Abstract
Objective
A self-expanding retrievable intracranial stent, such as Solitaire AB, is useful for mechanical thrombectomy, producing novel results in the treatment of acute ischemic stroke. On the other hand, difficult situations can arise after a thrombectomy when using as in first-line treatment.
Methods
This was a retrospective, single-center study of 23 patients with an acute ischemic stroke attributable to a large artery occlusion within the first eight hours from symptom onset. The occlusion sites were the T segment in five patients, proximal middle cerebral artery in six patients, distal middle cerebral artery in three patients, vertebral and/or basilar artery in five patients, proximal internal cerebral artery in one patient and tandem in three patients. All patients underwent a mechanical thrombectomy using the Solitaire™ stent system as the first-line treatment but required additional procedures due to the unsatisfactory results of a thrombectomy.
Results
Only six patients achieved complete recanalization by a thrombectomy using the Solitaire. Permanent stent deployment after the thrombectomy was performed in ten patients. Stent and balloon angioplasty was performed after a stent-based thrombectomy in six patients. Balloon angioplasty after thrombectomy was performed in one patient.
Conclusion
Mechanical thrombectomy with the Solitaire™ stent as a first-line treatment can produce unfortunate results that will require additional procedures.
Keywords: Atherosclerosis, Intervention, Stent, Stroke, Thrombectomy
INTRODUCTION
The early recanalization of occluded vessels in acute ischemic stroke (AIS) with intravenous thrombolysis or endovascular recanalization improves the clinical outcomes and reduces mortality. Recently, intra-arterial (IA) thrombolysis and mechanical thrombectomy has advantages over intravenous (IV) treatments for proximal lesions, including a longer therapeutic window and higher recanalization rates.10),12) In particular, there is growing concern regarding the use of stents in recanalizing an occluded artery. Self-expanding stents (SES) have achieved good results in AIS and stentrievers have promoted immediate reperfusion in 80 to 90% of cases.2),3) The present review shows that a mechanical thrombectomy with a self-expanding retrievable intracranial stent (Solitaire AB; ev3, Irvine, CA) results in a high recanalization rate and low procedure-related complications.6) The unique stent-based design features of the Solitaire allow dual functionality. First, it acts as a temporary intracranial bypass providing immediate flow restoration through the thrombus, and second, it acts as a clot retriever, trapping the thrombus into its cells for removal.8) With the subjects of this study, the Solitaire AB was used in initial treatment of AIS. This study assessed the limitations of a Solitaire-assisted thrombectomy in patients with AIS.
MATERIALS AND METHODS
Patient selection
Twenty three consecutive AIS patients, who were refractory to or ineligible for the use of intravenous recombinant tissue plasminogen activator (rt-PA) and met the inclusion criteria, were treated. The inclusion criteria were aged 18 years or older, National Institute of Health Stroke Scale score (NIHSS) ≥ 8 (or lower if there was a fluctuating neurological deficit), time from symptom onset to the endovascular procedure < 8 hours, absence of multiple microbleeds in a gradient echo image of magnetic resonance (MR), and an absence of hemorrhage in the flair image of MR. All patients were evaluated by cranial computed tomography (CT) or multimodal MR, and the vessel status was assessed by MR angiography or three dimensional CT angiography immediately before the endovascular intervention. A CT scan was performed routinely at 24 hours after the treatment (or before if any neurological worsening in the NIHSS score occurred at ≥ 4 points).
