 codes
| Chronic disease | ICPC-1 code |
|---|---|
| Tuberculosis |
A70 |
| HIV/AIDS |
B90 |
| Cancer |
A79, B72, B73, D74, D75, D77, L71, N74, R84, R85, S77, T71, U75, U76, U77, W72, X75, X76, X77, Y77, Y78 |
| Gastric or duodenal ulcer |
D85, D86 |
| Chronic enteritis/colitis ulcerosa |
D94 |
| Visual disorder |
F83, F84, F92, F93, F94 |
| Hearing disorder |
H84, H85 |
| Congenital cardiovascular anomaly |
K73 |
| Coronary heart disease |
K74, K75, K76 |
| Heart failure |
K77 |
| Stroke (including TIA) |
K89, K90 |
| Chronic back or neck disorder |
L83, L84, L85, L86 |
| Rheumatoid arthritis |
L88 |
| Osteoarthritis |
L89, L90, L91 |
| Osteoporosis |
L95 |
| Congenital neurological anomaly |
N85 |
| Multiple sclerosis |
N86 |
| Parkinson’s disease |
N87 |
| Epilepsy |
N88 |
| Chronic alcohol abuse |
P15 |
| Dementia |
P70 |
| Schizophrenia |
P72 |
| Anxiety disorder, neurosis, PTSS |
P74, P79 |
| Depressive disorder |
P76 |
| Mental retardation |
P85 |
| Chronic obstructive pulmonary disease |
R91, R95 |
| Asthma |
R96 |
| Anorexia |
T06 |
| Diabetes mellitus | T90 |
The selection of chronic diseases is based on ‘Defining chronic conditions for primary care using ICPC-2: supplementary data'.[17] ICPC-2 codes are encoded into ICPC-1 codes.
Prevalence
Given that diagnoses are recorded based on patient contacts, the prevalence of some chronic diseases is underestimated when medical records from one year are used. In general, patients with diabetes or COPD visit their general practitioner frequently throughout a year but patients with osteoarthritis or asthma for example visit their general practitioner infrequently, sometimes even less than once a year. Therefore, only patients registered for a minimum period of 3 consecutive years in a general practice within the LINH network were selected.
Analyses
The selection of patients registered for a minimum period of 3 consecutive years resulted in a study population of 212,902 patients registered with 59 general practices.
Sex and age standardization was applied in all prevalence estimates to account for differences with the Dutch population in 2008 (http://statline.cbs.nl). The prevalence of chronic diseases and multimorbidity was defined as the number of patients with one or more diseases divided by the total number of 212,902 registered patients. In addition, prevalence estimates were stratified according to sex and age groups. To determine prevalence estimates it was assumed that a chronic disease, once recorded, remains prevalent during all follow-up years in the registration (recovery is not possible).
Analyses for clustering and comorbidity were restricted to 52,014 patients of 55 years and older. If diseases are completely independent of one another, they can be expected to co-occur at a rate which equals the product of the prevalence rates of the separate diseases [5]. For some pairs of diseases, the rate of co-occurrence may be higher than expected, which is referred to as disease clustering [18]. Clustering of chronic diseases is determined by the ratio of the observed prevalence rate and the expected prevalence rate of the pair of diseases. Logistic regression analyses adjusted for sex and age were used to investigate disease clustering.
For each of the 10 chronic diseases the proportion patients without comorbidity and those with 1, 2, 3, and 4 or more comorbid diseases was calculated. Finally, the five most prevalent comorbid chronic diseases (from 28 other diseases) were determined for the 10 specific diseases.
All analyses were performed in SAS version 9.2 (SAS Institute, Cary, North Carolina, USA).
Results
One-third of all registered patients had at least one chronic disease out of 29 chronic diseases (all ages) and about 13% had multimorbidity (Table2). The prevalence rate of chronic diseases and multimorbidity is higher for women and higher age groups. Of patients of 75 years and older 84% had a chronic disease and 59% had more than one chronic disease. In total, 37% of all patients of 55 years and older was known with multimorbidity.
Table 2.
