Abstract
Since the launching of Global Initiative, VISION 2020 “the Right to Sight” many innovative, practical and unique comprehensive eye care services provision models have evolved targeting the underserved populations in different parts of the World. At places the rapid assessment of the burden of eye diseases in confined areas or utilizing the key informants for identification of eye diseases in the communities are promoted for better planning and evidence based advocacy for getting / allocation of resources for eye care. Similarly for detection and management of diabetes related blindness, retinopathy of prematurity and avoidable blindness at primary level, the major obstacles are confronted in reaching to them in a cost effective manner and then management of the identified patients accordingly. In this regard, the concept of tele-ophthalmology model sounds to be the best solution. Whereas other models on comprehensive eye care services provision have been emphasizing on surgical output through innovative scales of economy that generate income for the program and ensure its sustainability, while guaranteeing treatment of the poorest of the poor.
Keywords: Diabetes-related blindness, diabetic retinopathy, key informant, rapid assessment of avoidable blindness, retinopathy of prematurity, tele-ophthalmology
At the half way mark into the Global Initiative, VISION 2020 “the Right to Sight”, we find that many successes have been achieved across the World.[1,2] The goal of VISION 2020 has been to provide comprehensive eye care services, and this is made possible by incorporating a variety of innovative strategies. Over the years, the learning from various models has led to an evidence-based improvement in eye care with sustained and integrated development.
The largest obstacle faced in the fight against blindness in different parts of the world is lack of access to good quality and affordable eye care services, especially in the far flung rural areas.
The successful comprehensive eye care model should be a program that targets the underserved population and emphasizes surgical output through innovative scales of economy that generate income for the program and ensure its sustainability, while guaranteeing treatment to the poorest of the poor.
There have been several new developments in terms of pilot programs and best practice models; this paper discusses some of the more promising ones.
Successful Models of Comprehensive Eye Care across the World
Evidence has been the hallmark of development, be it for national planning, advocacy or monitoring. The East Mediterranean Region (EMR) undertook several rapid assessments of avoidable blindness (RAAB) to generate valuable data for further planning in the region.
Rapid Assessment of Avoidable Blindness in the East Mediterranean Region
The EMR office of the international agency for the prevention of blindness (IAPB) is responsible for the coordination of eye care and prevention of blindness activities in 22 countries in the Middle East, North Africa, and parts of Asia. The body has ensured a coordinated regional approach to all prevention of blindness and eye care activities.
Thus with the adoption by the 65th World Health Assembly (WHA) of World Health Organization's (WHO's) action plan for the prevention of blindness in May 2009, the IAPB-EMR devised a regional approach to implement this plan.[3] The IAPB EMR adopted RAAB as well as the RAAB plus Diabetic Retinopathy (DR)[4,5] survey as a cost effective and simpler methodology to be implemented across the region to generate data on visual impairment and eye care services.
A total of 22 RAAB and 3 RAAB plus DR surveys have been conducted in 5 countries in the region to date[4,6] [Fig. 1].
Figure 1.
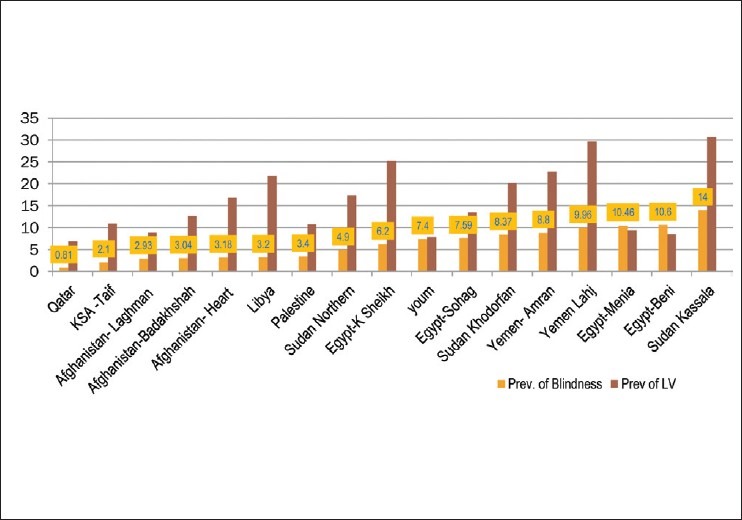
Results of RAAB Surveys conducted in 5 countries by IAPB-EMR showing prevalence of blindness and low vision
Amranand Lahj districts of Yemen
In 2009, two RAAB surveys were conducted jointly by Christoffel-Blinden mission (CBM) and the Yemeni Ministry of Health (MoH) in the Districts of Amran and Lahj. The surveys showed the prevalence of blindness to be 8.8% and 9.96% and prevalence of low vision of 22.7% and 29.6% for Amran and Lahj, respectively.[7]
These prevalence figures stimulated the MoH, CBM, and the IAPB EMR to organize evidence-based district planning workshops for these districts. Based on evidence and stakeholder participation, the MoH with the support of CBM agreed to fund the eye care plan[8] for Amran as a pilot, with the possibility of including other districts later.
