Abstract
Cold preservation has greatly facilitated the use of cadaveric kidneys for transplantation but damage occurs during the preservation episode. It is well established that oxidant production increases during cold renal preservation and mitochondria are a key target for injury. Our laboratory has demonstrated that cold storage of renal cells and rat kidneys leads to increased mitochondrial superoxide levels and mitochondrial electron transport chain damage, and that addition of Mitoquinone (MitoQ) to the preservation solutions blunted this injury. In order to better translate animal studies, the inclusion of large animal models is necessary to develop safe preclinical protocols. Therefore, we tested the hypothesis that addition of MitoQ to cold storage solution preserves mitochondrial function by decreasing oxidative stress, leading to less renal tubular damage during cold preservation of porcine kidneys employing a standard criteria donor model. Results showed that cold storage significantly induced oxidative stress (nitrotyrosine), renal tubular damage, and cell death. Using High Resolution Respirometry and fresh porcine kidney biopsies to assess mitochondrial function we showed that MitoQ significantly improved complex II/III respiration of the electron transport chain following 24 hours of cold storage. In addition, MitoQ blunted oxidative stress, renal tubular damage, and cell death after 48 hours. These results suggested that MitoQ decreased oxidative stress, tubular damage and cell death by improving mitochondrial function during cold storage. Therefore this compound should be considered as an integral part of organ preservation solution prior to transplantation.
Introduction
Renal transplantation is the treatment of choice for end stage renal disease (ESRD), because it increases patient survival and quality of life, and reduces medical costs for ESRD patients [1]. Brain death and cardiac death donors (both termed deceased donors) are the major sources of donor kidneys used in transplantation. These kidneys are routinely flushed with and preserved in cold storage solution to prolong viability while being matched for recipients [2].
Static cold storage is a convenient and fairly inexpensive method for renal allograft preservation [3], [4]. Short-term cold storage reduces cellular oxygen demand, but prolonged storage can cause extensive renal damage within the tubular and medullar compartments as well as marked mitochondrial damage resulting in reduced graft function and survival [5]–[7]. This could be due to renal cell damage mediated by high amounts of oxidants generated by the mitochondria, especially superoxide [8]–[11]. Currently, there are few specific therapies or approaches to reduce oxidative stress mediated cellular damage prior to transplantation. One growing strategy, however, is to counter the detrimental effects of ischemia, mediated by mitochondrial superoxide, as a consequence of prolonged cold storage, thereby improving graft survival function following transplantation.
Mitoquinone or MitoQ™ is a mitochondrial targeted antioxidant compound and has an ubiquinol (antioxidant) moiety on one end and a triphenylphosphonium (charged lipophilic cation that targets mitochondria) moiety on the other end [12]. MitoQ has been shown to modulate mitochondrial oxidant formation, which has numerous downstream effects that could be involved with its protection in a variety of pathologies including ischemia/reperfusion (cardiac [13], hepatic [14]), sepsis [15], diabetes [16], [17], cisplatin-induced nephropathy [18], and chronic alcohol-induced liver disease [19]. Our earlier report showed that the addition of MitoQ to a cold storage solution partially protected renal tubular cells and rat kidneys against cold storage mediated injury [20]. Furthermore, this report demonstrated that MitoQ minimizes the impact of oxidative stress in the cells by lowering steady state superoxide levels and improving electron transport chain (ETC) activity.
Experimental animal models play a crucial role in all stages of developing future clinical strategies and therapeutic interventions for human health and diseases. Large animal models are particularly necessary to develop safe preclinical protocols that are directly transferable to human subjects due to similarities in anatomical structure, size and physiology as well as disease progression. The pig is considered to be an ideal large animal model for human disease research [21]. Using porcine kidney as a renal model, we tested the hypothesis that addition of MitoQ to the cold storage solution would decrease mitochondrial superoxide, as well as preserve mitochondrial function; and that both effects would lead to less renal tubular damage during cold preservation. The results show that MitoQ blunted the cold-storage mediated oxidative stress and tubular damage, and preserved mitochondrial function by partially stabilizing respiration.
Methods
Animals
A standard criteria donor model was employed in which pig kidneys were explanted approximately 10 minutes after cessation of heart beat and brain death. Kidneys were obtained from 10 male farm pigs (25–30 kg, Hambone Farms, SC) donating other abdominal organs in IACUC approved studies. At the conclusion of IACUC approved liver or pancreas organ harvesting procedures, the pigs were euthanized by exsanguination under anesthesia according to the latest guidelines from the American Veterinary Medical Association Panel on Euthanasia (AVMA). Animal care and handling complied with the “Principles of Laboratory Animal Care” as formulated by the National Society for Medical Research and the “Guide for the Care and Use of Laboratory Animals” published by the National Research Council (National Academy press, 1996).
The animals were weighed and pre-anesthetized with a mixture of ketamine (22 mg/kg), acepromazine (1.1 mg/kg) and atropine (0.05 mg/kg) given IM. After establishing an ECG, the pigs were intubated, and placed on isoflurane anesthesia at 1.5–2%. The pigs were anticoagulated with heparin (400 IU/kg, IV). A midline incision was made from the top of the sternum to the pubis. The chest was opened to allow access to clamp off the dorsal aorta and the inferior vena cava in the thorax. After cannulation of the abdominal dorsal aorta the inferior vena cava was cut above the diaphragm. The abdominal organs were then perfused with 4L of cold Lactated Ringers followed by 1L cold Belzer’s solution also known as UW solution (SPS-1, Organ Recovery Systems, Itasca, IL). The kidneys were excised (with the renal artery, vein and ureter attached) and immersed in cold Belzer’s solution, placed on ice and moved to the back table for renal cannulation.
