Abstract
The present study used data from the Alzheimer’s Study of Emotions in Caregivers (ASEC) to evaluate perceptions of social support assessed at baseline, as well as changes in social support assessed at a follow-up eight-years later, as predictors of symptoms of change in depression, with a focus on race as a potential moderator of these relationships. Specifically, multiple regression analyses adjusted for age, sex, income, education, race, living arrangement of care recipient at baseline, death of care recipient, the cultural justification for caregiving scale (CJCS), and baseline depressive symptoms were conducted to assess baseline social support ratings, as well as the change in social support over time as a predictor of depression at follow-up—with a focus on moderation by race. Baseline social support (F(1,77) = 7.60, p=.008) was associated with fewer depressive symptoms at follow-up for all participants. The change in social support over time was also related to depressive symptoms, with effects moderated by race (F(1,77) = 7.97, p = .007), such that when support decreased over time depressive symptoms at follow-up were higher for Whites, as compared with African Americans, whereas, when social support increased over time depressive symptoms tended to be similar for both groups. These findings indicate that research designed to plan interventions in caregivers must not ignore potential racial differences with regard to the effects of caregiving on mental health.
Caregiving for a relative or loved one can be a profoundly rewarding experience, however, the duties and behaviors involved in the process may contribute to mental and physical health problems in certain individuals. Indeed, providing care for a relative with dementia or Alzheimer’s Disease is known to be one of the more common chronic stressors that middle aged and older persons face, with well known physiological consequences(Gruenewald & Seeman, 2010). According to the Alzheimer’s Association, currently almost 15 million Americans serve as caregivers and these individuals, both black and white, are at risk for exhaustion, irritability, depression, and physical health problems (www.Alz.Org). Although there is a large literature on caregiving, relatively few studies have examined longitudinal associations between social support and depressive symptoms over the extended cycle of caregiving, and fewer still have assessed differences between African American and White caregivers with respect to this association. In the only study to evaluate racial differences and change in social support over time that we are aware of, Clay et al., (2008) have shown that social support is related to decreased depressive symptoms over a five-year period, and that social support was a partial mediator of the effects of race on depressive symptoms. Thus, additional work in this area is needed to elucidate potential racial differences with respect to the importance of social support in caregivers.
As a group, black caregivers tend to report fewer depressive symptoms during the caregiving experience e.g., (Dilworth-Anderson, Williams, & Gibson, 2002; W. E. Haley & al, 1995; Pinquart & Sorensen, 2005). In a twenty year review of research on race, ethnicity, and culture in caregiving Dilworth-Anderson (Dilworth-Anderson, et al., 2002) found that a commonly held belief about black caregivers is that they are generally less distressed than their white counterparts, a finding that is particularly strong when the index of distress is depressive symptoms. One explanation offered is that blacks are more resilient, as compared to whites (W. E. Haley & al, 1995). Such findings, however, may also be a function of aspects of the caregiving experience that differ among caregivers and may also vary by race. For example, results from our own work examining racial differences in depressive symptoms has shown that black caregivers report fewer depressive symptoms, as compared to white caregivers, but only when living in a separate residence from the care recipient (Siegler, Dilworth-Anderson, Brummett, Haney, & Williams, 2010).
With regard to associations between depressive symptoms and social support, race differences may also be influenced by the cultural meanings attached to caregiving. Culture, defined as a way of life shared by members of a population group, includes values that give meaning to experience (Dilworth-Anderson, et al., 2002) and has dynamic effects across the lifespan (Jackson, Antonucci, & Brown, 2004). We have previously reported (Dilworth-Anderson et al., 2005) findings from the first study of the cultural justification for caregiving scale (CJCS: (Dilworth-Anderson, Goodwin, & Williams, 2004) that compared African American and White caregivers of dementia patients. African American, as compared to White caregivers, had higher scores on the CJCS. The Cultural Justifications for Caregiving Scale (CJCS; Dilworth-Anderson et al., 2004), the first of its kind in caregiving research, is a 10- item measure designed to assess caregivers’ cultural reasons and expectations in providing care. Responses are coded as follows: 4 strongly agree, 3 somewhat agree, 2 somewhat disagree, and 1 strongly disagrees. Items are summed, and scores may range from 10 to 40, with higher scores indicating stronger cultural reasons for giving care. In African Americans, their higher scores on the CJCS may be indicative of the long-standing cultural tradition for providing care, and this, in part, may help account for differences in depressive symptoms between White and African American caregivers. Similarly, differences in family composition that may influence which family members become caregivers (Pinquart & Sorensen, 2011) may also contribute to potential race differences.