Rapid assessments of avoidable blindness-diabetic retinopathy surveys in Saudi Arabia
No population-based survey on DR had ever been formally conducted in the Kingdom of Saudi Arabia despite the reports of increasing incidence of Diabetes Mellitus in the country. The IAPB EMR and the Saudi MoH conducted a RAAB-DR survey in a district of the western region in 2010, in which 3012 persons aged 50 years and older were examined.[9] The results showed a higher magnitude of DR (35%) and sight threatening diabetic retinopathy (STDR) 17.2% than that was expected.
The survey results prompted the Saudi National Committee for the Prevention of Blindness to request the MoH for more funds in order to carry out more such studies across different regions of the country. A National DR Control Committee was formed with the task of developing an action plan for the country.
Two more RAAB-DR Surveys are now in progress in the regions of Jizan and Al-Ahsa. The gathered data will be used to develop effective action plans to control diabetes-related blindness in the country with funding from the government.
Rapid assessments of avoidable blindness surveys in seven states of Sudan
The Sudanese Government and the IAPB EMR undertook RAAB surveys in 7 of the 12 states in the country. Data from these seven surveys were used to develop district eye care plans with a recalculated and revised cataract surgical rate (CSR) for each state. Kassala state was found to have one of the highest prevalence rates of blindness (14%) among the surveyed states.[10] In order to accelerate intervention in this state, the MOH and IAPB EMR developed an effective eye care plan for Kassala state[11] following which an International NonGovernmental Organization (INGO) established an eye hospital in the state.
Qatar national eye care survey
Nationwide RAAB, Glaucoma, and DR surveys were conducted in 2009. The results showed lower prevalence of blindness as 1.28% and low vision at 3.66%,[12] which was found lower than many other parts of the region, still demonstrated that the CSR was far from adequate (80%), suggesting lack of access to eye care and leading to a backlog of visual impairment.
This served as an impetus for the National Program for the prevention of blindness in Qatar to justify the inclusion of eye care in the health strategic plan for 2011–2030, which is still under development. The survey had also mobilized the government to increase eye care resources in three general hospitals across the small country.
Public Private Partnership Model in Nigeria
Nigeria has a population of 140 million[13,14] distributed across its 36 states and the Federal Capital territory of Abuja.
The Eye Foundation service delivery model
The Eye Foundation has been running a public-private community-based tripartite eye care system since 1993. This social entrepreneurship model of equitable, affordable and sustainable eye care delivery system has given the foundation a competitive edge both locally and internationally.
The private sector
The foundation's private sector activities are carried out through five private eye care hospitals outfitted with modern ophthalmic equipment. The hospitals are located at Ikeja, V. Island (Lagos), Ijebu-Imushin (Ogun State), Abuja and Calabar.
The public sector
The public sector hospitals located at Ikeja-GRA Lagos and Ijebu-Imushin (Ogun State), operate independently and have been rendering services to the less privileged along a sliding scale. Over 67% of these services are subsidized and 33% of the services are provided at no cost to patients who are unable to pay.
The community sector
The Deseret Community Vision Institute was established on January 26, 2006 in Ijebu-Imushin of Ogun State which is one of the country's 36 states. Out of 3.7 million population, 45% is urban and 55% is rural.[13,14]
The Institute's main goal was to reduce the prevalence of blindness among a million population of the Ogun east senatorial district but during the past 2 years, all the 20 local government areas of Ogun state have been covered in addition to sections of the population in neighboring states of Oyo, Ondo, Lagos, Edo, and Delta. The core mandate of this institution is human resource development and provision of high quality eye care services to the underserved [Fig. 2].
Figure 2.
