Abstract
AIM: To evaluate the efficacy of human thrombin in the treatment of bleeding gastric and ectopic varices.
METHODS: Retrospective observational study in a Tertiary Referral Centre. Between January 1999-October 2005, we identified 37 patients who were endoscopically treated with human thrombin injection therapy for bleeding gastric and ectopic varices. Patient details including age, gender and aetiology of liver disease/segmental portal hypertension were documented. The thrombin was obtained from the Scottish National Blood Transfusion Service and prepared to give a solution of 250 IU/mL which was injected via a standard injection needle. All patient case notes were reviewed and the total dose of thrombin given along with the number of endoscopy sessions was recorded. Initial haemostasis rates, rebleeding rates and mortality were catalogued along with the incidence of any immediate complications which could be attributable to the thrombin therapy. The duration of follow up was also listed. The study was conducted according to the United Kingdom research ethics guidelines.
RESULTS: Thirty-seven patients were included. 33 patients (89%) had thrombin (250 U/mL) for gastric varices, 2 (5.4%) for duodenal varices, 1 for rectal varices and 1 for gastric and rectal varices. (1) Gastric varices, an average of 15.2 mL of thrombin was used per patient. Re-bleeding occurred in 4 patients (10.8%), managed in 2 by a transjugular intrahepatic portosystemic shunt (TIPSS) (one unsuccessfully who died) and in other 2 by a distal splenorenal shunt; (2) Duodenal varices (or type 2 isolated gastric varices), an average of 12.5 mL was used per patient over 2-3 endoscopy sessions. Re-bleeding occurred in one patient, which was treated by TIPSS; and (3) Rectal varices, an average of 18.3 mL was used per patient over 3 endoscopy sessions. No re-bleeding occurred in this group.
CONCLUSION: Human thrombin is a safe, easy to use and effective therapeutic option to control haemorrhage from gastric and ectopic varices.
Keywords: Variceal haemorrhage, Ectopic Varices, Gastric varices, Portal hypertension, Thrombin
INTRODUCTION
Haemorrhage from gastric or ectopic varices is associated with high morbidity and mortality and can account for up to one third of all cases of variceal haemorrhage[1]. In the presence of oesophageal varices, the prevalence of gastric varices ranges from 15% to 100%[2,3] with the risk of bleeding generally regarded to range from 4%-65% over the first 2 years after diagnosis[2,4]. More importantly it has been reported that although gastric varices are less likely to bleed than oesophageal varices, once they bleed, they tend to do so more severely and haemostasis can be difficult to achieve[2].
Unlike oesophageal variceal haemorrhage, bleeding from gastric varices has not been extensively studied. The natural history of bleeding gastric varices differs from that of oesophageal varices and thus the precipitating event for gastric variceal haemorrhage remains uncertain. Predictive factors for oesophageal variceal haemorrhage such as a hepatic venous pressure gradient (HVPG) of > 20 mmHg[5] is not felt to be as relevant to gastric variceal bleeding and this is partly attributed to the development of gastrorenal shunts. Indeed we have previously demonstrated that a portal pressure gradient (PPG) of < 12 mmHg does not necessarily protect against gastric variceal bleeding and that a PPG < 7 mmHg is a better safeguard against rebleeding[6]. The variceal size, tortuosity and stigmata of recent bleeding such as red signs however remain alarming features[4].
Thrombin was first used for the management of gastric varices in 1947[7] and affects haemostasis by converting fibrinogen to a fibrin clot. It also has other influences on the coagulation system with one effect being the enhancement of local platelet aggregation. Endoscopic treatment with thrombin has been reported in the treatment of bleeding oesophageal, gastric and duodenal varices[8-10] with a low rate of rebleeding. The most recent study from Ramesh et al[11] reported that haemostasis was achieved in the acute setting in 92% patients presenting with bleeding gastric varices, with only one patients requiring a transjugular intrahepatic portosystemic shunt (TIPSS) to control bleeding. The majority of these studies are however retrospective and include small patient numbers.