Revascularization procedure
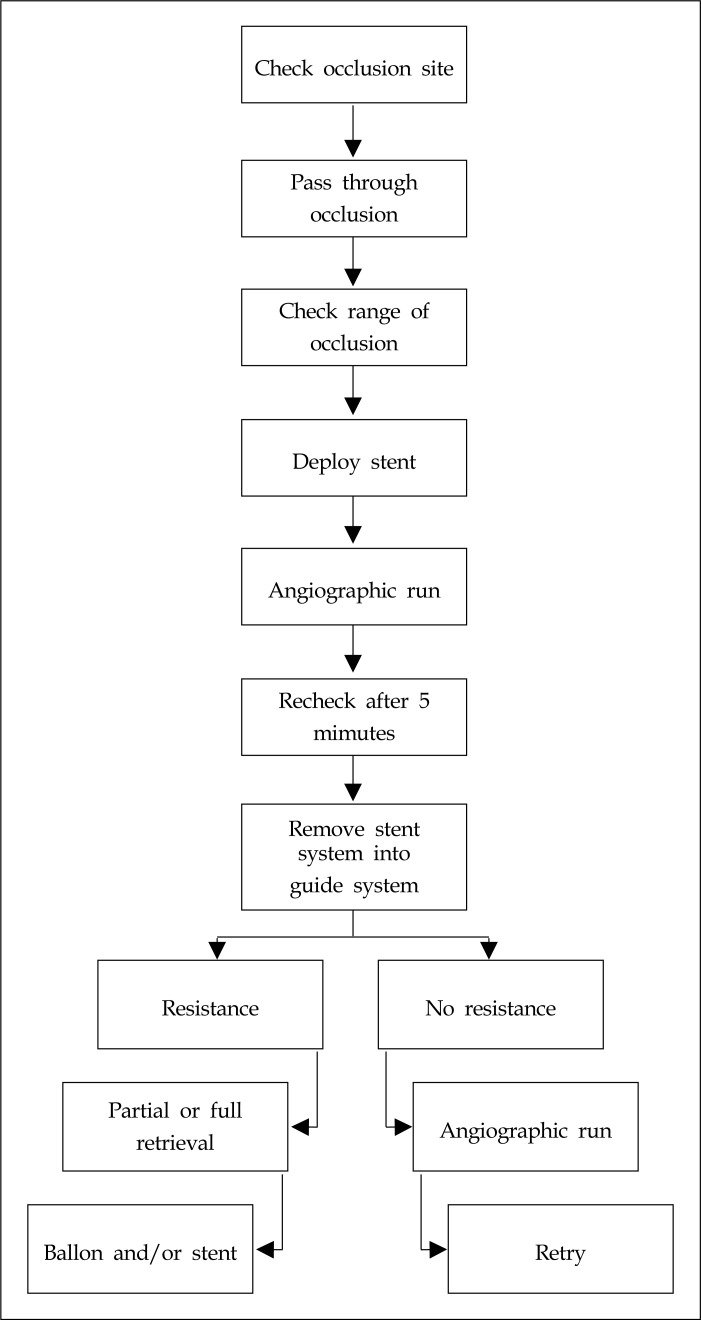
All procedures were carried out under local anesthesia using a monoplanar system (Integris V3,000, Philips, Netherlands). Using the transfemoral approach, a 6-Fr guide catheter was placed either in the proximal internal carotid artery or vertebral artery. The common carotid artery is compressed manually for proximal control. A heparinized saline solution was perfused continuously through the catheter during the procedure. The Solitaire stent system was introduced as a first-line treatment in all patients. Using a coaxial system, a Rebar 18 microcatheter (ev3) for the 4-mm Solitaire stent or a Rebar-27 microcatheter for the 6-mm Solitaire stent was advanced over a 0.014-inch guidewire placed through the thrombus. Microcatheter positioning distal to the thrombus was confirmed using a contrast injection. The stent was then advanced up to the distal tip of the microcatheter. Unsheathing resulted in half of the stent being deployed distal to the thrombus, and the other half of the stent being deployed within the thrombus. The distal marker for the microcatheter was aligned just over the proximal marker for the stent. Full deployment of the stent and flow restoration were checked by a contrast injection immediately after the stent was deployed, and the Solitaire AB was maintained in place for 5 minutes. After the flow was rechecked, the unsheathed Solitaire stent and Rebar microcatheter were removed as a system into the guide catheter while manual compression of the common carotid artery was applied. Suction through the guide catheter was performed when the unsheathed Solitaire stent came close to the distal tip of the guide catheter until the stent appeared outside of the guide system. The angiographic runs were repeated to assess the revascularization, distal emboli and vessel injury. If resistance was felt while pulling the unsheathed stent, an attempt was made to retrieve the stent or the introduction of a permanent stent deployment and balloon angioplasty were considered. The entire process was repeated up to three times if no resistance was felt. An additional procedure (balloon angioplasty and/or permanent stent insertion) was considered if flow restoration was not achieved after third trials and there was no thrombi captured in the stent (Fig. 1).