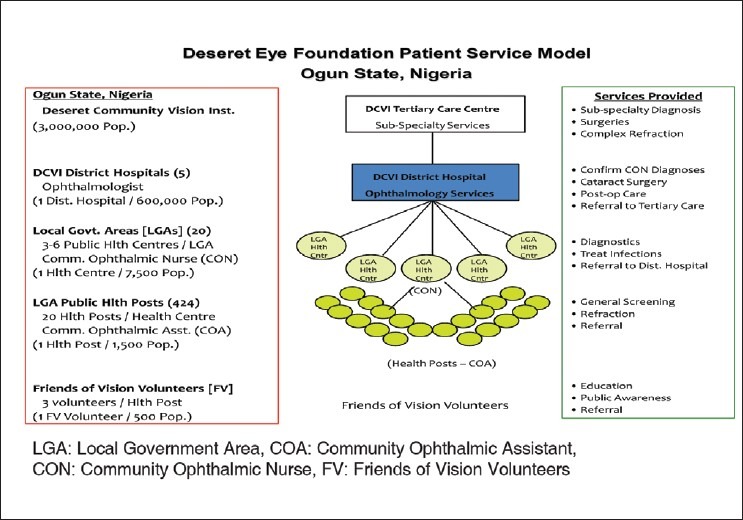
Desert Eye Foundation Service Model in Ogun State, Nigeria
The Institute's Community Outreach Program serves disadvantaged populations in all the states. The outreach is conducted free of cost with subsidy from the private sector of the eye foundation.
Eye Foundation Hospital (EFH) Group offers free eye screening and cataract surgeries. These have been mostly financed by the center and sometimes in collaboration with private and corporate bodies. The center undertakes regular visits to vision centers managed by community ophthalmic nurses to reach the rural population.
Screening in an outreach mobile clinic followed by cataract surgery at the hospital
Between 1993 and 2011, over 1.3 million persons were screened by the EFH group. Over 40,000 spectacles were provided free of cost to the poor in urban/rural areas and more than 20,000 cataract surgeries were performed [Figs. 3 and 4].
Figure 3.
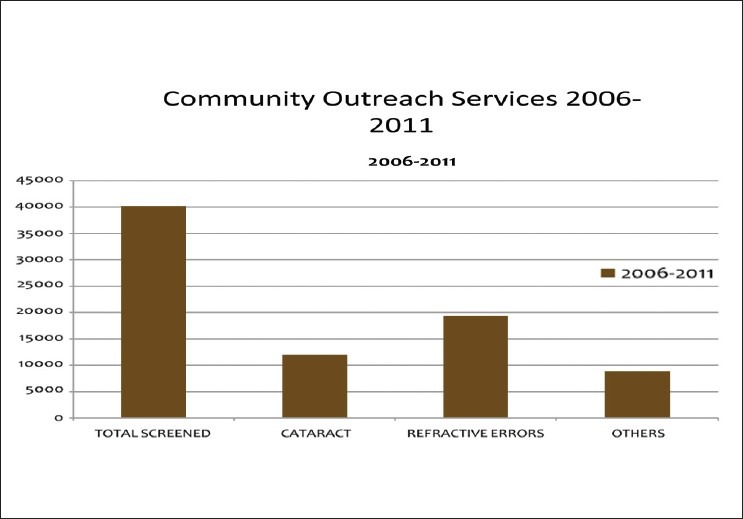
Cataract Surgical Volume of the Eye Foundation Hospital, Ogun State of Nigeria
Figure 4.
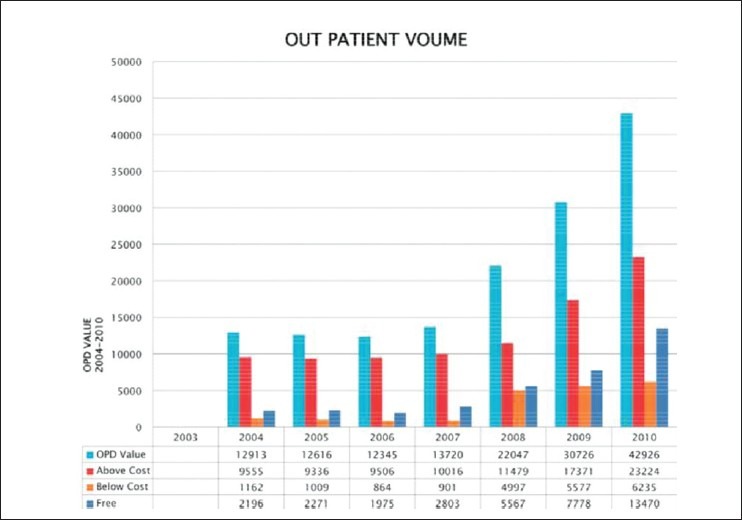
Out-Patient Attendance at the outreach and the Eye Foundation Hospital, Ogun State of Nigeria
Tele-Ophthalmology
Tele-ophthalmology has become one of the latest tools to be utilized in diagnostic and therapeutic management of eye care. India has been a pioneer in developing and applying this in ophthalmic practice. There have been several experimental models that are currently in the process of being scaled up.
