Abstract
Reliable information is required for the planning and management of eye care services. While classical research methods provide reliable estimates, they are prohibitively expensive and resource intensive. Rapid assessment (RA) methods are indispensable tools in situations where data are needed quickly and where time- or cost-related factors prohibit the use of classical epidemiological surveys. These methods have been developed and field tested, and can be applied across almost the entire gamut of health care. The 1990s witnessed the emergence of RA methods in eye care for cataract, onchocerciasis, and trachoma and, more recently, the main causes of avoidable blindness and visual impairment. The important features of RA methods include the use of local resources, simplified sampling methodology, and a simple examination protocol/data collection method that can be performed by locally available personnel. The analysis is quick and easy to interpret. The entire process is inexpensive, so the survey may be repeated once every 5–10 years to assess the changing trends in disease burden. RA survey methods are typically linked with an intervention. This article provides an overview of the RA methods commonly used in eye care, and emphasizes the selection of appropriate methods based on the local need and context.
Keywords: Blindness, eye care services, planning rapid assessment methods, visual impairment
Health care in developing countries has limited resources and huge needs. These limited resources should reach those in greatest need. Rapid assessment (RA) methods are useful to prioritize the most affected regions, identify high risk groups and help develop targeted intervention for those who can benefit the most. RA methods are indispensable tools in situations where data are needed quickly and where time- or cost-related factors prohibit the use of classical epidemiological surveys. While they are not a substitute for conventional study methods, they have a wide range of applications in public health in needs analyses and monitoring interventions.[1,2] They work in tandem to plan and achieve the goal of efficient and effective health care services for all those in need.
RA methods evolved due to the perceived need of program planners and decision makers to generate baseline data and evaluate an intervention. In practice, classical surveys and rapid assessments play complementary roles. In ideal situations, classical epidemiological studies can provide the initial baseline, set up priority areas and help in developing realistic, time-bound interventions. In situations where classical surveys are not possible, RA methods can be used to plan interventions and then to evaluate the outputs and outcomes of the interventions. Because of this reason, RA methods have been rightly described as ‘striking a balance between methodologically appropriate and logistically feasible.’[3]
RA methods have been developed and field tested, covering almost the entire gamut of health care. The 1990s witnessed the emergence of RA methods in eye care for cataract, onchocerciasis, and trachoma and, more recently, the main causes of avoidable blindness and visual impairment.[4,5] In fact current global estimates of visual impairment are now derived from RA methods applied in various parts of the world.[6,7]
Principles of Rapid Assessment Methods
Even though RA methods are used with modifications in various public health contexts, certain factors are common to all of them. The problem under investigation should be of public health importance and information is a prerequisite for planning the services. The important features of RA methods include the use of local resources, simplified sampling methodology, and a short and simple examination protocol/data collection method that can be performed by locally available personnel. The analysis needs to be quick and easy to interpret. The entire process of RA is inexpensive, so that the survey can be repeated every 5–10 years to assess the changing trends in disease burden. RA surveys are typically linked with an intervention.
Sampling Methods in Rapid Assessment Studies
The Extended Program of Immunization (EPI) Random Walk method and Compact Segment (CS) sampling method are commonly used sampling methods in rapid assessment studies.
Expanded programme on immunization survey methodology
The World Health Organization's (WHO) expanded programme on immunization (EPI) is one of the earliest RA surveys to be used in health care.[8] It was a survey technique originally developed to assess immunization coverage in the United States of America and was used to monitor levels of smallpox vaccination coverage in West Africa.[9] Based on experiences from small pox eradication program, a novel method was developed at WHO for assessing vaccination coverage under the EPI.[10] These survey methods came to be known as EPI methods.[11]
The first step in EPI sampling is to obtain the census data of the survey area and list clusters with the appropriate number of households and the average number of people in each household. Clusters are randomly selected from this list.[10,12]
The second stage involves the selection of individual households in the clusters that have been randomly selected as described above. The EPI methodology recommends choosing a central location in the cluster after walking through the area. After reaching the center of a cluster, one direction is randomly selected (e.g., by spinning a bottle) and the first household is chosen for the survey. The household whose door is closest to the current household is selected next and so on. This process is continued till the required sample is obtained. This method is popularly known as EPI Random Walk method. All RA methods subsequently developed are largely modifications of the EPI method.[10,12]
Despite the popularity of the EPI survey method, it has a few limitations. The first stage sampling is done based on population proportionate to the size method based on the recent census estimates, but in developing countries the census may not be accurate and up to date and hence may not reflect the true size of the population and the demographic profile at the time of survey. A census once in ten years does not reflect the possible changes and growth rate.
