Abstract
Plication techniques are not a panacea for deformities associated with Peyronie’s disease or congenital curvature. However, they do provide certain advantages, both theoretic and real, over competing procedures such as grafting. Depending on the technique, plication procedures have minimal risk of de novo erectile dysfunction, minimal risk of injury to the dorsal neurovascular bundle, and may be used for a variety of angulation deformities, including multiplanar curvature and severe degrees of curvature. A variety of incisions may be used, including the classic circumcision with degloving but also ventral raphe, dorsal penile inversion, and penoscrotal. These may be helpful in preventing postoperative morbidity and in sparing the prepuce if desired. Plication may also be combined with procedures such as penile prosthesis for correction of residual curvature. Lastly, despite its complications, plication techniques are very well tolerated, are relatively simple to perform and result in the very high satisfaction rates.
Keywords: Peyronie’s disease, corporoplasty, plication, grafting, erection, chordee, penis
Background
Peyronie’s disease (PD) is an acquired inflammatory condition of the tunica albuginea related to abnormal development of fibrotic, nonexpansile scars of the tunica albuginea. These scars, referred to as plaques, can present as a protean variety of penile deformities. Patients may present with penile mass, pain, or deformity; deformity may preclude coitus. In many men, PD is accompanied by lack of erectile rigidity. Historically, the symptomatic incidence has been estimated at 1%, but modern studies and the introduction of widely used treatments for erectile dysfunction demonstrate that the overall incidence is increasing and now is conservatively estimated at 4–5% [El Sakka, 2006; Kadioglu et al. 2004; Mulhall et al. 2004; Sommer et al. 2002]. It is commonly found in men between the ages of 40 and 70 years, although it can affect younger patients as well [LaRochelle and Levine, 2007; Tal et al. 2012].
The natural history of PD includes active and stable phases. Although the natural history of PD is not completely understood, the commonly held view that PD often spontaneously regresses has been challenged by recent studies [LaRochelle and Levine, 2007]. In a large study of untreated patients with PD presenting with penile curvature, only 12% felt that there was spontaneous improvement, while 40% and 48% noticed stable or worsening disease with time, respectively [Akin-Olugbade and Mulhall, 2007]. Men with restrictive deformity or who have active/progressive disease should be offered some form of stabilizing therapy. Many patients only require reassurance, while more invasive treatments such as surgery are infrequently necessary. For those who do need therapy, there are both medical and surgical options. In this chapter, we will exclusively focus on plication as a surgical approach to the management of PD and other causes of penile curvature, and will attempt to review the more recent literature regarding outcomes and complications of plication procedures.
In addition to PD, curvature of the penis may be a congenital or an acquired deformity. Congenital deformities include chordee (with or without associated hypospadias) and congenital curvature. The former is typically associated with abnormalities of the tissue planes and/or the corpus spongiosum, while the latter results from asymmetric expansion of the corpora cavernosa. Acquired curvature can be a result of overzealous circumcision, other penile surgeries, or trauma to the penis, such as buckling trauma during intercourse or overt penile fractures. PD is one form of an acquired curvature of the penis, and is not considered to be congenital.
Appreciation of the anatomy of the tunica albuginea and the corpora is important in understanding the etiology and the potential treatments of PD. The tunica albuginea is bilaminar, with an outer longitudinal layer and an inner circular layer. The outer longitudinal layer attenuates in the ventral midline, and thus the tunica is monolaminar at that point. It is also thin at the lateral aspects of the corpora. It is thickest on the dorsum and at the ventrum adjacent to the corpus spongiosum. The tunica albuginea varies in thickness from 1.5 to 3.0 mm. Supporting fibers from the incomplete septum of the corpora are attached to the inner layer of the tunica along the dorsal and ventral midlines. Plaques occur in the tunica albuginea at the site of the septal attachments. Despite the tunica being thickest in the region, most scars of PD develop on the dorsal aspect of the corpora [Brock et al. 1997].
The etiology of PD is controversial. The most widely accepted theory is that an injury to the penis, causing a buckling or tearing of the tunica albuginea, results in the disruptions of blood vessels, leading to an inflammatory response with subsequent remodeling of the connective tissue into fibrosis. The resultant deformity, caused by fibrotic inelastic tunica, predisposes the area to further injury.
Treatment for PD is aimed at achieving an erection that allows for successful and pain-free coitus for both patient and partner. The decision on how best to approach treatment of PD is often challenging. A candid discussion with the patient and his partner is a necessity to elucidate acceptability of current and potential deformity, goals of treatment if medical or surgical options are entertained, complications associated with treatment, and realistic expectations of outcomes. The decision to actively treat is typically based on multiple factors, including patient age, degree of deformity, associated erectile dysfunction (ED) and its onset in relation to development of PD, degree of pain with erection or intercourse, partner satisfaction or pain with intercourse, inability to penetrate, cosmetic displeasure, and the phase of plaque maturation. That being said, it is essential to take a thorough medical and sexual history and to perform a complete physical exam, including objective measurements of penile curvature at maximal rigidity, as it has been well documented that many patients tend to overestimate the degree of their curvature [Bacal et al. 2009] (see below for further discussion).