Informed by the empirical literature on caregiving and depression, the present study used data from the Alzheimer’s Study of Emotions in Caregivers (ASEC) to evaluate perceptions of social support assessed at baseline, as well as changes in social support assessed at a follow-up eight-years later, as predictors of symptoms of depression at follow-up (adjusted for baseline depressive symptoms). We also focused on examination of race as a potential moderator of these relationships. Importantly, our study included assessment of a number of measures that have often been lacking in caregiving research protocols. Specifically, our analyses were adjusted for CJCS ratings, death of the care recipient, living arrangement at baseline, as well as age, education, and income. Results from this eight-year follow-up study extend our prior work in this area and expand upon the work conducted by other dementia caregiver researchers. This work is particularly important for aging researchers as the number of individuals with dementia and the burden on caregivers continues to increase (Gruenewald & Seeman, 2010), and as thesurvival of African American patients with Alzheimer’s disease may be longer than White patients with Alzheimer’s disease, thus the caregiving experience may also be longer (Mehta et al., 2008).
Methods
Participants
The participants in this study are from the Alzheimer’s Study of Emotions in Caregivers (ASEC) that were recruited from the Duke Caregiver Study (see Brummett et al., 2006 and Dilworth-Anderson et al, 2005 for additional information on the parent study). Caregivers for the Duke Caregiver study were recruited using flyers, adds in the local media and community outreach efforts conducted in collaboration with the Duke Caregiver Support Program. The original Duke Caregiver Study was designed to evaluate caregiving as a major naturally occurring stressor in the second half of the lifecycle. The size of the follow-up sample for the ASCE study was limited by the number of African American caregivers in the initial study. Once an African American caregiver agreed to participate they were matched to a White participant of the same age group, baseline living arrangement status, educational attainment and type of caregiver (spouse vs. adult child). The ASEC was designed to examine the emotional health of African American and White caregivers. Follow-up data on the ASEC caregivers (N = 82) was gathered approximately eight-years after their original baseline assessment between June 2002 and May 2004. All participants lived within driving distance of Duke Hospital. Four respondents were dropped from the analysis due to missing data, thus 78/82 or 95.1 % of eligible respondents included in this report. The majority were adult children caregivers (72 of 78, 92.3%).
Study procedures
Respondents were interviewed by phone in order to assess the manner in which diverse caregivers respond to the demands of caregiving in terms of the emotional responses it generates. As part of the interview process, re-assessment of depressive symptoms, perceptions of social support, and information regarding status of the care recipient were also gathered. With regard to baseline measures, see Brummett et al., 2006 for description of study procedures. The study was approved by the Duke University Medical Center Institutional Review Board.
Measures
Age was measured in years; race was assessed by self-report and categorized as White and African American; gender was modeled as female and male; education was measured in years and categorized as 12 years or less, 13 to 16 years, and greater than 16 years; and income was measured in categories from under $10,000 to over $100,000 per year in $5,000 increments. Residential living arrangements (LAR) of the caregiving dyad at baseline were categorized as: 1) living together in the same residence, 2) living apart in the community, or 3) care recipient lived in a long-term care facility (LTC). Death of the care recipient at follow-up was categorized as not deceased, or deceased.
Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, 1977). The questions refer to symptoms experienced during the week prior to the interview. The items were scored on a 4-point scale, with the total score ranging between 0–60. Higher scores represent depressive responses, and a score of 16 or greater is generally considered suggestive of a depressive disorder. Measures of internal consistency for the CES-D are acceptable, with alpha coefficients of .85 in a general population and .90 in a patient sample. Test-retest correlations range between .45 and .70 (31).