Prevalence rates of patients with chronic diseases and patients with multimorbidity according to sex and age, LINH 2002-2008
| N | Prevalence rate of patients with chronic diseases (%)* | Prevalence rate of multimorbid patients (%)* | |
|---|---|---|---|
| Total |
212,902 |
33.7% |
12.9% |
| Men |
105,547 |
30.7% |
10.9% |
| Women |
107,355 |
36.6% |
15.0% |
| 0-14 years |
38,944 |
12.6% |
0.6% |
| 15-24 years |
26,718 |
15.2% |
2.0% |
| 25-54 years |
95,226 |
30.0% |
8.1% |
| 55-64 years |
22,592 |
52.9% |
22.7% |
| 65-74 years |
17,465 |
70.0% |
39.1% |
| 74+ years | 11,957 | 83.5% | 59.2% |
* According to the selection of 29 chronic diseases in Table1.
The prevalence estimates for pairs of chronic diseases in the population of 55 years and older are presented in Table3. The prevalence of co-occuring diabetes and coronary heart disease was 3.6% for example, and COPD and osteoarthritis co-occur in 1.7% of the patients. Most odds ratios are significantly higher than 1.0, indicating that almost all pairs of chronic diseases co-occur more frequently than expected on basis of statistical independency of diseases. The highest odds ratios were found for the disease pairs depression and anxiety disorder, coronary heart disease and heart failure, and COPD and heart failure.
Table 3.
Prevalence (P) co-occuring chronic diseases (%)1and the sex and age adjusted odds ratio (OR) for clustering for patients of 55 years and older2, LINH 2002–2008
| |
Coronary heart disease |
Osteoarthritis |
COPD |
Chronic neck or back disorder |
Cancer |
Stroke |
Depression |
Heart failure |
Anxiety disorder |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P | OR | P | OR | P | OR | P | OR | P | OR | P | OR | P | OR | P | OR | P | OR | |
| Diabetes mellitus |
3.6 |
1.9*3 |
2.8 |
1.1* |
2.1 |
1.3* |
2.5 |
1.3* |
1.9 |
1.1 |
1.9 |
1.6* |
1.4 |
1.2* |
2.2 |
1.7* |
0.5 |
1.1 |
| Coronary heart disease |
|
|
2.5 |
1.3* |
2.2 |
1.6* |
2.3 |
1.6* |
1.8 |
1.2* |
1.5 |
1.3* |
1.3 |
1.5* |
2.8 |
3.7* |
0.4 |
1.5* |
| Osteoarthritis |
|
|
|
|
1.7 |
1.2* |
2.8 |
2.0* |
1.7 |
1.1* |
1.2 |
1.0* |
1.4 |
1.4* |
1.6 |
1.3* |
0.4 |
1.1 |
| COPD |
|
|
|
|
|
|
1.5 |
1.4* |
1.4 |
1.3* |
1.0 |
1.3* |
1.0 |
1.7* |
1.9 |
3.4* |
0.4 |
1.7* |
| Chronic neck or back disorder |
|
|
|
|
|
|
|
|
1.4 |
1.2* |
1.0 |
1.3* |
1.2 |
1.5* |
0.9 |
1.2* |
0.5 |
1.4* |
| Cancer |
|
|
|
|
|
|
|
|
|
|
0.9 |
1.0 |
0.9 |
1.4* |
1.2 |
1.3* |
0.3 |
1.4* |
| Stroke |
|
|
|
|
|
|
|
|
|
|
|
|
0.8 |
1.6* |
1.2 |
1.5* |
0.2 |
1.3* |
| Depression |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
0.7 |
1.5* |
0.8 |
5.9* |
| Heart failure | 0.2 | 1.5* | ||||||||||||||||
1Prevalence estimates are standardized according to the age and sex distribution in the Dutch population in 2008.
2 The odds ratio represents the ‘probability’ for co-occurrence of 2 chronic diseases. Two chronic diseases co-occur more frequent than would be expected on basis of independency if the odds ratio is larger than 1.0 and the 95% confidence interval does not include 1.0.
3 The prevalence of comorbidity of diabetes mellitus and coronary heart disease is 3.6%. Diabetes mellitus and coronary heart disease co-occur significantly more frequent than expected on basis of independency, with an odds ratio of 1.9.