Fortunately, not all patients need treatment because some will maintain good erectile function and only have mild curvature that does not preclude coitus. These patients should receive reassurance and expectant management. For those with more debilitating forms of the disease, many active treatment options exist, including medical and surgical therapies. Surgical therapy is reserved for only patients with deformity that precludes intercourse or is associated with significant ED. Thus, the goal of surgical therapy is to restore an erection that is sufficiently straight and rigid for coitus. In an effort to minimize the risk of postoperative recurrence, surgery is delayed in these patients until the plaque has matured and the curvature has stabilized.
Surgical therapy can be classified into three main categories: tunical shortening procedures, tunical lengthening procedures, and penile prosthetics [Tornehl and Carson, 2004]. This nomenclature can be somewhat misleading, as not all patients undergoing tunical shortening procedures notice postprocedural loss of penile length, and likewise, most patients undergoing tunical lengthening procedures do not enjoy a longer phallus post procedurally. Independent of curvature, PD commonly causes penile shortening as a result of the fibrotic, inelastic, and nonexpansible scarring of the tunica albuginea. Theoretically, incision or excision of the plaque with grafting of the defect should correct this issue. Unfortunately, there are changes in the tunica albuginea and underlying corporal tissue, and most data demonstrate that grafting procedures have not invariably resulted in reclamation of lost penile length caused by the disease process itself [Perovic and Djinovic, 2010]. It is best to attempt to explain this to the patient prior to any surgical procedure so that postoperative expectations are realistic.
The decision on which procedure is best suited for the patient must take into account many patient factors, such as erectile rigidity, use and effect of pharmacologic therapies for ED, degree of curvature, baseline penile length taking into account the patient’s curvature, and patient comfort with the various surgical options. While many have suggested that the tunical shortening procedure be reserved only for patients with adequate preoperative potency, rigidity, penile length (>13cm), predicted postoperative penile length loss of less than 20%, and penile curvature less than 60° [Kadioglu et al. 2001; Langston and Carson, 2011; Levine and Lenting, 1997], it is our belief that plication can be successfully employed in patients with more significant disease. At our institution, we find plication to be a very versatile technique that can be employed in a variety of clinical scenarios, and we routinely plicate men with curvature approaching 90°, those with significant hourglass deformities, and those with ED but rigidity that is adequate for penetration.
Surgical plication options for Peyronie’s disease
Tunical shortening procedures include incisional/excisional corporoplasty techniques and nonincisional plication techniques. They are all referred to as ‘shortening procedures’ because straightening of the corpora is achieved by shortening or tightening of the convex side of the tunica albuginea.
Two corporoplasty techniques include the Nesbit procedure and the Yachia technique. In the 1960s, Nesbit conceived a surgical treatment for congenital curvature of the penis in which an ellipse of tunica on the convex side is excised and the remaining defect closed horizontally with nonabsorbable suture [Nesbit, 1965]. It was adapted in the late 1970s as a treatment for PD as well [Pryor and Fitzpatrick, 1979]. In the 1990s, Yachia described his modification of the Nesbit procedure, in which one or more longitudinal incisions is made in the convex tunica and then closed in a horizontal, Heineke-Mikulicz fashion [Yachia, 1990].
Corporal plication without incision or excision of the plaque gained acceptance after its successful use and description by Essed and Schröder [Essed and Schröder, 1985. An example is the modified tunica albuginea plication (TAP), which Levine adapted from the originally described procedure by Baskin and Duckett [Levine, 2007; Baskin and Duckett, 1994]. In the TAP procedure, based on the direction of curvature, partial thickness incisions in the outer layer of the tunica, and tunical shaving if needed, are performed. This is followed by suture plication between the incisions in a vertical mattress fashion. Other techniques have tried avoiding tunical incisions, focusing purely on suture plication for straightening. An example is the Lue ‘16 dot’ plication technique in which nonabsorbable, braided suture is used to plicate the convex tunica around the point of maximal curvature drawn on the convex tunica during an artificial erection [Gholami and Lue, 2002]. This procedure may be accomplished through a variety of incisions (see Figures 1–15) including the classic circumcision with degloving, a ventral raphe, or a dorsal base with penile inversion. The results of this technique have been encouraging and we have adopted this procedure in our institution for most patients. Likewise, the multiple parallel plication (MPP) technique does not involve incision or removal of the tunica, but simply utilizes multiple deep plication sutures into the tunica at the point of maximal curvature [Baskin and Lue, 1998]. More recently, Dugi and Morey described a minimally invasive approach to tunical plication, in which a 2 cm longitudinal penoscrotal incision is used to perform plication with parallel series of braided nonabsorbable sutures in a vertical mattress fashion. Their results have been quite encouraging as well [Dugi and Morey, 2009].
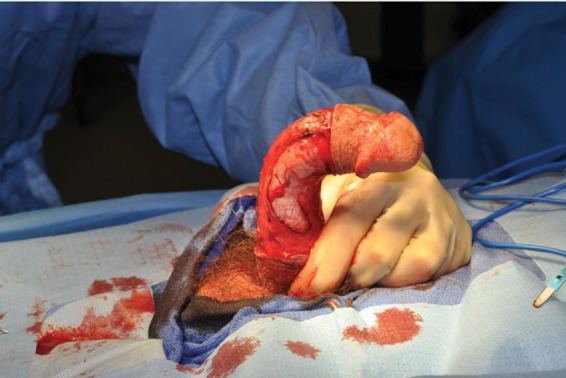
Figure 1.

Pharmacologic erection demonstrates the curvature intraoperatively.
