Even with provision of antiretroviral therapy and tuberculosis treatment, almost 50% of patients with bacteremic disseminated tuberculosis die within one month of hospitalization. This study characterizes survival, predictors of Mycobacterium tuberculosis bacteremia, and predictors of death.
Abstract
Background. Disseminated tuberculosis is a major health problem in countries where generalized human immunodeficiency virus (HIV) infection epidemics coincide with high tuberculosis incidence rates; data are limited on patient outcomes beyond the inpatient period.
Methods. We enrolled consecutive eligible febrile inpatients in Moshi, Tanzania, from 10 March 2006 through 28 August 2010; those with Mycobacterium tuberculosis bacteremia were followed up monthly for 12 months. Survival, predictors of bacteremic disseminated tuberculosis, and predictors of death were assessed. Antiretroviral therapy (ART) and tuberculosis treatment were provided.
Results. A total of 508 participants were enrolled; 29 (5.7%) had M. tuberculosis isolated by blood culture. The median age of all study participants was 37.4 years (range, 13.6–104.8 years). Cough lasting >1 month (odds ratio [OR], 13.5; P < .001), fever lasting >1 month (OR, 7.8; P = .001), weight loss of >10% (OR, 10.0; P = .001), lymphadenopathy (OR 6.8; P = .002), HIV infection (OR, undefined; P < .001), and lower CD4 cell count and total lymphocyte count were associated with bacteremic disseminated tuberculosis. Fifty percent of participants with M. tuberculosis bacteremia died within 36 days of enrollment. Lower CD4 cell count (OR, 0.88; P = .049) and lower total lymphocyte count (OR, 0.76; P = .050) were associated with death. Magnitude of mycobacteremia tended to be higher among those with lower CD4 cell counts, but did not predict death.
Conclusions. In the era of free ART and access to tuberculosis treatment, almost one half of patients with M. tuberculosis bacteremia may die within a month of hospitalization. Simple clinical assessments can help to identify those with the condition. Advanced immunosuppression predicts death. Efforts should focus on early diagnosis and treatment of HIV infection, tuberculosis, and disseminated disease.
Disseminated tuberculosis is a major health problem in countries where generalized human immunodeficiency virus (HIV) infection epidemics coincide with high tuberculosis incidence rates [1]. Disseminated tuberculosis often causes rapidly fatal illness in patients with immunologically advanced HIV disease and has persisted as a public health problem even since the expansion of HIV care and treatment programs [2, 3]. Because the median survival of patients with bacteremic disseminated tuberculosis following admission to hospital may be very short [3–5], early recognition and treatment are likely to be important to avert mortality [6]. However, the clinical diagnosis of disseminated tuberculosis may be challenging in areas with limited laboratory services [7, 8], as patients may present with nonspecific symptoms and signs, and classic radiographic features of pulmonary or miliary tuberculosis may be absent [4, 5, 9]. Consequently, the diagnosis is often overlooked and is a frequent postmortem finding among HIV-infected patients in areas with high rates of tuberculosis [1]. Where laboratory services are available, disseminated tuberculosis may be strictly defined as isolation of Mycobacterium tuberculosis from blood or bone marrow, from a liver biopsy specimen, or from specimens from ≥2 noncontiguous organs in a single patient [10, 11].
M. tuberculosis was first recognized as a cause of bloodstream infection almost a century ago [12, 13]. Today, when sought using mycobacterial blood culture techniques, M. tuberculosis is a leading cause of community-acquired bloodstream infection among febrile hospitalized patients in sub-Saharan Africa [4, 14–18] and Asia [5, 9]. In-hospital case fatality rates for bacteremic disseminated tuberculosis in the era before the widespread availability of antiretroviral therapy (ART) approached 50% [4]. Unfortunately, the median time to positivity for M. tuberculosis, even in continuously monitored blood culture systems, exceeds 3 weeks, limiting its value for clinical management [19, 20]. M. tuberculosis nucleic acid amplification tests (NAATs) following extraction of large volumes of whole blood show promise for more rapid diagnosis, but they need refinement to improve sensitivity and adaptation for low-resource settings [21]. Although patient survival after Mycobacterium avium complex bacteremia was established for HIV-infected persons during the 1990s [22], little is understood about the natural history of M. tuberculosis bacteremia beyond the inpatient period or during the era of widespread availability of ART in endemic countries.
In order to improve approaches to the clinical recognition of disseminated tuberculosis, to enhance our understanding of the natural history of the disease in the context of timely use of tuberculosis treatment and ART, and to improve identification of patients at greatest risk for death, we enrolled and followed up consecutive patients with M. tuberculosis bacteremia identified at 2 hospitals in Tanzania, a country experiencing a generalized HIV epidemic and high incidence of tuberculosis.
METHODS AND MATERIALS
Setting
Moshi (population, >144 000) is the administrative center of the Kilimanjaro Region (population, >1.4 million) in northern Tanzania and is situated at an elevation of approximately 890 meters above mean sea level. Malaria transmission intensity is low [23]. National adult HIV seroprevalence was estimated at 7.0% in 2003–2004 [24] and has since declined; national tuberculosis incidence was estimated at 297 cases per 100 000 persons in 2007 [25]. Kilimanjaro Christian Medical Centre (KCMC) is a consultant referral hospital with 458 inpatient beds serving several regions in northern Tanzania, and Mawenzi Regional Hospital (MRH), with 300 beds, is the regional hospital for Kilimanjaro. Together KCMC and MRH serve as the main providers of hospital care in the Moshi area. In 2008, KCMC admitted 22 099 patients and MRH admitted 21 763 patients.