* Co-occurrence of diseases occurred more frequent than expected on basis of independency (p < 0.05).
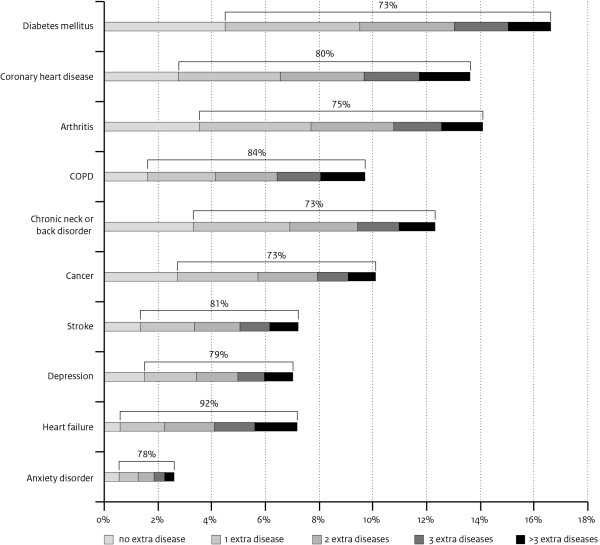
Over 70% of those with one of the selected 10 chronic diseases had also one or more other chronic diseases (comorbidity). The highest proportion of comorbidity is shown for heart failure, of all patients with heart failure 92% had at least one extra chronic disease (Figure1). About a quarter of the patients with heart failure had one extra disease, 23% two extra diseases, 21% three extra diseases, and 22% had four or more extra chronic diseases.
Figure 1.
Prevalence of 10 chronic diseases and comorbidity (%) among patients of 55 years and older.
Diabetes mellitus, osteoarthritis, and coronary heart disease were the most prevalent co-occuring diseases for all 10 diseases (Table4). From all patients with cancer and one or more extra diseases, 26% was recorded with diabetes mellitus, 24% with coronary heart disease, 23% with osteoarthritis, 19% with chronic neck- or back disorders, and 18% with COPD. One-third of those with cancer and comorbidity had only diseases included in the top-5 comorbid diseases for cancer, the other patients (two-thirds) had at least one disease that was not included in the top-5 comorbid diseases for cancer. Similar numbers were shown for the 9 other specific diseases (Table4): about 30% of the patients with comorbidity had only diseases included in the top-5 whereas 70% had one or more diseases not included in the top-5.
Table 4.
Top 5 of most prevalent comorbidity for 10 chronic diseases (first column) and prevalence of co-occuring diseases among all patients of 55 years and older with the specific chronic disease and comorbidity
|
Chronic disease |
Comorbidity top 5 and prevalence |
Contribution of top 5 to all comorbidity with the specific chronic disease* |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |||||||
|
Diabetes mellitus |
Coronary heart disease |
30.0% |
Osteoarthritis |
22.7% |
Chronic neck or back disorder |
20.3% |
Heart failure |
18.1% |
COPD |
17.2% |
31.5% |
|
Coronary heart disease |
Diabetes mellitus |
33.5% |
Heart failure |
25.5% |
Osteoarthritis |
23.0% |
Chronic neck or back disorder |
20.8% |
Cancer |
16.7% |
32.8% |
|
Osteoarthritis |
Chronic neck or back disorder |
26.8% |
Diabetes mellitus |
26.0% |
Coronary heart disease |
23.6% |
Visual disorder |
16.4% |
Cancer |
16.0% |
33.5% |
|
COPD |
Asthma |
32.4% |
Coronary heart disease |
27.4% |
Diabetes mellitus |
25.8% |
Heart failure |
24.0% |
Osteoarthritis |
20.5% |
29.9% |
|
Chronic neck or back disorder |
Osteoarthritis |
31.5% |
Diabetes mellitus |
27.3% |
Coronary heart disease |
25.2% |
COPD |
17.0% |
Cancer |
15.5% |
35.8% |
|
Cancer |
Diabetes mellitus |
25.6% |
Coronary heart disease |
24.4% |
Osteoarthritis |
22.8% |
Chronic neck or back disorder |
18.8% |
COPD |
18.3% |
33.1% |
|
Stroke |
Diabetes mellitus |
32.4% |
Coronary heart disease |
26.0% |
Osteoarthritis |
21.0% |
Heart failure |
20.2% |
COPD |
17.5% |
27.8% |
|
Depression |
Osteoarthritis |
24.7% |
Diabetes mellitus |
24.6% |
Coronary heart disease |
22.8% |
Chronic neck or back disorder |
22.3% |
COPD |
18.0% |
26.4% |
|
Heart failure |
Coronary heart disease |
42.0% |
Diabetes mellitus |
33.3% |
COPD |
29.4% |
Osteoarthritis |
24.5% |
Stroke |
18.0% |
30.4% |
| Anxiety disorder | Depression | 38.0% | Diabetes mellitus | 22.3% | Chronic neck or back disorder | 22.2% | Coronary heart disease | 20.7% | Osteoarthritis | 19.8% | 31.4% |
1 Prevalence is determined by dividing the number of patients with a specific combination of co-occuring diseases through the number of patients with the specific chronic disease and 1 or more other chronic diseases. Prevalence estimates are standardized according to the sex and age distribution in the Dutch population in 2008.