Figure 2.

In this case, a longitudinal ventral raphe incision was chosen for a 16-dot procedure. The corpus spongiosum (to the right of the dots) and left-sided tunica albuginea are evident. Four of the ‘dots’ have been marked on the tunica.
Figure 3.

All of the dots have been made, and the sutures have been placed for the 16-dot procedure.
Figure 4.
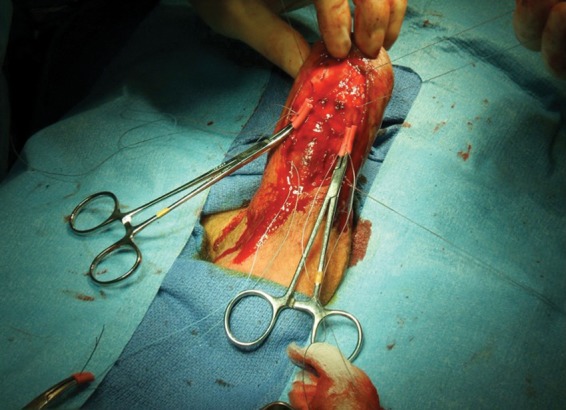
The suture knots have been partially placed proximally and are held in position by rubber shodded clamps.
Figure 5.

The knots have all been tied, demonstrating a straight phallus prior to closure.
Figure 6.

Intraoperative pharmacologic erection in an uncircumcised male who wished to preserve his prepuce.
Figure 7.

The same patient as Figure 6, with a straight phallus and a preserved prepuce.
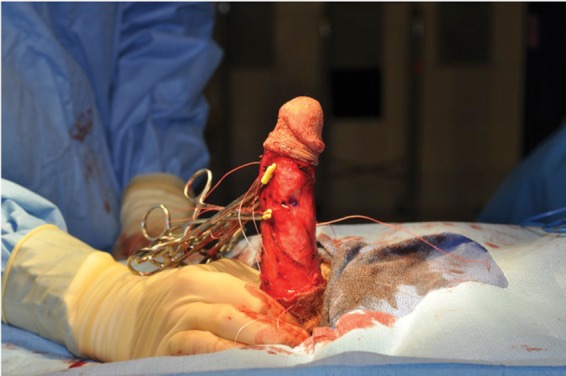
Figure 8.
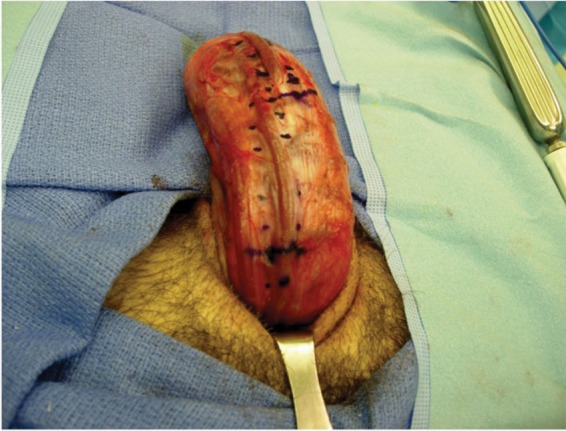
Long ventral curvature in an uncircumcised patient who wanted to preserve his prepuce. A dorsal, penile inversion approach was taken via an incision at the dorsal base. Since the patient had a long, gradual curve, a total of 24 dots were marked to correct his curvature.
Figure 9.

The same patient as Figure 8, with the sutures in place for correction. The deep dorsal vein as well as laterally mobilized dorsal nerve fibers are evident.
Figure 10.

The same patient as Figures 8 and 9, with a straight phallus and preserved prepuce.
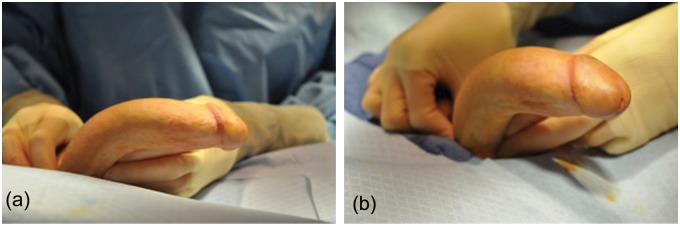
Figure 11.
(a, b) This patient has congenital curvature with multiplanar curvature.
Figure 12.

Same patient as Figure 11, a circumcision incision was employed and differential tension on the sutures resulted in a straight phallus.
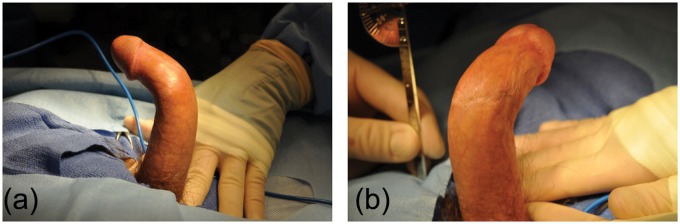
Figure 13.
(a) A different patient with a multiplanar Peyronie’s disease curvature. (b) Same patient with multiplanar curvature.
Figure 14.
Same patient as Figure 13, with planned ventral and lateral sutures to correct the multiplanar curvature.
Figure 15.
Shods are holding the knots, demonstrating correction of multiplanar deformity.