Fig. 1.
Revascularization procedure
Outcome measures
The primary outcome was the rate of vascular recanalization defined as thrombolysis in cerebral infarction (TICI) of 2b or 3.5) Functional independence was defined as modified Rankin scale (mRS) score ≤ 90 for two days, and good early neurological outcome as NIHSS score 0,1 or improvement to ≥ 10 points at day seven (or at discharge if occurred within the first week).
Statistical analysis was performed using Statistical Product and Service Solutions. A Pearson correlation index was used. A p value < 0.05 was considered significant.
RESULTS
From December 2010 to February 2012, 23 consecutive patients with AIS were treated with mechanical thrombolysis. The mean age of the patients was 66 ± 13 years, the male to female ratio was 12 to 11, the mean NIHSS score upon admission was 14 ± 4, the mean time from the onset of symptoms to femoral puncture was 3.4 ± 1.6 hours, the mean time from femoral artery puncture to flow restoration was 2.5 ± 1.14 hours, and mRS was 2 ± 2. The mean recanalization rate was 91.3% (Table 1).
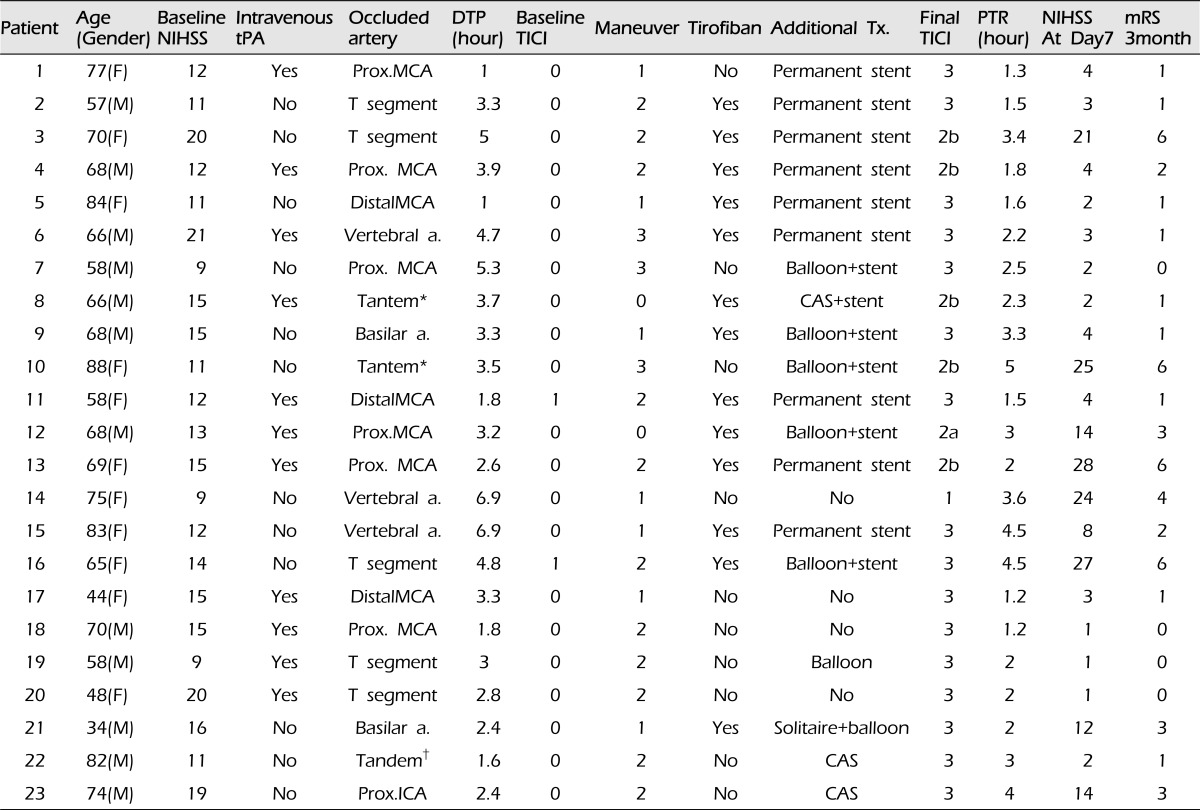
Table 1.