The aim of this study is therefore to evaluate the use of human thrombin in the treatment of gastric and ectopic varices.
MATERIALS AND METHODS
We identified 37 consecutive patients who were treated with human thrombin (Scottish National Blood Transfusion Service) from January 1999-October 2005 for isolated bleeding from gastric and ectopic varices. Thrombin was injected rather than cyanoacrylate as this was our Units protocol. The case notes were reviewed and total volume of thrombin used and the incidence of complications recorded, as was the incidence of re-bleeding or death. Those patients with bleeding oesophageal varices who underwent banding of varices or any patient in which there was diagnostic doubt as to the aetiology of bleeding were excluded. The study was conducted according to the United Kingdom research ethics guidelines. Following consideration by the local ethics committee, further specific ethical review and approval was not required, as the study was considered a retrospective audit using anonymised data obtained as part of usual patient care.
Patient characteristics
Twenty-eight of the patients were male (male:female ratio = 28:9) with a mean age at presentation of 53.2 years (range: 18-83 years). The underlying aetiology was alcoholic liver disease in 15 patients, splenic vein thrombosis in 6, cryptogenic cirrhosis in 6, primary biliary cirrhosis in 2, chronic active hepatitis in 2, portal vein thrombosis in 2, primary sclerosing cholangitis in 2, α1-antitrypsin deficiency in 1, congenital hepatic fibrosis in 1 and hepatitis C in 1 patient. The Childs-Pugh grade: grade A = 5 patients, grade B = 16 patients and grade C = 10 patients. Segmental portal hypertension was defined as extrahepatic portal hypertension in the absence of liver cirrhosis and was seen in 6 patients whose underlying aetiology was splenic vein thrombosis.
Endoscopic therapy
All patients had an upper gastrointestinal endoscopy/flexible sigmoidoscopy performed by an experienced operator within 12 h of presentation. Gastric variceal haemorrhage was defined as visible spurting or oozing of blood from the lesser curve or fundal vessels at the time of endoscopy with varices subdivided into fundal and non fundal. Sarin’s classification for gastric varices was used but it was noted that it is often difficult to differentiate the types of fundal varices in patients who are actively bleeding. The gastric and duodenal varices were also considered to have bled if there were stigmata of recent bleeding such as red spots or adherent clot. Rectal variceal haemorrhage was defined by the presence of rectal varices with either adherent clot or visible active bleeding combined with a history of profuse fresh blood loss per rectum.
In those patients with splenic vein thrombosis, an alternative therapy such as splenectomy may be considered by some but it is important that bleeding is controlled and therefore all these patients underwent endoscopy and stabilization of bleeding prior to consideration for splenectomy.
Protocol for thrombin therapy
All patients were adequately resuscitated at the time of endoscopy. Human thrombin concentrate obtained from the Scottish National Blood Transfusion Service and each vial was reconstituted with 5 mL of water to give a concentration of 250 U/mL. As thrombin was being used outwith its licensed use, informed written consent was obtained from each patient prior to endoscopy. The thrombin was injected directly into the varices using a standard injection sclerotherapy needle to a maximum volume of 10 mL at any one session by multiple injections. Repeat endoscopy was arranged initially for one week then at two weekly intervals until further injection was deemed unnecessary by the endoscopist as the overlying mucosa had returned to normal in which the varix appeared well covered with no stigmata of recent haemorrhage. The number of endoscopy sessions, the total volume of thrombin used and the incidence of complications were documented.
RESULTS
Thirty-three patients (89%) had thrombin for gastric varices, two (5.4%) for duodenal varices, one for rectal varices and one for gastric and rectal varices. A small number of patients in this cohort were in our original pilot study[12]. Twenty seven patients (82%) also had oesophageal varices with 19 patients (58%) already in a banding programme. Only 3 patients were on beta-blocker therapy prior to admission. The average total volume of thrombin used per patient was 15.2 mL (range: 5-47.5 mL, combined rectal and gastric varices) over 1-7 endoscopy sessions (median 3.6 sessions).