Cold Storage of Kidney
One of each pair of kidneys was allocated as an untreated control and the other experimental kidney to the MitoQ (100 µM) treatment group. 10–20 minutes after cessation of heartbeat, cannulation and time zero biopsy collection, the kidneys were flushed with cold Belzer’s solution ±100 µM MitoQ. The flush was performed at low pressure (20–40 mmHg) until the effluent was clear and residual blood eliminated. The kidneys were placed in sterile plastic bags with the remainder of 1L of cold Belzer’s solution ±100 µM MitoQ, respectively, and stored on ice during transportation to the research laboratory. The organs were then shipped in preservation solution (± MitoQ) on ice by express courier to the University of Arkansas for Medical Sciences (UAMS) for analysis. This type of organ transportation mimics that which occurs clinically with most human kidney donations. Biopsy specimens were then taken (at UAMS) at 24 h and 48 h of cold storage for histochemical and High Resolution Respirometry (HRR) analyses.
Cold storage group
Right kidneys were flushed with cold Belzer’s solution and stored in cold Belzer’s solution at 4°C for 24 and 48 h (n = 5).
Cold storage + MitoQ (100 µM) group
Left kidneys were flushed with cold Belzer’s solution and stored in cold Belzer’s solution +100 µM MitoQ at 4°C for 24 and 48 h (n = 5).
Kidney Morphology Based on PAS Staining
Renal sections were assessed for tissue injury using the Periodic Acid-Schiff’s (PAS) reaction as described [22]. Evaluation was conducted in a blinded fashion based on the following criteria: cell swelling, loss of tubular brush border, tubular cell degeneration, sloughing of epithelial cell, and casts in lumen. All parameters were graded on a scale of 0-no lesion, 1-minimal change, 2-mild change, and, 3-prominent change. Finally, comparisons were made between the groups (cold storage group and cold storage +100 µM MitoQ group). All images were taken using a Nikon Eclipse E800 microscope (Q Capture imaging and Nikons Elements software).
Immunohistochemistry
Immunohistochemical analysis was done as described previously [22]. The primary antibodies against anti-nitrotyrosine (1∶6000 dilution; Millipore, MA, USA) was prepared in antibody diluent solution (0.5% non-fat dry milk and 1% BSA in TBS) and incubated overnight at 4°C. Immunoreactivity was detected by Dako Envision+ System-HRP (Dako, CA, USA). Counterstaining was performed using Mayer’s Hematoxylin (Electron Microscopy Science, PA, USA). Semi quantitative evaluation on nitrotyrosine staining was performed as described [22].
TUNEL Assay
For visualization of apoptotic cells in situ terminal transferase-mediated dUTP nick-end labeling (TUNEL) method was utilized according to the protocol provided by the manufacturer (TACS™ TdT Kit, R&D Systems, MN, USA). Counterstaining was performed using methyl green solution.
High Resolution Respirometry (HRR)
Complex activity of the electron transport chain (ETC) was measured by high resolution respirometry (HRR) with the OROBOROS Oxygraph-2k (Oroboros instruments, Innsbruck, Austria) according to substrate-inhibitor-titration (SIT) protocol. Briefly, renal biopsies representing cortex and medulla were taken transversely using Speed Cut Biopsy Needle (18G x 10 cm, Gallini). The biopsy specimen was then minced, weighed (6–8 mg, wet weight), and permeabilized with 100 µg/ml saponin prepared in mitochondrial respiration medium MiRO5 [23], [24] by shaking gently at 4°C for 30 min. Permeabilized renal biopsies were then washed 3 times (2 min each) with MiRO5 medium and data acquisition was performed at 37°C. Mitochondrial respiration was initiated by adding 2 mM malate and 10 mM glutamate (Complex I substrate) and maximum active respiration was achieved by adding 2.5 mM ADP. Rotenone (0.2 mM) was then added to completely inhibit complex I respiration. To measure Complex II+III respiration 10 mM succinate (complex II substrate) was added followed by 10 µM antimycin A to inhibit complex III respiration. Finally, Complex IV respiration was monitored by adding 1 mM N,N,N′,N′-Tetramethyl-p-phenylenediamine (TMPD, substrate for complex IV) made in 0.8 M Ascorbate (pH = 6.0). Inhibition of complex IV was achieved by titrating 800 mM Sodium azide. Finally, data analysis was done using DATLAB 4.2 software (Oroboros) and tissue respiration was presented as oxygen flux (pmol/mg/s).
Statistical Analysis
Results are presented as mean ± standard error of the mean (SEM). Student's t test (paired) was used to compare differences between the mean of paired groups at 95% level of confidence. Differences with a P value less than 0.05 were considered statistically significant.
Results and Discussion
Recently, we have shown that cold storage of rat kidneys leads to increased tubular damage [20], [25] and MitoQ partially protected the cold stored rat kidneys from such damage [20]. The current study was designed for preclinical translation to a large animal renal model to determine whether or not similar protective effects of MitoQ would be observed during cold storage. Preliminary experiments using histopathology (PAS staining) as the primary endpoint for 25, 50, 100 and 200 µM MitoQ doses were tested in at least four kidneys cold stored for 48 hr. The 100 µM MitoQ dose demonstrated the greatest cortical protection (data not shown) and was used in further experiments.
It should be noted that the concentration of MitoQ used in these cold storage studies is quite high compared to other studies, which use nM concentrations. However, since MitoQ uptake within mitochondria is dependent on mitochondrial membrane potential, which is dramatically lowered during cold storage [10]; it is expected that only a fraction of the dose used is actually taken up in renal mitochondria. In addition, the use of intact, whole kidneys also likely impairs the diffusion of MitoQ.
