Abstract
Background
Hip fracture is a serious injury for older adults, usually requiring surgical repair and extensive therapy. Informal caregivers can help older adults make a successful recovery by encouraging them to adhere to the therapy plans and improve their health behaviors. Few resources, however, are available for these caregivers to learn about how to assist their care receivers and cope with their unique caregiving situations.
Objective
To develop a comprehensive theory-based online hip fracture resource center for caregivers, Caring for Caregivers, and conducted a feasibility trial.
Method
The resource center included self-learning modules, discussion boards, Ask the Experts, and a virtual library. The feasibility of the intervention was assessed by usage and usability. The feasibility of the future trial was tested using a one-group pre-post design on 36 caregiving-care receiver dyads recruited from six hospitals. The caregivers used the resource center for 8 weeks. The impact of the intervention was assessed on both caregivers (primary) and care receivers (secondary). The data were analyzed by descriptive statistics, paired t-tests, and content analyses.
Results
On average, caregivers reviewed five modules and used the discussion board 3.1 times. The mean perceived usability score for the resource center was 74.04 ± 7.26 (range = 12–84). Exposure to the resource center significantly improved caregivers’ knowledge about the care of hip fracture patients (t = 3.17, p = .004) and eHealth literacy (t = 2.43, p = .002). Changes in other caregiver outcomes (e.g., strain, coping, social support) and care receiver outcomes (e.g., self-efficacy for exercise, osteoporosis medication adherence) were favorable but not significant.
Discussion
The findings suggest that the resource center was user-friendly and could be beneficial for caregivers. Additional larger scale trials are needed to assess the effectiveness of the intervention on outcomes.
Keywords: Internet resource, caregivers, hip fracture
Hip fracture is a serious public health problem in older adults (Duthie, Katz, & Malone, 2007; Magaziner et al., 2003; Orwig et al., 2011). In 2006, there were 316,000 hospital admissions for hip fractures among adults age 65 years and older (Centers for Disease Control and Intervention, 2010). Older adults surviving hip fractures have a high risk (up to 50%) for having functional disability (Magaziner et al., 2003; Roth, Kammerlander, Gosch, Luger, & Blauth, 2010) and subsequent fractures (10–20%; Magaziner et al., 2003). Unlike other debilitating conditions (e.g., Alzheimer’s disease), however, hip fracture is an acute event, and older adults can recover their functional abilities with appropriate interventions (Magaziner et al., 2003; Nahm, Resnick, Orwig, Magaziner, & Degrezia, 2010; Resnick et al., 2007). In fact, a hip fracture event can provide a unique education opportunity to change prefracture health behaviors (e.g., exercise) and implement appropriate interventions (e.g., environmental changes) to prevent future fractures (Nahm et al., 2010; Shawler, 2006).
The role of informal caregivers (CGs; e.g., family members, significant others) is particularly important during recovery because most hip fracture patients develop significant functional dependency that persists even after undergoing a surgical repair of the fracture (Nahm et al., 2010; Shyu, Chen, Wu, & Cheng, 2010). Caregivers have unique support needs related to the acute and unexpected nature of hip fractures and the quick transition of care settings. They often assume their role for the first time and have to learn quickly about many aspects of care, such as provision of personal care to their care recipients (CRs), arrangement of rehabilitation services, and management of medical bills (Nahm et al., 2010). In addition, most CGs have to juggle care-related tasks, work, and family responsibilities, and experience exhaustion. These CGs need a program that is timely and easily accessible. An online hip fracture resource center could be an effective method to meet these CGs’ support needs (Kernisan, Sudore, & Knight, 2010). Using the Internet, CGs could access the resource program at their own convenience (Nahm et al., 2010; Zickuhr, 2010), and healthcare providers could deliver timely health information and demonstrate specific procedures to CGs. A social networking component could be used to facilitate CGs’ peer support and provide a motivational intervention.
The purpose of this study was to develop a theory-based Online Hip Fracture Resource Center (OHRC) for CGs and to conduct a feasibility study to test the OHRC for a future randomized controlled trial. The two theories guiding the study are: stress, appraisal, and coping, and self-efficacy and outcome expectations. The OHRC was focused on maximizing the care relationship in the CG-CR dyad by providing interactive, anticipatory support (e.g., information about the recovery process and the care needed) to the CGs and facilitating CGs in delivery of self-efficacy based interventions to their CRs.
The feasibility of the OHRC was assessed by the degree of usage and the perceived usability. The feasibility of the OHRC intervention protocol was assessed through the implementation of the protocol to identify any issues related to recruitment and data collection processes and to assess the recruitment and retention rates. The primary outcome measures were focused on CGs (CG strain, coping effectiveness, social support, and knowledge about hip fracture care). Care recipient outcomes [self-efficacy and outcome expectations for exercise and osteoporosis medication adherence, exercise behaviors, activities of daily living (ADLs), and safe home environment] were secondary because CRs received the effects of the OHRC through their CGs.
The Recovery Process for Hip Fracture
To provide effective care to hip fracture patients, CGs must understand the recovery process for hip fractures, which usually transitions quickly through the care delivery system. Many older adult hip fracture patients are at high risk for medical complications due to their preexisting illnesses (Duthie et al., 2007). The average length of hospital stay for hip fracture, however, has decreased from 20.1 days in 1981 to 6.5 days in 2003. In this study, most patients who did not have medical complications were discharged from the acute hospital within 3 days. This shorter length of stay results in more patients being discharged “sicker and quicker” (Centers for Disease Control and Prevention, 2005), increasing the burden to CGs.
Rehabilitation progress for hip fracture varies depending on each individual’s health condition. If the patient’s condition allows, physical therapy usually begins within 1 to 3 days after surgery (Chudyk, Jutai, Petrella, & Speechley, 2009; Koval, Chen, Aharonoff, Egol, & Zuckerman, 2004). Once a patient meets certain discharge criteria, he or she is discharged to one of the following: home with home care, a subacute place for rehabilitation therapy (e.g., rehabilitation center, subacute unit), or a nursing home. Prior findings showed that approximately 7% to 10% of hip fracture patients go home directly with home physical therapy; 5% to 13% go to nursing homes for a prolonged stay; and the rest go to rehabilitation facilities for a short stay before they go home (Khasraghi, Christmas, Lee, Mears, & Wenz, 2005; Koval et al., 2004). The time spent in rehabilitation varies based on the patient’s condition; however, the patient usually stays 10 to 15 days (based on in-house data from two rehabilitation facilities in Baltimore).