For those patients with gastric varices, 82% were classified as gastro-oesophageal varices (GOV) type 2 with the remainder being classified as isolated gastric varices (IGV) type 1 (12 %) and type 2 (6%). In two cases where it was not absolutely clear whether they were GOV type 1 or type 2 they were included as type 2. An average of 15.2 mL of thrombin was used per patient (Figure 1). Re-bleeding occurred in four patients (10.8%), three of which bled before the 2nd endoscopy session (i.e., within 7 d of index bleed) and two of whom were managed by TIPSS. One of the TIPSS procedures was unsuccessful and the patient subsequently died after a rebleed. The two other patients were successfully treated by distal splenorenal shunt.
Figure 1.
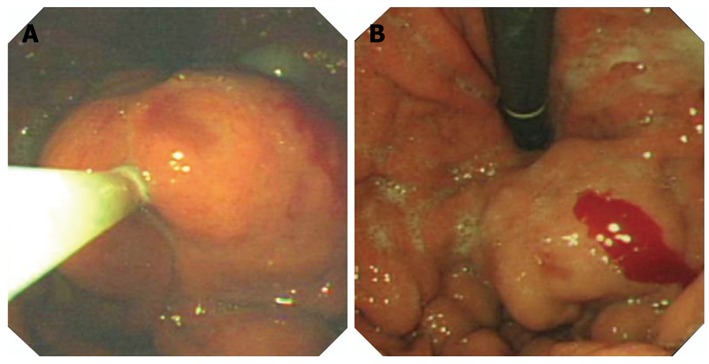
Injection of gastric varices with thrombin. A: During thrombin injection the gastric varix swells; B: Post thrombin injection.
For those two patients with duodenal varices, an average of 12.5 mL was used per patient over 2-3 endoscopy sessions. Re-bleeding occurred at day 3 in one patient which was treated successfully by TIPSS insertion.
For the patient with rectal varices, an absolute volume of 18.3 mL was used over three endoscopy sessions. No re-bleeding occurred in this group.
Only a small proportion of patients (15%) had additional therapy with vasopressor agents, the use of which did not change outcome. All patients with liver disease received five days of intravenous antibiotics as per our units protocol. In addition, true eradication of varices was rare with varices deemed visually eradicated in only two patients. No HVPG measurements were obtained in any patient as this is not our Units protocol. Overall mortality was 2.7% after median follow up of 22 mo.
Complications
No clinically significant adverse events occurred following thrombin therapy with median follow up of 22 mo.
DISCUSSION
Gastric varices are generally classified by their location in the stomach and their relationship with oesophageal varices, as proposed by Sarin et al[2]. GOV is the term used to describe gastric varices that are associated with oesophageal varices and are classified as either type 1 or type 2. IGV is used to refer to gastric varices that occur independently of oesophageal varices. It is observed that type 1 GOV (which are primarily supplied by the left gastric vein) represent 75% of all gastric varices observed. However it is generally regarded that the most serious haemorrhage occurs when type 1 IGV gastric varices (primarily supplied by the short gastric vein) bleed.
Various treatment options exist for the management of bleeding gastric varices and include endoscopic methods, TIPSS and other radiological procedures. Surgical procedures such as under running of gastric varices or devascularization procedures has previously been used but in the small studies performed have shown no great benefit and thus are rarely performed today.
Although there is debate regarding optimum treatment of gastric variceal haemorrhage, endoscopic therapy is an established treatment and it is currently recommended in the United Kingdom to be the first line treatment in the management of acute gastric variceal haemorrhage[13]. Endoscopic treatment options include standard sclerotherapy, band and snare ligation or endoscopic injection with cyanoacrylate or thrombin.
