Peutz Jeghers syndrome (PJS) is an autosomal dominant condition characterized by hamartomatous polyps throughout the gastrointestinal (GI) tract and mucosal cutaneous pigmentation [Beggs et al. 2010]. PJS is associated with increased risk of GI and non-GI malignancies, the most common site being colorectal followed by breast, stomach, small bowel and pancreas. These hamartomatous polyps can be present anywhere in the GI tract. Most of these polyps become symptomatic at an early age requiring emergent laparotomies and bowel resections. Published guidelines have suggested frequent surveillance starting at an early age and endoscopic removal of polyps intraoperatively [Beggs et al. 2010]. Lately double-balloon enteroscopy (DBE) alone has been used for excision of these polyps [Gao et al. 2010]. Since the overtube and enteroscope balloons are made of latex, the procedure is not suitable for patients with severe latex allergy. In our institution, we recently used single-balloon enteroscopy (SBE) (Figure 1) for radical polypectomy in a patient with PJS and latex allergy highlighting the feasibility and safety of the procedure.
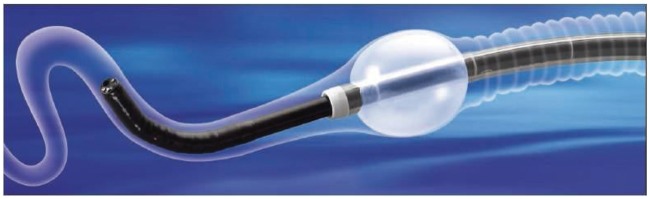
Figure 1.

Single-balloon enteroscope.
A 33-year-old female patient with a history of PJS presented for deep enteroscopy to evaluate for small bowel polyps. She complained of intermittent mid-abdominal pain. Small bowel follow through and capsule endoscopy showed significant polyp burden with size ranging from 5 mm to 3 cm primarily in the proximal and mid jejunum. Thrice in the past she had resections of her small bowel for polyps; on one occasion this was an emergency procedure due to obstruction. This time the patient had severe reservations against surgery. She also had a history of severe latex allergy with anaphylaxis and therefore we wanted to avoid DBE. We performed a series of four SBEs over a period of 1 year. Most of the large polyps >1 cm were removed (Figure 2). Some small polyps were also removed to clear the lumen and visibility. All procedures lasted between 89 and 124 minutes and were done under monitored anesthesia care (MAC) without needing any intubation. Roth nets were used to retrieve polyps. The enteroscope was inserted to a greater depth with each procedure and a depth of 300 cm from the ligament of Treitz was achieved during the last procedure. Capsule and CT enterography were performed intermittently to reassess polyp burden. We encountered one complication of bleeding after polypectomy that was managed conservatively. Histopathology of her polyps was confirmed to be hamartomatous with no adenomatous or malignant polyps.
Figure 2.
Polyps snaring.
SBE is a novel technique of enteroscopy. The enteroscope currently available, Olympus SIF- Q180®, uses one balloon to pleat the small bowel over the overtube while the tip of the endoscope is utilized for stabilization by hooking against bowel folds. The main advantages of SBE over DBE are ease of setup, shorter procedure time and lower operative cost [Upchurch et al. 2010] while maintaining the same therapeutic and diagnostic yield. Further, initial reports have suggested lower incidence of complications particularly pancreatitis with the use of SBE [Aktas et al. 2010; Upchurch et al. 2010; Sharma et al. 2011], however data is still limited. One main advantage of SBE is the use of a nonlatex balloon and hence it can be used in patients with latex allergy.