* According to the selection of 29 chronic diseases in Table1.
Discussion
Our analyses show that multimorbidity is common, especially among older persons, and that among those with a chronic disease over two thirds has other comorbidities. A more detailed look at the combinations of diseases showed a wide variety in multimorbidity. We observed that all chronic diseases tend to cluster, i.e. most disease pairs co-occur more often than expected by chance. Furthermore, the top-5 of co-occurring chronic diseases represents only a minor proportion of the comorbidity: all diseases co-occur together. These findings may have important consequences since the organization and funding of health care is organized by disease-specific programs in many countries. Such disease-specific approaches do not match the reality of most people with a chronic disease.
Strengths and weaknesses of the study
Primary care registries represent an interesting source to describe multimorbidity of chronic diseases because often most health problems are known and recorded by the general practitioner, especially in countries as the Netherlands where general practice is the entry point for health care and general practitioners act as gatekeeper for secondary care. Analyzing multimorbidity among general practice patients can be used for different research questions [3,4,19,20] but ideally we need to know the underlying population or epidemiological denominator. Strength of general practice registries in the Netherlands is that almost everybody is registered within a general practice. Hence, it is possible to use morbidity data from the general practice registries to describe morbidity of the general population.
In addition, use of long-term registration data of a country-wide network of general practices for the analyses on multimorbidity has several advantages, like the distribution of the general practices over the Netherlands, the relatively long registration period, and the standardized registration procedures. A general strength of general practice medical records compared to self-reported data is the availability of diagnosed chronic diseases. A disadvantage is that diseases for which patients do not consult a general practitioner are not in the general practitioners’ medical record system. In addition, the small group of elderly in nursing homes, usually having more than one chronic disease, are generally not registered within a general practice. Owing to these exclusions the prevalence of chronic diseases in the general population may be underestimated based on general practice registrations. Underdiagnosis and underreporting of health problems like depression may also lead to underestimation of the prevalence of multimorbidity.
Length of follow-up in a registration affects the extent and the reliability of multimorbidity estimates [21]. The frequency of general practitioner consultations for some diseases, such as osteoarthritis, are even less than once a year. The prevalence of those diseases is underestimated in a registration with a one-year follow-up, therefore the minimum patient follow-up in our study was three years. With a longer follow-up period selection may play a role since patients move away and general practices drop out from the registration.
Apparently, the prevalence of multimorbidity in this study is completely determined by the selection of 29 chronic diseases. Generally speaking, the more chronic conditions are included the higher prevalence rates of multimorbidity will be found. We presume that an important part of chronic morbidity is included in our selection of diseases. By counting the number of chronic diseases we did not take into account any differences in the severity of diseases [22]. When interpreting the results of our and similar studies that are based on general practice registrations, it should be noticed that the varying consequences of diseases on patients’ physical and mental functioning, disability and independency are not considered [8,23].