Standard sclerotherapy using ethanolamine as the sclerosing agent has been used with moderate success in the treatment of bleeding oesophageal varices but has limited success in the treatment of bleeding gastric varices. It is widely accepted that sclerotherapy for gastric varices requires significantly greater volumes of sclerosant[2] which is thought to account for the increased number of side effects that are observed[14]. The initial haemostasis rates obtained when using sclerotherapy have been reported to vary widely from 26%-100%[11-16] which may reflect different operator ability and injection techniques. However a rebleeding rate of 60%-90% has been reported in most studies which is generally observed in patients with bleeding fundal varices[1,17]. The majority of the rebleeding episodes have been reported to be related to ulceration at the injection site.
Endoscopic injection therapy with tissue adhesives such as cyanoacrylate has also been shown to be of benefit in the management of bleeding gastric varices and is becoming more popular due to the high rebleeding rates observed with sclerotherapy. A 90% success rate in achieving initial haemostasis has been reported in a number of non randomised studies[18-20] but Ramond et al[21] also reported a rebleeding rate of 50%. Several studies have also demonstrated that the use of tissue adhesives is superior to standard sclerotherapy. Oho et al[3] have published results of a controlled but non-randomised study which demonstrated that initial control of gastric variceal bleeding and survival was significantly greater in patients treated with cyanoacrylate than standard sclerotherapy. Sarin et al[22] have published results for a small randomised control trial which again suggested that the use of cyanoacrylate was superior to standard sclerotherapy. Complications rates between the two procedures have been reported to be similar but of course this depends primarily on the expertise available. In the hands of inexperienced operators, tissue adhesives can cause irreparable damage to the endoscope. In addition, a few centres have reported the occurrence of systemic emboli after the use of tissue adhesives to control variceal haemorrhage[23,24].
Gastric variceal band ligation using ‘O’rings and detachable snares have also been used in the management of gastric variceal haemorrhage but with high rebleeding rates being observed[25]. Yoshida et al[26,27] have however published data on the combined use of the detachable snare and simultaneous injection sclerotherapy and O-ring ligator. In a study of 43 patients[26], 97% had eradication of gastric varices with an 8% rebleeding rate observed within a 2 year follow up period.
The optimal treatment for the management of gastric varices therefore remains uncertain but as our results suggest, a promising therapeutic option is the use of intravariceal injection of thrombin. The use of thrombin in bleeding gastric or ectopic varices has only previously been reported in a handful of studies in which a variety of thrombin preparations have been used. To our knowledge, this study is currently the largest published study using human thrombin.
For the management of bleeding gastric varices, our rates of achieving initial haemostasis were in keeping with 93% published by Datta et al[10] and 100% by Williams et al[9]. Our rebleed rate of 14% was again in keeping with data published by Williams et al[9] but it should however be recorded that the median follow up time in these studies varied greatly from six weeks to nine mo. It should also be documented that this rebleed rate was observed without us actively attempting to visually eradicate the varices and may suggest that continued thrombin injection to achieve visual eradication appears unnecessary. This point was emphasised when we examined the number of endoscopic sessions in which thrombin was given as initially the procedure was performed out to 7 sessions. It was only after analysis of these pilot data that rebleeding was deemed extremely rare after 3 endoscopic sessions and that eradication of gastric varices was unnecessary. It is therefore now our Units adopted policy that patients should be treated with thrombin for 3 endoscopic sessions. Overall, our mortality rate of 2.7% highlights how effective thrombin therapy can be, but it should be recorded that these results were obtained after 5 patients who rebleed underwent further interventions: namely TIPSS or splenorenal shunt surgery.
The thrombin used in this study was obtained free of charge from Blood Transfusion Service but we have now changed to using a recombinant thrombin preparation at cost of £250 for concentration of 250 IU/mL. This is comparable to the cost of cyanoacrylate and the cost of TIPSS (at £5000).
Currently, no randomised controlled trials comparing thrombin with tissue adhesives or sclerotherapy have been performed. Interestingly however, Kojima et al[28] have published results for 30 patients with bleeding fundal varices that underwent sclerotherapy with ethanolamine under fluoroscopic guidance with the injection site being sealed with topical thrombin glue. All participants also received intravenous vasopressin and transdermal nitroglycerin. They reported an initial haemostasis rate of 93% with a rebleed rate of 19% after 5 years of follow up. The efficacy of the topical thrombin is however difficult to determine and the specialized technique and equipment required for this procedure may limit its future application.