The selection of the first household in the cluster in the second stage of the survey may be subject to interviewer bias. The household selection is, therefore, not truly random in a statistical sense and may introduce an unquantifiable degree of bias. Centrally located households may be different from those in the periphery of the cluster. Again, the selection of households that are close to each other could mean that there are commonalities among them. Use of a design effect can minimize this bias, but may not entirely eliminate it. Lastly, ignoring households where individuals are not available and excluding non responders can result in biased estimates, as those who have not responded may be at a higher risk or systematically different from those who have responded to the interview or were examined.[13]
Compact segment sampling
To overcome the deficiencies of the EPI method, Turner et al. proposed an improved cluster sampling method. In the first stage of this proposed method, called compact segment sampling, clusters are selected with probability proportional to size using the last population census. For the second stage of sampling, a rough map of each selected cluster, showing important landmarks, is obtained or drawn with the help of local people in the village. Based on the map, the cluster is divided into a number of segments of equal populations. All the segments are numbered; one segment is randomly chosen from the map and all households in the segment are included in the sample. This method removes subjectivity and minimizes a possible bias due to the household selection process followed in the EPI method. This compact segment sampling method also facilitates a re-visit to households when there is no response.[13]
Rapid Assessment Methods in Eye Care
With an estimated 285 million people in the world with visual impairment, including 39 million blind and 246 million with low vision, visual impairment poses a serious public health problem.[6] More so when 43% and 33% of the visual impairment is caused due to uncorrected refractive errors and cataract, respectively.[6] Studies from several parts of the world have demonstrated the adverse impact of visual impairment on the quality of life.[14–16] There is an urgent need to tackle the problem of avoidable blindness. The global program for the elimination of avoidable blindness, VISION 2020: The Right to Sight Initiative, is designed to achieve this objective.[17] Based on the magnitude of the problem and availability of cost-effective treatment methods, VISION 2020 initially prioritized five areas, including cataract, uncorrected refractive errors and low vision, childhood blindness, trachoma, and onchocerciasis.[17]
Scientifically, valid methodologies that can help in needs assessment and monitoring of output of eye care services are essential for the elimination of avoidable blindness. RA surveys have a major role to play in this context and have been developed for the assessment of cataract, trachoma, and onchocerciasis. An RA tool for avoidable blindness (RAAB) is now extensively used in various parts of the world. A Rapid Assessment method for Refractive Errors (RARE) and presbyopia has been field tested recently.[18] A protocol for presbyopia and near vision impairment has also been reported.[19]
Visual impairment in children is comparatively uncommon. The key informant approach that was devised to assess the burden of ocular morbidity in children has been successfully used in Bangladesh, Malawi, and other places for the assessment of childhood blindness.[20–23] In this method, information on children who are blind is collected from prominent people in the community who are likely to know about these children.
Rapid Assessment of Cataract Surgical Services
The Rapid Assessment of Cataract Surgical Services (RACSS) is one of the earliest RA methods developed in eye care. The RA method for cataract blindness was first reported by Venkataswamy et al. in 1989.[24] This method was developed further and software for data entry and analysis was created by Limburg et al.[25]
Cataract causes nearly 50% of the blindness across the world and is most commonly seen after the age of 50 years. By its sheer magnitude, it is a disease of great public health importance. It is universal in occurrence and relatively easy to detect in a field situation. Cataract surgery is one of the most cost-effective interventions in health care.[26] RACSS is based on sound epidemiological principles that can provide information on the prevalence of blindness due to cataract, cataract surgical coverage, and visual outcomes after cataract survey and barriers for uptake of cataract surgery in the age group ≥50 years.[25]
A random cluster sampling method similar to the EPI methodology is used with the modification that non-respondents are re-visited and, if not available after repeated visits, the basic information is collected from neighbors or other family members. The age group ≥50 years is chosen for the survey as the prevalence of cataract in them is higher, and the sample size required is considerably smaller compared with a selection of younger age groups or another disease with a lower prevalence. Cluster sizes of 40–50 are considered appropriate for the survey.[25]
The eye examination protocol consists of visual acuity assessment using the modified Snellen ‘tumbling E’ chart with 6/60 and 6/18 optotypes on either side. A torchlight examination is performed to assess the status of the crystalline lens. The fundus is examined using a direct ophthalmoscope through an undilated pupil. Individuals with visual acuity <6/18 in either eye are referred to the nearest eye care facility for further investigation and treatment.
Several survey teams work in parallel in different clusters so the fieldwork is completed in a few weeks depending on the sample size. The RACSS software is available from WHO to provide assistance at every stage of the survey–sample selection, data entry, and automated data analysis–without the need of a statistician, so as to make the whole survey process simple. Locally available staff are trained and used for the survey.