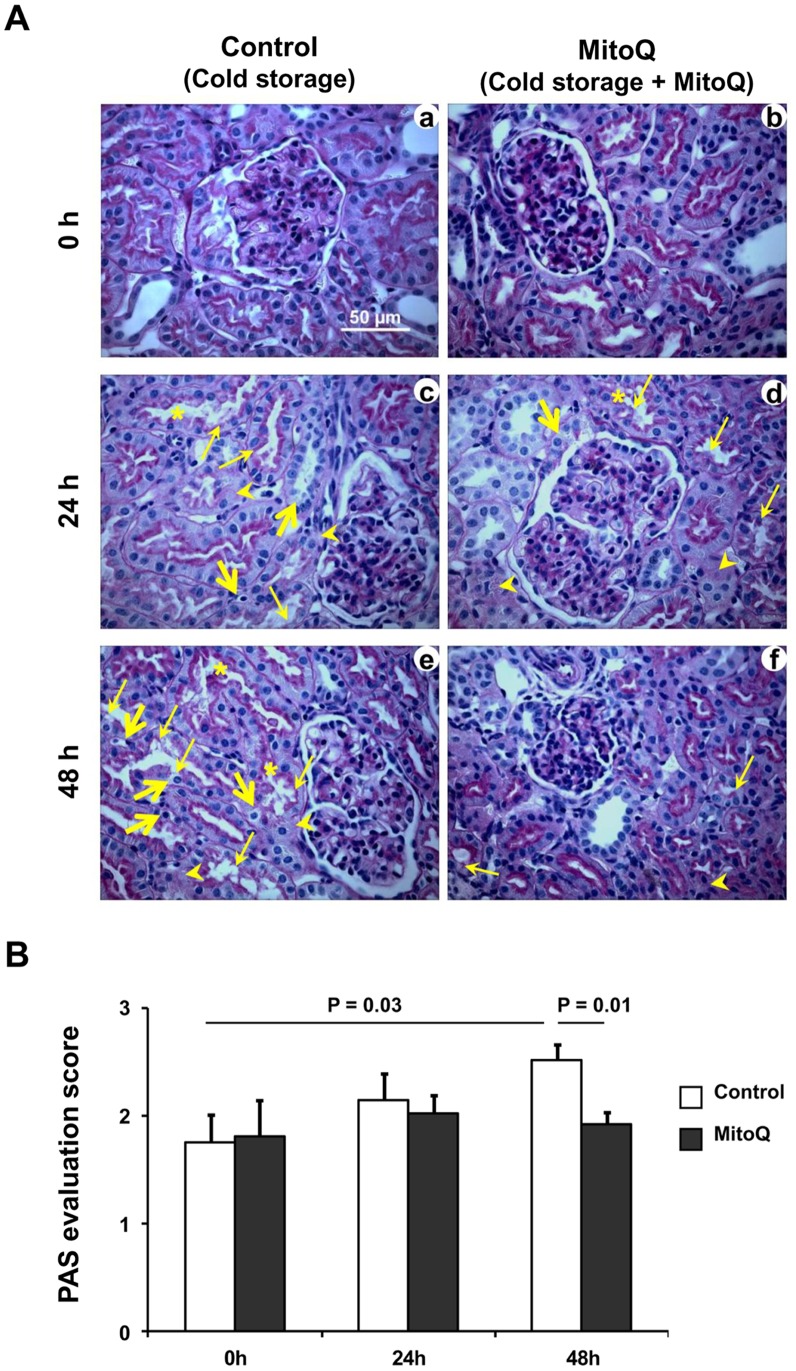
The porcine kidney model was selected because canine kidneys in contrast to human are relatively resistant to cold ischemic injury [26]. Primates were not considered due to cost. The porcine kidney is more sensitive to cold preservation [27] and is therefore more likely to demonstrate a clear impact of ischemic injury. The pig was also chosen because its renal anatomy and physiology resemble humans [21]. Although hypothermia reduces the metabolic activity and energy demand [7], renal structural changes occur during static cold preservation [20], [25]. Cold ischemia induced prominent tubular damage including epithelial cell degeneration (arrow heads) loss of brush border (thin arrows), detachment of epithelial cells from basement membrane and sloughing of epithelial cells (thick arrows), and cast formation (asterisks) were observed after 24 and 48 h in the kidneys when compared to the baseline tubular injury of control porcine kidneys ( Fig. 1A panel a, 0 h; panel c, 24 h; panel e, 48 h). Mito Q reduced this cold storage mediated tubular damage after 48 h ( Fig. 1A panel b, 0 h; panel d, 24 h; panel f, 48 h). Semi-quantitative evaluation based on the histopathology review scores showed that renal tubular damage increased significantly after 48 h of cold storage (P = 0.03) compared to baseline, and MitoQ significantly blunted this cold storage mediated tubular damage when compared to the contralateral control cold stored kidneys without MitoQ ( Fig. 1B, P = 0.01). Cold ischemia induces renal tubular cell necrosis and the injury increases with time [28]. Acute tubular necrosis, especially in the papilla/inner medulla, is a common event following transplantation of cold stored renal allografts. We also observed a similar necrotic episode of renal tubules after cold ischemia and surprisingly, MitoQ failed to blunt this tubular necrosis in the inner medulla (Figure S1). This could be due to limited availability of MitoQ to this deeper region during flushing and static cold preservation. These results suggest that MitoQ facilitated preservation of the renal tubular structure in the cortex and outer medullary regions in cold storage solution for up to 48 h.
Figure 1. MitoQ (100 µM) blunts tubular injury following cold storage.