The Interpersonal Support Evaluation List (ISEL) (Cohen & Wills, 1985) was used to assess perceptions of social support. The ISEL assesses the dimensions of “Appraisal, Self-Esteem, Belonging, and Tangible” support. The following items are examples of the constructs: “When I feel lonely, there are several people I can talk to”, ” If I were sick, I could easily find someone to help me with my daily chores”, ”When I need suggestions on how to deal with a personal problem, I know someone I can turn to”. A shortened 16-item version of the ISEL was used in the present study (Brummett et al., 1998; Brummett et al., 2004). The original ISEL consists of 40 items and selection for the 16 items for the abbreviated scale was determined by an item consistency analysis performed in two independent samples. The percent of the full scale’s variance accounted for by items in the short scale 90.9%. The correlations between the shortened subscales and the original version subscales ranged between .87 and .94. Items were rated on a 4-point scale, with a potential range of 0–48 for total ISEL. Higher scores reflect greater perceived support.
Reasons for giving care that reflect cultural values were indexed by the Cultural Justification for Caregiving Scale (Dilworth-Anderson, et al., 2004). This is a 10-item scale that has a Chronbach Alpha = .86. Confirmatory factor analysis have shown that the CJCS is appropriate for both use in African American and White caregivers(Dilworth-Anderson, et al., 2005). The following three items are representative of the CJCS, “I give care because: a) It is my duty to provide care to elderly dependent family members, b) It is important to set an example for the children in the family, c) I was taught by my parents to take care of elderly dependent family members.
Statistical Analyses
The focus of the present study was to examine associations between social support (assessed at baseline and change in support from baseline to follow-up) and symptoms of depression at follow-up (adjusted for baseline depressive symptoms). Furthermore, because baseline support was also included in all models, the change in support over time can be viewed as that with effects of baseline levels removed. Importantly, race was examined as a potential moderator of interest with regard to social support→ depressive symptoms associations.
Because prior work has shown that LAR may influence the relation between race and depressive symptoms, we also included interaction terms with regard to baseline LAR. In addition, for the majority of caregivers the care recipient had died during the extended follow-up. Thus we included product terms examining the potential effect of death of the care recipient with regard to social support→ depression associations. Thus, an initial regression model included the following interaction terms: race X baseline support, race X change in support, LAR X race, LAR X baseline support, and LAR X change in support, death of recipient X baseline support, and death of recipient X change in support. A final model was tested after removal of non-significant interaction terms from the initial model. Analyses were adjusted for CJCS scores, baseline depressive symptoms, age, sex, income, and education. A value of p < 0.05 was considered statistically significant in the present study.
We also evaluated the extent to which overfitting may have occurred given the predictor-to-sample size ratio in our model by comparing our initial regression results to those generated using the penalization procedure recommended by Steyerberg et al (Steyerberg, Eijkemans, Harrell, & Habbema, 2001). The estimates after penalization were virtually identical to those from the model estimated without penalization and we therefore report only the original model here. In addition, we examined the potential impact on multicollinearity on the standard errors of the regression coefficient tests by calculating the variance inflation factor (VIF) for each term. I no case did the square root of the VIF exceed 2 (range = 1.05 to 1.27).
Results
The descriptive data, presented by race, are shown in Table 1. The only construct that was significantly different by race was whether or not the caregiver lived with the care recipient at baseline. African American caregivers tended to more often live separately in the community, as compared to White caregivers who more frequently lived together in the same dwelling, or the care recipient lived in a long term care facility.
Table 1.