In addition to tunical lengthening procedures, which will be covered in a different article in this publication, penile prosthetics may be placed solo or can be combined with other procedures, such as modeling, incision and grafting, or plication either at the time of prosthetic placement or if curvature persists or recurs postoperatively. Prosthetics are typically used in the situation where there is significant loss of erectile rigidity such that straightening alone will not allow successful coitus. Concurrent plication and prosthesis placement has been shown to lead to durable cosmetic and functional results [Rahman et al. 2004], and is frequently employed in our patients with severe curvature and coexisting refractory ED.
Results of plication surgery for penile curvature
Each of the surgical techniques described above have a number of common postoperative findings that are well documented in the contemporary literature. Here we will limit our review to the literature discussing the complications and benefits of penile plication techniques for surgical correction of penile curvature. The most common postoperative complications are loss of length, recurrent or residual penile curvature, ED, change in penile sensation, and painful or palpable suture knots. Many of these outcomes can be quite distressing to the patient and may impact the operative technique that is selected and overall satisfaction postoperatively. Men considering a plication procedure should be counseled appropriately about these findings.
Loss of penile length:
Loss of penile length is a common complaint after penile plication surgery and can be quite distressing to the patient. Gholami and Lue found that in 132 patients undergoing the 16-dot procedure, 41% experienced objective shortening of the penis [Gholami and Lue, 2002]. The loss ranged from 0.5 to 1.5 cm and 7% of men stated that, subjectively, their loss of length affected sexual activity. In a series of 51 patients undergoing the Nesbit procedure, Andrews and colleagues found that 37.2% of patients had greater than 2 cm of shortening and, of these, 21% reported that the loss of length was significant enough to prevent intercourse [Andrews et al. 2001]. However, the method of measurement was not described in the study and it is unclear if length was objectively measured or if shortening was only patient reported. Leonardo and colleagues compared the Nesbit technique to the MPP technique and found that 100% of patients undergoing the Nesbit procedure had penile shortening versus only 73.5% in the MPP group, though this was not statistically significant (p = 0.19) [Leonardo et al. 2012]. Notably, none of the patients undergoing either procedure complained of loss of length that was clinically significant. Greenfield and colleagues reviewed the outcomes of 154 men who underwent the TAP procedure and found similar results, with an average objective loss of penile length of 0.36 cm with a range of 0–2.5 cm loss [Greenfield et al. 2006]. In this study, both degree of penile curvature and direction of curvature were found to be predictive of postoperative penile shortening. A greater degree of penile curvature was associated with an increased percent of mean length lost. When measured by mean percent of length lost, ventral curvature was associated with significantly more penile shortening than dorsal curvature, at 3.6% and 0.5%, respectively. The authors theorize that this may be confounded by the technique of measuring penile length, which was measured from the pubis to the corona; a ventral curvature may be more difficult to measure in this manner. Neither the age nor the primary pathology of the curvature, that is, PD versus chordee, was predictive of length loss. In both of these studies, the results were based on pre and postoperative measurement of the penis using stretched penile length to estimate the approximate erect length of the penis. This method had previously been demonstrated to provide a good surrogate for erect length [Wessells et al. 1996].
Table 1.
Complication rates after penile plication surgery (various plications included).
| Objective loss of penile length | 18–41% [Taylor and Levine, 2008; Gholami and Lue, 2002] |
| Subjective loss of penile length | 50–75% [Syed et al. 2003; Van Der Horst et al. 2004] |
| Loss of penile length affecting intercourse | 5–11.9% [Andrews et al. 2001; Syed et al. 2003] |
| Recurrent curvature requiring reoperation | 0–20% [Leonardo et al. 2012; Van Der Horst et al. 2004, Andrews et al. 2001; Baskin and Lue, 1998] |
| Worse erectile dysfunction | 0–6% [Van Der Horst et al. 2004; Gholami and Lue, 2002] |
| Change in penile sensation | 6–75% [Gholami and Lue, 2002; Syed et al. 2003; Leonardo et al. 2012] |
| Palpable suture knots (using nonabsorbable suture) | 50–100% [Van Der Hors et al. 2004; Baskin and Lue, 1998; Leonardo et al. 2012] |
| Sutures interfering with intercourse | 0–10% [Syed et al. 2003; Baskin and Lue, 1998] |
Several studies have reported patients’ subjective loss of length. Van Der Horst and colleagues reported that 74% of patients complained of subjective loss of length with the Essed–Schröder technique [Van Der Horst et al. 2004]. Syed and colleagues reported that after undergoing the Nesbit procedure 50% of patients noticed no change in penile length, 38.1% of patients felt they had a shorter penis but that this did not preclude intercourse, while another 11.9% had shortening severe enough that successful intercourse was impossible [Syed et al. 2003].