(A) Representative 400X micrographs of PAS staining in renal cortical section of pig after 24 and 48 h of cold storage (CS) and CS + MitoQ. Representative bar indicates 50 µm. Thin arrows indicate loss of brush border; thick arrows indicate renal epithelial cell detachment and/or cell sloughing; arrow heads indicate epithelial cell degeneration; and asterisks indicate tubular casts. (B) Pathological scoring for tubular injury as a result of cold storage. Error bar indicates Mean ± S.E.M. (n = 5 for both groups). Cold storage significantly induced renal tubular damage at 48 h time point (P = 0.03), and MitoQ significantly blunted this injury (P = 0.01).
Limited availability of MitoQ in the inner medulla during flush cold preservation could be overcome by hypothermic machine perfusion (HMP) preservation. Significant clinical improvements in the quality of kidney preservation and patient treatment have been reported using HMP [29]–[31]. The results of an international randomized, controlled trial in which hypothermic machine perfusion was compared with static cold stored kidneys demonstrated significantly reduced delayed graft function and improved graft survival when one kidney from each donor was randomly assigned to machine perfusion, and the contralateral organ was assigned to cold storage [29]. More recently, the authors reported three year follow-up data showing survival was better for machine-perfused kidneys (P<0.04) and the survival advantage after machine perfusion was most pronounced from expanded criteria (ECD) donors (86 v 76%, p<0.04) [32]. Future experiments are planned to investigate whether the addition of MitoQ to HMP solution improves preservation of the inner medulla.
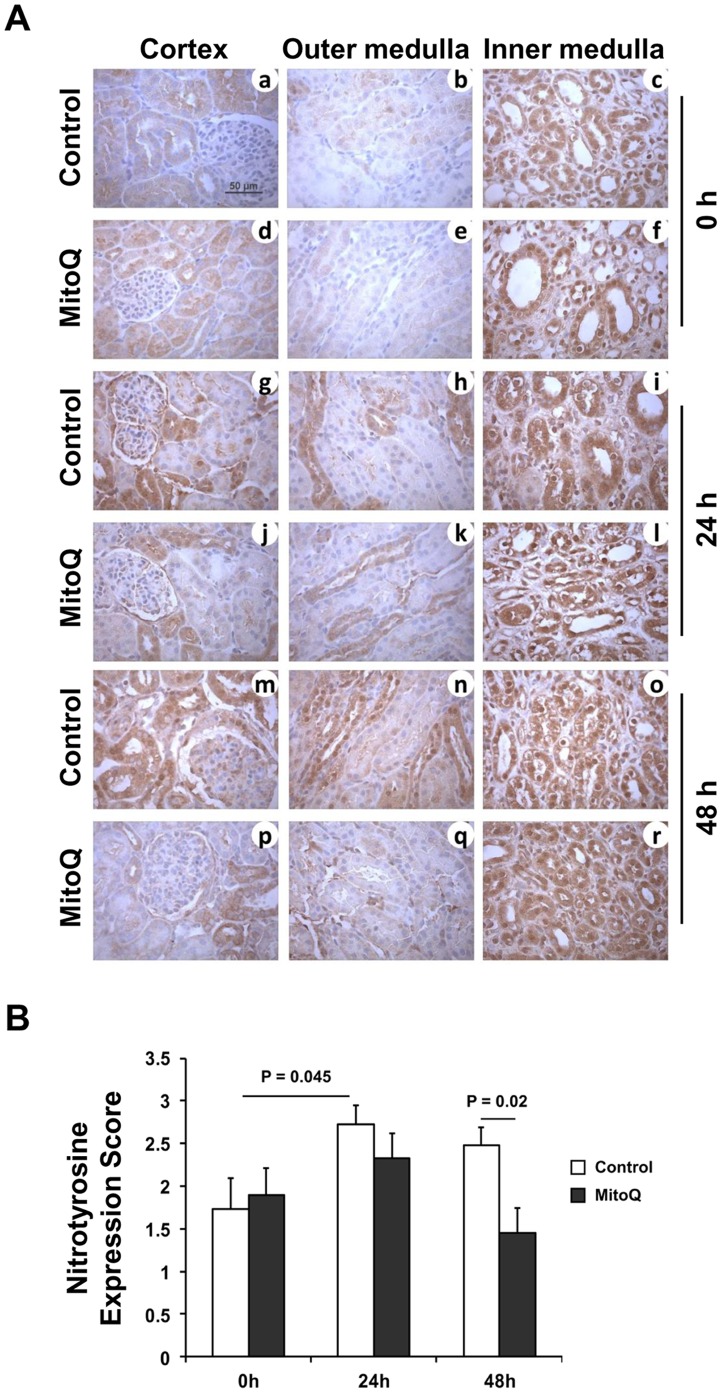
Oxidative stress has been shown to play a detrimental role during cold preservation [11], [25], [33], and mitochondria are a potential source of reactive oxygen species (ROS) during cold storage [10], [20]. MitoQ targets mitochondria and scavenges mitochondrial ROS thereby reducing the oxidative stress load [14], [15], [17]–[19], [34], [35]. Using nitrotyrosine as an oxidative stress marker, we evaluated MitoQ’s role in blunting cold ischemia induced oxidative stress in porcine kidneys. In control porcine kidneys exposed to cold storage, nitrotyrosine was present, especially within the inner medullary region ( Fig. 2A ) suggesting that oxidative stress increases rapidly following preservation [36]. Similar to earlier reports in rodent models [20], [25], porcine kidneys also showed increased nitrotyrosine protein accumulation after 24 h and 48 h of cold storage in the cortex and outer medullary region ( Fig. 2A ). As expected, MitoQ blunted cold ischemia induced oxidative stress in the renal tubules after 24 and 48 h as evident by less nitrotyrosine protein accumulation in the cortical and outer medullary region. Surprisingly, nitrotyrosine protein expression in the inner medulla remained unchanged even after addition of MitoQ in the cold storage solution. The reason can be two-fold: 1) the inner medulla actually endured the maximum level of oxidative stress before the organ collection was initiated and MitoQ could not correct the irreversible nature of nitrotyrosine formation; and 2) the concentration of MitoQ during cold storage may be different in the cortex, outer medulla and inner medulla, with the inner medulla concentration being the lowest likely due to poor perfusion during the initial cold flush. Semi-quantitative evaluation based on nitrotyrosine expression score (see methods) showed a significant reduction of nitrotyrosine protein following inclusion of MitoQ at 48 h of cold storage of kidneys when compared to the cold stored kidneys without MitoQ ( Fig. 2B, P = 0.02). These results suggest that MitoQ reduces the oxidative stress load when the organs are stored for up to 48 h.