Tele-ophthalmology for the control of diabetic retinopathy
Since the onset of DR is usually symptomless, most diabetic persons only present themselves for an eye examination when a complication sets in. The major barrier in the management of DR has to do with reaching diabetics in a cost effective manner and then scheduling their comprehensive eye examination every 6 months or annually as indicated by the condition.
Pilot projects were started 7 years ago when bandwidth and data transfer capabilities were limited. Thus the initial experimentation involved a large bus fitted with fundus camera, slit lamp, telemedicine equipment, and all the controls required for a V-Sat connection.
Such a bus used to go to preselected locations where diabetics would have been brought together for the screening. The vehicle staffed by an ophthalmic technician, would take fundus images and transfer them through the V-Sat link to the tertiary care facility where images would be read, graded and a report sent back immediately.
The patient was then counseled on appropriate follow-up examination scheduling or taken to an ophthalmologist immediately for clinical management. These practices helped in establishing remote diagnosis of DR thus leading to timely management of the condition. Aravind Eye Hospitals and Sankara Netralaya where this experimentation had been pioneered, were helped to a large extent by agencies like Indian Space Research Organization (ISRO) and World Diabetic Foundation (WDF).
Tele-ophthalmology in the management of retinopathy of prematurity
Worldwide roughly 10% of the births or about 13 million deliveries a year are estimated to be preterm (less than 37 weeks of gestation).[15] In India the preterm deliveries are much higher at an estimated 21%.[16] With improving neo-natal care, the survival rates of the preemies has gone up from 75% in the past to over 90% now.[17] Many of these preemies are at risk of developing Retinopathy of Prematurity (RoP). RoP is another condition which is highly amendable to image-based diagnosis, thus offering an opportunity for tele-diagnosis.
Narayana Netralaya in the State of Karnataka, India, has taken the initiative to link up with maternity centers where at-risk children assemble on a scheduled date each month. A technician with a portable RetCam captures images of the retina of these at-risk preemies and transfers these images to the tertiary care facility from where an immediate report is sent if further management is indicated. Till the end of 2010, Narayana Netralaya had screened 17,550 at-risk children, identified 3,258 cases and provided laser treatment to 392. Recognizing the importance of this initiative, the Government of Karnataka has adopted it under its Rural Health Scheme and plans to have the entire state covered within the next 3 years.[18]
Tele-ophthalmology in primary eye care
The availability of primary eye care services at a basic health post is a recent phenomenon born out of the recognition that universal coverage will become a reality only when eye care services are easily accessible and regularly available.[19] However, given the paucity, started establishing Vision Centers about 8 years ago and supported the technicians there through tele-ophthalmology. This practice has now become a mainstream strategy and Aravind Eye Hospitals has established 40 tele-ophthalmology enabled vision centers.
Eye examinations are carried out by an ophthalmic technician at the vision center, who then presents the findings in real time to the ophthalmologist at base hospital. The ophthalmologist in turn discusses with the patient, confirms the diagnosis and then writes/sends a prescription as appropriate. Patients who need surgery or advanced diagnostic procedures are given counseling to proceed to the base hospital and this account for about 9% of the 200,000 consultations done annually. This has since been replicated in the state of Tripura and by a few eye hospitals that are developing their own network of Vision Centers.
Control of Childhood Blindness in Bangladesh
Childhood blindness has been one of the major challenges right from detection to management. Epidemiological data on prevalence and causes of blindness in children is required for planning, developing, and monitoring the control programs.[20,21]
Recently efforts have been made to obtain accurate estimates of the magnitude and causes of blindness globally.[18] This information being crucial for priority setting in blindness control programs for defining strategies and monitoring change.[22]
It has been observed that the prevalence and causes of blindness in children vary widely from country to country reflecting differences in levels of socio-economic development as well as health care provision.[23] A national survey in Bangladesh in 2000 provided accurate estimates on the prevalence and causes of blindness in adults,[24] but children were not included in that survey.