In RACSS, the eye examination is limited to a torchlight examination and as the fundus examination is done through the undilated pupil with a direct ophthalmoscope, the prevalence of cataract is easily determined but not all posterior segment disorders. Performing a fundus examination through the undilated pupil is difficult in a field situation, this difficulty is compounded if a media opacity is present. The sampling procedure has drawbacks that are inherent in the EPI methodology, such as a bias in the selection of households by using random walk method.
Despite the drawbacks, the data generated from the RACSS is useful for needs assessment and planning cataract services in a given area. When repeated at intervals of 5–10 years, RACSS can be an indispensable tool to evaluate cataract surgical services in a given area.
Rapid Assessment of Avoidable Blindness
The Rapid Assessment of Avoidable Blindness (RAAB) is a modified version of RACSS.[27] RAAB aims to provide information on the prevalence of visual impairment due to avoidable and correctable causes of vision loss like cataract, uncorrected refractive errors, trachoma, onchocerciasis, corneal scarring, and other posterior segment diseases. Similar to RACSS, it also provides information on cataract surgical coverage, major barriers to the uptake of cataract surgery, and visual outcome after surgery. Like in RACSS, RAAB covers individuals aged ≥50 years, among whom the prevalence of visual impairment is higher.[4]
RAAB uses compact segment sampling as opposed to the EPI random walk method used in RACSS.[13] The first stage involves determining the sample size and then the selection of clusters based on the ‘population proportionate to the size’ sampling method. For the second stage sampling, a map of the study clusters with important landmarks/housing groups or blocks is obtained or if not available, prepared with the help of villagers and divided into equal segments so that each segment includes the number of individuals for each cluster, usually 50 people aged ≥50 years of age. One of the segments is randomly selected and the required number of subjects is examined using the RAAB protocol. The freely available RAAB software can assist at each stage of the survey.
The examination protocol includes visual acuity assessment as in RACSS, but the examination of crystalline lens is performed by both torch and distant direct ophthalmoscopy. A slit lamp examination is done and if the subject's visual acuity is <6/18 in either eye, the is fundus examined through a dilated pupil using a direct ophthalmoscope. The initial part of the eye examination is performed by paramedical ophthalmic personnel and the latter part is performed by an ophthalmologist or an ophthalmic clinical officer.
The RAAB method overcomes the limitations of EPI methods and is hence more robust than its precursor RACSS. However, its main drawback is that ophthalmologists or ophthalmic medical officers are required for the eye examination and to diagnose eye diseases. The availability of ophthalmologists is a crucial issue in many parts of the developing world. Moreover, the diagnosis of posterior segment disease using a direct ophthalmoscope may not be very accurate and the procedure is difficult to perform in a field situation. RAAB, like its predecessor RACSS, overestimates the prevalence of cataract and the examination protocol takes much longer compared with RACSS. Still, each cluster in RAAB is completed in one day, hence the validity of the term ‘rapid’.
The definition for uncorrected refractive errors is also not based on any sound and validated definition and does not address the problem of presbyopia. In RAAB, uncorrected refractive errors is defined as ‘unable to see 6/60, but can see 6/18 when pinhole is used.’ It should be noted that only two optotypes of 6/60 and 6/18 are used. Similar definitions are used in many studies. The other information that is specific to uncorrected refractive errors like spectacle coverage is also not provided by RAAB.
The barriers data derived from RAAB relates to uptake of eye care services for cataract like RACSS. Besides, RAAB focuses on individuals aged 50 years and above and thus misses the data on younger age groups, although the data on ≥50 years age may be useful for planning eye care services.[4] Recently, a novel approach where an examination to detect diabetic retinopathy has been added to the RAAB methodology has been tried successfully in Mexico and holds promise for replication to other areas.[28]
Rapid Assessment of Refractive Errors
Rapid Assessment of Refractive Errors (RARE) is used to assess the prevalence of uncorrected refractive errors, presbyopia, spectacle coverage, and barriers to uptake of services for refractive errors and presbyopia.[18,29] RARE is a methodology developed with a focus on uncorrected refractive errors and presbyopia. Typically, younger age groups, 15–49 years are selected for the survey, as refractive errors are a common cause of visual impairment in this age group.
Rapid Assessment of Visual Impairment
The Rapid Assessment of Visual Impairment (RAVI) is a hybrid RA method evolved from RACSS and RARE. It is used to estimate the prevalence and common causes of visual impairment, prevalence of presbyopia, spectacle coverage, cataract surgical coverage, visual outcomes after cataract surgery, and barriers to the uptake of eye care services.[5] The sampling protocol is similar to that employed in RACSS and the EPI random walk method. The examination protocol consists of visual acuity assessment with and without pinhole and near vision assessment. A standard Snellen chart is used instead of the simplified Snellen chart with only 6/18 and 6/60 optotypes. In contrast to RACSS and RAAB, individuals aged ≥40 years are enrolled, which increases the sample size, as the prevalence of visual impairment in younger age groups is relatively low. The inherent drawback of overestimation of cataract in RAVI protocol remains, as posterior segment examination is not performed. Increase in sample size may impact the use of resources but may not be significant considering the nature of the survey.