Participants
Participants were prospectively identified from among adult and adolescent inpatients at KCMC and MRH from 10 March 2006 through 28 August 2010. As described elsewhere, all admitted patients aged ≥13 years and with oral temperatures of ≥38.0°C were invited to participate in the study [2]. From 31 August 2008, enrollment was restricted to those who also had HIV infection, subjective fever for >1 month, and weight loss of >10%. A standardized clinical history was taken and physical examination was performed on consenting patients by a trained clinical officer who was a member of the study team. Following cleansing of the skin with povidone iodine and isopropyl alcohol, blood was drawn for aerobic blood culture (10 mL) and for up to 3 simultaneous mycobacterial blood cultures (5 mL each) as well as for complete blood count, examination for blood parasites, and HIV antibody testing. For patients found to be HIV seropositive, CD4-positive T-lymphocyte count (CD4 cell count) was also measured. A chest radiograph was ordered for all patients and was reported using a standardized form by a radiologist. The results of all study investigations were provided immediately to the hospital clinical team to inform patient management. A discharge form was completed at the time of discharge from hospital that captured whether the patient died in hospital. Participants with M. tuberculosis bloodstream infection were referred for immediate initiation to tuberculosis chemotherapy and asked to return for follow-up by the study team monthly for 12 months. Those who did not return for follow-up visits were contacted by telephone and, if necessary, sought at home by a field worker. Deaths were recorded and standardized verbal autopsies were performed for outpatient deaths. Those with HIV infection were referred to an HIV care and treatment center. The timing of initiation of ART was at the discretion of the clinical team, although national guidelines recommended that patients with immunologically advanced HIV disease and tuberculosis start ART with stavudine, lamivudine, and efavirenz as early as 2 weeks after the initiation of the intensive phase of tuberculosis treatment [26].
Laboratory Methods
Complete blood count and differential were performed using the CellDyn 3500 automated hematology analyzer (Abbott Laboratories, Abbott Park, Illinois). Manual differentials were performed when necessary on blood films stained with Giemsa.
Blood culture bottles were assessed for volume adequacy by comparing the weight before and after inoculation with blood. BacT/ALERT standard aerobic (SA) and mycobacterial (MB) bottles were loaded into the BacT/ALERT 3D automated microbial detection system (bioMérieux, Durham, North Carolina) where they were incubated for 5 and 42 days, respectively. BACTEC Myco/F Lytic bottles (Becton Dickinson, Franklin Lakes, New Jersey) were incubated at 35°C for 42 days; bottle bottoms were examined for fluorescence daily using a Wood lamp. ISOLATOR10 lysis-centrifugation tubes were centrifuged and processed using the Wampole ISOSTAT/ISOLATOR Microbial System (Inverness Medical, Princeton, New Jersey), plated to Middlebrook 7H10 agar, and incubated at 35°C in 5% carbon dioxide for 42 days. An aliquot of the blood-broth mixture was removed from bottles flagged positive by the instrument or by inspection of the bottom, using a 1-mL tuberculin syringe for SA and 5-mL syringe with 19-gauge needle for MB and Myco/F Lytic. A portion was examined by Gram stain, Kinyoun stain (MB and Myco/F Lytic), and India ink stain when yeast-like morphology was observed. Aliquots were plated to solid medium according to stain results. Nonmycobacterial plates were examined daily for growth and subsequent isolation and identification according to standard techniques. Mycobacterial plates were examined weekly for growth. AccuProbe Culture Identification Test MTB and MAC kits (Gen-Probe, San Diego, California) were used to identify members of M. tuberculosis complex and M. avium complex; other Mycobacterium species were identified by a reference laboratory [27, 28]. Colonies growing on lysis-centrifugation plates were counted and colony-forming units per milliliter of blood were calculated.
HIV type 1 (HIV-1) antibody testing was performed on whole blood using both the Capillus HIV-1/HIV-2 (Trinity Biotech, Bray, Ireland) and Determine HIV-1/2 (Abbott Laboratories) rapid HIV antibody tests. The Capillus test was replaced with the SD Bioline HIV-1/2 3.0 (Standard Diagnostics, Kyonggi-do, Korea) on 4 March 2008 after a change in Tanzania Ministry of Health HIV testing guidelines. If rapid tests were discordant, the sample was tested with an enzyme-linked immunosorbent assay (ELISA; Vironostika Uni-Form II plus O Ab, bioMérieux). If the ELISA was negative, no further testing was done. If the ELISA was positive, a Western blot (Genetic Systems HIV-1 Western Blot kit, Bio-Rad, Hercules, California) was done to confirm [29]. The CD4 cell count was measured using the FACSCalibur system (Becton Dickinson).
During the study, the laboratory participated successfully in external quality assurance programs of the College of American Pathologists for serology, bacteriology, mycology, mycobacteriology, blood parasites, rapid HIV, and India ink; the Viral Quality Assurance program of the AIDS Clinical Trials Group for HIV-1 RNA polymerase chain reaction; and the United Kingdom National External Quality Assessment Service for flow cytometry.