Description of study variables, by race.
| Construct, mean and (SD) | African American (N = 38) | White (N = 40) |
|---|---|---|
| Age at baseline | 52.3 (9.3) | 53.9 (9.6) |
| Depressive symptoms at baseline | 10.8 (10.6) | 12.2 (10.0) |
| Depressive symptoms at follow-up | 7.3 (6.4) | 10.2 (8.8) |
| Social support at baseline | 39.6 (6.7) | 38.0 (6.2) |
| Social support at follow-up | 39.6 (6.9) | 39.4 (7.0) |
| Cultural justification for caregiving scale | 35.0 (6.2) | 32.4 (6.1) |
| Income, $ | 56,000 (29,000) | 66,000 (36,000) |
| Education level, N (%) | ||
| 12 years or fewer | 4 (10.5) | 5 (12.5) |
| 13 – 16 years | 21 (55.3) | 23 (29.5) |
| 17 years and higher | 13 (34.2) | 12 (30.0) |
| Living Arrangement, N (%)* | ||
| Live together same dwelling | 10 (26.3) | 17 (42.5) |
| Live separately in community | 18 (47.4) | 5 (12.5) |
| Recipient in long term care facility | 10 (26.3) | 18 (45.0) |
| Care recipient dead at follow-up, N (%) | 23 (60.5) | 32 (80.0) |
Note:
denotes p < 0.05, for difference between African American and White participants. Differences for continuous variable were assessed using t-tests, and differences for categorical variables were assessed using chi-square tests.
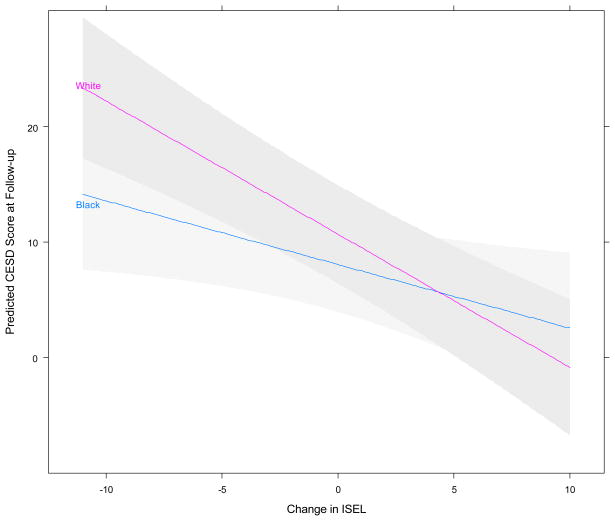
Results from the initial model predicting depressive symptoms containing all interaction terms indicated that only the race X change in social support was significant (F(1,77) = 7.97, p = 007). The remaining non-significant terms were removed and the final model is presented in Table 2. The race X change in social support interaction is graphically depicted in Figure 1, with results suggesting that when support decreased over time depressive symptoms at follow-up were lower for African Americans, as compared to Whites; whereas, when support increased over time depressive symptoms at follow-up tended to be similar for African Americans and Whites. Based on the interaction, the predicted slope for African Americans was −0.38 (95% Confidence Interval = −.66, −.10), for Whites the slope was −.91 (95% CI = −1.19, −.64). As shown in Figure 1, for African Americans a 10 point decrease in social support over time is associated with an approximate 11point increase in symptoms of depression, as compared to African American individuals with a similar increase in social support. Whereas, for Whites, a10 point decrease in social support is associated almost a 20 point increase in depressive symptoms, as compared with White individuals with a similar increase in social support. Thus, the magnitude of the effect of a decrease in social support for Whites is nearly two-fold that of the effect in African Americans. Indeed, the effect size for the difference in change depressive symptoms between Whites and African Americans, for a similar change in levels of social support, is equal to approximately a standard deviation, which is typically considered a large effect.
Table 2.