With regards to the safety of human thrombin, we did not record any complications of thrombin use and this is again in keeping with all of the previously published studies that have used human thrombin. Complications such as anaphylaxis or altered thrombogenesis that have previously been reported with the use of bovine thrombin did not occur[29].
Although in this study we have not monitored the effect of thrombin by any means, we have evidence that results can be further improved by assessing clot formation with other means such as endoscopic ultrasound[30].
In conclusion, We have shown that human thrombin is a safe, easy to use and effective therapeutic option in the management of bleeding gastric and ectopic varices. Our study also suggests that continued thrombin injection to achieve visual eradication appears unnecessary. Larger randomised control trials are necessary to compare the use of human thrombin with the current available therapeutic modalities.
COMMENTS
Background
Haemorrhage from gastric or ectopic varices is associated with high morbidity and mortality and can account for up to one third of all cases of variceal haemorrhage.
Research frontiers
Unlike oesophageal variceal haemorrhage, bleeding from gastric varices has not been extensively studied. The natural history of bleeding gastric varices differs from that of oesophageal varices and thus the precipitating event for gastric variceal haemorrhage remains uncertain.
Innovations and breakthroughs
Initial haemostasis rates, rebleeding rates and mortality were catalogued along with the incidence of any immediate complications which could be attributable to the thrombin therapy. The duration of follow up was also listed. The study was conducted according to the United Kingdom research ethics guidelines.
Applications
Human thrombin is a safe, easy to use and effective therapeutic option in the management of bleeding gastric and ectopic varices.
Peer review
The results of a retrospective study concerning 37 patients, who were treated with thrombin injection for bleeding gastric or ectopic varices. Their major finding is that in patients with gastric varices this treatment is effective. The authors conclude that thrombin injection may be used to treat patients with gastric or ectopic variceal bleeding.
Footnotes
Peer reviewers: Dr. Andrea De Gottardi, Hepatology-Inselspital, Freiburgstrasse, 3010 Berne, Switzerland; Dr. Marco Senzolo, Department of Gastroenterology, University-Hospital of Padova, Via Giustiniani 2, 35128 Padova, Italy
S- Editor Gou SX L- Editor A E- Editor Zhang DN
References
- 1.Trudeau W, Prindiville T. Endoscopic injection sclerosis in bleeding gastric varices. Gastrointest Endosc. 1986;32:264–268. doi: 10.1016/s0016-5107(86)71843-9. [DOI] [PubMed] [Google Scholar]
- 2.Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–1349. doi: 10.1002/hep.1840160607. [DOI] [PubMed] [Google Scholar]
- 3.Oho K, Iwao T, Sumino M, Toyonaga A, Tanikawa K. Ethanolamine oleate versus butyl cyanoacrylate for bleeding gastric varices: a nonrandomized study. Endoscopy. 1995;27:349–354. doi: 10.1055/s-2007-1005712. [DOI] [PubMed] [Google Scholar]
- 4.Kim T, Shijo H, Kokawa H, Tokumitsu H, Kubara K, Ota K, Akiyoshi N, Iida T, Yokoyama M, Okumura M. Risk factors for hemorrhage from gastric fundal varices. Hepatology. 1997;25:307–312. doi: 10.1053/jhep.1997.v25.pm0009021939. [DOI] [PubMed] [Google Scholar]