Statistics
Data were entered using the Cardiff Teleform system (Cardiff, Vista, California) into an Access database (Microsoft Corp, Redmond, Washington). For continuous responses, analysis of variance was used to assess treatment difference between groups. For categorical data and binary responses, Cochran-Mantel-Haenszel test was performed to compare groups. Descriptive statistics for demographics and patient characteristic baseline were obtained for baseline comparability. A logistic regression analysis was performed to identify risk factors associated with death with bacteremic disseminated tuberculosis. An estimate of survival curve using the Kaplan-Meier method was computed. The log-rank test was performed to compare difference between 2 survival distributions. The Kendall τ correlation was used to measure the association between 2 groups. All statistical tests performed were 2-sided at the 5% level of significance. Statistical analyses were performed with SPSS software, version 12.0 (IBM SPSS, Chicago, Illinois).
Research Ethics
This study was approved by the KCMC Research Ethics Committee, the Tanzania National Institutes for Medical Research National Research Ethics Coordinating Committee, and an institutional review board of Duke University Medical Center.
RESULTS
Of 508 participants enrolled during the total study period, 29 (5.7%) had M. tuberculosis bacteremia and 25 (4.9%) had both M. tuberculosis bacteremia and complete clinical data available. Of the 29 with M. tuberculosis bacteremia, 9 (31.0%) had both a positive lysis-centrifugation blood culture and CD4 cell count available. Of the 25 with complete clinical data, 12 (48.0%) were identified during the period of unrestricted enrollment. The median age of all study participants was 37.4 years (range, 13.6–104.8 years) and 281 (56.2%) were female; 236 (46.5%) of the participants were HIV seropositive. Of HIV-infected patients, the median CD4 cell count was 111 cells/μL (range, 1–1105 cells/μL), 69 (29.2%) were taking trimethoprim-sulfamethoxazole prophylaxis, and 84 (35.6%) were receiving ART. Of all participants, 403 (79.3%) were enrolled during the period of unrestricted enrollment and 12 (2.9%) of these had M. tuberculosis bloodstream infection. The characteristics of these patients have been described elsewhere [2]. An additional 105 participants (20.7%) were enrolled during the period of restricted enrollment after 31 August 2008.
Characteristics of Participants With and Without Bacteremic Disseminated Tuberculosis
The characteristics of participants enrolled from 17 September 2007 through 31 August 2008 during the period of unrestricted enrollment with and without disseminated tuberculosis are shown in Table 1. All participants with M. tuberculosis bacteremia were HIV-infected. Cough lasting >1 month (odds ratio [OR], 13.5; P < .001), fever lasting >1 month (OR, 7.8; P = .001), weight loss of >10% (OR, 10.0; P = .001), lymphadenopathy (OR 6.8; P = .002), HIV infection (OR undefined; P < .001), and lower CD4 cell count and total lymphocyte count were associated with bacteremic disseminated tuberculosis.
Table 1.
Characteristics of Participants With and Without Bacteremic Disseminated Tuberculosis, Kilimanjaro Christian Medical Centre and Mawenzi Regional Hospital, 2007–2008
| No. (%) of Participantsa |
||||||
|---|---|---|---|---|---|---|
| Characteristic | All (n = 403) | Disseminated Tuberculosis (n = 12) | No Disseminated Tuberculosis (n = 391) | OR | (95% CI) | P Valueb |
| Age, years, median (range) | 37.0 (13.6–95.5) | 39.0 (21.2–55.7) | 36.1 (13.6–95.5) | … | … | .935 |
| Female sex | 217 (53.8) | 9 (75.0) | 208 (53.2) | 2.6 | (.70–9.9) | .150 |
| Ever treated for tuberculosis | 39 (9.7) | 2 (16.7) | 37 (9.5) | 1.9 | (.40–9.1) | .413 |
| Symptoms | ||||||
| Cough | 261 (64.8) | 10 (83.3) | 251 (64.2) | 2.8 | (.60–12.9) | .190 |
| Cough >1 month | 80 (19.9) | 9 (75.0) | 71 (18.2) | 13.5 | (3.6–51.2) | <.001 |
| Fever >1 month | 88 (21.8) | 8 (66.7) | 80 (20.5) | 7.8 | (2.3–26.5) | .001 |