Trachoma Rapid Assessment
Trachoma is chronic conjunctivitis caused by an organism called Chlamydia trachomatis. Trachoma is classified into two phases: active inflammatory phase commonly seen in children and cicatrical phase seen in adults leading to entropion, trichiasis, corneal scarring and, ultimately, to blindness. Poor environmental sanitation, lack of facial cleanliness in children, and crowding are the main risk factors for trachoma.
Trachoma Rapid Assessment (TRA) was developed to identify and prioritize areas with a high prevalence of trachoma to plan interventions using the WHO SAFE [lid surgery (S), Antibiotics to treat the infection (A), Facial cleanliness (F), and Environmental changes (E)] strategy.[30,31] The WHO standard grading system is used to grade the presence of the stages of trachoma.[32] TRA is conducted in two phases, passive and active. In the passive phase, the information available from hospitals, clinics, and other key informants is reviewed to identify areas with high prevalence. In the active phase, the number of adults with trichiasis, children with active infection, and hygiene and environmental risk factors are assessed. For this phase, the worst section of the village is selected and 50 children aged between 1 and 9 years are examined from 15 to 20 geographically scattered households. The information provided by this method includes percentage of children with dirty faces, percentage of households more than half an hour's walk from a water source, percentage of households without functional latrines, and percentage of households situated within 20 meters of garbage or animal pens.[31] The TRA survey methodology is not based on probability sampling and is not designed to provide prevalence estimates. TRA has been conducted at several places and helps prioritize the areas for intervention.[33]
Rapid Epidemiological Mapping of Onchocerciasis and Rapid Epidemiological Assessment
Onchocerciasis is an eye and skin disease caused by the organism Onchocerca volvulus. It is transmitted to humans through the bite of a black fly (Simulium species). The organism also invades the eye and causes irreversible blindness.[34] The African Program for Onchocerciasis Control (APOC) used the Community-Directed Treatment with Ivermectin (CDTI) method for distribution of annual doses of Ivermectin. In CDTI communities take ownership for planning and implementing the Ivermectin distribution strategy. Before the mass distribution of Ivermectin, the target area is mapped using a technique called ‘Rapid Epidemiological Mapping of Onchocerciasis’ (REMO).[35] From maps, areas with environmental risk factors like free-flowing rivers are identified. Following this, a Rapid Epidemiological Assessment (REA) is conducted, which estimates the prevalence of onchocercal nodules in adult males using simple palpation. Communities with nodule prevalence of 20% and above are eligible for CDTI.
Several reports have confirmed the side-effects of overreaction to Ivermectin in individuals infected with Loa parasite.[36] A rapid assessment tool (RAPLOA) was developed to find out the prevalence and spread of Loa infection.[37] Later, REA and RAPLOA were piggy-backed in Cameroon and proved to be very successful.[37] This was the first instance of combining the two RA methods, and was found to lead to better results without using too much extra resources and time.[37] This could be a good example to emulate in other areas of eye care. Other than the applications described above, RA methods are also used in other areas of public health including nutritional blindness and micronutrient surveys.[38,39]
Selecting a Locally Relevant and Appropriate RA Method
With a plethora of RA methods being available in eye care, it is quite a challenge to select an appropriate and locally relevant method. Tables 1 and 2 provide an overview of RA methods in eye care. The selection of a method depends on several factors, including:
Table 1.