Caregiving to Older Adult Hip Fracture Patients
In a previous qualitative study (Nahm et al., 2010), 10 CGs of older adult hip fracture patients were interviewed twice over the first 6 months after hip fracture. The majority of CGs reported exhaustion from caregiving tasks, frustration with communication issues in the healthcare delivery system, and a lack of information about how to provide care to their loved ones. In another study of 230 CGs of hip fracture patients, participants reported the highest stress at 2 months due to the increased care demand and care cost (Magaziner et al., 2000). Caregiving, however, also has been perceived as an opportunity for renewing the bond between the CG and CR (Nahm et al., 2010; Shawler, 2006). Through the caregiving situation, they had an opportunity to get reacquainted with each other, and CGs became advocates for their CRs.
Caregiving is a dyadic process involving both the CG and the CR, and a few studies have shown the effectiveness of CG support programs on health outcomes of CRs (Gitlin, Hauck, Dennis, & Winter, 2005; Shyu et al., 2010; Wolff & Kasper, 2004). In a study (n = 255) of the CGs of Alzheimer’s patients, researchers assessed the effects of a home environment skill-building program on CG-CR dyads; there was a significant improvement in CGs’ caregiving skills and a reduction in CRs’ behavioral problems (e.g., aggressive behaviors, arguing; Gitlin et al., 2005). Another study with 420 older adults receiving informal care showed that participants whose CGs felt competent in their roles were 48% less likely to have a delayed hospital discharge (Wolff & Kasper, 2004). However, there have been few studies to investigate the effects of CG training on functional recovery or health behaviors of hip fracture patients.
Online Resource Sites for Caregivers
Currently, many health websites are available for CGs (Kernisan et al., 2010). These programs provide health information needed for care, emotional support, or both. Prior studies have demonstrated the effectiveness of technology-based interventions for the CGs of Alzheimer’s patients. These programs include Resources for Enhancing Alzheimer’s Caregiver Health (REACH; Epidemiology Data Center University of Pittsburgh, 2011) and the Comprehensive Health Enhancement Support System (CHESS™; University of Wisconsin-Madison, 2011). Most of these sites, however, are focused on chronic or debilitating illnesses.
Application of Theories to Online Resource Sites
Based on the stress, appraisal, and coping theory, when a situation is appraised as a challenge, people use two types of coping mechanisms: problem-focused and emotion-focused. The first uses available resources to resolve the problem, and the latter aims to reduce stress. The OHRC was developed to provide CGs with the anticipatory knowledge and skills that they need to manage upcoming caregiving situations and cope with the potential challenges. In particular, the discussion board component of the OHRC has shown to serve as an excellent medium to provide emotional support (Nahm, Resnick, & Brothemakle, 2009; Temesgen, Knappe-Langworthy, St. Marie, Smith, & Dierkhising, 2006).
Self-efficacy and outcome expectations-based interventions can affect individuals’ health behaviors (Resnick et al., 2007; Rhodes & Fiala, 2009). Individuals’ self-efficacy beliefs can be improved through the following four mechanisms (Bandura 1997, 1998): (a) enactive mastery experience (i.e., through prior successful behavioral accomplishments); (b) vicarious experiences (i.e., through modeling others’ successful performances); (c) verbal persuasion (i.e., through verbal encouragement); and (d) physiological and emotional states (i.e., through enhancing physical states and reducing emotional stress). Outcome expectations are the beliefs that a certain consequence will be produced by personal actions (Bandura 1997, 1998). In the OHRC, a two-tiered approach was used in applying self-efficacy and outcome expectations theory to the study. Using various components, the OHRC was designed to strengthen CRs’ confidence in caregiving-related tasks and to educate CGs in how to help CRs strengthen their confidence and beliefs related to engaging in physical activities and other health behaviors throughout the recovery process (Table 1).
Table 1.
Application of Theories to the OHRC
| Underpinning Theories | Application in Online Hip Fracture Resource Center | |
|---|---|---|
| SAC | Problem-focused coping | Anticipatory knowledge and skills necessary to take care of hip fracture patients (e.g., learning modules, hip library, Ask the Experts) |
| Emotion-focused coping | Emotional support through moderated discussions (e.g., discussion boards) Information about CGs’ psychological, social, emotional needs and methods to meet their needs (e.g., learning modules, discussion boards) |
|
| SE/OE | Outcomes expectations | Emphasize expected outcomes of care and methods to deliver outcome-oriented care (e.g., learning modules, discussion boards) |
| Self-efficacy | Mastery experience: Encourage CGs to set and monitor goals in care provision and to assist CRs in setting and monitoring their goals. Vicarious experiences: Introduce CG role models (e.g., video clips); Encourage CGs to become role models for CRs (e.g., exercise). Verbal persuasion: Provide verbal encouragement to CGs on the discussion board; Teach CGs to provide verbal encouragement to their CRs Physiological and emotional states: Provide methods to relieve stress; Provide information to assist CRs in relieving their stress, fatigue, or avoidable pain (e.g., learning modules, discussion boards) |
|
Notes. SAC = Stress, Appraisal and Coping, SE/OE = Self-Efficacy and Outcome Expectations
Methods
Design
The feasibility of the OHRC intervention was assessed by participants’ evaluation of the program and usage. The feasibility of the OHRC trial protocol was assessed by implementing the OHRC intervention using a one-group pre-post design (at baseline and 8 weeks). The OHRC was used by CGs only; however, its impact was assessed by both CG and CR outcomes.
Sample and Setting
A dyad was included only if both the CR and CG met the eligibility criteria. A CR was eligible if the person (a) was 50 years or older; (b) received hip repair surgery due to hip fracture (i.e., International Classification of Disease codes 820.0 to 820.9) within a week; and (c) was able to perform ADLs (Jette, 1980) independently before experiencing the hip fracture. A CR was excluded if the person was non-English speaking, was institutionalized at the time of the fracture, or had any of the selected serious comorbidities (e.g., myocardial infarction or stroke concurrently with the hip fracture, or schizophrenia).
A CG was eligible if the person (a) was 21 years or older; (b) was a family member, friend, or significant other who was identified by a participating CR as the person who provided the majority of assistance in personal care and household tasks during postsurgery recovery; (c) resided in Maryland; (d) had access to the Internet (e.g., at home or a library); (e) could use the Internet independently; and (f) was cognitively intact--having a Mini-Mental State Examination (MMSE) score of at least 27. A CG was excluded if the person was non-English speaking; required selected, active medical treatment (e.g., active chemotherapy, radiation therapy, or hemo/peritoneal dialysis); or depended on selected assistive devices for ambulation (e.g., scooter, walker, or wheelchair).