| Hemoptysis | 22 (5.5) | 2 (16.7) | 20 (5.1) | 3.7 | (.76–18.1) | .105 |
| Dyspnea | 45 (11.2) | 3 (25.0) | 42 (10.7) | 2.8 | (.72–10.6) | .138 |
| Weight loss >10% | 99 (24.6) | 9 (75.0) | 90 (23.0) | 10.0 | (2.7–37.9) | .001 |
| Signs | ||||||
| Body mass index, median (range) | 21.0 (13.5–41.8) | 19.1 (15.5–33.3) | 21.1 (13.5–41.8) | … | … | .489 |
| Lymphadenopathy | 42 (10.4) | 5 (41.7) | 37 (9.5) | 6.8 | (2.1–22.6) | .002 |
| Systolic blood pressure, median (range), mm Hg | 112 (60–200) | 110 (84–146) | 112 (60–200) | … | … | .874 |
| Diastolic blood pressure, median (range), mm Hg | 70 (20–128) | 70.0 (51–103) | 70.0 (20–128) | … | … | .255 |
| Respiratory rate, breaths/minute, median (range) | 25 (14–137) | 28 (18–40) | 25 (14–137) | … | … | .562 |
| Oxygen saturation, %, median (range) | 96 (71–100) | 95 (88–99) | 96 (71 100) | … | … | .514 |
| Abnormal breath sounds | 165 (40.9) | 7 (58.3) | 158 (40.4) | 2.1 | (.64–6.6) | .223 |
| Crepitations | 178 (44.2) | 8 (66.7) | 170 (43.5) | 2.6 | (.77–8.8) | .124 |
| Absent breath sounds | 6 (1.5) | 0 (0.0) | 6 (1.5) | c | c | >.999 |
| Bronchial breathing | 57 (14.1) | 4 (33.3) | 53 (13.6) | 3.2 | (.93–11.0) | .066 |
| Pleural rub | 15 (3.7) | 1 (8.3) | 14 (3.6) | 2.5 | (.30–20.3) | .407 |
| Splenomegaly | 15 (3.7) | 0 (0.0) | 15 (3.8) | c | c | >.999 |
| Hepatomegaly | 32 (7.9) | 1 (8.3) | 31 (7.9) | 1.1 | (.13–8.5) | .959 |
| Abdominal mass | 9 (2.2) | 0 (0.0) | 9 (2.3) | c | c | >.999 |
| Glasgow coma score, median (range) | 15.0 (3.0–15.0) | 15.0 (14.0–15.0) | 15.0 (3.0–15.0) | … | … | .010 |
| Neck stiffness | 20 (5.0) | 1 (8.3) | 19 (4.9) | 1.8 | (.22–14.5) | .590 |
| Kernig sign positive | 0 (0.0) | 0 (0.0) | 0 (0.0) | c | c | >.999 |
| Skin lesion | 17 (4.2) | 0 (0.0) | 17 (4.3) | c | c | >.999 |
| BCG scar | 368 (91.3) | 12 (100.0) | 356 (91.0) | Und | Und | .611 |
| Laboratory findings | ||||||
| HIV infection | 157 (39.0) | 12 (100.0) | 147 (37.6) | Und | Und | <.001 |
| CD4 cell count, cells/μL, median (range) | 105 (1–1400) | 41 (3–179) | 112 (1–1400) | … | … | <.001 |
| Hemoglobin level, g/dL, median (range) | 8.3 (5.0–16.0) | 8.3 (6.0–11.0) | 8.0 (5.0–16.0) | … | … | .561 |
| Lab test results | ||||||
| Hematocrit level, %, median (range) | 25 (14–45) | 25 (18–33) | 27.40 (14–45) | … | … | .482 |
| Lab test results | ||||||
| Platelet count, 109 cells/L, median (range) | 213 (27–887) | 263 (168–887) | 202 (27–515) | … | … | .179 |
| Neutrophil count, 109 cells/L, median (range) | 4.6 (0.1–88.2) | 5.4 (0.7–9.8) | 4.5 (0.1–88.2) | … | … | .119 |
| Lymphocyte count, 109 cells/L, median (range) | 1.1 (0.0–7.0) | 0.8 (0.1–2.1) | 1.2 (0.0–7.0) | … | … | .007 |
| Chest radiograph | ||||||
| Normal | 15 (3.7) | 3 (25.0) | 12 (3.1) | 10.5 | (2.5–43.9) | .001 |
| Parenchymal abnormality | 14 (3.5) | 3 (25.0) | 11 (2.8) | 11.5 | (2.7–48.5) | .001 |
| Nodular abnormality | 5 (1.2) | 1 (8.3) | 4 (1.0) | 8.8 | (.91–85.3) | .061 |
| Pleural abnormality | 7 (1.7) | 2 (16.7) | 5 (1.3) | 15.4 | (2.7–89.4) | .002 |
| Central structure abnormality | 2 (0.5) | 1 (8.3) | 1 (0.3) | 35.5 | (2.1–604.3) | .014 |
Abbreviations: BCG, Bacille Calmette-Guérin; CI, confidence interval; HIV, human immunodeficiency virus; OR, odds ratio; Und, undefined.
a Data are no. (%) of participants unless stated otherwise.
b The P value is based on an independent t test with equal valance not assumed for continuous variables, χ2 test for categorical variables, and Fisher exact test for undefined OR.
c Numbers are too small to calculate a test statistic.
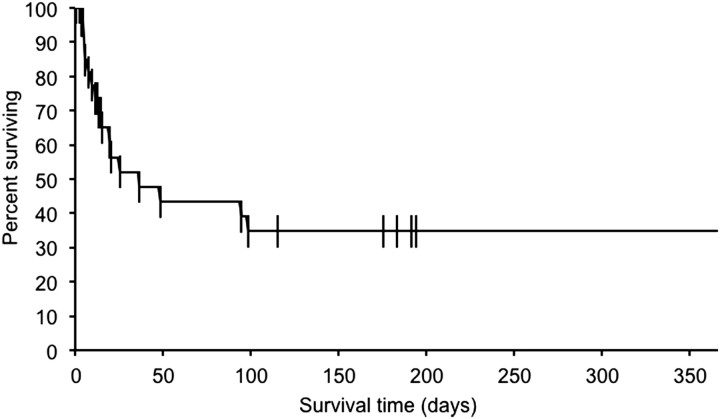
Outcome of Participants With Bacteremic Disseminated Tuberculosis
The survival curve for all participants with bacteremic disseminated tuberculosis is shown in Figure 1. Of participants with bacteremic disseminated tuberculosis, 50% died within 36 days of enrollment. There was no significant difference in survival between those enrolled before and those enrolled after 31 August 2008, when enrollment was restricted (P = .722).