Comparison between rapid assessment of cataract surgical services, rapid assessment of avoidable blindness, rapid assessment of refractive errors, and rapid assessment of visual impairment
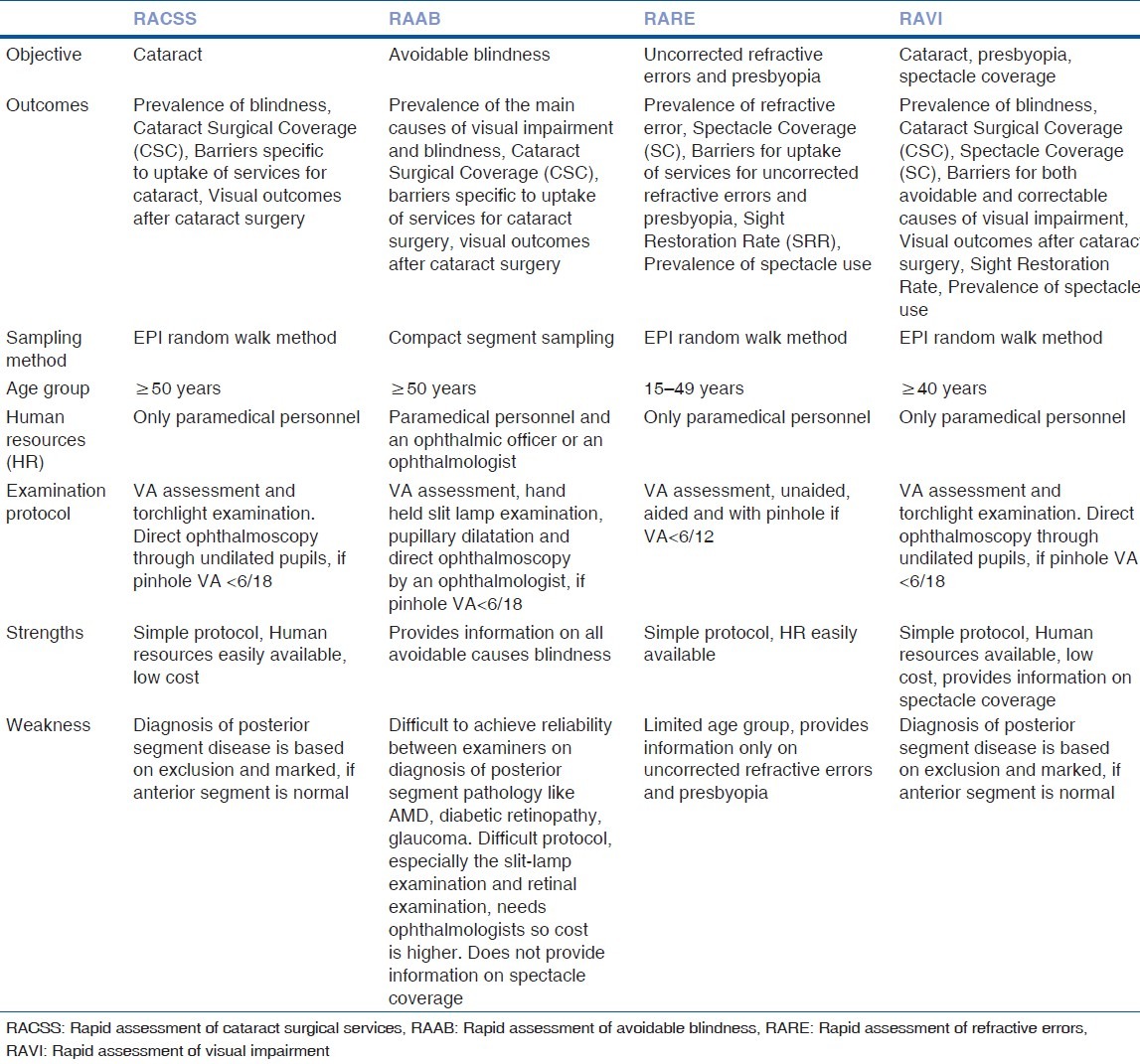
Table 2.
Relevance of rapid assessment methods in eye care
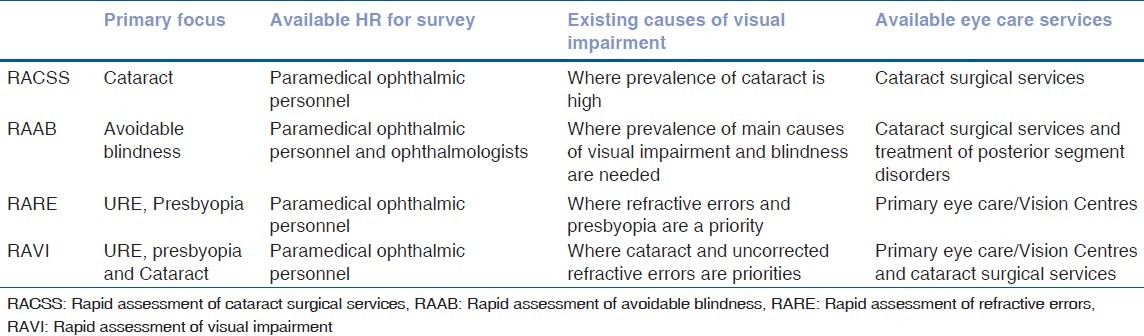
Priority causes of visual impairment
Availability of human resources
Prevalence of posterior segment disease
Availability of eye care services in the region
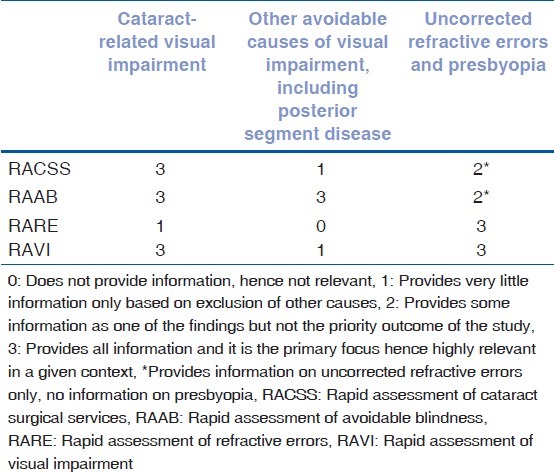
The interplay of these factors in the RA methods is presented in Table 3.