Baseline research for program planning
In 2001, a large-scale study was initiated[25,26] on childhood blindness in Bangladesh.
40,000 children were found blind in Bangladesh.
12,000 children were found blind due to congenital or developmental bilateral cataract.
The Key Informant Methodology (KIM)[27] was practiced to identify and refer children who were blind in remote and rural areas of Bangladesh.
Key informant method for case-detection
Key informants (KI) are people who live or work in their local community who have a social role. Local key informants acted as volunteers for case detection after getting a short training in ‘how to recognize blindness and severe eye conditions in children’. School teachers, local council leaders, youth volunteers, Imams, and village leaders acted as key informants.
Cataract in children
In a study in Bangladesh, disorders of the lens (mainly un-operated cataract) were the single commonest cause of severe visual impairment and blindness particularly among the younger children. A qualitative study on barriers[28] showed that parents often delayed taking their child for an ophthalmic opinion. The low rates of aphakia in young children in this study also suggested that young children were not receiving cataract surgery or been lack of accessible eye care services for children.
How the findings of research have been used in developing a national program: Bangladesh Childhood Cataract Campaign
In 2004, the results of this study on barriers[28] were presented at a national workshop on planning strategies for the control of blindness in children. They recommended that primary eye care be strengthened, and tertiary services developed specifically for preschool aged children.
The Bangladesh Childhood Cataract Campaign (BCCC) was launched, key elements of this campaign included training of ophthalmologists and mid-level eye care personnel in pediatric ophthalmology, developing a health education strategy, and community-based approaches for active case finding through KIs.
Recently, an independent evaluation was accomplished on BCCC and it was concluded that the campaign was highly relevant and effective as it addressed a known public health problem in Bangladesh.
During the BCCC 32, 641 children were identified as blind and among them 10,337 children were found with cataract. Out of those blind due to cataract, 7,674 children received sight-restoring surgery. Eight pediatric eye care centers were developed in Bangladesh. The highest number of blind children was found through the KI method. The child sight foundation was developed by the research team of the above study under which 9,615 blind children were identified, and among them 3,439 children were found cataract blind.
This community linked pediatric eye care program already had a huge impact directly on thousands of blind children in Bangladesh and through the local organization of Child Sight Foundation (CSF) it will continue to create a difference in the lives of children who are blind and their families in the years to come.
Subsidization of Cataract in Latin America
Latin America (LA) is the paradox of plenty, a region rich in resources, talent, and culture, that struggles with political instability, the worst economic inequality and rural marginalization. More than 563 million people live in LA, and up to 90% of the population is urban.[29]
Cataract is the leading cause of blindness in LA (60% of individuals bilaterally blind due to cataract followed by glaucoma (15%), diabetic retinopathy (7%), corneal scarring (6%), age-related macular degeneration (6%), and refractive errors 6%.[30] Among the children, ROP is the leading cause of blindness at 28%.[30]
Coverage of eye care services is only 10% of the rural areas and surgical output is below minimum, leaving more than 60% of the region's population without access to eye care.[30]
Cataract business model in Guatemala
Guatemala is a low income Central American country with a population of 14.9 million. More than 50% of the population is below the poverty line with 13% living in extreme poverty.[31] The CSR is 800, and there is no government support or budget provided for cataract surgeries.
Visualiza[32] is a private program that was successfully implemented with donor support and financial planning to not only guarantee sustainability, but also expanding its services in Guatemala City and in the tropical sierra region of the Peten.
Dr. Mariano Yee and his brothers opened an outreach clinic in Peten in 1998 with the support of the Volunteer Optometric Service to Humanity of Pennsylvania and Lions Clubs International Foundation.
Dr. Yeewas aspired to further expand the community eye health (CEH) program incorporating a sustainable business model. After being trained at the Lions Aravind Institute in India and International Eye Foundation (IEF), they opened their new clinic in 2002 in Guatemala City.
Approximately 20% of the patients treated were private paying patients, 80% subsidized, and 10% received free treatment. The income generated by the private clinic, optical labs, eye drops, and medications covers the costs of the social clinic.
Eye health campaigns are regularly scheduled in Guatemala City and the outreach clinic in Peten to find more patients to increase output and productivity, and generating more income for the social clinic.
From 2002 to 2007 the number of patients attended grew by an impressive 344% from 6,312 to 28,040 patients. Today, Visualiza performs more than 2,000 cataract surgeries, which is more than 16% of surgical output in the country or 33% in Guatemala City.