Figure 1.
Survival curve of participants with bacteremic disseminated tuberculosis, Kilimanjaro Christian Medical Centre and Mawenzi Regional Hospital, 2006–2010 (n = 29).
Predictors of Death Among Participants With Bacteremic Disseminated Tuberculosis
Table 2 shows risk factors for death among participants with bacteremic disseminated tuberculosis. Lower CD4 cell count (OR, 0.89; P = .049) and lower total lymphocyte count (OR, 0.76; P = .050) were associated with death from disseminated tuberculosis.
Table 2.
Predictors of Death Among Participants With Bacteremic Disseminated Tuberculosis, Kilimanjaro Christian Medical Centre and Mawenzi Regional Hospital, 2006–2010 (n = 20)
| Variable | OR | P Value |
|---|---|---|
| Age | 1.0 | .578 |
| Sex | 0.60 | .583 |
| Fever >1 month | 0.00 | >.999 |
| Cough >1 month | 0.00 | .999 |
| Diarrhea >1 month | a | a |
| Weight loss >1 month | a | a |
| Receipt of antituberculosis drugs since current illness started | 0.00 | >.999 |
| Receipt of antiretroviral therapy since current illness started | 1.3 | .796 |
| Receipt of cotrimoxazole prophylaxis since current illness started | 0.60 | .538 |
| Years since first positive HIV test | 0.59 | .538 |
| Past treatment for tuberculosis | 0.00 | .999 |
| Years since first treated for tuberculosis | a | a |
| Temperature | 0.91 | .898 |
| Body mass index | 0.87 | .318 |
| Conjunctival pallor | 0.45 | .427 |
| Oral candidiasis | 6.7 | .120 |
| Lymphadenopathy | 2.9 | .287 |
| Blood pressure, systolic | 0.99 | .681 |
| Blood pressure, diastolic | 0.99 | .524 |
| Respiratory rate | 1.0 | .812 |
| Reduced oxygen saturation | 1.4 | .123 |
| Abnormal breath sounds | a | a |
| Presence of ascites | 0.80 | .881 |
| Hepatomegaly | 1.3 | .796 |
| Splenomegaly | a | a |
| Glasgow coma score | a | a |
| Neck stiffness | a | a |
| Kernig sign positive | a | a |
| Presence of herpes zoster scar | 0.70 | .812 |
| Presence of Kaposi sarcoma | 0.00 | >.999 |
| Presence of BCG scar | a | a |
| Abnormal chest radiograph | 0.42 | .512 |
| Presence of infiltrates on chest radiograph | 1.0 | 1.000 |
| Presence of nodules on chest radiograph | 0.00 | .999 |
| Presence of cavities on chest radiograph | 2.0 | .638 |
| Presence of pleural effusion on chest radiograph | 0.80 | .887 |
| Presence of hilar lymphadenopathy on chest radiograph | a | a |
| Presence of pericardial effusion on chest radiograph | a | a |
| HIV infection laboratory confirmed | 1.3 | .881 |
| CD4 cell count | 0.89 | .049 |
| Positive cryptococcal antigen test | a | a |
| Hemoglobin level | 1.2 | .584 |
| Hematocrit level | 1.1 | .499 |
| Total lymphocyte count | 0.76 | .050 |
| Platelet count | 1.0 | .226 |
| Raised neutrophil count | 1.1 | .226 |
| Blood culture time to positivity for M. tuberculosis | 1.0 | .720 |
| M. tuberculosis bacteremia magnitude | 1.1 | .272 |
For continuous variables, odds ratios are per unit increase in value.
Abbreviations: HIV, human immunodeficiency virus; OR, odds ratio.
a Unavailable due to missing values, or the variable is constant for all data.
Relationship Between Degree of HIV-Associated Immune Suppression and Magnitude of Mycobacteremia
Figure 2 shows the relationship between CD4 cell count and the magnitude of mycobacteremia, measured directly as colony-forming units per milliliter. The Pearson product-moment correlation coefficient for the relationship is −0.0486 with a P value of .155, and the Kendall τ correlation coefficient for the relationship is −0.333 with a P value of .497.
Figure 2.
Number of Mycobacterium tuberculosis colony-forming units per milliliter by CD4-positive T-lymphocyte count among participants with bacteremic disseminated tuberculosis, Kilimanjaro Christian Medical Centre and Mawenzi Regional Hospital, 2006–2010 (n = 9). Abbreviation: CFU, colony-forming unit.
DISCUSSION
We describe the survival of patients with bacteremic disseminated tuberculosis over 12 months of follow-up in a setting where ART and tuberculosis treatment are readily available. In this context, we demonstrate that bacteremic disseminated tuberculosis is often rapidly fatal, with almost one-half of affected patients dying within a month of enrollment. We find that a range of clinical and laboratory features may assist with the identification of patients with bacteremic disseminated tuberculosis. Those patients with immunologically advanced HIV disease are at greatest risk of death and also experience the highest magnitudes of mycobacteremia.