Table 3.
Relative strengths and weakness of rapid assessment methods in eye care
Ethically, no survey should be done without service provision in place for all those who need it, and this should hold true for RA methods as well. Hence availability and range of eye care services impact the selection of method. However, RA methods can also be used to establish the need for services and in such situations, RA surveys provide the evidence base to prioritize the setting up services.
RAAB would be an appropriate method where comprehensive eye care services are available or where there are plans for establishing comprehensive eye care services. In situations where only the services for cataract surgery and primary eye care services are available, doing a RACSS is preferable. Even a RAVI could be a good option and the services could be expanded to include uncorrected refractive errors and presbyopia.
In cases where there is a high prevalence of posterior segment disease, it is appropriate to use a RAAB survey, although a cross sectional survey would be ideal if resources are available. As part of the survey, eye care services can be provided for all those who need them. Where services are not available, the results are used to plan and then provide services for those in need. For example, retinal laser for all individuals who have diabetic retinopathy and need such intervention should be helped with. Where vision cannot be restored, such as in ARMD, low vision devices and appropriate rehabilitation services should be provided.
In summary, RARE and RAVI are good options as uncorrected refractive errors and cataract are priorities and services for these conditions are available in many places. Where there is a higher prevalence of posterior segment disease (including management of posterior segment disease and glaucoma), RAAB can be used with modifications to include better evaluation techniques to examine posterior segment disease as has been done in Mexico.[28]
Because of its sheer magnitude, visual impairment is a challenge, which can only be tackled with a targeted approach involving three steps–(1) Planning based on evidence and an understanding of the perceived or felt needs of the community, (2) Appropriately trained human resources or in other words ‘right people at right places,’ and (3) Mechanisms to ensure long-term sustainability. Rapid assessments offer a comprehensive package of information that can help tackle the problem of visual impairment.
It is nearly ten years since the launch of the VISION 2020 initiative, and probably time to look back and assess the achievements of this massive initiative. RA methods can play an important role in this process. Several new modes and models of community level intervention like vision centres have been introduced in different parts of the world, to reach people in need. It is now time to evaluate these models and replicate them in other places where such services are needed. RA methods can be useful tools in this endeavor.
In Oman and Timor Leste, the surveys that were repeated at different time intervals in same geographical locations have shown trends in prevalence of visual impairment.[40,41] The RA can be repeated in other areas where were they conducted previously to gauge the impact of the VISION 2020 initiative. RA methods have stood the test of time and have evolved depending on the priorities in public health. When new and low cost technology like low cost portable non mydriatic cameras, and tele-ophthalmology to evaluate posterior segment becomes more easily available, RA methods may be modified to include more difficult and emerging conditions like diabetic retinopathy, glaucoma, and age-related macular degeneration.