There are a number of techniques for measuring penile length. Standardization of measurement is a challenge in many studies, making interpretation of results difficult across studies. Although multiple series have reported subjective shortening of penile length, Taylor and Levine demonstrated that patients often overestimate this loss from an objective perspective [Taylor and Levine, 2008]. In their series of 61 patients undergoing TAP, 69% of patients reported subjective loss of length with an average perceived loss of 1.37 cm. However, only 18% of patients had an objective loss of length, with an average loss of 1.2 cm in these patients. Interestingly, when averaged as a group, the objective change in penile length was + 0.6 cm (range –3.5 to 3.5 cm). This outcome is unusual, as TAP should not augment penile length based on surgical and geometric principles. This finding may be a result of residual curvature or the method of measurement, but it is not explicitly explained in the paper. These results suggest that studies in which subjective length is reported may overestimate the actual length lost and should be interpreted with caution as the results may be deceiving. The fear of perceived loss may dissuade patients from a safe and successful technique for surgical correction of curvature. It may be helpful in preoperative counseling to measure penile length and demonstrate it to the patient so they have realistic expectations for postoperative outcomes, as it has been noted that only about 20% of patients are able to accurately estimate their penile curvature within 5° of objective measures [Bacal et al. 2009]. Although there is some controversy about which method is best, most practitioners prefer either a photograph taken at home that demonstrates the deformity or a pharmacologically induced erection in clinic that allows for real-time evaluation.
Recurrent and persistent curvature
As with all surgeries for PD deformity, there is an incidence of recurrence or persistence of curvature after plication procedures. The acceptable degree of curvature varies among surgeons and patients. Since the overall goal is successful and pain-free coitus, angulation of up to 30° may be considered acceptable by some. Other surgeons and patients may define success as 0° or only slight curvature. Others may focus predominantly on patient satisfaction and ability to have intercourse, regardless of degree of curvature. Several studies have been published reporting rates of recurrent or persistent curvature, though these outcomes are quite varied. Van Der Horst found that 12% of patients required reoperation for recurrent curvature after undergoing the Essed–Schröder tunical plication technique [Van Der Horst et al. 2004]. In this study, the degree of curvature was not identified, nor was the functional status. Leonardo and colleagues found that no patients who underwent the Nesbit procedure had significant relapse at a mean follow up of 141 months; 50% of patients had no curvature and 50% had minimal curvature of less than 30° at follow up [Leonardo et al. 2012]. The same study showed a 15.8% recurrence rate following the MPP technique. All of these cases were performed with the use of absorbable suture and all required surgical revision. There were no cases of recurrence in patients who had nonabsorbable suture. Overall, with the MPP technique, 68.4% of patients had optimal correction, while 31.6% had minimal deviation at the end of follow up. Notably, there was no significant difference between the two techniques with respect to rates of severe or mild recurrence of curvature.
Several studies do provide more objective data on timing of recurrence and measurable degree of curvature. Syed and colleagues found that with a median of 84 months of follow up for the Nesbit procedure, 61.9% and 28.6% of patients had no curvature or less than 30° curvature, respectively [Syed et al. 2003]. However, 9.5% of men had persistent, disabling curvature, which precluded coitus. In a review of Nesbit failure, Andrews and colleagues reported that 8.6% of patients had persistent or recurrent deformity greater than 30° [Andrews et al. 2001]. Of these cases, 9.6% presented immediately after surgery, 25.8% were initially straight but developed curvature at an average of 2.5 months, and 64.5% recurred at a mean of 11 months; early recurrence was thought to be the result of suture failure, whereas later recurrence was thought to be due to progressive PD. Surgical revision was required in 51.6% of patients with recurrent curvature.
Similarly, in a report on their small series of 10 patients utilizing the MMP technique, Baskin and Lue reported a 10% recurrence rate with at least 1 year of follow up [Baskin and Lue, 1998]. Overall, 80% of patients in this study were satisfied with the surgical outcome with respect to a self-documented straighter penis and a result satisfactory for intercourse. They noted that two patients (20%) requested reoperation for residual curvature of 15°; this residual curvature was considered to be a successful result by the authors and highlights the need for adequate preoperative counseling with regards to surgical outcomes.
Recently, there has been increased interest in the use of absorbable suture to help prevent the complication of palpable suture knots and associated postoperative pain (see discussion below). There have been reports of recurrent curvature following use of absorbable and nonabsorbable suture to perform corporal plication. While nonabsorbable suture remains the most commonly used for plication for fear of suture breakdown and recurrent curvature, there have been reports of successful use of absorbable suture. For example, Hsieh and colleagues reported on their use of absorbable suture in 114 patients undergoing plication. Overall 86% of patients had complete correction of curvature or less than 15° of residual curvature at 6 months postoperatively [Hsieh et al. 2007]. About 28% of patients had suture failure, defined as hearing a snap or feeling the penis pop. Despite evidence of suture failure, only half of these patients developed recurrent curvature and only a few felt it necessary to have a repeat operation. In a recent study by Parker and colleagues, six patients underwent plication with absorbable suture for mild to moderate penile curvature [Parker et al. 2012]. At a median of 7.2 months of follow up, three patients had no residual curvature and three patients had only 5–10° of residual curvature. Future studies should help further elucidate the role of absorbable sutures in plication surgery.
Erectile dysfunction
ED is a common finding in patients with penile curvature, especially in patients with curvature severe enough to require surgical correction. It can be challenging to determine if the cause of ED is a result of the disease process itself, other pre-existing conditions, or if it is secondary to surgical correction of the curvature. In their series of 50 patients undergoing Essed–Schröder tunical plication for either congenital penile deviation or PD, Van Der Horst and colleagues reported that 24% of patients had improved erectile function after correction of curvature and 24% had persistent ED; no patients had worsening of their ED [Van Der Horst et al. 2004]. Gholami and Lue, in a series of 132 patients undergoing the 16 dot plication, found that only 3% of patients complained of worse ED at 6 months postoperatively; this increased to 6% with follow up extending to as long as 6 years [Gholami and Lue, 2002]. It is unclear whether this loss of function over time is due to the corrective surgery or whether it represents loss of rigidity with aging and underlying disease processes.