Characteristics of the patients
*, Carotid stenosis with "T" occlusion
†, Carotid stenosis with distal MCA occlusion.
NIHSS = National Institute of Health Stroke Scale score; tPA = tissue Plasminogen Activator; Prox = Proximal, MCA = middle cerebral artery; a = artery; ICA = internal carotid artery; TICI = thrombolysis in cerebral infarction; mRS = modified Rankin scale; additional Tx. = indicates next intervention after stent-based thrombectomy is aborted; Balloon = angioplasty; Balloon+stent = angioplasty with permanent stenting; CAS = carotid angioplasty with stent insertion; DTP = the time from hospital arrival to femoral puncture; F = female; M = male; maneuver = the number that mechanical thrombectomy with the Solitaire stent is performed; PTR = the time from femoral puncture to recanalization; Tirofiban = GP IIb/IIIa antagonist
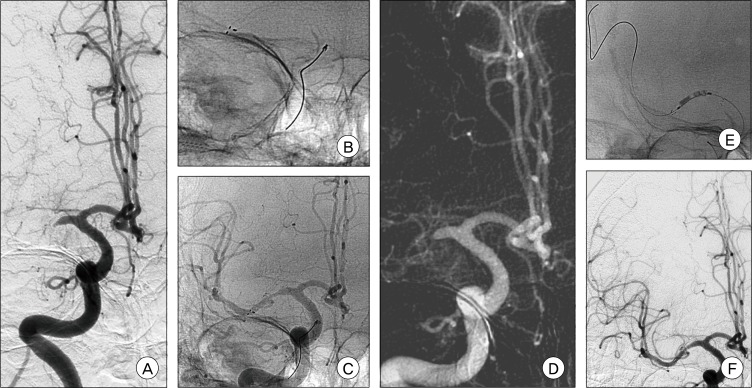
Eleven of the 23 patients received an intravenous thrombolysis using an rt-PA, and mechanical thrombolysis was performed if the NIHSS had not improved by more than 2 points. In only six out of 23 cases, the results of complete recanalization could be achieved directly by mechanical thrombectomy using a Solitaire stent (Fig. 2). The remaining patients underwent additional procedures (Fig. 3). Two of these patients who had tandem lesions, underwent an angioplasty procedure with stent insertion for carotid stenosis or occlusion. The mean number of repetitions of mechanical thrombectomy performed per procedure was two (median 2, range 0-3). The number of repetitions was determined by the resistance occurring during the retrieval or passing of the microwire or microcatheter. Flow restoration was not affected by the number of repetitions of direct mechanical thrombectomy. The procedure for complete recanalization using mechanical thrombectomy with the Solitaire AB was aborted in ten patients despite third trials of mechanical thrombectomy with the stent. With these patients, the deployment of a permanent stent was considered, and an Enterprise™ (Cordis Neurovascular, Miami, Florida) stent was used in cases where the resistance was present while retrieving the microwire or microcatheter or when they could not be passed through a severe stenotic lesion, which determined the termination of the thrombectomy trials. Flow restoration was unsatisfactory in most of these ten patients after deploying the stents. An intra-arterial GP IIb/IIIa antagonist (tirofiban) was injected in such cases. As a result, two patients presented with improved angiographic findings, and one patient presented with almost complete recanalization without the GP IIb/IIIa antagonist ten minutes after deployment. Permanent stent insertion with balloon angioplasty for recanalization was performed in six cases. Only one case showed unsuccessful recanalization because the Solitaire stent system could not be removed by the guide catheter after deployment, and even the microwire could not be passed through the occluded lesion in the stent. Four patients died from massive brain swelling with hemorrhagic formations caused by the reperfusion injuries. In one of the 23 cases, the etiology of the ischemic stroke was a thrombus in the right atrium.