Figure 2. MitoQ blunts protein nitration from oxidative stress during cold storage.
(A) Representative 400 X micrographs of nitrotyrosine immunostaining are shown. Representative bar indicates 50 µm. (B) Expression level of Nitrotyrosine was evaluated semi-quantitatively and scored. Error bar indicates Mean ± S.E.M. (n = 5 for both groups). Cold storage significantly increased nitrotyrosine protein accumulation at 24 h time point (P = 0.045). MitoQ significantly blunted protein nitration at 48 h time point (P = 0.02).
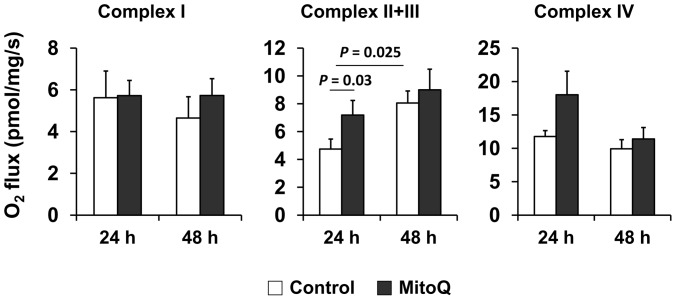
Previous studies show that cold storage induced mitochondrial oxidative stress leads to alteration of renal ETC activity [10], [20], [25]. Therefore, in this pig model, we studied whether MitoQ altered mitochondrial respiration function during cold storage. Because isolating mitochondria from injured tissues for conventional respiration studies may yield inconsistent populations of mitochondria, we assessed mitochondrial respiration on kidney biopsies using High Resolution Respirometry (HRR). Fresh biopsy specimens from 24 and 48 h cold stored kidneys (with or without MitoQ) were employed to study ETC complexes (I, II+III and IV) using substrate-inhibitor-titration (SIT) protocol (see methods). MitoQ treatment lead to increased complex II+III respiration when compared to the control kidneys cold stored for 24 h ( Fig. 3 , P = 0.032, 24 h). This is important since complex III has been shown to be one of the major sites of superoxide generation in cells [25], [37]–[41]. The other complexes (I and IV) respiration remained unaltered by MitoQ addition during cold storage ( Fig. 3 ).
Figure 3. MitoQ improves electron transport chain function during cold storage.
Respiration status of complex I, II+III, and IV of the ETC evaluated using SIT protocol (see methods). The graph shows mitochondrial complex respiration (measured as oxygen flux) of fresh renal biopsies that were cold stored with or without MitoQ. Error bar indicates Mean ± S.E.M. (n = 5 for both groups). MitoQ significantly improved complex II+III respiration at 24 h time point (P = 0.03). Cold preservation (without MitoQ) also improved complex II+III respiration after 48 h (P = 0.025).
Interestingly, control kidneys exposed to prolonged cold storage (48 h) resulted in significantly increased mitochondrial complex II+III respiration when compared to the 24 h time point ( Fig. 3 . P = 0.025). Since 48 h cold storage increased complex II+III respiration, no further increase was observed with MitoQ treatment at this later time point. The precise mechanism for improved mitochondrial function by prolonged cold storage and MitoQ remains unknown. One possibility is that prolonged cold storage stimulates other compensatory pathways such as autophagy to clear damaged cellular constituents [42], which could include dysfunctional mitochondria (called mitophagy). In addition, it has been shown that cold acclimation [43], [44] and oxidative stress [45]–[47] can induce mitochondrial biogenesis. Increased autophagy and biogenesis could collectively remove damaged mitochondria and restore new mitochondria, hence improve mitochondrial function. In fact, we have rodent data showing that increased mitochondrial superoxide (as a result of MnSOD knockdown) results in increased autophagy and biogenesis (unpublished results). Our new data (porcine) suggest that cold storage (24 hr) induces oxidant production and mitochondrial damage early on (24 hr) and this in turn leads to renal damage (48 hr). Since MitoQ has been shown to modulate mitochondrial ROS formation [14], [15], [17]–[19], [35], it is plausible that reduced ROS leads to improved complex II/III activity. Our data also suggest use of the HRR technique could be quite useful in the determination of donor status prior to transplantation.