Although almost one-half of participants with bacteremic disseminated tuberculosis had died by 1 month of follow-up, the fact that more than one-third of participants were still alive after 1 year is cause for some optimism. It is likely that earlier identification of patients with disseminated tuberculosis may increase the proportion of long-term survivors. We have previously demonstrated that mycobacterial blood culture plays an increasingly important role in the diagnosis of disseminated tuberculosis in the United States [11]. However, the median time to positivity for M. tuberculosis in continuously monitored blood culture systems exceeds 3 weeks [19, 20]. Because bacteremic disseminated tuberculosis is rapidly fatal in a substantial proportion of patients before a mycobacterial blood culture instrument signals positivity, alternative approaches to facilitate early diagnosis are needed. M. tuberculosis NAATs on whole blood can yield results within a day, but improvements to sensitivity are needed to detect low-magnitude mycobacteremia [21].
Previous research has shown that a substantial group of patients with bacteremic disseminated tuberculosis may be identified by consistently applying a routine approach to tuberculosis clinical and laboratory diagnosis [6, 30]. However, a proportion of patients with disseminated disease will not be detected with a standard approach, and the size of this group appears to vary according to local clinical practices, laboratory services, and epidemiologic conditions [5, 6, 31, 32]. It is notable that a substantial minority of patients have a normal chest radiograph. We confirm that chronic cough and fever lasting >1 month, a history of weight loss of >10%, lymphadenopathy, and HIV infection [4, 17, 33] assist with the identification of patients with disseminated tuberculosis. Furthermore, among those patients with HIV infection, we demonstrate that lower CD4 cell count is a useful predictor of disseminated disease.
As far as we are aware, risk factors for death among patients with bacteremic disseminated tuberculosis have not previously been studied prospectively. Although the sample size was small, lower CD4 cell count and the related measure of lower total lymphocyte count were the only predictors of death identified among many evaluated by our study. Of interest, there was a trend of patients with bacteremic disseminated tuberculosis with immunologically advanced HIV disease having higher magnitudes of mycobacteremia. However, magnitude of mycobacteremia was not itself associated with increased risk for death. It is possible that host, organism, and clinical management factors not measured by our study could contribute to the outcome of survival. Although we did not study the role of M. tuberculosis genotype or antimicrobial resistance, the epidemiology of both has been described elsewhere among tuberculosis patients in northern Tanzania [34]. The most appropriate timing for initiation of ART among the subset of patients with bacteremic disseminated tuberculosis has not been specifically studied. However, randomized trials confirm that early initiation of ART is associated with improved outcomes in HIV and tuberculosis coinfected patients, with and without immunologically advanced disease [35–39]. Participants with tuberculosis identified in this study were recommended to have ART initiated 2 weeks after the start of treatment for tuberculosis [26], although clinician practices may have varied. It is not known whether M. tuberculosis bacteremia independently influences risk for the immune reconstitution inflammatory syndrome, and our study was not designed to answer this potentially important question.
The high case fatality rate of bacteremic disseminated tuberculosis underscores the importance of intervention earlier in the course of HIV infection and prior to the loss of immunologic control of tuberculosis among latently infected individuals or prior to dissemination in those with pulmonary infection. Provision and promotion of HIV counseling and testing services facilitates the early detection of HIV infection. Referral of HIV-infected individuals to healthcare services that identify and effectively treat active tuberculosis [40], treat latent tuberculosis infection [41], and initiate trimethoprim-sulfamethoxazole prophylaxis [42] and ART in a timely manner [43] may all contribute to a reduction in the number of persons presenting late with fatal disseminated tuberculosis. The use of empiric tuberculosis treatment in patients suspected to have disseminated tuberculosis can be considered and is an area where further research is needed [44].
Our study had a number of limitations. The number of patients with bacteremic disseminated tuberculosis identified was quite small, limiting our ability to identify minor risk factors. Nonetheless, our study was conducted over 4 years and likely represents one of the largest prospective studies on bacteremic disseminated tuberculosis yet reported. Although it was a component of the routine clinical care of study participants, the systematic collection of samples for routine diagnosis of pulmonary tuberculosis was not part of the study design, preventing assessment of sputum mycobacteriology as a predictor of disseminated tuberculosis. Our study was not designed to comprehensively evaluate host and organism factors associated with bacteremic disseminated tuberculosis. Future studies might build on our work by incorporating a pulmonary tuberculosis comparison arm, evaluating host genomic risk factors for extrapulmonary disease, and studying the role of M. tuberculosis genotype and antimicrobial resistance.
In conclusion, bacteremic disseminated tuberculosis is rapidly fatal in a large proportion of patients, especially those with immunologically advanced HIV disease. However, early recognition and consequently early initiation of potentially lifesaving treatment may be facilitated by careful clinical history, physical examination, and use of laboratory tests that are widely available at district hospitals in endemic areas [45]. Specific laboratory diagnosis can be augmented with mycobacterial blood culture, but assays yielding a more rapid result such as NAATs are needed to influence management in the first few days after presentation to a healthcare facility.
Notes
Acknowledgments. The authors thank Ahaz T. Kulanga for providing administrative support to this study; Pilli M. Chambo, Beata V. Kyara, Beatus A. Massawe, Anna D. Mtei, Godfrey S. Mushi, Lillian E. Ngowi, Flora M. Nkya, and Winfrida H. Shirima for reviewing and enrolling study participants; Gertrude I. Kessy, Janeth U. Kimaro, Bona K. Shirima, and Edward Singo for managing participant follow-up; and Evaline M. Ndosi and Enock J. Kessy for their assistance in data entry. We are grateful to the leadership, clinicians, and patients of KCMC and MRH for their contributions to this research.