- 5.Moitinho E, Escorsell A, Bandi JC, Salmerón JM, García-Pagán JC, Rodés J, Bosch J. Prognostic value of early measurements of portal pressure in acute variceal bleeding. Gastroenterology. 1999;117:626–631. doi: 10.1016/s0016-5085(99)70455-5. [DOI] [PubMed] [Google Scholar]
- 6.Tripathi D, Therapondos G, Jackson E, Redhead DN, Hayes PC. The role of the transjugular intrahepatic portosystemic stent shunt (TIPSS) in the management of bleeding gastric varices: clinical and haemodynamic correlations. Gut. 2002;51:270–274. doi: 10.1136/gut.51.2.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daly BM. Use of buffer thrombin in the treatment of gastric hemorrhage; a preliminary report. Arch Surg. 1947;55:208–212. doi: 10.1001/archsurg.1947.01230080213011. [DOI] [PubMed] [Google Scholar]
- 8.Fujii Y, Sugawa C, Ozawa T, Nakumura R, Brown-Castillo J, Mammen EF. Hemostasis activation during esophageal variceal sclerotherapy with thrombin in cirrhotics. Am Surg. 1991;57:222–225. [PubMed] [Google Scholar]
- 9.Williams SG, Peters RA, Westaby D. Thrombin--an effective treatment for gastric variceal haemorrhage. Gut. 1994;35:1287–1289. doi: 10.1136/gut.35.9.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Datta D, Vlavianos P, Alisa A, Westaby D. Use of fibrin glue (beriplast) in the management of bleeding gastric varices. Endoscopy. 2003;35:675–678. doi: 10.1055/s-2003-41517. [DOI] [PubMed] [Google Scholar]
- 11.Ramesh J, Limdi JK, Sharma V, Makin AJ. The use of thrombin injections in the management of bleeding gastric varices: a single-center experience. Gastrointest Endosc. 2008;68:877–882. doi: 10.1016/j.gie.2008.02.065. [DOI] [PubMed] [Google Scholar]
- 12.Yang WL, Tripathi D, Therapondos G, Todd A, Hayes PC. Endoscopic use of human thrombin in bleeding gastric varices. Am J Gastroenterol. 2002;97:1381–1385. doi: 10.1111/j.1572-0241.2002.05776.x. [DOI] [PubMed] [Google Scholar]
- 13.Jalan R, Hayes PC. UK guidelines on the management of variceal haemorrhage in cirrhotic patients. British Society of Gastroenterology. Gut. 2000;46 Suppl 3-4:III1–III15. doi: 10.1136/gut.46.suppl_3.iii1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sarin SK. Long-term follow-up of gastric variceal sclerotherapy: an eleven-year experience. Gastrointest Endosc. 1997;46:8–14. doi: 10.1016/s0016-5107(97)70202-5. [DOI] [PubMed] [Google Scholar]
- 15.Gimson AE, Westaby D, Williams R. Endoscopic sclerotherapy in the management of gastric variceal haemorrhage. J Hepatol. 1991;13:274–278. doi: 10.1016/0168-8278(91)90068-m. [DOI] [PubMed] [Google Scholar]
- 16.Sarin SK, Sachdev G, Nanda R, Misra SP, Broor SL. Endoscopic sclerotherapy in the treatment of gastric varices. Br J Surg. 1988;75:747–750. doi: 10.1002/bjs.1800750809. [DOI] [PubMed] [Google Scholar]
- 17.Korula J, Chin K, Ko Y, Yamada S. Demonstration of two distinct subsets of gastric varices. Observations during a seven-year study of endoscopic sclerotherapy. Dig Dis Sci. 1991;36:303–309. doi: 10.1007/BF01318201. [DOI] [PubMed] [Google Scholar]
- 18.Huang YH, Yeh HZ, Chen GH, Chang CS, Wu CY, Poon SK, Lien HC, Yang SS. Endoscopic treatment of bleeding gastric varices by N-butyl-2-cyanoacrylate (Histoacryl) injection: long-term efficacy and safety. Gastrointest Endosc. 2000;52:160–167. doi: 10.1067/mge.2000.104976. [DOI] [PubMed] [Google Scholar]