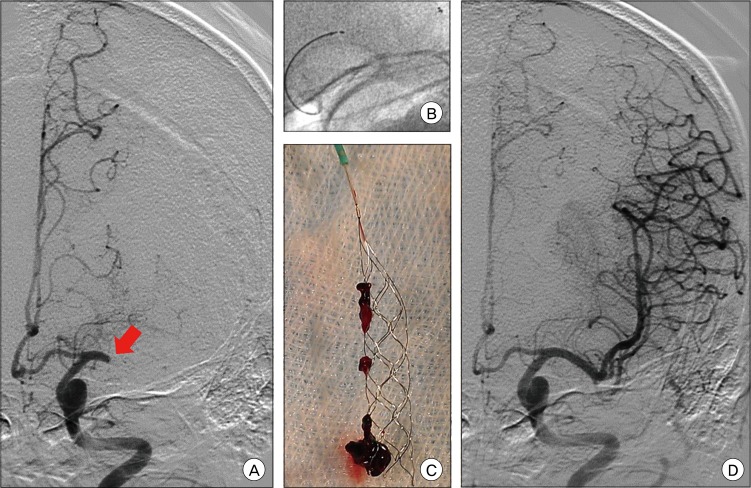
Fig. 2.
Occlusion of the middle cerebral artery. Symptom onset at 30 minutes before angiography. The National Institute of Health Stroke Scale score (NIHSS) score was 15. Antero-posterior view of a left middle cerebral artery angiogram depicts a thrombus in the proximal middle cerebral artery (arrow) (A). Solitaire AB stent deployment (B). Solitaire AB Device with a captured thrombus (C). Complete recanalization after stent retrieval. The time to recanalization was 40 minutes (D).
Fig. 3.
Occlusion of the right middle cerebral artery. Symptom onset at 12 hours before angiography. The NIHSS score was 17. Antero-posterior view of the right middle cerebral artery angiogram presents the occlusion in the proximal middle cerebral artery (A). Solitaire AB stent deployment (B), Early recanalization after stenting (C). Re-occlusion after retrieval (D). Enterprise stent deployment and balloon angioplasty (E). Complete recanalization after stenting and angioplasty (F).
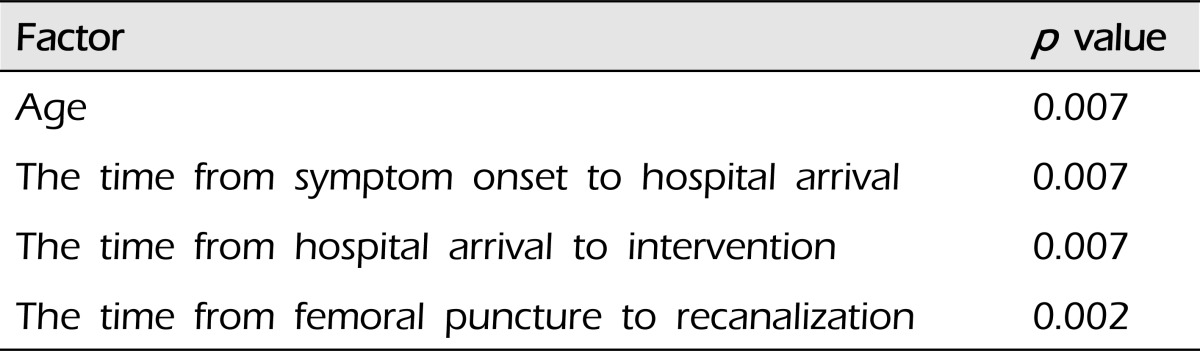
Significant results were difficult to obtain due to the small-sized study. The younger the patient was, the higher the recanalization rate. Intravenous thrombolysis did not affect the prognosis but the recanalization rate was higher in those patients who arrived at hospital and underwent a mechanical thrombectomy earlier. The time from femoral puncture to recanalization was also related to mRS (Table 2).