Upon approval from all necessary institutional review boards, participants were recruited in six hospitals (three inner city and three suburban) from July 2008 to August 2009.
Intervention
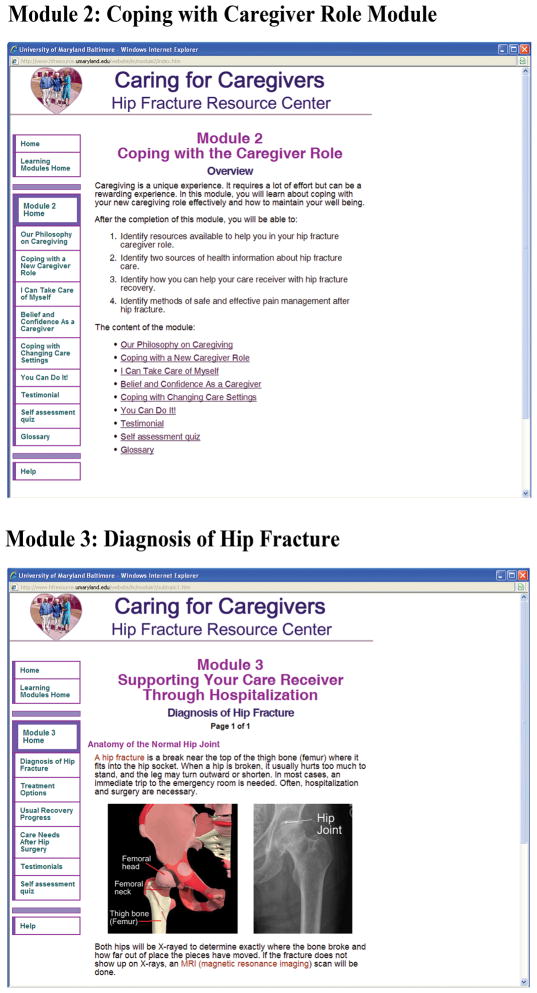
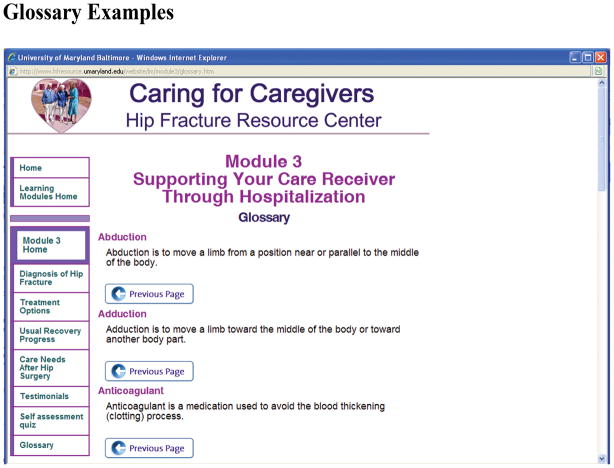
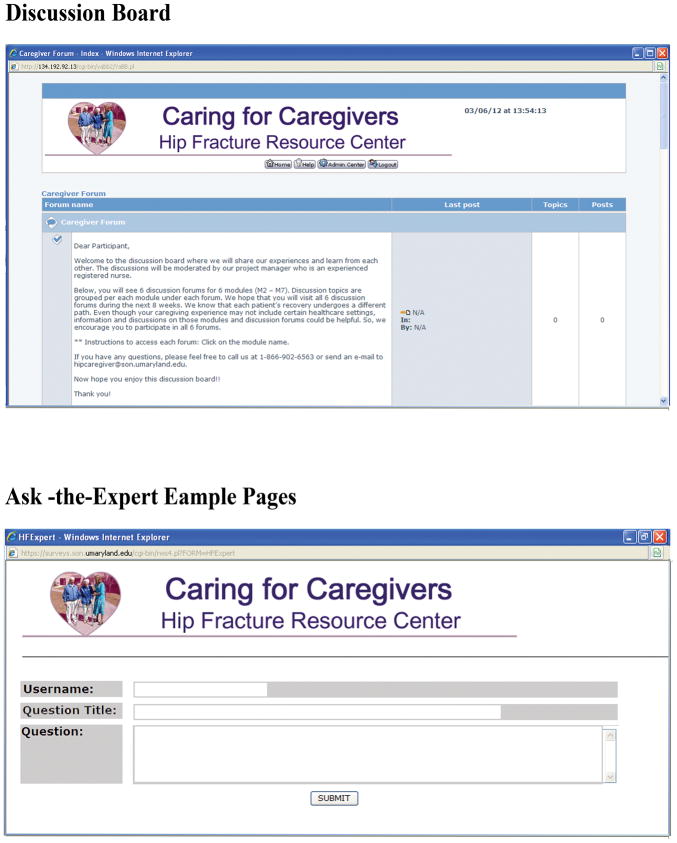
The OHRC program is an 8-week interactive online program that includes web-based learning modules, nurse-moderated discussion boards, Ask the Experts, and a virtual Hip Library (Figure 1). The content of the learning modules and virtual libraries were developed by an expert panel including a geriatrician, orthopedic surgeon, geriatric nurse practitioner, physical therapist, and social worker. The website was developed by a University of Maryland School of Nursing Research Web Development Team and stored in a secure network. The Help Desk was available via e-mail or a toll-free telephone number during business hours.
Figure 1.
Example Screen Shots
Each learning module included specific learning objectives, content, interactive self-assessment quizzes, and testimonials (Table 2). The modules were tailored to CRs’ progressive needs. During the orientation session, the project manager (PM), a nurse who had expertise in hip fracture care, and the CG participant developed a weekly course plan based on the specific caregiving needs. Out of seven modules, two (Care Needs in a Long-Term Care Facility and Care Needs in the Rehabilitation Unit) were not applicable for all participants. Each module was developed to be completed within 20 to 30 minutes. Participants were encouraged to complete all recommended modules for the first 4 to 5 weeks (one to two modules per week) and to review the modules as needed for the remaining 3 to 4 weeks. At the end of each module, participants were asked to complete self-assessment quizzes.
Table 2.