- 19.Dhiman RK, Chawla Y, Taneja S, Biswas R, Sharma TR, Dilawari JB. Endoscopic sclerotherapy of gastric variceal bleeding with N-butyl-2-cyanoacrylate. J Clin Gastroenterol. 2002;35:222–227. doi: 10.1097/00004836-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Kind R, Guglielmi A, Rodella L, Lombardo F, Catalano F, Ruzzenente A, Borzellino G, Girlanda R, Leopardi F, Pratticò F, et al. Bucrylate treatment of bleeding gastric varices: 12 years’ experience. Endoscopy. 2000;32:512–519. doi: 10.1055/s-2000-3817. [DOI] [PubMed] [Google Scholar]
- 21.Ramond MJ, Valla D, Mosnier JF, Degott C, Bernuau J, Rueff B, Benhamou JP. Successful endoscopic obturation of gastric varices with butyl cyanoacrylate. Hepatology. 1989;10:488–493. doi: 10.1002/hep.1840100415. [DOI] [PubMed] [Google Scholar]
- 22.Sarin SK, Jain AK, Jain M, Gupta R. A randomized controlled trial of cyanoacrylate versus alcohol injection in patients with isolated fundic varices. Am J Gastroenterol. 2002;97:1010–1015. doi: 10.1111/j.1572-0241.2002.05622.x. [DOI] [PubMed] [Google Scholar]
- 23.Sée A, Florent C, Lamy P, Lévy VG, Bouvry M. [Cerebrovascular accidents after endoscopic obturation of esophageal varices with isobutyl-2-cyanoacrylate in 2 patients] Gastroenterol Clin Biol. 1986;10:604–607. [PubMed] [Google Scholar]
- 24.Roesch W, Rexroth G. Pulmonary, cerebral and coronary emboli during bucrylate injection of bleeding fundic varices. Endoscopy. 1998;30:S89–S90. doi: 10.1055/s-2007-1001406. [DOI] [PubMed] [Google Scholar]
- 25.Lo GH, Lai KH, Cheng JS, Chen MH, Chiang HT. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology. 2001;33:1060–1064. doi: 10.1053/jhep.2001.24116. [DOI] [PubMed] [Google Scholar]
- 26.Yoshida T, Harada T, Shigemitsu T, Takeo Y, Miyazaki S, Okita K. Endoscopic management of gastric varices using a detachable snare and simultaneous endoscopic sclerotherapy and O-ring ligation. J Gastroenterol Hepatol. 1999;14:730–735. doi: 10.1046/j.1440-1746.1999.01941.x. [DOI] [PubMed] [Google Scholar]
- 27.Yoshida H, Onda M, Tajiri T, Mamada Y, Taniai N, Mineta S, Yoshioka M, Hirakata A, Yamashita K. New techniques: combined endoscopic injection sclerotherapy and ligation for acute bleeding from gastric varices. Hepatogastroenterology. 2002;49:932–934. [PubMed] [Google Scholar]
- 28.Kojima K, Imazu H, Matsumura M, Honda Y, Umemoto N, Moriyasu H, Orihashi T, Uejima M, Morioka C, Komeda Y, et al. Sclerotherapy for gastric fundal variceal bleeding: is complete obliteration possible without cyanoacrylate? J Gastroenterol Hepatol. 2005;20:1701–1706. doi: 10.1111/j.1440-1746.2005.03992.x. [DOI] [PubMed] [Google Scholar]
- 29.Tadokoro K, Ohtoshi T, Takafuji S, Nakajima K, Suzuki S, Yamamoto K, Ito K, Miyamoto T, Muranaka M. Topical thrombin-induced IgE-mediated anaphylaxis: RAST analysis and skin test studies. J Allergy Clin Immunol. 1991;88:620–629. doi: 10.1016/0091-6749(91)90156-i. [DOI] [PubMed] [Google Scholar]
- 30.Krystallis C, McAvoy NC, Wilson J, Hayes PC, Plevris JN. EUS-assisted thrombin injection for ectopic bleeding varices--a case report and review of the literature. QJM. 2012;105:355–358. doi: 10.1093/qjmed/hcr030. [DOI] [PubMed] [Google Scholar]