Results of final regression model predicting follow-up symptoms of depression at 7-years, adjusted for baseline depressive symptoms and other covariates.
| Estimate (SE) | P | |
|---|---|---|
| Intercept | 22.3 (7.8) | 0.006 |
| Age at baseline | 0.1 (0.1) | 0.956 |
| Income | 0.1 (0.1) | 0.674 |
| Education level (referent 17 years and higher) | ||
| 12 years or fewer | 7.3 (2.6) | 0.006 |
| 13 – 16 years | 3.1 (1.5) | 0.048 |
| Care recipient deceased (no) | −0.9 (1.5) | 0.569 |
| Gender (female) | 1.2 (2.1) | 0.574 |
| Race (African American) | −3.1 (1.5) | 0.040 |
| Cultural justification for caregiving scale | −0.1 (0.1) | 0.794 |
| Living arrangement care recipient (referent long term care) | ||
| Apart in community | 0.1 (1.8) | 0.957 |
| Together | −2.1 (1.8) | 0.211 |
| Baseline depressive symptoms | 0.2 (0.1) | 0.023 |
| Baseline social support ratings | −0.4 (0.1) | 0.008 |
| Change in social support (Follow-up – Baseline) | −1.0 (0.1) | 0.001 |
| Change in social support (Follow-up – Baseline) X race | 0.5 (0.2) | 0.007 |
Note: terms that are products in significant interactions should be interpreted as such.
Figure 1.
Depressive symptoms at follow-up (Total CES-D scores, adjusted for baseline CES-D and other covariates) predicted by change in perceptions of social support (ISEL rating at follow-up – ISEL ratings at baseline): by race (shaded areas represent 95% confidence intervals). (Color figure available online.)
Baseline social support was associated with fewer depressive symptoms at follow-up for all participants, such that higher social support at baseline predicted lower levels of depression at follow-up (F(1,77) = 7.60, p=.008).
With regard to covariates, only education level (F(2,77) = 4.27, p = .018) and baseline depressive symptoms (F(1,77) = 5.41, p = .023) were statistically significant predictors of depressive symptoms at follow-up. Individuals with less than or equal to 12 years of education (t = 2.85, p = .006), as well as those with between 13 and 16 years of education (t = 2.02, p= .046), had significantly higher follow-up depressive symptoms, as compared to those individuals having 17 or higher years of education. As expected, higher baseline depressive symptoms were associated with higher depressive symptoms at follow-up.
Discussion
The present study suggests that over time, the impact of change in social support on depressive symptoms may vary by race in caregivers of relatives with dementia. When caregivers’ perceptions of social support decreased over time during the caregiving experience, depressive symptoms tended to worsen for all participants, however, this worsening of depressive symptoms was magnified for Whites, as compared to African Americans. Indeed, in those with the largest decrease in support, Whites had CES-D scores in the clinical range (i.e., > 16), while even at the largest decrease in support, African Americans had CES-D scores were below 16. With regard to individuals whose support tended to increase over time, depressive symptoms decreased and the impact of such change was similar for all participants.
Our longitudinal findings on depression among caregivers and differences by race support findings from many cross-sectional studies. These findings provide further evidence that depressive symptomotology varies by race, but they leave unanswered questions regarding how and why African American caregivers express very limited negative emotionalproblems in their caregiving role as compared to Whites. Williams et al. (D. R. Williams, Yu, Jackson, & Anderson, 1997) reported that “race-related stress may have a more adverse impact on the mental health functioning of whites as compared to blacks.” (pg. 346). It is possible that declining social support is a more adverse stressor in whites, as compared to blacks.
It is also possible, on the other hand, that race and ethnicity may significantly influence the expression of depression with the result that reports of depressive symptoms are not always synonymous across cultures (W. E. Haley et al., 2004; Perreira, Deeb-Sossa, Harris, & Bollen, 2005; Pinquart & Sörensen, 2005). Hence, it has been suggested that the application of standard mood inventories in African American groups may contribute to the observation of lower prevalence rates of depression in this group when compared to White samples (Harrelson et al., 2002). We propose that future studies use a sociocultural perspective when researching emotional effects of caregiving on culturally diverse groups, which moves us beyond just examining race differences. A sociocultural perspective takes into consideration an ethnic and cultural group’s history, values, beliefs, and ways of thinking that may influence how we measure and interpret outcomes such as depression (Dilworth-Anderson & Palmer, 2011). To accomplish this goal, in addition to assessing depression using the standard CES-D as we used in this study, it may be important to allow caregivers to describe and give meaning to each of their emotions, which can inform the measuring and interpreting depression (Bernstein, Lee, Park, & Jyoung, 2007). Thus, a mixed methods approach is needed whereby probing questions are used to better understand emotional reactions to providing care. The goal of such approach would allow researchers to go beyond the summation of a measure of depression, but instead it would better ensure that the expressions of depression for any group are not “lost in summation.”