To conclude, RA survey methods can be one of those many stepping stones that lead to the success of VISION 2020: The global initiative to eliminate the avoidable blindness by year 2020.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.MacIntyre K. Rapid assessment and sample surveys: Trade-offs in precision and cost. Health Policy Plan. 1999;14:363–73. doi: 10.1093/heapol/14.4.363. [DOI] [PubMed] [Google Scholar]
- 2.Macintyre K, Bilsborrow RE, Olmedo C, Carrasco R. Rapid surveys for program evaluation: Design and implementation of an experiment in Ecuador. Rev Panam Salud Publica. 1999;6:192–201. doi: 10.1590/s1020-49891999000800007. [DOI] [PubMed] [Google Scholar]
- 3.Guha-Sapir D. Rapid assessment of health needs in mass emergencies: Review of current concepts and methods. World Health Stat Q. 1991;44:171–81. [PubMed] [Google Scholar]
- 4.Dineen B, Foster A, Faal H. A proposed rapid methodology to assess the prevalence and causes of blindness and visual impairment. Ophthalmic Epidemiol. 2006;13:31–4. doi: 10.1080/09286580500473787. [DOI] [PubMed] [Google Scholar]
- 5.Marmamula S, Madala SR, Rao GN. Rapid Assessment of Visual Impairment (RAVI) in marine fishing communities in South India--study protocol and main findings. BMC Ophthalmol. 2011;11:26. doi: 10.1186/1471-2415-11-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2011;96:614–8. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 7.Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86:63–70. doi: 10.2471/BLT.07.041210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Expanded Programme on Immunization (EPI) Wkly Epidemiol Rec. 1993;68:323–7. [PubMed] [Google Scholar]
- 9.Henderson RH, Davis H, Eddins DL, Foege WH. Assessment of vaccination coverage, vaccination scar rates, and smallpox scarring in five areas of West Africa. Bull World Health Organ. 1973;48:183–94. [PMC free article] [PubMed] [Google Scholar]
- 10.Bennett S, Woods T, Liyanage WM, Smith DL. A simplified general method for cluster-sample surveys of health in developing countries. World Health Stat Q. 1991;44:98–106. [PubMed] [Google Scholar]
- 11.Henderson RH, Sundaresan T. Cluster sampling to assess immunization coverage: A review of experience with a simplified sampling method. Bull World Health Organ. 1982;60:253–60. [PMC free article] [PubMed] [Google Scholar]
- 12.Lemeshow S, Robinson D. Surveys to measure programme coverage and impact: A review of the methodology used by the expanded programme on immunization. World Health Stat Q. 1985;38:65–75. [PubMed] [Google Scholar]
- 13.Turner AG, Magnani RJ, Shuaib M. A not quite as quick but much cleaner alternative to the Expanded Programme on Immunization (EPI) Cluster Survey design. Int J Epidemiol. 1996;25:198–203. doi: 10.1093/ije/25.1.198. [DOI] [PubMed] [Google Scholar]
- 14.Chia EM, Mitchell P, Ojaimi E, Rochtchina E, Wang JJ. Assessment of vision-related quality of life in an older population subsample: The Blue Mountains Eye Study. Ophthalmic Epidemiol. 2006;13:371–7. doi: 10.1080/09286580600864794. [DOI] [PubMed] [Google Scholar]
- 15.Nutheti R, Shamanna BR, Nirmalan PK, Keeffe JE, Krishnaiah S, Rao GN, et al. Impact of impaired vision and eye disease on quality of life in Andhra Pradesh. Invest Ophthalmol Vis Sci. 2006;47:4742–8. doi: 10.1167/iovs.06-0020. [DOI] [PubMed] [Google Scholar]
- 16.Wong HB, Machin D, Tan SB, Wong TY, Saw SM. Visual Impairment and Its Impact on Health-related Quality of Life in Adolescents 2009;147:505-511. Am J Ophthalmol. 2009;147:505–511.e1. doi: 10.1016/j.ajo.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 17.Global Initiative for the Elimination of Avoidable Blindness. WHO 97.61. Geneva, Switzerland: World Health Organization; 1997. WHO. [Google Scholar]
- 18.Marmamula S, Keeffe JE, Rao GN. Uncorrected refractive errors, presbyopia and spectacle coverage: Results from a Rapid Assessment of Refractive Error survey. Ophthalmic Epidemiol. 2009;16:269–74. [PubMed] [Google Scholar]
- 19.Lu Q, He W, Murthy GV, He X, Congdon N, Zhang L, et al. Presbyopia and near-vision impairment in rural northern China. Invest Ophthalmol Vis Sci. 2011;52:2300–5. doi: 10.1167/iovs.10-6569. [DOI] [PubMed] [Google Scholar]
- 20.Chakraborty S, Dutt D. Rapid assessment of childhood disabilities through key informant approach. Indian Pediatr. 2004;41:1064–6. [PubMed] [Google Scholar]
- 21.Kalua K, Patel D, Muhit M, Courtright P. Causes of blindness among children identified through village key informants in Malawi. Can J Ophthalmol. 2008;43:425–7. doi: 10.3129/i08-084. [DOI] [PubMed] [Google Scholar]