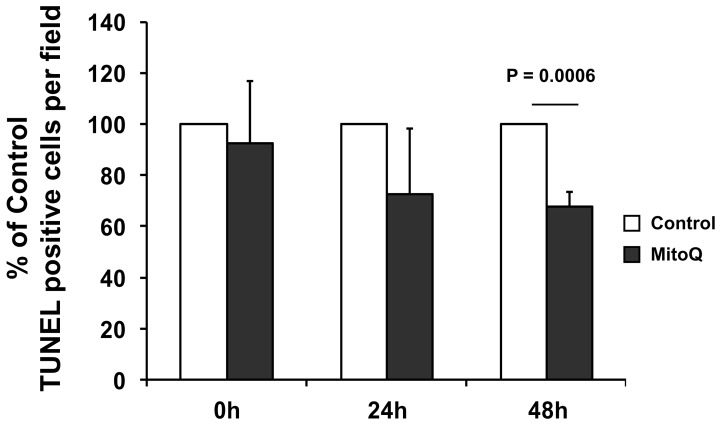
Cold ischemia causes a rapid depletion of ATP and accumulation of ROS that leads to mitochondrial injury and renal cell death [7]–[10], [25], [33], [48]. We further evaluated whether MitoQ also blocked cold ischemia induced renal cell death in the pig model. Similar to the PAS and nitrotyrosine data, TUNEL staining showed a significant increase of TUNEL positive cells, i.e., renal cell death, after 48 h of cold storage. Also similar to the reduced amount of tubular damage as observed in PAS staining, and decreased oxidative stress observed in nitrotyrosine staining, MitoQ significantly blocked cold storage mediated renal cell death after 48 h, as evident by less TUNEL positive cells in the porcine kidneys ( Fig. 4 , P = 0.0006). These results suggest that the antioxidant property of MitoQ may have prevented renal cell death during cold storage. All results combined, indicate that MitoQ partially improved ETC function which blunted cold storage induced oxidative stress, renal tubular damage, and cell death. MitoQ has also been shown to protect against complex I inactivation during hepatic I/R [18] and complex IV inactivation during cisplatin nephrotoxicity [14]. Lu et al. also showed that a functional electron transport chain is not required for MitoQ mediated protection [49]. We believe that MitoQ is working via decreased mitochondrial superoxide production which also reduces downstream ROS production including hydrogen peroxide and peroxynitrite.
Figure 4. MitoQ blocks cold storage induced renal cell death. TUNEL positive cells were counted in 8 different fields (200X), and the average was reported.
The graph shows percentage change of TUNEL positive cells after MitoQ treatment when compared to respective contra lateral control kidneys. Error bar indicates Mean ± S.E.M. (n = 5 for both groups). MitoQ significantly reduced TUNEL positive nuclei after 48 h of cold storage (P = 0.0006).
The availability of human kidneys for clinical transplantation is limited and the need of transplantable, good quality human organs is growing. It is therefore crucial to improve organ preservation quality to maximize procured renal allograft for clinical transplantation. In this report we demonstrated the significantly improved quality of cadaveric porcine kidneys by addition of 100 µM MitoQ in Belzer’s solution during cold storage (4°C). The addition of MitoQ reduced oxidative stress during cold storage for up to 48 h, which decreased tubular damage, improved mitochondrial function, and led to decreased renal cell death. These results highlight MitoQ as a promising anti-oxidant drug to be included in cold solution (UW) for improved quality and prolonged renal allograft preservation.
Supporting Information
MitoQ (100 µM) blunts tubular injury following cold storage. Representative 400X micrographs of PAS staining in renal cortex, inner and outer medulla of pig after 24 and 48 h of control (cold storage) and MitoQ (cold storage + MitoQ). Representative bar indicates 50 µm. N = 5 for both groups.
(TIF)
Acknowledgments
Authors would also like to thank Ishwori B. Dhakal for assistance with statistical evaluation, Dr. Michael P. Murphy for providing MitoQ, Amanda Hunt and Grayson Greer for assistance with immunohistochemical analysis, and UAMS Translational Pathology Shared Resource for the excellent service in processing paraffin embedded tissue blocks.
Funding Statement
The study was supported by a US Public Health Grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), Grant #R43DK089659, to KGMB/LAMC. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIDDK or the National Institutes of Health.
References
- 1. Schnuelle P, Lorenz D, Trede M, van der Woude FJ (1998) Impact of renal cadaveric transplantation on survival in end-stage renal failure: evidence for reduced mortality risk compared with hemodialysis during long-term follow-up. J Am Soc Nephrol 9: 2135–2141. [DOI] [PubMed] [Google Scholar]
- 2. Bon D, Chatauret N, Giraud S, Thuillier R, Favreau F, et al. (2012) New strategies to optimize kidney recovery and preservation in transplantation. Nat Rev Nephrol 8: 339–347. [DOI] [PubMed] [Google Scholar]
- 3. McAnulty JF (2010) Hypothermic organ preservation by static storage methods: Current status and a view to the future. Cryobiology 60: S13–S19. [DOI] [PubMed] [Google Scholar]
- 4. Watson CJE, Wells AC, Roberts RJ, Akoh JA, Friend PJ, et al. (2010) Cold Machine Perfusion Versus Static Cold Storage of Kidneys Donated After Cardiac Death: A UK Multicenter Randomized Controlled Trial. American Journal of Transplantation 10: 1991–1999. [DOI] [PubMed] [Google Scholar]