Outline of Categories and Learning Modules
| Learning Modules | Content |
|---|---|
| Coping with the CG Role | Our Philosophy on Caregiving; Coping with a New CG Role; I Can Take Care of Myself; Belief and Confidence as a CG; Coping With Changing Care Settings; You Can Do It! |
| Care Needs During Hospitalization | Diagnosis of Hip Fracture; Treatment Options for Hip Fracture: Surgery and Early Mobilization; General Recovery Progress; Care Needs After Hip Surgery |
| Care Needs in the Rehabilitation Unit Care Needs After Discharge to Home | Working With the Staff; Exercise Instructions; Using Assistive Devices; Activities of Daily Living; Pain Management; Social Support To Prepare for Recovery at Home; How to Assist Your Care Receiver; Pain Management; Fall Prevention; Safety in the Home Environment; Medication Management and Safety |
| Care Needs in a Long- Term Care Facility | Long-Term Care: Selection, Types, and Payment (including Medicare and Medicaid); Making the Transition to Nursing Home Facility Life; Methods to Help Your Loved One Make the Transition to Nursing Home Setting; Working With Care Facility Staff; Elder Rights: Long- Term Care Ombudsman Program |
| Prevention of Future Fracture | Osteoporosis; Falls and Hip Fractures; Dietary Calcium; Exercise |
Notes. Each module included objectives, testimonial, and self-assessment quizzes.
A discussion forum accompanied each learning module. The PM moderated online discussions based on social cognitive theory. Participants also could submit specific questions using an interactive online form in the Ask the Experts section. In consultation with appropriate expert panel members, the PM responded to inquiries. Additional, more in-depth information and articles recommended by experts were stored in the virtual library.
Procedures
Upon participants’ consent to the study, the research nurse interviewed the CG and CR separately using the baseline survey (participants were assured that they could stop at any time). After completion of the survey, the PM scheduled a face-to-face orientation session with the CG at the location where the CG usually accesses the Internet. During this session, the PM provided instructions on how to use the OHRC and set a course plan with the CG. The CG then used the program over an 8-week period as scheduled. At the end of the 8 weeks, the research nurse visited both the CG and CR and completed the end-of-treatment survey.
Instruments
Demographic and descriptive data
Selected demographic data were collected for both CGs and CRs; including gender, race, MMSE, marital status, educational level, and general health status. For CGs, computer or web experience and caregiving experience were assessed also. For CRs, prefracture ADLs, exercise behaviors, use of osteoporosis medications, and use of healthcare services were assessed.
Perceived usability and the usage of the intervention
Usability of the site was evaluated using the Perceived Health Web Site Usability Questionnaire (PHWUQ) and the CGs’ comments on the program. The PHWUQ includes 12 items on a 7-point Likert scale (Nahm, Resnick, & Mills, 2006). The PHWUQ is used to assess three usability dimensions: satisfaction, ease of use, and usefulness. Some evidence of the validity was indicated by comparing the results measured by the PHWUQ with those from the evaluation by usability experts. The internal consistency (calculated alpha coefficient) of the scale was .84. Participants’ usage of learning modules and discussion boards was assessed by frequency with which the program was accessed and the number of minutes using the program.
Caregiver outcome measures
The Caregiver Strain Index (CSI) is a 13-item measure with a yes/no response option (Robinson, 1983; Sullivan, 2004). Construct validity was supported by correlations with the physical and emotional health of the CG and with subjective views of the caregiving situation (Robinson, 1983). The calculated alpha coefficient in this study was .80.
The coping subscale of the 12-item Rhode Island Stress and Coping Inventory (RISCI) (Fava, Ruggiero, & Grimley, 1998) was used to assess CGs’ coping effectiveness. The original RISCI is a 12-item measure on a 5-point Likert scale that was developed to examine perceived stress (7 items) and coping (5 items). (Only the coping subscale was used because most items on the stress subscale overlap with those on the CSI.) The construct validity of the measure was evidenced by a confirmatory factor analysis (Fava et al., 1998). The calculated alpha coefficient was .89.
Social support from the OHRC was assessed using a 7-item computer-mediated social network scale (CMSNS; one item about online chat was not used) and a 9-item computer-mediated functional social support scale (CMFSSS; Nahm, Resnick, & Gaines, 2004). Some evidence of the validity was indicated by the theory-testing approach (Nahm et al., 2004). The calculated alpha coefficient was .78 and .92, respectively.
A 14-item questionnaire was developed based on the content of the learning modules. This questionnaire was then validated by two experts (a geriatrician and geriatric nurse practitioner) and pilot-tested during the usability test phase of the developmental phase. The internal consistency reliability of the measure was not as high as the other measures used in this study (calculated alpha coefficient = .57); however, this result is common with dichotomously scored learning measures.
The eHealth Literacy Scale (eHEALS; Norman & Skinner, 2006a, 2006b) is an 8-item tool developed to assess individuals’ knowledge, comfort, and perceived skills for locating, evaluating, and applying electronic health information for specific health issues. Construct validity of the scale was evidenced by principal components analysis (factor loadings ranged from .60 to .84). The calculated alpha coefficient was .89.
Completion of specific caregiving activities was assessed using a 29-item checklist developed by CG experts based upon the learning content included in this study. The list uses a yes/no/not applicable response option. The calculated alpha coefficient was .79.
Care recipient outcomes
The Self-Efficacy for Exercise (SEE) scale includes 9 items on an 11-point Likert Scale (Resnick, Wehren, & Orwig, 2003). Validity of the measure was based on efficacy expectations being related significantly to exercise activity and by the confirmatory factor analysis (Resnick & Jenkins, 2000). The calculated alpha coefficient was .88.
The original Yale Physical Activity Survey (YPAS) includes five categories of common groups of work, exercise, and recreational activities performed during a typical week. Participation in each activity (hours per week) is multiplied by an intensity code (kcal/min) and then summed over all activities (Dipietro, Caspersen, Ostfeld, & Nadel, 1993). Previously, 2-week repeatability has been demonstrated using a sample of 76 older adults, and the measure has been validated against several physiological variables (Dipietro et al., 1993).
The Self-Efficacy for Osteoporosis Medication Adherence (SEOMA) is a 14-item measure on an 11-point Likert scale (Resnick et al., 2003). Outcome Expectations for Osteoporosis Medication Adherence (OEOMA) is a 5-item scale on a 5-point Likert scale (Resnick et al., 2003). Validity of the measures was indicated through confirmatory factor analysis (Resnick et al., 2003). Calculated alpha coefficients of the SEOMA and OEOMA were .87 and .92, respectively.