A cataract outreach cost model in Paraguay
Paraguay is a lower-to-middle income, South American country with a population of 6.6 million. Approximately 15% of the population is aged 50 years or older and 61% of the population is urban. Approximately 19% of the population is below the poverty line.[31] The CSR is 1,351, government financially supports up to 800 cataract surgeries per yea
Fundación Visión (FV)[33] in 2010 inaugurated its new Latin American Lions Vision Institute (ILEV) in Asuncion. ILEVI hosts the regional CEH management courses with the latest teaching technology, a private and social clinic and two satellite clinics in the interior and north of Paraguay.
FV provides majority of the cataract surgeries. Most of the procedure is Manual Small Incision Cataract Surgery (SICS) and costs averagely US$300 per surgery. FV uses a rigid intra-ocular lens with a variable cost of approximately US$117. So the cost per patient can vary from around $235 to more than $352. However, the more surgeries done, the less fixed costs per surgeries are and thereby decreasing the cost of surgery to FV.
In 2011, the FV carried-out 3,700 cataract surgeries, 250 of which were financed by the state. Patients, their families, and the active fundraising department of the FV paid for rest of the surgeries. Patients also have the options to take out credit through a microcredit business that is on-site at FV. The FV adopted the Aravind sliding scales which allow them to operate on 17% of their patients for free. Up to 68% are subsidized and 15% pay all the costs.
Subsidized cataract surgery (business model in Mexico)
Mexico is a middle-income country with a population of 116.4 million. Approximately 17.4% of the population is aged 50 years or older and 78% of the population is urban.[31] The CSR in Mexico is 1,720. Additionally, a national insurance program reimburses for cataract surgery but not evenly, and rural areas in particular are still without access to basic eye care.
The national cataract program has helped increase the CSR from 1,000 to 1,720 in 2005; with the additional financial support of local foundations such as Carlos Slim's TelMex Foundation. Mexico has not yet met its CSR of 3,000 to provide adequate coverage to the population. Cataract costs are quite high. In a regional cost study, the average cost of extracapsular cataract extraction ECCE was found to be US$425 per surgery, $550 per SICS surgery, and $1,025 per phacoemulsification cataract surgery.
Instituto de la Visión (IdV)[34] (Vision Institute) in Montemorelos, Mexico is an example of successful cataract business model that combines the sliding scale of costs from Aravind with advocacy and resource mobilization from public-private partnerships.
The IdV receives additional support from private partners such as CBM, IEF, and Lions. Medical Missions International (MMI) also carries out outreach campaigns with the IdV at their satellite clinics in Tabasco and Baja California. The IdV is rendering services approximately 20% to private patients and 80% to social patients. Private and social patients are divided into four costing groups:
1st group: 10% – People with no economic resources. Their services are free.
2nd group: 20% – People with scarce economic resources. They pay a small contribution.
3rd group: 50% – People with some/medium economic resources. They receive a discount for treatment.
4th group: 20% – People with sufficient economic resources to cover the cost of their surgery. They pay 100% for their treatment.
Surgical output has increased from 3,048 in 2007 to 4,467 in 2011, and more underserved patients are helped every year by IdV. IdV also provides affordable consultancies to both their private and social patient groups with costs below the average cost per consultancy in the region and in the country. Likewise, their consultancies have (dramatically) increased from 18,378 in 2007 to 29,992 in 2011.
Coverage of eye care services is only 10% in rural areas, and surgical output is below minimum leaving more than 60% of the region's population without access to eye care.
Integrated Model for Providing Comprehensive Eye Care
L V Prasad Eye Institute (LVPEI) has created an integrated pyramidal model of eye health delivery system at primary level with appropriate linkages. The model consist of a pyramidal structure that is tiered into 5 levels with the “Vision Health Guardian” (VHG) being at the base of the pyramid and serve a population of 5,000. The next level is Vision Centre (“VC”) network, manned by a high school graduate called as a Vision Technician (“VT”). The VT is the core of this community eye care team and helps in developing horizontal and vertical linkages. The next level consists of a Secondary Centre (“SC”) that caters to a population of 500,000 and has provision of comprehensive eye care. This network of 100 VHGs, 10 VCs and 1 SC for a population of 500,000 is also known as a Village Vision Complex (“VVC”). Further functional detailing of this structure has been provided in a subsequent article by Rao and colleagues in this issue.