- 5. Salahudeen AK, Haider N, May W (2004) Cold ischemia and the reduced long-term survival of cadaveric renal allografts. Kidney Int 65: 713–718. [DOI] [PubMed] [Google Scholar]
- 6. Stubenitsky BM, Booster MH, Kootstra G, Brasile L, Haisch C (2001) Deletrious effect of prolonged cold ischemia on renal function. Transpl Int 14: 256–260. [DOI] [PubMed] [Google Scholar]
- 7. Belzer FO, Southard JH (1988) Principles of solid-organ preservation by cold storage. Transplantation 45: 673–676. [DOI] [PubMed] [Google Scholar]
- 8. Salahudeen AK (1999) Free radicals in kidney disease and transplantation. Saudi J Kidney Dis Transpl 10: 137–143. [PubMed] [Google Scholar]
- 9. Peters SM, Rauen U, Tijsen MJ, Bindels RJ, van Os CH, et al. (1998) Cold preservation of isolated rabbit proximal tubules induces radical-mediated cell injury. Transplantation 65: 625–632. [DOI] [PubMed] [Google Scholar]
- 10. Mitchell T, Saba H, Laakman J, Parajuli N, Macmillan-Crow LA (2010) Role of mitochondrial-derived oxidants in renal tubular cell cold-storage injury. Free Radic Biol Med 49: 1273–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Salahudeen AK, Huang H, Patel P, Jenkins JK (2000) Mechanism and prevention of cold storage-induced human renal tubular cell injury. Transplantation 70: 1424–1431. [DOI] [PubMed] [Google Scholar]
- 12. Kelso GF, Porteous CM, Coulter CV, Hughes G, Porteous WK, et al. (2001) Selective Targeting of a Redox-active Ubiquinone to Mitochondria within Cells. J Biol Chem 276: 4588–4596. [DOI] [PubMed] [Google Scholar]
- 13. Adlam VJ, Harrison JC, Porteous CM, James AM, Smith RA, et al. (2005) Targeting an antioxidant to mitochondria decreases cardiac ischemia-reperfusion injury. FASEB J 19: 1088–1095. [DOI] [PubMed] [Google Scholar]
- 14. Mukhopadhyay P, Horvath B, Zsengeller Z, Batkai S, Cao Z, et al. (2012) Mitochondrial reactive oxygen species generation triggers inflammatory response and tissue injury associated with hepatic ischemia-reperfusion: Therapeutic potential of mitochondrially targeted antioxidants. Free Radic Biol Med 53: 1123–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lowes DA, Thottakam BM, Webster NR, Murphy MP, Galley HF (2008) The mitochondria-targeted antioxidant MitoQ protects against organ damage in a lipopolysaccharide-peptidoglycan model of sepsis. Free Radic Biol Med 45: 1559–1565. [DOI] [PubMed] [Google Scholar]
- 16. Chacko BK, Reily C, Srivastava A, Johnson MS, Ye Y, et al. (2010) Prevention of diabetic nephropathy in Ins2(+/)(−)(AkitaJ) mice by the mitochondria-targeted therapy MitoQ. Biochem J 432: 9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mercer JR, Yu E, Figg N, Cheng KK, Prime TA, et al. (2012) The mitochondria-targeted antioxidant MitoQ decreases features of the metabolic syndrome in ATM+/−/ApoE−/− mice. Free Radic Biol Med 52: 841–849. [DOI] [PubMed] [Google Scholar]
- 18. Mukhopadhyay P, Horvath B, Zsengeller Z, Zielonka J, Tanchian G, et al. (2012) Mitochondrial-targeted antioxidants represent a promising approach for prevention of cisplatin-induced nephropathy. Free Radic Biol Med 52: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chacko BK, Srivastava A, Johnson MS, Benavides GA, Chang MJ, et al. (2011) Mitochondria-targeted ubiquinone (MitoQ) decreases ethanol-dependent micro and macro hepatosteatosis. Hepatology 54: 153–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mitchell T, Rotaru D, Saba H, Smith RA, Murphy MP, et al. (2011) The mitochondria-targeted antioxidant mitoquinone protects against cold storage injury of renal tubular cells and rat kidneys. J Pharmacol Exp Ther 336: 682–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Giraud S, Favreau F, Chatauret N, Thuillier R, Maiga S, et al. (2011) Contribution of large pig for renal ischemia-reperfusion and transplantation studies: the preclinical model. J Biomed Biotechnol 2011: 532127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Parajuli N, Marine A, Simmons S, Saba H, Mitchell T, et al. (2011) Generation and characterization of a novel kidney-specific manganese superoxide dismutase knockout mouse. Free Radic Biol Med 51: 406–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kuznetsov AV, Veksler V, Gellerich FN, Saks V, Margreiter R, et al. (2008) Analysis of mitochondrial function in situ in permeabilized muscle fibers, tissues and cells. Nat Protocols 3: 965–976. [DOI] [PubMed] [Google Scholar]
- 24.Gnaiger E, Kuznetsov AV, Schneeberger S, Seiler R, Brandacher G, et al.. (2000) Mitochondria in the Cold. In: Heldmaie G., Klingenspor M., editors. Life in the Cold. Springer Berlin Heidelberg New York. 431–442.