Comparison with literature
Registry characteristics affect the prevalence and nature of multimorbidity, especially the selection and definition of diseases affect the actual prevalence rates [21,24]. This limits comparisons with other studies, even those based on general practice registries. However, the general patterns we found are similar to those of other studies. First, multimorbidity being rather the rule than the exception and prevalences increasing with age but also found at younger age [3-8,25-27]. Second, clustering of diseases is commonly found in all recent studies on multimorbidity of (chronic) diseases [5,28-32]. Third, the most prevalent diseases like heart disease, diabetes and osteoarthritis end up high in every multimorbidity rank [4,29]. Most studies showed hypertension, obesity and hyperlipidemia to rank high in prevalence when it was defined as a chronic disease [21,28,29]. To our opinion these are chronic conditions that increase the risk on chronic disease but are not diseases, we therefore did not include these in our analyses. Fourth, a majority of persons with one chronic disease also have at least one (and often more) other disease and these are not limited to a few common diseases, these can be any disease [6,28,29]. While a descriptive approach was used in our analyses and others [6,29] few other studies performed cluster analyses to identify comorbidity patterns [28,30-32]. These studies identified 3 to 6 clusters of diseases and most revealed a cluster with vascular conditions and a cluster with mental diseases along with pain [28,30,32]. We focused on common co-occuring conditions and our findings indicate a wide variety of co-occuring conditions since only 30% of the comorbidity spectrum can be attributed to the 5 most common comorbidities. In line with this, van den Bussche described that combinations of the six most prevalent chronic conditions span only 42% of the comorbidity spectrum [29].
Implications of the study
A substantial proportion of the older population being characterized by multimorbidity of chronic diseases requires reconsiderations of medical research as well as the organization of care. Most research and clinical practice are based on a single disease paradigm, which may not be appropriate for patients with multiple complex health problems [33,34]. Studies investigating the (cost-)effectiveness of new treatments commonly exclude patients with multimorbidity. Findings from these studies have a very limited reach since multimorbidity affects the majority of the aged. There is thus a clear need to shift research from disease-specific treatments and patients with single diseases to research which takes into account multimorbidity or is explicitly focused on patients with multimorbidity [35].
Multimorbidity leads to complex care through the use of different treatment strategies and the involvement of various health care professionals, which may lead to opposing advices (counseling) or medications [36]. Due to fragmented expertise and focus by different care providers, patients preferences, expectancies, values and needs regarding their daily life are often overlooked [37]. Patients’ main priorities are usually an adequate quality of life and appropriate daily functioning in addition to the improvement of disease-specific health problems.
Currently, disease management programs are implemented worldwide in order to enhance quality and continuity of care for the chronically ill [38,39]. These programs are characterized by a patient-centered approach of coordinated multiple healthcare interventions that structure chronic care to a specific patient group [39,40]. However, participating in multiple single-disease oriented programs in combination with regular primary care, may lead to fragmented care. In designing these programs insufficient attention is paid to multimorbid conditions. Multimorbid patients are therefore at risk for suboptimal treatment, unsafe care, inefficient use of health care services, unnecessary costs and consequently run higher risks for adverse events [41]. Case management is a potential model which might counteract fragmented care for multimorbid patients. It is an individualized care program which coordinates all care involved for patients enrolled in different single-disease management programs, who have to adhere to various treatment protocols. It draws on evidence-based optimal care for systematically managing all existing conditions in a patient, and is tailored to the individual patients’ preferences [42-44].
The finding that multimorbidity cannot be captured with a few common combinations of diseases represents a challenge for disease-specific treatment as well as disease-specific disease management programs and rises the question for which patient group case management should be implemented. Given the enormous variety in multimorbidity, we need more knowledge about the co-occurring conditions that are leading to a high need for care, a major decline in quality of life, and/or an increase in functional limitations.
Conclusion
Multimorbidity is common at all ages and cannot be captured by a few common combinations of diseases.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SO, HP, LL, BG, NH, and CB participated in the conceptual development, study design and the interpretation of the results. SO and HP drafted the manuscript and SO analysed the data. LL, BG, NH, CD, RV, FG, and CB revised the manuscript. RV, FG and CD participated in data collection. All authors read and approved the final manuscript.