This approach certainly informs us as researchers regarding measurement issues, but it also could provide needed and relevant information to inform culturally appropriate interventions for caregivers in diverse groups. It also moves the discussion of racial differences among caregivers to another level in understanding resilience and vulnerability among them to better address their supportive needs.
In addition to the change in social support, ratings of support at baseline were also associated with follow-up depressive symptoms in the present caregiver sample. As expected, those with lower ratings of perceived support had higher depression at follow-up. Unlike the effect for change of support, race was not a significant modifier of the relation between baseline support ratings and depression at follow-up.
Death of the care recipient at follow-up did not significantly interact with either baseline support, or the change in social support, as a predictor of depressive symptoms. In addition, the death of the care recipient was not significantly associated with depressive symptoms at follow-up. The literature on depression following the death of a care recipient has been sparse and the findings have been mixed. However, in one of the few studies that has followed caregivers for a prolonged period following the demise of the care recipient it was shown that depressive symptoms declined over the course of follow-up (Aneshensel, Pearlin, Mullan, Zarit, & Whitlach, 1995).
By design, caregiving studies have often been restricted to samples that include only co-resident caregivers. Thus, caregiving studies have generally not included the types of residential arrangements assessed in our study, nor have they included their interactions with race as a factor predicting the emotional health of caregivers. A meta analysis examining the psychological and physical difficulties associated with caregiving (Pinquart & Sorensen, 2003) noted racial differences in co-residence, but not as a factor in the prediction of depression, nor did they consider the caregiving situation when the care recipient was in long-term care. The only studies we are aware of that have examined this topic have found opposite effects for living arrangement, i.e., one found that African American caregivers reported fewer depressive symptoms, as compared to Whites only when the caregiver and recipient were living together (Skarupski, McCann, Bioenias, & Evans, 2009), whereas another study found opposite effects (Siegler, et al., 2010). In the present study, we found no interaction of race by living arrangement. In addition, social support (baseline ratings, nor change in social support) did not interact with living arrangement to predict change in depressive symptoms over time.
With regard to covariates, the measure of cultural justification for caregiving used in the present study was not a significant predictor of depressive symptoms. As expected, education, however, was significantly associated with depressive symptoms. Specifically, as has been previously shown (Ross & Huber, 1985), those with higher education tended to have higher symptoms of depression.
Many caregiving situations not found in a single study are present in this data set. For example, in many studies caregivers have similar living arrangements and participants are at similar stages in the caregiving process. In addition, many studies do not include adequate numbers of both African American and White intergenerational family caregiving dyads. We view these factors as both strengths and weaknesses, and have attempted to model covariates in a manner that will at least allow researchers to interpret the findings accordingly. Our study has other limitations. Hispanic participants were not enrolled and thus we cannot address this source of ethnic variation. The majority of participants were adult children caregivers, thus our findings may not apply to spousal caregivers. Our sampling frame was community, rather than population based. The limited sample size may have reduced our power to detect certain findings and restricted the number of potentially interesting interactions we could examine. As with many studies in caregiving samples, replication of our findings from larger, more representative data sets is needed to see if our findings are generalizable. Lastly, the measurement of depression used in the present study may differpsychometrically between Whites and African Americans and this could have accounted for some of the racial differences observed.
Depression in caregivers has been associated with the development of cardiovascular disease e.g. (Mausbach, Patterson, Rabinowitz, Grant, & Schulz, 2007), and the negative health outcomes that accompany depression associated with caregiving may also vary by race (Vitaliano, Jianping, & Scanlan, 2003). Although race effects were not examined, Williams et al.(V. P. Williams et al., 2010) have shown, in a controlled trial of video-based coping skills training in African American and White Alzheimer’s Disease family caregivers, that those receiving the training experienced reduced depressive symptoms and blood pressure levels that were maintained at six months following the completion of training.