Loss of sensation
Loss of sensation, particularly of the glans, occurs variably after plication. Most studies report on subjective hypoesthesia of the glans, as objective measurements are difficult. Reported rates of decreased penile sensation range from as low as 6% with the 16-dot plication technique to as high as 75% with the Nesbit procedure [Gholami and Lue, 2002; Leonardo et al. 2012]. Syed and colleagues found that 21.4% of patients with up to 84 months of follow up noted a change in penile sensation, predominantly at the glans [Syed et al. 2003]. None of these patients had loss of sensation severe enough to interfere with intercourse. While the exact etiology of this change is uncertain, a multifactorial etiology seemed possible and several theories were included in the paper, such as concomitant circumcision and dorsal dissection of the neurovascular bundle for correction of ventral penile curvature [Syed et al. 2003]. This may account for the low prevalence reported with the 16-dot procedure, as there is no dissection of the dorsal neurovascular bundles during correction of ventral curvature.
Discomfort of sutures
Traditionally, permanent sutures are utilized for penile plication because of the theoretical risk of recurrent curvature with suture failure or absorption. The knots in the permanent sutures are frequently palpable and have been noted to be painful in some patients. Van Der Horst and colleagues reported that 50% of patients were able to feel suture knots following the Essed–Schröder plication technique using polytetrafluoroethylene suture, and as many as 88% with the use of polypropylene suture [Van Der Horst et al. 2003]. Leonardo and colleagues reported that sutures were palpable in 75% and 100% following plication corporoplasty and the Nesbit technique, respectively [Leonardo et al. 2012]. Baskin and Lue reported that 100% of patients could palpate the suture following the MPP technique, in which a braided nonabsorbable suture was used [Baskin and Lue, 1998].
Though high numbers of patients can feel the sutures, the rates of the sutures being bothersome are significantly lower, ranging from 0 to 40%, regardless of suture material [Baskin, 1998; Gholami and Lue, 2002; Van Der Horst et al. 2003]. Very rarely does the discomfort of the suture interfere with sexual intercourse, with rates reported by Syed and colleagues and Baskin and Lue as 0% and10%, respectively [Syed et al. 2003; Baskin and Lue, 1998].
Recently, Basiri and colleagues performed a randomized trial with 38 men comparing absorbable and nonabsorbable sutures for corporal plication surgery. Both sutures resulted in acceptable correction of the curvature in 88% of patients. There was a trend favoring absorbable vicryl suture over nonabsorbable nylon with regards to patient satisfaction, though this was not significant [Basiri et al. 2011]. However, a significantly higher number of patients were able to palpate the suture material in the nylon group (39%) versus the vicryl group (6%), and this was statistically significant. There was no comment made on how much bother the patients experienced with palpable knots.
Patient satisfaction
Despite all of these postoperative findings after penile plication, it is important to stress the importance of patient satisfaction. Though many patients report discomfort, loss of length, diminished glans sensation and ED, most patients are satisfied with their results after surgery. In the study by Leonardo and colleagues comparing the Nesbit technique with plication corporoplasty, 75% and 68.5% were completely satisfied, 25% and 31.5 % were partially satisfied and none were dissatisfied, respectively [Leonardo et al. 2012]. Similarly, the results from Syed and colleagues were encouraging, with 76.2% of patients being satisfied with their Nesbit operation [Syed et al. 2003]. Geertsen and colleagues reported that 82% of patients were satisfied with their suture plication operation [Geertsen et al. 1996]; the majority of patients who were dissatisfied with this operation had preoperative ED, which did not improve postoperatively. Van Der Horst and colleagues found that 90% of patients were capable of sexual intercourse following Essed–Schröder plication and 78% of patients were satisfied with their surgery [Van Der Horst et al. 2004]. Of almost comparable importance, they also found that 78% of patients’ partners were satisfied with the surgical outcome. Taylor and Levine found that 82% of patients with TAP were either satisfied or very satisfied with their surgical outcome, and the majority of men would have chosen to do the surgery again knowing the outcome [Taylor and Levine, 2008].
In a study to evaluate the psychosocial impact of penile reconstructive surgery for congenital curvature, Tal and colleagues found that correction of curvature led to significant improvements in sexual relationships, overall relationships, confidence, libido, and satisfaction [Tal et al. 2010]. However, there was not any significant change in erectile function, consistent with data presented above. Interestingly, predictors of improvement in the above-mentioned domains were perceived complete straightness of the penis and preservation of penile length. Seemingly to the contrary, Cavallini and Caracciolo found that, while surgical straightening of the penis may improve ability to achieve vaginal intromission and subjective judgment of penile features, it did not necessarily improve interpersonal relationships or psychogenic ED [Cavallini and Caracciolo, 2008]. In this study, patient satisfaction with penile cosmesis improved from only 3.7% preoperatively to 83.3% postoperatively. Similarly, rates of comfortable vaginal intromission improved from 0% to 100% after surgery. However, despite these vast improvements, patients’ interpersonal relationships and rates of psychogenic ED did not improve after correction of their curvature. The authors caution that cosmetic surgery of the penis for the improvement of social relationships is dubious.