The submitted manuscript is an adapted and extended version of a Dutch paper
van Oostrom SH, Picavet HS, van Gelder BM, Lemmens LC, Hoeymans N, Verheij RA, Schellevis FG, Baan CA: Multimorbiditeit en comorbiditeit in de Nederlandse bevolking – gegevens van huisartsenpraktijken [Multimorbidity and comorbidity in the Dutch population - data from general practices]. Ned Tijdschr Geneeskd 2011, 155:A3193.
Author details
Author details1Centre for Prevention and Health Services Research, National Institute for Public Health and the Environment, P.O. Box 1, Bilthoven 3720 BA, the Netherlands. 2Centre for Public Health Forecasting, National Institute for Public Health and the Environment, P.O. Box 1, Bilthoven 3720 BA, the Netherlands. 3Department of General Practice, Netherlands Institute for Health Services Research, P.O. Box 1568, Utrecht 3500 BN, the Netherlands.4Department of General Practice/EMGO Institute, VU University Medical Centre, Amsterdam, the Netherlands.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Sandra H van Oostrom, Email: Sandra.van.oostrom@rivm.nl.
H Susan J Picavet, Email: susan.picavet@rivm.nl.
Boukje M van Gelder, Email: boukje.van.gelder@rivm.nl.
Lidwien C Lemmens, Email: lidwien.lemmens@rivm.nl.
Nancy Hoeymans, Email: nancy.hoeymans@rivm.nl.
Christel E van Dijk, Email: c.vandijk@nivel.nl.
Robert A Verheij, Email: r.verheij@nivel.nl.
François G Schellevis, Email: F.Schellevis@nivel.nl.
Caroline A Baan, Email: caroline.baan@rivm.nl.
References
- Fortin M, Soubhi H, Hudon C, Bayliss EA, van den Akker M. Multimorbidity's many challenges. BMJ. 2007;334(7602):1016–1017. doi: 10.1136/bmj.39201.463819.2C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercer SW, Smith SM, Wyke S, O'Dowd T, Watt GC. Multimorbidity in primary care: developing the research agenda. Fam Pract. 2009;26(2):79–80. doi: 10.1093/fampra/cmp020. [DOI] [PubMed] [Google Scholar]
- Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2005;3(3):223–228. doi: 10.1370/afm.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laux G, Kuehlein T, Rosemann T, Szecsenyi J. Co- and multimorbidity patterns in primary care based on episodes of care: results from the German CONTENT project. BMC Health Serv Res. 2008;8:14. doi: 10.1186/1472-6963-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol. 1998;51(5):367–375. doi: 10.1016/S0895-4356(97)00306-5. [DOI] [PubMed] [Google Scholar]
- Britt HC, Harrison CM, Miller GC, Knox SA. Prevalence and patterns of multimorbidity in Australia. Med J Aust. 2008;189(2):72–77. doi: 10.5694/j.1326-5377.2008.tb01919.x. [DOI] [PubMed] [Google Scholar]
- Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. 2008;14:28–32. doi: 10.1080/13814780802436093. [DOI] [PubMed] [Google Scholar]
- Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, Meinow B, Fratiglioni L. Aging with multimorbidity: A systematic review of the literature. Ageing Res Rev. 2011;10(4):430–439. doi: 10.1016/j.arr.2011.03.003. [DOI] [PubMed] [Google Scholar]
- Lehnert T, Heider D, Leicht H, Heinrich S, Corrieri S, Luppa M, Riedel-Heller S, Konig HH. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68(4):387–420. doi: 10.1177/1077558711399580. [DOI] [PubMed] [Google Scholar]
- Verheij RA, van Dijk CE, Abrahamse H, Davids R, van den Hoogen H, Braspenning J, van Althuis T. Landelijk Informatienetwerk Huisartsenzorg. Feiten en cijfers over huisartsenzorg in Nederland. (Netherlands Information Network of General Practice: facts and figures of general practice in the Netherlands) NIVEL/WOK, Utrecht/Nijmegen; 2009. [Google Scholar]
- Lamberts H, Wood M. The birth of the International Classification of Primary Care (ICPC). Serendipity at the border of Lac Leman. Fam Pract. 2002;19(5):433–435. doi: 10.1093/fampra/19.5.433. [DOI] [PubMed] [Google Scholar]