The fact that at a follow-up of approximately 7 years roughly 30% of care recipients remained alive suggests that future longitudinal studies of caregiving need to plan for extended follow-up periods if they intend on capturing the full length of the caregiving experience. In addition, the present findings suggest racial differences with regard to depressive symptoms in caregivers for dementia patients do exist but need to be more fully explored in future research. These findings also indicate that research designed to plan interventions must not ignore racial differences in the caregiving process. Our results suggest that social support may be a salient factor for prevention of future depressive symptoms, in particular for African American caregivers. Thus, periodic assessment of changes in social support may be a factor that clinicians and health care providers might consider. Attention to race differences in health outcomes is important as demographic projections for the US show that by 2030, 22% of the population will be over age 65 and those elders will be more ethnically and racially diverse--with 25% composed of ethnic minorities. The study of psychosocial responses to caregiving in diverse groups provides an excellent vehicle for developing a psychology of diversity. This is particularly important for clinicians when the focus of intervention is organized around important transitions in care for caregivers (Dilworth-Anderson & Palmer, 2011).
Acknowledgments
This research was supported by grant # IIRG-08-89565 from the Alzheimer’s Association, R01 AG19605 from the National Institute on Aging with co-funding by the National Institute of Environmental Health Sciences, and the National Institute of Mental Health, P01HL36587 from the National Heart Lung and Blood Institute, The Claude D. Pepper Older Americans Independence Centers grant P30 AG028716, and the Duke Behavioral Medicine Research Center. We would like to thank Jaye Efland and Shirley Austin for their excellent staff work on study, Robin French for programming and data management, and Michael A. Babyak, PhD, for statistical consultation.
Contributor Information
BEVERLEY H. BRUMMETT, Duke University.
ILENE C. SIEGLER, Duke University
REDFORD B. WILLIAMS, Duke University
PEGGYE DILWORTH-ANDERSON, University of North Carolina at Chapel Hill.
References
- Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, Whitlach CJ. Profiles in caregiving: the unexpected career. San Diego: Academic Press; 1995. [Google Scholar]
- Bernstein KS, Lee JK, Park SY, Jyoung JPP. Symptom manifestations and expression among Korean immigrant women suffering with depression. Journal of Advanced Nursing. 2007;61:393–402. doi: 10.1111/j.1365-2648.2007.04533.x. [DOI] [PubMed] [Google Scholar]
- Brummett BH, Babyak MA, Barefoot JC, Bosworth HB, Clapp-Channing NE, Siegler IC, Mark DB. Social support and hostility as predictors of depressive symptoms in cardiac patients one month following hospitalization: A prospective study. Psychosomatic Medicine. 1998;60:707–713. doi: 10.1097/00006842-199811000-00008. [DOI] [PubMed] [Google Scholar]
- Brummett BH, Babyak MA, Mark DB, Clapp-Channing NE, Siegler IC, Barefoot JC. Prospective study of perceived stress in cardiac patients. Annals of Behavioral Medicine. 2004;27:22–30. doi: 10.1207/s15324796abm2701_4. [DOI] [PubMed] [Google Scholar]
- Clay OJ, Roth DL, Wadley VG, Haley WE. Changes in social support and their impact on psychosocial outcome over a 5-year period for African American and White dementia caregivers. Int J Geriatr Psychiatry. 2008;23:857–862. doi: 10.1002/gps.1996. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Dilworth-Anderson P, Brummett BH, Goodwin P, Williams SW, Williams RB, Siegler IC. Effect of race on cultural justifications for caregiving. Journal of Gerontol: Social Science. 2005;60B:257–262. doi: 10.1093/geronb/60.5.s257. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P, Goodwin PY, Williams SW. Can culture help explain the physical health effects of caregiving over time among African American caregivers? Journal of Gerontology: Social Sciences. 2004;59B:S138–145. doi: 10.1093/geronb/59.3.s138. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P, Palmer MH, editors. Annual Review of Gerontology and Geriatrics. Vol. 31. Springer; New York: Pathways through the Transitions of Care for Older Adults. in press. [Google Scholar]
- Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980–2000) The Gerontologist. 2002;42:237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- Gruenewald TL, Seeman TE, editors. Stress and aging: A biological double jeoardy? New York: Springer; 2010. [Google Scholar]
- Haley WE, et al. Psychological, social and health impact of caregiving: A comparison of black and white dementia family caregivers and non-caregivers. Psych and Agina. 1995;10:540–552. [PubMed] [Google Scholar]
- Haley WE, Gitlin LN, Wisniewski SR, Feeney-Mahoney D, Coon DW, Winter L, et al. Well-being, appraisal, and coping in African-American and Caucasian dementia caregivers: Findings from the REACH study. Aging Ment Health. 2004;8:316–329. doi: 10.1080/13607860410001728998. [DOI] [PubMed] [Google Scholar]
- Jackson JJ, Antonucci TC, Brown E. A cultural lens on Biopsychosocial models of aging. In: Costa PT, Siegler IC, editors. Advances in Cell Aging and Gerontology. Vol. 15. Amsterdam, the Netherlands: Elsevier; 2004. pp. 221–241. [Google Scholar]
- Mausbach BT, Patterson TL, Rabinowitz YG, Grant I, Schulz R. Depression and distress predict time to cardiovascular disease in dementia caregivers. Health Psy. 2007;26:539–544. doi: 10.1037/0278-6133.26.5.539. [DOI] [PubMed] [Google Scholar]
- Mehta KM, Yaffe K, Pérez-Stable EJ, Stewart A, Barnes D, Kurland BF, Miller BL. Race/ethnic differences in AD survival in US Alzheimer’s Disease Centers. Neurology. 2008;70:1163–1170. doi: 10.1212/01.wnl.0000285287.99923.3c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perreira KM, Deeb-Sossa N, Harris KM, Bollen K. What are we measuring? An evaluation of the CES-D across race/ethnicity and immigrant generation. Social Forces. 2005;83:1567–1602. [Google Scholar]
- Pinquart M, Sorensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Ethnic differences in stressors, resources and a psychological outcomes of family caregiving: A meta-analysis. The Gerontologist. 2005;45:90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Spouses, adult children anmd children -in -law as caregivers of older adults. Psych and Aging. 2011;26:1–14. doi: 10.1037/a0021863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: A meta-analysis. The Gerontologist. 2005;45:90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Ross CE, Huber J. Hardship and depression. Journal of Health and Social Behavior. 1985;26(312–327) [PubMed] [Google Scholar]
- Siegler IC, Dilworth-Anderson P, Brummett BH, Haney TL, Williams RB. Caregiving, residence, race, and depressive symptoms. Aging and Mental Health. 2010;72 doi: 10.1080/13607861003713257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skarupski KA, McCann JJ, Bioenias JL, Evans DA. Race differences in emotional adaptation of family caregivers. Aging Ment Health. 2009;13:715–724. doi: 10.1080/13607860902845582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steyerberg EW, Eijkemans MJ, Harrell FE, Habbema JDF. Prognostic modeling with logistic regression analysis: in search of a sensible strategy in small data sets. Med Decis Making. 2001;21:45–56. doi: 10.1177/0272989X0102100106. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Jianping Z, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychological Bulletin. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health. Journal of Health Psychology. 1997;2(335–51) doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Williams VP, Bishop-Fitzpatrick L, Lane JD, Gwyther GP, Ballard EL, Analise P, Williams RB. Video-based coping skills to reduce health risk and improve psychological and physical well being in Alzheimer’s Disease family caregivers. Psychosom Med. 2010;72:897–904. doi: 10.1097/PSY.0b013e3181fc2d09. [DOI] [PMC free article] [PubMed] [Google Scholar]