Table 2.
Factors affecting recanalization and the prognosis
DISCUSSION
Intracranial self-expanding microstents have been used successfully as a temporary or permanent endovascular bypass in the invasive management of AIS.7) On the other hand, stenting as a first-line treatment in AIS is debatable due to the risks associated with intracranial stent placement and the recent success of thrombectomy.4)
The aim of treatment was to revascularize the occluded vessel without stents. The Solitaire stent was first deployed, flow restoration was achieved, and a mechanical thrombectomy with the stent was performed. On the other hand, there were some limitations using Solitaire stents for mechanical thrombectomy. The first limitation was how many times the thrombectomy with stents was performed. The second shortcoming was the aborted retrieval for stents, and third was the difficult navigation after permanent stenting.
Atherosclerotic lesions can be retracted into the guide catheter with the thrombus in tow using the deployed Stent. The atherosclerotic intracranial lesion, however, resists the retracting movement. This resistance dictates what should be done in the next step. Without resistance, the same maneuver can be repeated. The number of times stent-based thrombectomy needs to be performed should be considered before considering other treatment modalities if the second attempt has failed or no thrombi removal could be achieved using the Solitaire stent. The difficulty in navigating through the occlusion site during the clot extraction maneuver increases as the maneuver is repeated. The different underlying causes of cerebral artery occlusion (e.g., cardio-embolic, arterio-arterial and veno-arterial emboli, cerebral artery stenosis, plaque or dissection) require different methods and tools for revascularization. Cardiogenic thrombi may be softer than atherosclerotic ones, and the Solitaire stent system can be superior in treating the thrombi from a cardiogenic origin.
The hard clots or calcified lesions can catch the Solitaire stent with intermingling torn thrombi with struts. Sometimes there were situations where the device could not be retrieved or the stent had to be deployed permanently. The deployment of the Solitaire stent can offer early flow restoration but not guarantee whether flow restoration is sustained. Therefore, the next step after deployment is critical. Partial resheathing of the stent facilitates device removal but decreases the likelihood of thrombi capture. In addition, it can minimize the risk of vessel trauma or device fracture.9) At times, the Solitaire stent should not be deployed and may have to be retrieved when deployed. Re-occlusion occurs in most cases of stent deployment, which explains the early re-thrombosis.11) Other negative consequences of stenting include vessel injuries secondary to stent expansion, such as dissection, inflammation, subintimal necrosis and vasospasm.1)
Only a limited number of cases have shown satisfactory outcomes in permanent stent deployment. The establishment of temporary endovascular bypass has the benefits of rapid flow restoration by displacing and disrupting the occluding clot and enhancing the efficacy of thrombolytic drugs.13)
Better outcomes are expected if the occlusion site is fully covered and thrombolysis in a cerebral infarction (TICI) is improved after ten minutes from an IA GP IIb/IIIa antagonist injection.
On the other hand, additional procedures would be very difficult to perform if re-occlusion occurs. The Solitaire stent is difficult to navigate during its deployment. In particular, atherosclerotic lesions make this process difficult. Vessel injuries can occur if a microwire or microcatheter is navigated outside the stent. In such situations, the stent with a stent delivery wire is superior to the Solitaire stent system. This type of stent produces similar results for anterior circulation lesions and posterior circulation lesions in acute ischemic stroke, whereas a Solitaire stent does not. This is because the basilar artery is straight and the middle cerebral artery is tortuous to navigate in. Navigation is easier in posterior circulation.
CONCLUSION
The Solitaire stent system is a good modality for the treatment of AIS. On the other hand, careful consideration when choosing the best treatment modalities is necessary. In hard lesions, mechanical thrombectomy using a stent may not be effective enough to remove the thrombi, and additional procedures may need to be considered. In addition, stent-based thrombectomy increases the risk of vessel injury or struggle between devices.