Conclusion
Though, many other models of service delivery exist but we have tried to give examples of some of the best ones in eye care. The RAAB survey results demonstrated the need and promoted the development of evidence-based eye care plans.
The Eye Foundation center for the prevention of blindness in Nigeria has pursued its policy of public-private partnership that has paid off. This is an example for some other developing countries to emulate because it has resulted in this center being one of the fastest growing hospitals in the world because of its sustainability.
Tele-ophthalmology has become one of the latest tools to find application in the advancement of diagnostic and therapeutic management of eye care, especially for the emerging blinding eye diseases which slowly progress, initially not giving any symptoms and so need screening at community level. India has developed this very interesting program. It was not very long before these technologies started finding applications in medicine and ophthalmology directly benefiting patient care. While it is yet to become a mainstream technology; there have been several experimental models that are currently in the process of being scaled up.
A more recent development has been to translate this experience in remote diagnosis into static facilities such as physician or specialist clinics who are predominantly managing diabetics. In addition to rapidly growing broadband network across the countries, the newer data communication technologies like 3G and 4G are making multiple connectivity options available.
This technology may be of great use where there is lack of ophthalmologists particularly in rural areas or small towns; these centers can be run by ophthalmic technicians.
National and disaggregated data on childhood blindness in Bangladesh would allow the development of an evidence-based plan of action for pediatric eye care programs, and would provide a baseline for monitoring progress and evaluation of impact. It showed that baseline data is the pre-requisite to formulate strategies for the control of blindness in children which are quite indifferent to those for adults; where specific training, expertise, equipment, a more comprehensive and multidisciplinary team approach are required.
The successful Latin American CEH model is a comprehensive eye care program that targets the underserved population and emphasizes surgical output through innovative scales of economy that generate income for the program and ensure its sustainability while guaranteeing treatment of the poorest of the poor.
The successful regional model addresses the disparity between urban and rural populations, offers outreach services and also manages satellite clinics. The three LA institutions covered in this section come from very different socio-economic environments in the region but have many common characteristics with regard to output, outreach, costs, funding, and impact.
Finally, LVPEI has created an integrated pyramidal model of eye health delivery system at primary level with appropriate linkages for the provision of comprehensive eye care to the under-served.
Acknowledgments
The author acknowledges the contributions and the efforts made by all the organizations involved in the designing and implementing different models to develop and establish sustainable programs for the delivery of comprehensive eye care services to the underserved and the program managers for their write-ups.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.World Health Organization. State of the World's Sight: VISION 2020: The Right to Sight. 1999-2005 [Google Scholar]
- 2.Prevention of Blindness and Deafness Programme. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 3.Action plan for the prevention of avoidable blindness and visual impairment 2009-2013. Geneva: World Health Organization; 2010. [Google Scholar]
- 4.Kuper H, Polack S, Limburg H. Rapid assessment of avoidable blindness. Community Eye Health. 2006;19:68–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Polack S, Yorston D, López-Ramos A, Lepe-Orta S, Baia RM, Alves L, et al. Rapid assessment of avoidable blindness and diabetic retinopathy in Chiapas, Mexico. Ophthalmology. 2012;119:1033–40. doi: 10.1016/j.ophtha.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Al-Mansouri FA, Kanaan A, Gamra H, Khandekar R, Hashim SP, Al Qahtani O, et al. Prevalence and determinants of glaucoma in citizens of Qatar aged 40 years or older: A community-based survey. Middle East Afr J Ophthalmol. 2011;18:141–9. doi: 10.4103/0974-9233.80703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rapid assessment of avoidable blindness in Amran and Lahj governorates of Yemen April-May 2009. National Program for Prevention of Blindness, General Directorate of Primary Health Care, Ministry of public health and population Sanaa [Google Scholar]
- 8.Five year district vision 2020 plan for Amran governorate Yemen, August 2009. National Program for Prevention of Blindness, General Directorate of Primary Health Care, Ministry of public health and population Sanaa [Google Scholar]
- 9.‘RAAB + DR survey in Taif governorate of Saudi Arabia’. A presentation at the Prevention of blindness session of the 2011 Saudi Ophthalmological society annual meeting March 2011, Riyadh [Google Scholar]
- 10.Results of RAAB survey in Kassala state of Sudan 2009. National Program for Prevention of Blindness. Ministry of Health Khartoum [Google Scholar]
- 11.District vision 2020 plan for Kassala state of Sudan October 2009. National Program for Prevention of Blindness. Ministry of Health Khartoum [Google Scholar]
- 12.Al Gamra H, Al Mansouri F, Khandekar R, Elshafei M, Al Qahtani O, Singh R, et al. Prevalence and causes of blindness, low vision and status of cataract in 50 years and older citizen of Qatar–a community based survey. Ophthalmic Epidemiol. 2010;17:292–300. doi: 10.3109/09286586.2010.508350. [DOI] [PubMed] [Google Scholar]
- 13.Nigeria 2006 census figure (population) [Last accessed on 2012 Jul 12]. Available from: http://www.nigeriamasterweb.com/Nigeria06censusng .