Conclusions
As demonstrated above, plication techniques are not a panacea for deformities associated with PD or congenital curvature. However, they do provide certain advantages, theoretic and real, over competing procedures such as grafting. Depending on the technique, plication procedures have minimal risk of de novo ED, minimal risk of injury to the dorsal neurovascular bundle, and may be used for a variety of angulation deformities, including multiplanar curvature and severe degrees of curvature [Brant et al. 2011]. A variety of incisions may be used, including the classic circumcision with degloving, but also ventral raphe, dorsal penile inversion, and penoscrotal. These may be helpful in preventing postoperative morbidity and in sparing the prepuce if desired. Plication may also be combined with procedures such as penile prosthesis for correction of residual curvature. Lastly, despite its complications, plication techniques are very well tolerated, are relatively simple to perform and result in very high satisfaction rates.
Footnotes
Funding: Dr Brant’s research is partially supported by a generous grant from the Joe W. and Dorothy Dorsett Brown Foundation.
Conflict of interest statement: The authors declare no conflicts of interest in preparing this article.
Contributor Information
Elizabeth M. Mobley, Division of Urology, University of Utah, Salt Lake City, UT, USA
Molly E. Fuchs, Division of Urology, University of Utah, Salt Lake City, UT, USA
Jeremy B. Myers, Center for Reconstructive Urology and Men’s Health, Division of Urology, University of Utah, Salt Lake City, UT, USA
William O. Brant, Center for Reconstructive Urology and Men’s Health, Division of Surgery (Urology), University of Utah, 30 N 1900 E, Room 3B420, Salt Lake City, UT, USA
References
- Akin-Olugbade Y., Mulhall J.P. (2007) The medical management of Peyronie’s disease. Nat Clin Pract Urol 4: 95–103 [DOI] [PubMed] [Google Scholar]
- Andrews H.O., Al-Akraa M., Pryor J.P., Ralph D.J. (2001) The Nesbit operation for Peyronie’s disease: an analysis of the failures. Br J Urol Int 87: 658–660 [DOI] [PubMed] [Google Scholar]
- Bacal V., Rumhor J., Sturm R., Lipshutz L.I., Schumacher M., Grober E.D. (2009) Correlation of degree of penile curvature between patient estimates and objective measures among men with Peyronie’s disease. J Sex Med 6: 862–865 [DOI] [PubMed] [Google Scholar]
- Basiri A., Sarhangnejad R., Ghahestani S.M., Radfar M.H. (2001) Comparing absorbable and nonabsorbable sutures in corporal plication for treatment of congenital penile curvature. Urol J 8: 302–305 [PubMed] [Google Scholar]
- Baskin L.S., Duckett J.W. (1994) Dorsal tunica albuginea plication for hypospadias curvature. J Urol 151: 1668–1671 [DOI] [PubMed] [Google Scholar]
- Baskin L.S., Lue T.F. (1998) The correction of congenital penile curvature in young men. Br J Urol 81: 895–899 [DOI] [PubMed] [Google Scholar]
- Brant W.O., Mobley E.M., Taylor M.B., Myers J.B. (2011) Emergent repair of congenital penile curvature for unconsummated marriage. J Sex Med 9: 3421699671 [Google Scholar]
- Brock G., Hsu G.L., Nunes L., von Heyden B., Lue T.F. (1997) The anatomy of the tunica albuginea in the normal penis and Peyronie’s disease. J Urol 157: 276–281 [PubMed] [Google Scholar]
- Cavallini G., Caracciolo S. (2008) Pilot study to determine improvements in subjective penile morphology and personal relationships following a Nesbit plication procedure for men with congenital penile curvature. Asian J Androl 10: 512–519 [DOI] [PubMed] [Google Scholar]
- Dugi D.D., Morey A.F. (2009) Penoscrotal plication as a uniform approach to reconstruction of penile curvature. Br J Urol Int 105: 1440–1444 [DOI] [PubMed] [Google Scholar]
- El Sakka A.I. (2006) Prevalence of Peyronie’s disease among patients with erectile dysfunction. Eur Urol 49: 564–569 [DOI] [PubMed] [Google Scholar]
- Essed E., Schröder F.H. (1985) New surgical treatment for Peyronie disease. Urology 25: 582–587 [DOI] [PubMed] [Google Scholar]
- Geertsen U.A., Brok K.E., Andersen B., Nielsen H.V. (1996) Peyronie curvature treated by plication of the penile fasciae. Br J Urol 77: 733–735 [DOI] [PubMed] [Google Scholar]
- Gholami S.S., Lue T.F. (2002) Correction of penile curvature using the 16-dot plication technique: a review of 13 patients. J Urol 167: 2066–2069 [PubMed] [Google Scholar]
- Greenfield J.M., Lucas S., Levine L.A. (2006) Factors affecting the loss of length associated with tunica albuginea plication for correction of penile curvature. J Urol 175: 238–241 [DOI] [PubMed] [Google Scholar]