- 22.Muhit MA, Shah SP, Gilbert CE, Hartley SD, Foster A. The key informant method: A novel means of ascertaining blind children in Bangladesh. Br J Ophthalmol. 2007;91:995–9. doi: 10.1136/bjo.2006.108027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xiao B, Fan J, Deng Y, Ding Y, Muhit M, Kuper H. Using key informant method to assess the prevalence and causes of childhood blindness in Xiu′shui County, Jiangxi Province, Southeast China. Ophthalmic Epidemiol. 2011;18:30–5. doi: 10.3109/09286586.2010.528138. [DOI] [PubMed] [Google Scholar]
- 24.Venkataswamy G, Lepkowski JM, Ravilla T, Brilliant GE, Shanmugham CA, Vaidyanathan K, et al. Rapid epidemiologic assessment of cataract blindness.The Aravind Rapid Epidemiologic Assessment Staff. Int J Epidemiol. 1989;18:S60–7. doi: 10.1093/ije/18.supplement_2.s60. [DOI] [PubMed] [Google Scholar]
- 25.Limburg H, Kumar R, Indrayan A, Sundaram KR. Rapid assessment of prevalence of cataract blindness at district level. Int J Epidemiol. 1997;26:1049–54. doi: 10.1093/ije/26.5.1049. [DOI] [PubMed] [Google Scholar]
- 26.Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007;114:1670–8. doi: 10.1016/j.ophtha.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 27.Kuper H, Polack S, Limburg H. Rapid Assessment of Avoidable Blindness. Community Eye Health. 2006;19:68–9. [PMC free article] [PubMed] [Google Scholar]
- 28.Polack S, Yorston D, Lopez-Ramos A, Lepe-Orta S, Baia RM, Alves L, et al. Rapid assessment of avoidable blindness and diabetic retinopathy in Chiapas, Mexico. Ophthalmology. 2012;119:1033–40. doi: 10.1016/j.ophtha.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 29.Marmamula S, Keeffe JE, Raman U, Rao GN. Population-based cross-sectional study of barriers to utilisation of refraction services in South India: Rapid Assessment of Refractive Errors (RARE) Study. BMJ Open. 2011;1:e000172. doi: 10.1136/bmjopen-2011-000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lansingh VC, Carter MJ. Acceptance sampling rapid trachoma assessment (ASTRA) Surv Ophthalmol. 2008;53:90. doi: 10.1016/j.survophthal.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 31.Negrel AD, Mariotti SP. Trachoma rapid assessment: Rationale and basic principles. Community Eye Health. 1999;12:51–3. [PMC free article] [PubMed] [Google Scholar]
- 32.Ngondi J, Reacher M, Matthews F, Brayne C, Emerson P. Trachoma survey methods: A literature review. Bull World Health Organ. 2009;87:143–51. doi: 10.2471/BLT.07.046326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Limburg H, Bah M, Johnson GJ. Trial of the Trachoma Rapid Assessment methodology in The Gambia. Ophthalmic Epidemiol. 2001;8:73–85. doi: 10.1076/opep.8.2.73.4157. [DOI] [PubMed] [Google Scholar]
- 34.Boatin BA, Richards FO., Jr Control of onchocerciasis. Adv Parasitol. 2006;61:349–94. doi: 10.1016/S0065-308X(05)61009-3. [DOI] [PubMed] [Google Scholar]
- 35.Ngoumou P, Walsh JF, Mace JM. A rapid mapping technique for the prevalence and distribution of onchocerciasis: A Cameroon case study. Ann Trop Med Parasitol. 1994;88:463–74. doi: 10.1080/00034983.1994.11812893. [DOI] [PubMed] [Google Scholar]
- 36.Oyibo WA, Fagbenro-Beyioku AF. Adverse reactions following annual ivermectin treatment of onchocerciasis in Nigeria. Int J Infect Dis. 2003;7:156–9. doi: 10.1016/s1201-9712(03)90013-0. [DOI] [PubMed] [Google Scholar]
- 37.Wanji S, Tendongfor N, Esum M, Yundze SS, Taylor MJ, Enyong P. Combined Utilisation of Rapid Assessment Procedures for Loiasis (RAPLOA) and Onchocerciasis (REA) in Rain forest Villages of Cameroon. Filaria J. 2005;4:2. doi: 10.1186/1475-2883-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gorstein J, Shreshtra RK, Pandey S, Adhikari RK, Pradhan A. Current status of vitamin A deficiency and the National Vitamin A Control Program in Nepal: Results of the 1998 National Micronutrient Status Survey. Asia Pac J Clin Nutr. 2003;12:96–103. [PubMed] [Google Scholar]
- 39.Katz J. Sample-size implications for population-based cluster surveys of nutritional status. Am J Clin Nutr. 1995;61:155–60. doi: 10.1093/ajcn/61.1.155. [DOI] [PubMed] [Google Scholar]
- 40.Khandekar R, Mohammed AJ, Raisi AA. Prevalence and causes of blindness & low vision; before and five years after ‘VISION 2020’ initiatives in Oman: A review. Ophthalmic Epidemiol. 2007;14:9–15. doi: 10.1080/09286580600864802. [DOI] [PubMed] [Google Scholar]
- 41.Ramke J, Brian G, Naduvilath T, Lee L, Qoqonokana MQ. Prevalence and causes of blindness and low vision revisited after 5 years of eye care in Timor-Leste. Ophthalmic Epidemiol. 2012;19:52–7. doi: 10.3109/09286586.2011.645108. [DOI] [PubMed] [Google Scholar]