- 14.The official website of Ogun state, Nigeria. [Last accessed on 2012 Jul 12]. Available from: http://www.ogunstate.gov.ng .
- 15.Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, et al. The worldwide incidence of preterm birth: A systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88:31–8. doi: 10.2471/BLT.08.062554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh U, Singh N, Shikha S. A prospective analysis of etiology and outcome of preterm labor. Obstet Gynecol India. 2007:5748–52. [Google Scholar]
- 17. [Last accessed on 2012 Jul 12]. Available from: http://www.preemiehelp.com .
- 18.Jain R, Manikutty S. Indian institute of management, Ahmedabad; case study – Narayana Nethralaya: A precious gift to a premature child. [Last accessed on 2012 Jul 12]. Available from: http://www.narayananethralaya.org/pdf_files/iim_ahmedabad_case_study_n_kidro .
- 19.Fletcher AE, Donoghue M, Devavaran J, Thulasiraj RD, Scott S, Abdalla M, et al. Low uptake of eye services in rural India: A challenge for programs of blindness prevention. Arch Ophthalmol. 1999;117:1393–9. doi: 10.1001/archopht.117.10.1393. [DOI] [PubMed] [Google Scholar]
- 20.WHO, Global Initiative for the Elimination of Avoidable Blindness: Vision 2020. 2000. [Last accessed on 2012 Jul 12]. Available from: http://WHO/PBL/97.61 .
- 21.Gilbert C, Foster A. Blindness in children: Control priorities and research opportunities. Br J Ophthalmol. 2001;85:1025–7. doi: 10.1136/bjo.85.9.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–51. [PMC free article] [PubMed] [Google Scholar]
- 23.Foster A. Childhood blindness. Eye (Lond) 1988;2(Suppl):S27–36. doi: 10.1038/eye.1988.131. [DOI] [PubMed] [Google Scholar]
- 24.Dineen BP, Bourne RR, Ali SM, Huq DM, Johnson GJ. Prevalence and causes of blindness and visual impairment in Bangladeshi adults: Results of the national blindness and low vision survey of Bangladesh. Br J Ophthalmol. 2003;87:820–8. doi: 10.1136/bjo.87.7.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muhit MA, Shah SP, Gilbert CE, Foster A. Causes of severe visual impairment and blindness Bangladesh -a study of 1935 children. Br J Ophthalmol. 2007;91:1000–4. doi: 10.1136/bjo.2006.108019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Muhit MA, Shah SP, Gilbert CE, Hartley SD, Foster A. The key informant method - a novel means of ascertaining blind children in Bangladesh. Br J Ophthalmol. 2007;91:995–9. doi: 10.1136/bjo.2006.108027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mohammad AM. Finding children who are blind. Community Eye Health. 2007;20:30–1. [PMC free article] [PubMed] [Google Scholar]
- 28.Muhit MA. Childhood cataract: Home to hospital. Community Eye Health. 2004;17:19–22. [PMC free article] [PubMed] [Google Scholar]
- 29. [Last accessed on 2012 Jul 12]. Available from: http://www.CIA World Fact Book/ Latin America .
- 30.Vision 2020 Latin America 2011 Indicators ' Vision 2020 Latin America Training Consortium Executive Summary. [Last accessed on 2012 Mar 26]. Available from: http://www.vision2020.org/main.cfm?type=WEF&itemid=2812 .
- 31. [Last accessed on 2012 Jul 12]. Available from: http://www.CIA World Fact Book/Latin America .
- 32. [Last accessed on 2012 Jul 12]. Available from: http://www.visualiza/Latin America .
- 33. [Last accessed on 2012 Jul 12]. Available from: http://www.Fundación Visión/Latin America .
- 34. [Last accessed on 2012 Jul 12]. Available from: http://www.Instituto de la Visión/Latin America .