- Hseih J.T., Liu S.P., Chen Y., Chang H.C., Yu H.J., Chen C.H. (2007) Correction of congenital penile curvature using modified tunical plication with absorbable sutures: the long-term outcome and patient satisfaction. Eur Urol 52: 261–266 [DOI] [PubMed] [Google Scholar]
- Kadioglu A., Küçükdurmaz F., Sanli O. (2001) Current status of the surgical management of Peyronie’s disease. Nat Rev Urol 8: 95–106 [DOI] [PubMed] [Google Scholar]
- Kadioglu A., Oktar T., Kandirali E., Kendirci M., Sanli O., Ozsoy C. (2004) Incidentally diagnosed Peyronie’s disease in men presenting with erectile dysfunction. Int J Impot Res 16: 540–543 [DOI] [PubMed] [Google Scholar]
- Langston J.P., Carson C.C. (2011) Peyronie’s disease: plication or grafting. Urol Clin North Am 38: 207–216 [DOI] [PubMed] [Google Scholar]
- LaRochelle J.C., Levine L.A. (2007) A survey of primary care physicians and urologists regarding Peyronie’s disease. J Sex Med 4: 1167–1173 [DOI] [PubMed] [Google Scholar]
- Leonardo C., De Nunzio C., Michetti P., Tartaglia N., Tubaro A., De Dominicis C., et al. (2012) Plication corporoplasty versus Nesbit operation for the correction of congenital penile curvature. A long-term follow-up. Int Urol Nephrol 44: 55–60 [DOI] [PubMed] [Google Scholar]
- Levine L.A. (2007) Penile straightening with the tunica albuginea plication procedure. In: Levine L.A. (ed.) Peyronie’s Disease: A Guide to Clinical Management. Totowa, NJ: Humana Press, pp; 151–159 [Google Scholar]
- Levine L.A., Lenting E.L. (1997) A surgical algorithm for the treatment of Peyronie’s disease. J Urol 158: 2149–2152 [DOI] [PubMed] [Google Scholar]
- Mulhall J.P., Creech S.D., Boorjian S.A., Ghaly S., Kim E.D., Moty A., et al. (2004) Subjective and objective analysis of the prevalence of Peyronie’s disease in a population of men presenting for prostate cancer screening. J Urol 171: 2350–2353 [DOI] [PubMed] [Google Scholar]
- Nesbit R.M. (1965) Congenital curvature of the phallus: report of three cases with description of corrective operation. J Urol 93: 230–232 [DOI] [PubMed] [Google Scholar]
- Parker J., Martinez D., Carrion R. (2011) Penile plication for Peyronie’s disease utilizing absorbable suture. Abstract presented at the annual Sexual Medicine Society of North America Meeting. J Sex Med 9: 9 [Google Scholar]
- Perovic S.V., Djinovic R.P. (2010) Current surgical management of severe Peyronie’s disease. Arch Esp Urol 63: 755–770 [PubMed] [Google Scholar]
- Pryor J.P., Fitzpatrick J.M. (1979) A new approach to the correction of penile deformity in Peyronie’s disease. J Urol 122: 622–623 [DOI] [PubMed] [Google Scholar]
- Rahman N.U., Carrion R.E., Bochinski D., Lue T.F. (2004) Combined penile plication surgery and insertion of penile prosthesis for severe penile curvature and erectile dysfunction. J Urol 171: 2346–2349 [DOI] [PubMed] [Google Scholar]
- Sommer F., Schwarzer U., Wassmer G., Bloch W., Braun M., Klotz T., et al. (2002) Epidemiology of Peyronie’s disease. Int J Impot Res 14: 379–383 [DOI] [PubMed] [Google Scholar]
- Syed A.H., Abbasi Z., Hargreave T.B. (2003) Nesbit procedure for disabling Peyronie’s curvature: a median follow-up of 84 months. Urology 60: 999–1003 [DOI] [PubMed] [Google Scholar]
- Tal R., Hall M.S., Alex B., Choi J., Mulhall J.P. (2012) Peyronie’s disease in teenagers. J Sex Med 9: 302–308 [DOI] [PubMed] [Google Scholar]
- Tal R., Nabulsi O., Nelson C.J., Mulhall J.P. (2010) The psychosocial impact of penile reconstructive surgery for congenital penile deviation. J Sex Med 7: 121–128 [DOI] [PubMed] [Google Scholar]
- Taylor F.L., Levine L.A. (2008) Surgical correction of Peyronie’s disease via tunica albuginea plication or partial plaque excision with pericardial graft: long-term follow up. J Sex Med 5: 2221–2228 [DOI] [PubMed] [Google Scholar]
- Tornehl C.K., Carson C.C. (2004) Surgical alternatives for treating Peyronie’s disease. Br J Urol Int 94: 774–783 [DOI] [PubMed] [Google Scholar]
- Van Der Horst C., Martinez Portillo F.J., Melchior D., Bross S., Alken P., Juenemann K.P. (2003) Polytetrafluoroethylene versus polyproplene sutures for Essed-Schröder tunical plication. J Urol 170: 472–475 [DOI] [PubMed] [Google Scholar]
- Van Der Horst C., Martinez Portillo F.J., Seif C., Alken P., Juenemann K.P. (2004) Treatment of penile curvature with Essed-Schröder tunical plication: aspects of quality of life from the patients’ perspective. Br J Urol Int 93: 105–108 [DOI] [PubMed] [Google Scholar]
- Wessells H., Lue T.F., McAninch J.W. (1996) Penile length in the flaccid and erect states: guidelines for penile augmentation. J Urol 156: 995–997 [PubMed] [Google Scholar]
- Yachia D. (1990) Modified corporoplasty for the treatment of penile curvature. J Urol 143: 80–82 [DOI] [PubMed] [Google Scholar]