Financial support. This research was supported by an International Studies on AIDS Associated Co-infections (ISAAC) award, a program funded by the National Institutes of Health (NIH) (U01 AI062563). Authors received support from NIH awards ISAAC (J. A. C., A. B. M., H. O. R., B. N. N., V. P. M., and J. A. B.); AIDS International Training and Research Program grant D43 PA-03-018 (J. A. C., H. O. R., B. N. N., V. P. M., and J. A. B.); the Duke Clinical Trials Unit and Clinical Research Sites grant U01 AI069484 (J. A. C., V. P. M., and J. A. B.); the Center for HIV/AIDS Vaccine Immunology grant U01 AI067854 (J. A. C. and J. A. B.); and the Duke Center for AIDS Research grant 2P30 AI064518 (J. A. B.). We acknowledge the Hubert-Yeargan Center for Global Health at Duke University for critical infrastructure support for the Kilimanjaro Christian Medical Centre–Duke University Collaboration.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed in the Acknowledgments section.
References
- 1.Lucas SB, Hounnou A, Peacock C, et al. The mortality and pathology of HIV infection in a West African city. AIDS. 1993;7:1569–79. doi: 10.1097/00002030-199312000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Crump JA, Ramadhani HO, Morrissey AB, et al. Invasive bacterial and fungal infections among hospitalized HIV-infected and HIV-uninfected adults and adolescents in northern Tanzania. Clin Infect Dis. 2011;52:341–8. doi: 10.1093/cid/ciq103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munseri PJ, Talbot EA, Bakari M, Matee M, Teixeira JP, Von Reyn CF. The bacteremia of disseminated tuberculosis among HIV-infected patients with prolonged fever in Tanzania. Scand J Infect Dis. 2011;43:696–701. doi: 10.3109/00365548.2011.577802. [DOI] [PubMed] [Google Scholar]
- 4.Archibald LK, den Dulk MO, Pallangyo KJ, Reller LB. Fatal Mycobacterium tuberculosis bloodstream infections in febrile hospitalized adults in Dar es Salaam, Tanzania. Clin Infect Dis. 1998;26:290–6. doi: 10.1086/516297. [DOI] [PubMed] [Google Scholar]
- 5.McDonald LC, Archibald LK, Rheanpumikankit S, et al. Unrecognised Mycobacterium tuberculosis bacteraemia among hospital inpatients in less developed countries. Lancet. 1999;354:1159–63. doi: 10.1016/s0140-6736(98)12325-5. [DOI] [PubMed] [Google Scholar]
- 6.Lewis DK, Peters RPH, Schijffelen MJ, et al. Clinical indicators of mycobacteremia in adults admitted to hospital in Blantyre, Malawi. Int J Tuberc Lung Dis. 2002;6:1067–74. [PubMed] [Google Scholar]
- 7.Archibald LK, Reller LB. Clinical microbiology in developing countries. Emerg Infect Dis. 2001;7:302–5. doi: 10.3201/eid0702.010232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petti CA, Polage CR, Quinn TC, Ronald AR, Sande MA. Laboratory medicine in Africa: a barrier to effective health care. Clin Infect Dis. 2006;42:377–82. doi: 10.1086/499363. [DOI] [PubMed] [Google Scholar]
- 9.Archibald LK, McDonald LC, Rheanpumikankit S, et al. Fever and human immunodeficiency virus infection as sentinels for emerging mycobacterial and fungal bloodstream infections in hospitalized patients >/=15 years old, Bangkok. J Infect Dis. 1999;180:87–92. doi: 10.1086/314836. [DOI] [PubMed] [Google Scholar]
- 10.Iseman MD. Extrapulmonary tuberculosis in adults: a clinician's guide to tuberculosis. 1st ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2000. pp. 145–97. [Google Scholar]
- 11.Crump JA, Reller LB. Two decades of disseminated tuberculosis at a university medical center: the expanding role of mycobacterial blood culture. Clin Infect Dis. 2003;37:1037–43. doi: 10.1086/378273. [DOI] [PubMed] [Google Scholar]
- 12.Clough MC. The cultivation of tubercle bacille from the circulation blood in miliary tuberculosis. Am Rev Tuberc. 1917;1:598–621. [Google Scholar]
- 13.Loewenstein E. Die züchtung der tuberkelbazillen aus dem strömenden blute. Zentralbl Bakteriol Parasitenkunde Infektionskrankheiten Hyg I Orig. 1931;120:127–9. [Google Scholar]
- 14.Gilks CF, Brindle RJ, Mwachari C, et al. Disseminated Mycobacterium avium infection among HIV-infected patients in Kenya. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;8:195–8. [PubMed] [Google Scholar]
- 15.Bell M, Archibald LK, Nwanyanwu O, et al. Seasonal variation in the etiology of bloodstream infections in a febrile inpatient population in a developing country. Int J Infect Dis. 2001;5:63–9. doi: 10.1016/s1201-9712(01)90027-x. [DOI] [PubMed] [Google Scholar]
- 16.McDonald LC, Archibald LK, Nwanyanwu O, Reller LB, Jarvis WR. Unrecognised Mycobacterium tuberculosis. Lancet. 2000;355:142–3. [Google Scholar]
- 17.Archibald LK, McDonald LC, Nwanyanwu O, et al. A hospital-based prevalence survey of bloodstream infections in febrile patients in Malawi: implications for diagnosis and therapy. J Infect Dis. 2000;181:1414–20. doi: 10.1086/315367. [DOI] [PubMed] [Google Scholar]