The Centers for Disease Control and Prevention developed a home fall prevention checklist with 28 items on hazards found at home (e.g., unanchored throw rugs; Stevens & Olson, 2004). To assess CRs’ home environments, this checklist was converted to an instrument with a dichotomous response format (yes or no).
Data Analysis
Descriptive statistics (e.g., mean, median, range, and frequency) were computed for demographics, CGs’ caregiving and computer experiences, and CGs’ perceived usability of the OHRC. Paired t-tests were used for all outcome measures to ascertain whether changes from baseline to the EOT assessment were statistically significant. The relationship between changes in CG outcomes and CR outcomes was examined by computing Pearson product-moment correlation coefficients. Messages posted on the discussion boards were subjected to content analysis (a manuscript that described qualitative analyses and results is under development).
Results
A total of 256 hip fracture patients were identified, and among those, 164 patients were ineligible (Figure 2). Nineteen patients were discharged before eligibility status could be confirmed. The most frequent reasons for patients to be ineligible were serious comorbidities (n = 49), not having an eligible CG (n = 35), and not living in the community setting prior to the hip fracture (n = 28). Comparable CG ineligibility statistics were unavailable because CG screening was initiated only if the CR was deemed to be eligible. Among 70 potentially eligible CGs and CRs, 3 CRs did not respond to follow-up calls for the baseline interviews and 17 CGs and 12 CRs refused to participate in the study. Of the 41 eligible CG-CR dyads, 36 dyads were enrolled (5 CRs refused later due to changes in health conditions) and 27 dyads completed the follow-up survey. Most frequent withdrawal reasons were illness of the CR or other family members.
Figure 2.
Dyad Enrollment Flow
Demographics
The majority of the CGs were female (n = 18, 67%), White (n = 24, 89%), and married (n = 22, 82%) and had at least some college education (n = 20, 74%). The mean age was 55.5 ± 12.7 years. A child of the CR assumed the CG role most frequently (n = 13, 48%), followed by the CR’s spouse (n = 10, 37%). One third (n = 9, 33%) were providing care to another person in addition to the CR. More than half (n = 14, 52%) were employed either part-time or full-time. The majority of the CGs owned a computer (n = 22, 81.5%). The average years of web experience was 11.7 ± 4.8 (range = 4 to 20), and the mean time spent using the web was 12.3 ± 11.07 hours per week (range = .5 to 50 hours).
The majority of CRs were White (n = 24, 89%) and female (n = 27, 63%). The mean age was 73.96 ± 11.0 years. Seventeen CRs were married (63%), and 16 (59.3%) had received at least some college education. Six CRs (22.2%) were employed either part-time or full-time. The majority (n = 21, 77.8%) of CRs had two or more comorbidities, and 10 (37%) reported having osteoporosis. At baseline, only 6 CRs were taking osteoporosis medications that needed a prescription, and 19 (70.4%) had experienced at least one fall other than the hip fracture in the past 3 months. At follow-up, 11 participants were taking prescription osteoporosis medications. On average, CRs were receiving two home healthcare services (e.g., physical therapy, occupational therapy, homecare nurse).
Resource Center Usability and Usage
Caregivers reported the OHRC to be user-friendly, as evidenced by an average mean PHWUQ score of 74.04 ± 7.26 (range = 58–84). On average, CGs reviewed five modules and posted on the discussion board 3.1 times. The mean frequency for using the program was 11.2 (range = 1 to 42 times), and the average total time spent using the program was 132.1 ± 97.1 minutes. Many participants commented that the content was comprehensive and might be useful to others. A few participants who were familiar with the content (e.g., retired nurses) reported that learning modules served as a refresher.
Outcomes
After completion of the intervention, CGs showed a significant improvement in knowledge about caring for hip fracture patients (t = 3.17, p = .004) and eHealth literacy [t = 2.43 (26), p = .022]. Changes in computer-mediated social support and CG stress and coping were in the expected direction; however, they were not statistically significant (Table 3).
Table 3.
Changes in Caregiver Outcome Variables
| Outcomes | n | Mean (SD) | Range | t | p |
|---|---|---|---|---|---|
| Knowledge | 0–14 | 3.17 | .004 | ||
| Baseline | 27 | 9.85 (1.85) | |||
| Follow-up | 27 | 11.07 (2.04) | |||
| eHealth Literacy | 8–40 | 2.95 | .007 | ||
| Baseline | 27 | 38.89 (6.49) | |||
| Follow-up | 27 | 41.85 (6.87) | |||
| Caregiver Strain | 0–13 | 1.02 | .318 | ||
| Baseline | 27 | 6.44 (3.46) | |||
| Follow-up | 27 | 6.04 (3.62) | |||
| Stress | 5–25 | 1.63 | 0.116 | ||
| Baseline | 27 | 20.89 (3.12) | |||
| Follow-up | 27 | 21.59 (2.96) | |||
| Computer-Mediated Social Network | 7–35 | 0.61 | 0.547 | ||
| Baseline | 27 | 19.30 (7.73) | |||
| Follow-up | 27 | 19.99 (6.33) | |||
| Comp-Mediated Perceived Social Support | 9–45 | 0.26 | 0.800 | ||
| Baseline | 27 | 33.26 (9.58) | |||
| Follow-up | 27 | 33.67 (7.83) |
Notes. There were one missing item in the baseline survey and four missing items in the follow-up survey. The summed scores were calculated using mean replacement.
Caregivers reported high compliance (80–100%) for the major CG activities that were general and encouraging in nature (e.g., encouraged CR to follow the healthcare provider’s instructions, helped CR with medications, praised CR when he or she followed the prescribed exercise routine). Fewer CGs addressed their own preventive health-related activities (e.g., regular exercise) or encouraged their CRs to consume sufficient calcium and vitamin D.
Self-efficacy and outcome expectations for exercise and adherence to osteoporosis medications were improved as expected but did not demonstrate statistical significance (Table 4). Care recipients’ overall physical activity (Kcal) decreased significantly (t = 2,73, p = .01) from the month prior to hip fracture to the 8-week follow-up period. Interestingly, individuals who were more active prior to their accidents were also more active afterwards (r = .50, p = 0.01). More participants were engaged in moderate-intensity exercise (e.g., pool exercise, exercycle) at follow-up, which could have been related to the physical therapy.
Table 4.