- An international glossary for general/family practice. WONCA Classification Committee. Fam Pract. 1995;12(3):341–369. doi: 10.1093/fampra/12.3.341. [DOI] [PubMed] [Google Scholar]
- Biermans MC, de Bakker DH, Verheij RA, Gravestein JV, van der Linden MW, de Vries Robbe PF. Development of a case-based system for grouping diagnoses in general practice. Int J Med Inform. 2008;77(7):431–439. doi: 10.1016/j.ijmedinf.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Biermans MC, Verheij RA, de Bakker DH, Zielhuis GA, de Vries Robbe PF. Estimating morbidity rates from electronic medical records in general practice. Evaluation of a grouping system. Methods Inf Med. 2008;47(2):98–106. [PubMed] [Google Scholar]
- van den Akker M, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity: what's in a name? A review of literature . Eur J Gen Pract. 1996;2(2):65–70. doi: 10.3109/13814789609162146. [DOI] [Google Scholar]
- Feinstein AR. The pre-therapeutic classification of co-morbidity in chronic disease. J Chron Dis. 1970;23:455–468. doi: 10.1016/0021-9681(70)90054-8. [DOI] [PubMed] [Google Scholar]
- The Family Medicine Research Centre. Defining chronic conditions for primary care using ICPC-2: supplementary data. University of Sydney, Sydney; 2004. http://www.fmrc.org.au/Download/DefiningChronicConditions.pdf. [Google Scholar]
- Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, van den Bos GA. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54(7):661–674. doi: 10.1016/S0895-4356(00)00363-2. [DOI] [PubMed] [Google Scholar]
- Fortin M, Bravo G, Hudon C, Lapointe L, Dubois MF, Almirall J. Psychological distress and multimorbidity in primary care. Ann Fam Med. 2006;4(5):417–422. doi: 10.1370/afm.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadam UT, Croft PR. Clinical multimorbidity and physical function in older adults: a record and health status linkage study in general practice. Fam Pract. 2007;24(5):412–419. doi: 10.1093/fampra/cmm049. [DOI] [PubMed] [Google Scholar]
- Schram MT, Frijters D, van de Lisdonk EH, Ploemacher J, de Craen AJ, de Waal MW, van Rooij FJ, Heeringa J, Hofman A, Deeg DJ. et al. Setting and registry characteristics affect the prevalence and nature of multimorbidity in the elderly. J Clin Epidemiol. 2008;61(11):1104–1112. doi: 10.1016/j.jclinepi.2007.11.021. [DOI] [PubMed] [Google Scholar]
- Huntley AL, Johnson R, Purdy S, Valderas JM, Salisbury C. Measures of multimorbidity and morbidity burden for use in primary care and community settings: a systematic review and guide. Ann Fam Med. 2012;10(2):134–141. doi: 10.1370/afm.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CM, Fortin M. Future of multimorbidity research: how should understanding of multimorbidity inform health system design? Public Health Reviews. 2010;32(2):451–474. [Google Scholar]
- Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012;10(2):142–151. doi: 10.1370/afm.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162(20):2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- Salisbury C, Johnson L, Purdy S, Valderas JM, Montgomery AA. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011;61(582):e12–e21. doi: 10.3399/bjgp11X548929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, Murphy AW. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011;28(5):516–523. doi: 10.1093/fampra/cmr013. [DOI] [PubMed] [Google Scholar]
- Marengoni A, Rizzuto D, Wang HX, Winblad B, Fratiglioni L. Patterns of chronic multimorbidity in the elderly population. J Am Geriatr Soc. 2009;57(2):225–230. doi: 10.1111/j.1532-5415.2008.02109.x. [DOI] [PubMed] [Google Scholar]