- 25. Saba H, Munusamy S, Macmillan-Crow LA (2008) Cold preservation mediated renal injury: involvement of mitochondrial oxidative stress. Ren Fail 30: 125–133. [DOI] [PubMed] [Google Scholar]
- 26. Ploeg RJ, Goossens D, McAnulty JF, Southard JH, Belzer FO (1988) Successful 72-hour cold storage of dog kidneys with UW solution. Transplantation 46: 191–196. [DOI] [PubMed] [Google Scholar]
- 27. Nicholson ML, Hosgood SA, Metcalfe MS, Waller JR, Brook NR (2004) A comparison of renal preservation by cold storage and machine perfusion using a porcine autotransplant model. Transplantation 78: 333–337. [DOI] [PubMed] [Google Scholar]
- 28. Salahudeen AK, Joshi M, Jenkins JK (2001) Apoptosis versus necrosis during cold storage and rewarming of human renal proximal tubular cells. Transplantation 72: 798–804. [DOI] [PubMed] [Google Scholar]
- 29. Moers C, Smits JM, Maathuis MH, Treckmann J, van Gelder F, et al. (2009) Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med 360: 7–19. [DOI] [PubMed] [Google Scholar]
- 30. Moers C, Varnav OC, van Heurn E, Jochmans I, Kirste GR, et al. (2010) The value of machine perfusion perfusate biomarkers for predicting kidney transplant outcome. Transplantation 90: 966–973. [DOI] [PubMed] [Google Scholar]
- 31. Treckmann J, Moers C, Smits JM, Gallinat A, Maathuis MH, et al. (2011) Machine perfusion versus cold storage for preservation of kidneys from expanded criteria donors after brain death. Transpl Int 24: 548–554. [DOI] [PubMed] [Google Scholar]
- 32. Moers C, Pirenne J, Paul A, Ploeg RJ (2012) Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med 366: 770–771. [DOI] [PubMed] [Google Scholar]
- 33. Salahudeen AK, Huang H, Joshi M, Moore NA, Jenkins JK (2003) Involvement of the mitochondrial pathway in cold storage and rewarming-associated apoptosis of human renal proximal tubular cells. Am J Transplant 3: 273–280. [DOI] [PubMed] [Google Scholar]
- 34. Skulachev VP (2005) How to Clean the Dirtiest Place in the Cell: Cationic Antioxidants as Intramitochondrial ROS Scavengers. IUBMB Life 57: 305–310. [DOI] [PubMed] [Google Scholar]
- 35. James AM, Cocheme HM, Smith RAJ, Murphy MP (2005) Interactions of Mitochondria-targeted and Untargeted Ubiquinones with the Mitochondrial Respiratory Chain and Reactive Oxygen Species. J Biol Chem 280: 21295–21312. [DOI] [PubMed] [Google Scholar]
- 36. Monton S, Herrera J, Ferrer JV, Guerrero D, Balen E, et al. (1999) Experimental model of non-heart-beating donors: oxidative stress metabolism in kidney after cardiac arrest (30 minutes of warm ischemia) and reimplantation 24 hours later. Transplant Proc 31: 2350–2351. [DOI] [PubMed] [Google Scholar]
- 37. Muller FL, Roberts AG, Bowman MK, Kramer DM (2003) Architecture of the Qo Site of the Cytochrome bc1 Complex Probed by Superoxide Production. Biochemistry (Mosc) 42: 6493–6499. [DOI] [PubMed] [Google Scholar]
- 38. Crofts AR (2004) The cytochrome bc1 complex: function in the context of structure. Annu Rev Physiol 66: 689–733. [DOI] [PubMed] [Google Scholar]
- 39. Ksenzenko M, Konstantinov AA, Khomutov GB, Tikhonov AN, Ruuge EK (1983) Effect of electron transfer inhibitors on superoxide generation in the cytochrome bc1 site of the mitochondrial respiratory chain. FEBS Lett 155: 19–24. [DOI] [PubMed] [Google Scholar]
- 40. Muller FL, Liu Y, Van Remmen H (2004) Complex III Releases Superoxide to Both Sides of the Inner Mitochondrial Membrane. J Biol Chem 279: 49064–49073. [DOI] [PubMed] [Google Scholar]
- 41. Muller F, Crofts AR, Kramer DM (2002) Multiple Q-Cycle Bypass Reactions at the Qo Site of the Cytochrome bc1 ComplexΓÇá. Biochemistry (Mosc) 41: 7866–7874. [DOI] [PubMed] [Google Scholar]
- 42. Turkmen K, Martin J, Akcay A, Nguyen Q, Ravichandran K, et al. (2011) Apoptosis and autophagy in cold preservation ischemia. Transplantation 91: 1192–1197. [DOI] [PubMed] [Google Scholar]
- 43. Bruton JD, Aydin J, Yamada T, Shabalina IG, Ivarsson N, et al. (2010) Increased fatigue resistance linked to Ca2+-stimulated mitochondrial biogenesis in muscle fibres of cold-acclimated mice. J Physiol 588: 4275–4288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Klingenspor M, Ivemeyer M, Wiesinger H, Haas K, Heldmaier G, et al. (1996) Biogenesis of thermogenic mitochondria in brown adipose tissue of Djungarian hamsters during cold adaptation. Biochem J 316 (Pt 2): 607–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Suliman HB, Welty-Wolf KE, Carraway M, Tatro L, Piantadosi CA (2004) Lipopolysaccharide induces oxidative cardiac mitochondrial damage and biogenesis. Cardiovasc Res 64: 279–288. [DOI] [PubMed] [Google Scholar]
- 46. Suliman HB, Carraway MS, Welty-Wolf KE, Whorton AR, Piantadosi CA (2003) Lipopolysaccharide stimulates mitochondrial biogenesis via activation of nuclear respiratory factor-1. J Biol Chem 278: 41510–41518. [DOI] [PubMed] [Google Scholar]
- 47. Yoboue ED, Devin A (2012) Reactive oxygen species-mediated control of mitochondrial biogenesis. Int J Cell Biol 2012: 403870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hauet T, Bauza G, Goujon JM, Caritez JC, Carretier M, et al. (1998) Effects of trimetazidine on lipid peroxidation and phosphorus metabolites during cold storage and reperfusion of isolated perfused rat kidneys. J Pharmacol Exp Ther 285: 1061–1067. [PubMed] [Google Scholar]
- 49. Lu C, Zhang D, Whiteman M, Armstrong JS (2008) Is antioxidant potential of the mitochondrial targeted ubiquinone derivative MitoQ conserved in cells lacking mtDNA? Antioxid Redox Signal 10: 651–660. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
MitoQ (100 µM) blunts tubular injury following cold storage. Representative 400X micrographs of PAS staining in renal cortex, inner and outer medulla of pig after 24 and 48 h of control (cold storage) and MitoQ (cold storage + MitoQ). Representative bar indicates 50 µm. N = 5 for both groups.
(TIF)