Patients with PJS have hamartomatous polyps throughout the GI tract and the number can range from 1 to 20 per segment of bowel. These polyps have a small potential for malignant transformation. However, they frequently present with complications such as intussusceptions, bleeding or obstruction requiring multiple emergency surgeries, increasing the risk for postoperative complications and short-gut syndrome. Recently published guidelines recommend surveillance for small bowel polyps by video capsule endoscopy (VCE) starting at 8 years of age every 3 years [Beggs et al. 2010]. When detected, removal of these polyps has traditionally been done surgically either by laparotomy or through intra-operative endoscopy. To avoid surgical morbidity an endoscopic approach would be ideal; however, due to the length of the small bowel, standard endoscopy is ineffective. DBE and SBE are two currently available techniques for diagnostic and therapeutic small bowel enteroscopy. Multiple studies have been published regarding successful use of DBE [Hsu et al. 2010; Chen et al. 2011; Sakamoto et al. 2011]; however, only very limited data is available regarding the use of SBE for prophylactic radical polypectomy from the small bowel in PJS patients. Since both balloons in DBE are made of latex, we were obligated to use SBE since our patient had severe latex allergy. The patient was counseled about the procedure and was also given an option for surgical referral. In total, four sessions were required to remove most of the polyps over the period of 1 year. Bleeding was encountered after the last procedure, which was managed conservatively and did not require any further intervention. Repeat enterography demonstrated very low polyp burden after the completion.
Our experience suggests that SBE can be utilized for polypectomy in patients with PJS especially in patients where DBE cannot be used for various reasons. However, further studies are required to explore the safety and efficacy of the procedure in comparison with DBE and surgical techniques to reduce tumor burden and complications.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare no conflicts of interest in preparing this article.
Contributor Information
Piyush Aggarwal, Creighton University Medical Center, 601 North 30th Street, Suite 3700, Omaha, NE 68154, USA.
Veena Kumaravel, Cleveland Clinic, Cleveland, OH, USA.
Bennie R. Upchurch, Creighton University Medical Center, Omaha, NE, USA
References
- Aktas H., De Ridder L., Haringsma J., Kuipers E.J., Mensink P.B. (2010) Complications of single-balloon enteroscopy: a prospective evaluation of 166 procedures. Endoscopy 42: 365–368 [DOI] [PubMed] [Google Scholar]
- Beggs A.D., Latchford A.R., Vasen H.F., Moslein G., Alonso A., Aretz S., et al. (2010) Peutz–Jeghers syndrome: a systematic review and recommendations for management. Gut 59: 975–986 [DOI] [PubMed] [Google Scholar]
- Chen T.H., Lin W.P., Su M.Y., Hsu C.M., Chiu C.T., Chen P.C., et al. (2011) Balloon-assisted enteroscopy with prophylactic polypectomy for Peutz-Jeghers syndrome: experience in Taiwan. Dig Dis Sci 56: 1472–1475 [DOI] [PubMed] [Google Scholar]
- Gao H., Van Lier M.G., Poley J.W., Kuipers E.J., Van Leerdam M.E., Mensink P.B. (2010) Endoscopic therapy of small-bowel polyps by double-balloon enteroscopy in patients with Peutz-Jeghers syndrome. Gastrointest Endosc 71: 768–773 [DOI] [PubMed] [Google Scholar]
- Hsu T.C., Lee T.C., Chiu H.M., Wu J.F., Yen T.J., Hsiao T.H., et al. (2010) Radical endoscopic polypectomy combined with double-balloon enteroscopy and colonoscopy for Peutz-Jeghers syndrome. J Pediatr Gastroenterol Nutr 51: 370–372 [DOI] [PubMed] [Google Scholar]
- Sakamoto H., Yamamoto H., Hayashi Y., Yano T., Miyata T., Nishimura N., et al. (2011) Nonsurgical management of small-bowel polyps in Peutz-Jeghers syndrome with extensive polypectomy by using double-balloon endoscopy. Gastrointest Endosc 74: 328–333 [DOI] [PubMed] [Google Scholar]
- Sharma M.K., Sharma P., Garg H., Sehgal L., Bhatia V. (2011) Clinical acute pancreatitis following anterograde single balloon enteroscopy. Endoscopy 43(Suppl. 2): E20–E21 [DOI] [PubMed] [Google Scholar]
- Upchurch B.R., Sanaka M.R., Lopez A.R., Vargo J.J. (2010) The clinical utility of single-balloon enteroscopy: a single-center experience of 172 procedures. Gastrointest Endosc 71: 1218–1223 [DOI] [PubMed] [Google Scholar]