Changes in Care Recipient Outcome Variables
| Outcomes | n | Mean (SD) | Range | t | p |
|---|---|---|---|---|---|
| Self-efficacy for exercise | 0–90 | 1.49 | .15 | ||
| Baseline | 27 | 58.59 (31.11) | |||
| Follow-up | 27 | 67.04 (23.64) | |||
| Outcome expectations for exercise | 9–45 | 0.73 | .47 | ||
| Baseline | 27 | 38.70 (4.82) | |||
| Follow-up | 27 | 39.44 (5.26) | |||
| Yale physical activity (Kcal) | 2.73 | .01 | |||
| Baseline | 27 | 5007.16 (4022.65) | |||
| Follow-up | 27 | 3081.96 (3125.37) | |||
| Yale physical activity (minutes) | 3.70 | < .01 | |||
| Baseline | 27 | 1561.69 (1112.48) | |||
| Follow-up | 27 | 957.80 (694.85) | |||
| Self- efficacy for Osteoporosis medication adherence | 14–98 | 1.54 | 0.14 | ||
| Baseline | 26 | 81.63 (16.83) | |||
| Follow-up | 26 | 85.34 (18.49) | |||
| Outcome expectations for osteoporosis medication adherence | (5–25) | 0.89 | .38 | ||
| Baseline | 27 | 12.96 (5.48) | |||
| Follow-up | 27 | 12.00 (5.28) | |||
| Environmental Safety | Index: 0–1 | 1.11 | .28 | ||
| Baseline | 27 | .6377 (.10) | |||
| Follow-up | 27 | .6657 (.12) |
Changes in CG knowledge and computer-mediated social support were correlated significantly with CRs’ self-efficacy for osteoporosis medication adherence at follow-up (r = .45, p = .02; r = .40, p = .043, respectively). Changes in CRs’ environmental safety were related to their levels of physical activities (r = .47, p = .012).
Discussion
A theory-based approach was helpful in developing and delivering an online behavioral health intervention because it served as a framework to identify content of the program, outcome variables, and how the intervention was delivered. The OHRC was found to be user-friendly (mean PHWUQ score, 74.04 ± 7.26), and the OHRC usage levels were also promising. Out of seven modules, two (Care Needs in a Long-Term Care Facility and Care Needs in the Rehabilitation Unit) were not appplicable for all participants. The average total visits to the site were 11.2 per participant and the average total time spent on the site was 132.1 ± 97.1 minutes. On average, participants viewed five modules while they were in the study.
During the study, some CRs were readmitted to the hospital for other health issues, causing their CGs to go through another stressful event. This is an important aspect in the provision of care to hip fracture patients, and this topic will be added when the OHRC if modified in a future trial.
The proposed sample size was recruited with an attrition rate (25%) lower than the projected rate (30%). The recruitment period was on schedule; however, there was a lack of eligible dyads in the hospitals located in the inner-city underserved areas. For future larger-scale trials, the recruitment hospitals may need to be stratified based on geographic locations.
Generally, the number of available CR-CG dyads is much smaller than that of individual CRs or CGs, and it took many more resources to get in contact with both the hip fracture patients and their CGs than initially planned. When the field nurse visited patients, it was often right after surgery, which necessitated a follow-up visit. Their CGs were often not present when the nurse visited participants. Those challenges were mitigated through working with clinical staff; for example, meeting with the CGs after they attended the discharge planning meeting or avoiding CRs’ therapy times.
Prior studies have shown challenges in recruiting CGs of older adults (Murphy et al., 2007; Steinhauser et al., 2006). Many CGs take on caregiving responsibilities in addition to their other obligations, and some CGs have their own health problems (Steinhauser et al., 2006). Recruitment of hip fracture patient–CG dyads in acute settings imposes additional challenges. Hip fracture patients stay in the hospital only for a few days for surgical procedures and then are transferred to another setting. This is a very busy and stressful time for the CGs, and the field research nurses must be able to make proper judgments when they approach participants. Those aspects must be discussed in field staff training, which is a vital component of successful studies (Leonard et al., 2003).
Caregivers’ knowledge about how to take care of hip fracture patients was improved significantly after completion of the OHRC (t = 3.17, p = .004). Although effectiveness of the OHRC intervention needs to be tested further, the results suggest a good potential for using the OHRC for CGs of hip fracture patients. Use of online programs can be a particularly timely and effective approach considering the increasing popularity of the Internet (80% of American adults are online; Zickuhr, 2010) and CGs’ busy schedules (51.9% had a regular job). The OHRC also can help clinicians use their time more efficiently as they can refer CGs to the OHRC for general information while they focus on more individualized and specific aspects of care.
There was a significant improvement in eHealth literacy (t = 2.43, p = .022). eHealth literacy is defined as “the ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem” (Norman & Skinner, 2006a). By improving eHealth literacy, individuals can be empowered to be more informed consumers of health care. Although the changes in the other variables (CG strain, stress, and computer-mediated social support) were in the expected direction, they were not statistically significant. Considering the small sample size, however, the findings are promising, and selected variables were found to be appropriate for future study.
Caregivers reported high compliance (80–100%) for the major CG activities that were general and encouraging in nature. Fewer CGs, however, performed activities related to caring for themselves. Considering the nature of the survey questions, social desirability response bias is a concern. The sensitivity of the items included in this survey will need to be evaluated also.
In this study, statistically significant effects on the CRs’ outcomes were not expected because of their distal position to the intervention. Rather, the main purpose of CR outcome analyses was to explore whether significant relationships exist within CR-CG dyads. Although a significant correlation was shown between the changes in CGs’ knowledge and CRs’ SEOMA and the changes in CG’s computer-mediated social support and CRs’ Self-Efficacy for Osteoporosis Medication Adherence, the impact of CG support on CR outcomes needs further investigation.
An active lifestyle is important in hip fracture recovery, as CR participants who were more active prior to the injury were also more active at follow up. More CR participants were engaged in moderate-intensity exercise (e.g., pool exercise, exercycle) at follow-up than at baseline (this could have been related to the physical therapy). This finding has important public health implications addressing the need for increased activity among older adults. Furthermore, a hip fracture event could serve as an excellent opportunity to inform older adults about the importance of exercise and changing their daily health behaviors (e.g., increasing exercise).
Limitations
This was a feasibility study for a future large scale randomized controlled trial, so the generlaizability of findings is limited. It is thought that online users tend to be more affluent. Once the intervention is proven to be effective, additional efforts must be made to implement these types of online interventions for underserved populations. Some of the strategies could include using computers in the library or at work during lunch or break times.