- van den Bussche H, Koller D, Kolonko T, Hansen H, Wegscheider K, Glaeske G, von Leitner EC, Schafer I, Schon G. Which chronic diseases and disease combinations are specific to multimorbidity in the elderly? Results of a claims data based cross-sectional study in Germany. . BMC Publ Health. 2011;11:101. doi: 10.1186/1471-2458-11-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornell JE, Pugh JA, Williams JW, Kazis L, Lee AFS, Parchman ML, Zeber J, Pederson T, Montgomery KA, Hitchcock P. Multimorbidity clusters: clustering binary data from multimorbidity clusters: clustering binary data from a large administrative medical database. Applied Multivariate Research. 2007;12(3):163–182. [Google Scholar]
- Garcia-Olmos L, Salvador CH, Alberquilla A, Lora D, Carmona M, Garcia-Sagredo P, Pascual M, Munoz A, Monteagudo JL, Garcia-Lopez F. Comorbidity patterns in patients with chronic diseases in general practice. PLoS One. 2012;7(2):e32141. doi: 10.1371/journal.pone.0032141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer I, Hansen H, Schon G, Maier W, Hofels S, Altiner A, Fuchs A, Gerlach FM, Petersen JJ, Gensichen J. et al. The German MultiCare-study: Patterns of multimorbidity in primary health care - protocol of a prospective cohort study. BMC Health Serv Res. 2009;9:145. doi: 10.1186/1472-6963-9-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortin M, Contant E, Savard C, Hudon C, Poitras ME, Almirall J. Canadian guidelines for clinical practice: an analysis of their quality and relevance to the care of adults with comorbidity. BMC Fam Pract. 2011;12(1):74. doi: 10.1186/1471-2296-12-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Weel C, Schellevis FG. Comorbidity and guidelines: conflicting interests. Lancet. 2006;367(9510):550–551. doi: 10.1016/S0140-6736(06)68198-1. [DOI] [PubMed] [Google Scholar]
- Smith SM, Soubhi H, Fortin M, Hudon C, O'Dowd T. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2012;4:CD006560. doi: 10.1002/14651858.CD006560.pub2. [DOI] [PubMed] [Google Scholar]
- Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716–724. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Studenski SA. Comparative effectiveness research and patients with multiple chronic conditions. N Engl J Med. 2011;364(26):2478–2481. doi: 10.1056/NEJMp1100535. [DOI] [PubMed] [Google Scholar]
- Ofman JJ, Badamgarav E, Henning JM, Knight K, Gano AD, Levan RK, Gur-Arie S, Richards MS, Hasselblad V, Weingarten SR. Does disease management improve clinical and economic outcomes in patients with chronic diseases? A systematic review. Am J Med. 2004;117(3):182–192. doi: 10.1016/j.amjmed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- Greß S, Baan CA, Clanan M, Dedeu T, Groenewegen P, Howson H, Maroy L, Nolte E, Redaèlli M, Saarelma O. et al. Co-ordination and management of chronic conditions in Europe: The role of primary care - Position paper of the European forum for primary care. Quality in Primary Care. 2009;17:75–86. [PubMed] [Google Scholar]
- Wagner EH, Bennett SM, Austin BT, Greene SM, Schaefer JK, Vonkorff M. Finding common ground: patient-centeredness and evidence-based chronic illness care. J Altern Complement Med. 2005;11(Suppl 1):S7–S15. doi: 10.1089/acm.2005.11.s-7. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T. Disease management–promises and pitfalls. N Engl J Med. 1999;340(15):1202–1205. doi: 10.1056/NEJM199904153401511. [DOI] [PubMed] [Google Scholar]
- Boult C, Karm L, Groves C. Improving chronic care: the "guided care" model. Perm J. 2008;12(1):50–54. doi: 10.7812/tpp/07-014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CM, Shadmi E, Conwell LJ, Griswold M, Leff B, Brager R, Sylvia M, Boult C. A pilot test of the effect of guided care on the quality of primary care experiences for multimorbid older adults. J Gen Intern Med. 2008;23(5):536–542. doi: 10.1007/s11606-008-0529-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starfield B, Lemke KW, Bernhardt T, Foldes SS, Forrest CB, Weiner JP. Comorbidity: implications for the importance of primary care in 'case' management. Ann Fam Med. 2003;1(1):8–14. doi: 10.1370/afm.1. [DOI] [PMC free article] [PubMed] [Google Scholar]