References
- 1.Ansari S, McConnell DJ, Azari H, Levy EI, Hoh BL, Waters MF, et al. Impact of intracranial self-expanding stents in the treatment of acute ischemic stroke: efficacy and limitations. J Neurointerv Surg. 2011 Dec;3(4):364–368. doi: 10.1136/jnis.2011.004614. [DOI] [PubMed] [Google Scholar]
- 2.Brekenfeld C, Schroth G, Mordasini P, Fischer U, Mono ML, Weck A, et al. Impact of retrievable stents on acute ischemic stroke treatment. AJNR Am J Neuroradiol. 2011 Aug;32(7):1269–1273. doi: 10.3174/ajnr.A2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castaño C, Dorado L, Guerrero C, Millán M, Gomis M, Perez de la Ossa N, et al. Mechanical thrombectomy with the solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke. 2010 Aug;41(8):1836–1840. doi: 10.1161/STROKEAHA.110.584904. [DOI] [PubMed] [Google Scholar]
- 4.Gralla J, Brekenfeld C, Mordasini P, Schroth G. Mechanical thrombolysis and stenting in acute ischemic stroke. Stroke. 2012 Jan;43(1):280–285. doi: 10.1161/STROKEAHA.111.626903. [DOI] [PubMed] [Google Scholar]
- 5.Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003 Aug;34(8):e109–e137. doi: 10.1161/01.STR.0000082721.62796.09. [DOI] [PubMed] [Google Scholar]
- 6.Koh JS, Lee SJ, Ryu CW, Kim HS. Safety and efficacy of mechanical thrombectomy with solitaire stent retrieval for acute ischemic stroke: a systematic review. Neurointervention. 2012 Feb;7(1):1–9. doi: 10.5469/neuroint.2012.7.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levy EI, Ecker RD, Horowitz MB, Gupta R, Hanel RA, Sauvageau E, et al. Stent-assisted intracranial recanalization for acute stroke; early results. Neurosurgery. 2006 Mar;58(3):458–463. doi: 10.1227/01.NEU.0000199159.32210.E4. discussion 458-63. [DOI] [PubMed] [Google Scholar]
- 8.Machi P, Costalat V, Lobotesis K, Maldonado IL, Vendrell JF, Riquelme C, et al. Solitaire FR thrombectomy system: immediate results in 56 consecutive acute ischemic stroke patients. J Neurointerv Surg. 2012 Jan;4(1):62–66. doi: 10.1136/jnis.2010.004051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miteff F, Faulder KC, Goh AC, Steinfort BS, Sue C, Harrington TJ. Mechanical thrombectomy with a self-expanding retrievable intracranial stent (Solitaire AB): experience in 26 patients with acute cerebral artery occlusion. AJNR Am J Neuroradiol. 2011 Jun-Jul;32(6):1078–1081. doi: 10.3174/ajnr.A2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nogueira RG, Smith WS MERCI and Multi MERCI Writing Committee. Safety and efficacy of endovascular thrombectomy in patients with abnormal hemostasis: pooled analysis of the MERCI and multi MERCI trials. Stroke. 2009 Feb;40(2):516–522. doi: 10.1161/STROKEAHA.108.525089. [DOI] [PubMed] [Google Scholar]
- 11.Papanagiotou P, Roth C, Walter S, Behnke S, Politi M, Fassbender K, et al. Treatment of acute cerebral artery occlusion with a fully recoverable intracranial stent: a new technique. Circulation. 2010 Jun;121(23):2605–2606. doi: 10.1161/CIRCULATIONAHA.110.948166. [DOI] [PubMed] [Google Scholar]
- 12.Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome; a meta-analysis. stroke. 2007 Mar;38(3):967–973. doi: 10.1161/01.STR.0000258112.14918.24. [DOI] [PubMed] [Google Scholar]
- 13.Stampfl S, Hartmann M, Ringleb PA, Haehnel S, Bendszus M, Rohde S. Stent Placement for flow restoration in acute ischemic stroke : a single-center experience with the Solitaire stent system. AJNR Am J Neuroradiol. 2011 Aug;32(7):1245–1248. doi: 10.3174/ajnr.A2505. [DOI] [PMC free article] [PubMed] [Google Scholar]