Conclusion
Comprehensive online CG resource programs can be beneficial to the CGs of hip fracture patients, who face the situation without much preparation. This study showed some promising findings for using the OHRC. This program is particularly timely considering the wide use of Internet technology and most CGs’ busy lives. Caregivers can obtain timely support and information at their convenience. From the clinician’s perspective, as the length of hospital stay for hip fracture is getting shorter, limited time is available for patient education during the hospital stay. By using this type of online resource program, clinicians will be able to focus on more individualized needs. During this study, specific challenges were identified in recruiting hip fracture patient–CG dyads for online studies in acute settings (e.g., complex composite eligibility criteria for the dyad, brief hospital stay, and CGs’ stress levels and busy schedules) (more detailed information about recruitment was published in Nahm et al., 2011). These findings provide helpful insights for future trials. Further studies, however, will be needed to investigate the impact of these programs on CR-CG dyads.
Figure 3.
Figure 4.
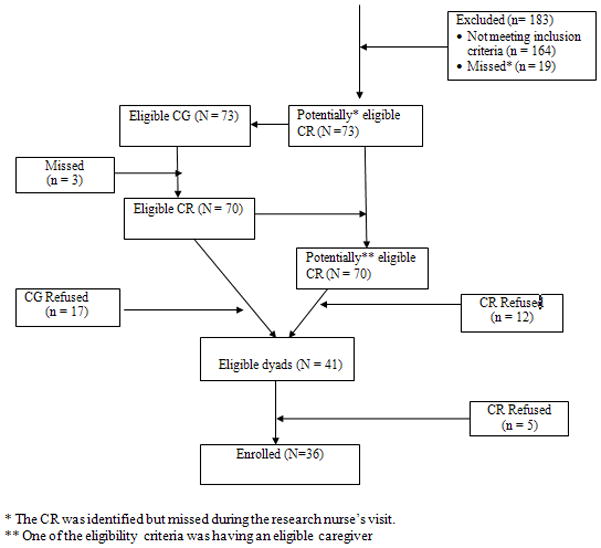
* The CR was identified but missed during the research nurse’s visit.
** One of the eligibility criteria was having an eligible caregiver
Acknowledgments
This study was supported by Grant R21 R21AG029578 from the National Institute on Aging, National Institutes of Health.
Footnotes
There are no conflicts of interest to declare.
Contributor Information
Eun-Shim Nahm, School of Nursing, University of Maryland, Baltimore, Maryland.
Barbara Resnick, School of Medicine, University of Maryland, Baltimore, Maryland.
Denise Orwig, School of Medicine, University of Maryland, Baltimore, Maryland.
Jay Magaziner, School of Medicine, University of Maryland, Baltimore, Maryland.
Michelle Bellantoni, School of Medicine, Johns Hopkins University, Baltimore, Maryland.
Robert Sterling, School of Medicine, University of Maryland, Baltimore, Maryland.
Patricia F. Brennan, University of Wisconsin-Madison, Madison, Wisconsin.
References
- Bandura A. Self-efficacy in changing societies. New York, NY: Cambridge University Press; 1997. [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology and Health. 1998;13:623–649. doi: 10.1080/08870449808407422. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. QuickStats: Average length of hospital stay for persons with hip fractures, by year--United States, 1990–2003. 2005 Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5409a4.htm.
- Centers for Disease Control and Prevention. Hip fractures among older adults. 2010 Retrieved from http://www.cdc.gov/nchs/data/nhsr/nhsr029.pdf.
- Chudyk AM, Jutai JW, Petrella RJ, Speechley M. Systematic review of hip fracture rehabilitation practices in the elderly. Archives of Physical Medicine & Rehabilitation. 2009;90:246–262. doi: 10.1016/j.apmr.2008.06.036. [DOI] [PubMed] [Google Scholar]
- Dipietro L, Caspersen CJ, Ostfeld AM, Nadel ER. A survey for assessing physical activity among older adults. Medicine and Science in Sports and Exercise. 1993;25:628–642. [PubMed] [Google Scholar]
- Duthie EH, Katz PR, Malone ML. Practice of geriatrics. Philadelphia, PA: W. B. Saunders; 2007. [Google Scholar]
- Epidemiology Data Center University of Pittsburgh. Resources for enhancing Alzheimer’s caregiver health. 2011 Retrieved from http://www.edc.gsph.pitt.edu/reach/
- Fava JL, Ruggiero L, Grimley DM. The development and structural confirmation of the Rhode Island Stress and Coping Inventory. Journal of Behavioral Medicine. 1998;21:601–611. doi: 10.1023/A:1018752813896. [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Hauck WW, Dennis MP, Winter L. Maintenance of effects of the home environmental skill-building program for family caregivers and individuals with Alzheimer’s disease and related disorders. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences. 2005;60:368–374. doi: 10.1093/gerona/60.3.368. [DOI] [PubMed] [Google Scholar]
- Jette AM. Functional status index: Reliability of a chronic disease evaluation instrument. Archives of Physical Medicine and Rehabilitation. 1980;61:395–401. [PubMed] [Google Scholar]
- Kernisan LP, Sudore RL, Knight SJ. Information-seeking at a caregiving website: A qualitative analysis. Journal of Medical Internet Research. 2010;12:e31. doi: 10.2196/jmir.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khasraghi FA, Christmas C, Lee EJ, Mears SC, Wenz JF., Sr Effectiveness of a multidisciplinary team approach to hip fracture management. Journal of Surgical Orthopaedic Advances. 2005;14:27–31. [PubMed] [Google Scholar]
- Koval KJ, Chen AL, Aharonoff GB, Egol KA, Zuckerman JD. Clinical pathway for hip fractures in the elderly: The Hospital for Joint Diseases experience. Clinical Orthopedics and Related Research. 2004;1(425):72–81. doi: 10.1097/01.blo.0000132266.59787.d2. [DOI] [PubMed] [Google Scholar]
- Leonard NR, Lester P, Rotheram-Borus MJ, Mattes K, Gwadz M, Ferns B. Successful recruitment and retention of participants in longitudinal behavioral research. AIDS Education & Prevention. 2003;15:269–281. doi: 10.1521/aeap.15.4.269.23827. [DOI] [PubMed] [Google Scholar]
- Magaziner J, Fredman L, Hawkes W, Hebel JR, Zimmerman S, Orwig DL, Wehren L. Changes in functional status attributable to Hip Fracture: A comparison of hip fracture patients to community-dwelling aged. American Journal of Epidemiology. 2003;157:1023–1031. doi: 10.1093/aje/kwg081. [DOI] [PubMed] [Google Scholar]
- Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M, Kenzora J. Recovery from hip fracture in eight areas of function. Journals of Gerontology: Series A, Biological Sciences & Medical Sciences. 2000;55:M498–507. doi: 10.1093/gerona/55.9.M498. [DOI] [PubMed] [Google Scholar]
- Murphy MR, Escamilla MI, Blackwell PH, Lucke KT, Miner-Williams D, Shaw V, Lewis SL. Assessment of caregivers’ willingness to participate in an intervention research study. Research in Nursing & Health. 2007;30:347–355. doi: 10.1002/nur.20186. [DOI] [PubMed] [Google Scholar]
- Nahm ES, Resnick B, Gaines J. Testing of the reliability and validity of the computer-mediated social support measures among older adults: A preliminary study. Computers, Informatics, Nursing: CIN. 2004;22:211–219. doi: 10.1097/00024665-200407000-00009. [DOI] [PubMed] [Google Scholar]
- Nahm ES, Resnick B, Mills ME. Development and pilot-testing of the perceived health Web site usability questionnaire (PHWSUQ) for older adults. Studies in Health Technology and Informatics. 2006;122:38–43. [PubMed] [Google Scholar]
- Nahm E-S, Resnick B, Brothemakle B. Use of discussion boards in a theory-based health website for older adults. Nursing Research. 2009;58:419–426. doi: 10.1097/NNR.0b013e3181bee6c4. [DOI] [PubMed] [Google Scholar]
- Nahm ES, Resnick B, Orwig D, Magaziner J, Degrezia M. Exploration of informal caregiving following hip fracture. Geriatric Nursing. 2010;31:254–262. doi: 10.1016/j.gerinurse.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahm E-S, Bausell B, Resnick B, Covington B, Magaziner J, Brennan PF, Mathews R, Park J-H. Online Research in Older Adults: Lessons Learned From Conducting an Online Randomized Controlled Trial. Applied Nursing Research. 2011;24:269–275. doi: 10.1007/s12126-011-9128-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman CD, Skinner HA. eHEALS: The eHealth Literacy Scale. Journal of Medical Internet Research. 2006a;8:e27. doi: 10.2196/jmir.8.4.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman CD, Skinner HA. eHealth literacy: Essential skills for consumer health in a networked world. Journal of Medical Internet Research. 2006b;8:e9. doi: 10.2196/jmir.8.2.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orwig DL, Hochberg M, Yu-Yahiro J, Resnick B, Hawkes WG, Shardell M, Magaziner J. Delivery and outcomes of a yearlong home exercise program after hip fracture: A randomized controlled trial. Archives of Internal Medicine. 2011;171:323–331. doi: 10.1001/archinternmed.2011.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick B, Jenkins LS. Testing the reliability and validity of the Self-Efficacy for Exercise scale. Nursing Research. 2000;49:154–159. doi: 10.1097/00006199-200005000-00007. [DOI] [PubMed] [Google Scholar]
- Resnick B, Orwig D, Yu-Yahiro J, Hawkes W, Shardell M, Hebel JR, Magaziner J. Testing the effectiveness of the exercise plus program in older women post-hip fracture. Annals of Behavioral Medicine. 2007;34:67–76. doi: 10.1080/08836610701495367. [DOI] [PubMed] [Google Scholar]
- Resnick B, Wehren L, Orwig D. Reliability and validity of the Self-Efficacy and Outcome Exectations for Osteoporosis Medication Adherence Scales. Orthopaedic Nursing. 2003;22:139–147. doi: 10.1097/00006416-200303000-00012. [DOI] [PubMed] [Google Scholar]
- Rhodes RE, Fiala B. Building motivation and sustainability into the prescription and recommendations for physical activity and exercise therapy: The evidence. Physiotherapy Theory and Practice. 2009;25:424–441. doi: 10.1080/09593980902835344. [DOI] [PubMed] [Google Scholar]
- Robinson BC. Validation of a Caregiver Strain Index. Journal of Gerontology. 1983;38:344–348. doi: 10.1093/geronj/38.3.344. [DOI] [PubMed] [Google Scholar]
- Roth T, Kammerlander C, Gosch M, Luger TJ, Blauth M. Outcome in geriatric fracture patients and how it can be improved. Osteoporosis international. 2010;21(Suppl):615–619. doi: 10.1007/s00198-010-1401-4. [DOI] [PubMed] [Google Scholar]
- Shawler C. The empowerment of older mothers and daughters: Rehabilitation strategies following a hip fracture. Geriatric Nursing. 2006;27:371–377. doi: 10.1016/j.gerinurse.2006.10.014. [DOI] [PubMed] [Google Scholar]
- Shyu YI, Chen MC, Wu CC, Cheng HS. Family caregivers’ needs predict functional recovery of older care recipients after hip fracture. Journal of Advanced Nursing. 2010;66:2450–2359. doi: 10.1111/j.1365-2648.2010.05418.x. [DOI] [PubMed] [Google Scholar]
- Steinhauser KE, Clipp EC, Hays JC, Olsen M, Arnold R, Christakis NA, Tulsky JA. Identifying, recruiting, and retaining seriously-ill patients and their caregivers in longitudinal research. Palliative Medicine. 2006;20:745–754. doi: 10.1177/0269216306073112. [DOI] [PubMed] [Google Scholar]
- Stevens JA, Olson SJ. Check for safety: A home fall prevention checklist for older adults. 2004 Retrieved from http://www.cdc.gov/ncipc/pub-res/toolkit/Check%20for%20Safety%20B_W.pdf.
- Sullivan MT. Caregiver Strain Index (CSI) Dermatology Nursing. 2004;16:385–386. [Google Scholar]
- Temesgen Z, Knappe-Langworthy JE, StMarie MM, Smith BA, Dierkhising RA. Comprehensive Health Enhancement Support System (CHESS) for people with HIV infection. AIDS and Behavior. 2006;10:35–40. doi: 10.1007/s10461-005-9026-x. [DOI] [PubMed] [Google Scholar]
- University of Wisconsin-Madison. The Center for Health Enhancement Systems Studies. 2011 Retrieved from http://chess.wisc.edu/chess/projects/current_studies_and_projects.aspx.
- Wolff JL, Kasper JD. Informal caregiver characteristics and subsequent hospitalization outcomes among recipients of care. Aging-Clinical & Experimental Research. 2004;16:307–313. doi: 10.1007/BF03324556. [DOI] [PubMed] [Google Scholar]
- Zickuhr K. Generations 2010. 2010 Retrieved from http://www.pewinternet.org/Reports/2010/Generations-2010.aspx.