- 18.Reddy EA, Shaw AV, Crump JA. Community acquired bloodstream infections in Africa: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:417–32. doi: 10.1016/S1473-3099(10)70072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crump JA, Morrissey AB, Ramadhani HO, Njau BN, Maro VP, Reller LB. Controlled comparison of BacT/ALERT MB system, manual MYCO/F LYTIC, and ISOLATOR 10 system for detection of Mycobacterium tuberculosis bacteremia. J Clin Microbiol. 2011;49:3054–7. doi: 10.1128/JCM.01035-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crump JA, Tanner DC, Mirrett S, McKnight CM, Reller LB. Controlled comparison of BACTEC 13A and MYCO/F LYTIC, BacT/ALERT MB, and ISOLATOR 10 systems for detection of mycobacteremia. J Clin Microbiol. 2003;41:1987–90. doi: 10.1128/JCM.41.5.1987-1990.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crump JA, Tuohy MJ, Morrissey AB, et al. Performance of nucleic acid amplification following extraction of 5 mL of whole blood for the diagnosis of Mycobacterium tuberculosis bacteremia. J Clin Microbiol. 2012;50:138–41. doi: 10.1128/JCM.05963-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore RD, Chaisson RE. Natural history of opportunistic disease in an HIV-infected urban clinical cohort. Ann Intern Med. 1996;124:633–42. doi: 10.7326/0003-4819-124-7-199604010-00003. [DOI] [PubMed] [Google Scholar]
- 23.Hay SI, Guerra CA, Gething PW, et al. A world malaria map: Plasmodium falciparum endemnicity in 2007. PLoS Med. 2009;6:e1000048. doi: 10.1371/journal.pmed.1000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mishra V, Vaessen M, Boerma JT, et al. HIV testing in national population-based surveys: experience from the Demographic and Health Surveys. Bull World Health Organ. 2006;84:537–45. doi: 10.2471/blt.05.029520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization. Geneva, Switzerland: World Health Organization; 2009. Global tuberculosis control: epidemiology, strategy, financing: WHO report 2009. [Google Scholar]
- 26.National AIDS Control Programme. National Guidelines for Clinical Management of HIV/AIDS. Dar es Salaam, Tanzania: Ministry of Health and Social Welfare, Republic of Tanzania; 2008. p. 320. [Google Scholar]
- 27.van Ingen J, Tortoli E, Selvarangan R, et al. Mycobacterium sherrisii sp. nov.; a slow growing nonchromogenic species. Int J Syst Evol Microbiol. 2011;61:1293–8. doi: 10.1099/ijs.0.024752-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crump JA, Van Ingen J, Morrissey AB, et al. Invasive disease caused by nontuberculous mycobacteria, Tanzania. Emerg Infect Dis. 2009;15:53–5. doi: 10.3201/eid1501.081093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mayhood MK, Afwamba IA, Odhiambo CO, et al. Validation, performance under field conditions, and cost-effectiveness of Capillus HIV-1/HIV-2 and Determine HIV-1/2 rapid human immunodeficiency virus antibody assays using sequential and parallel testing algorithms in Tanzania. J Clin Microbiol. 2008;46:3946–51. doi: 10.1128/JCM.01045-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.von Reyn CF, Kimambo S, Mtei L, et al. Disseminated tuberculosis in human immunodeficiency virus infection: ineffective immunity, polyclonal disease and high mortality. Int J Tuberc Lung Dis. 2011;15:1087–92. doi: 10.5588/ijtld.10.0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Monkongdee P, McCarthy KD, Cain KP, et al. Yield of acid-fast smear and mycobacterial culture for tuberculosis diagnosis in people with human immunodeficiency virus. Am J Respir Crit Care Med. 2009;180:903–8. doi: 10.1164/rccm.200905-0692OC. [DOI] [PubMed] [Google Scholar]
- 32.Heysell SK, Thomas TA, Gandhi NR, et al. Blood cultures for the diagnosis of multidrug-resistant and extensively drug-resistant tuberculosis among HIV-infected patients from rural South Africa: a cross-sectional study. BMC Infect Dis. 2010;10:344. doi: 10.1186/1471-2334-10-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ssali FN, Kamya MR, Wabwire-Mangen F, et al. A prospective study of community-aquired bloodstream infections among febrile adults admitted to Mulago Hospital in Kampala, Uganda. J Acquir Immune Defic Syndr Human Retrovirology. 1998;19:484–9. doi: 10.1097/00042560-199812150-00007. [DOI] [PubMed] [Google Scholar]
- 34.Kibiki GS, Mulder B, Dolmans WM, et al. Mycobacterium tuberculosis genotypic diversity and drug susceptibility pattern in HIV-infected and non-HIV-infected patients in northern Tanzania. BMC Microbiol. 2007;7:51. doi: 10.1186/1471-2180-7-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shao HJ, Crump JA, Ramadhani HO, et al. Early versus delayed fixed dose combination abacavir/lamivudine/zidovudine in patients with HIV and tuberculosis in Tanzania. AIDS Res Hum Retroviruses. 2009;25:1277–85. doi: 10.1089/aid.2009.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdool Karim SS, Naidoo K, Grobler A, et al. Integration of antiretroviral therapy with tuberculosis treatment. N Engl J Med. 2011;365:1492–501. doi: 10.1056/NEJMoa1014181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Havlir DV, Kendall MA, Ive P, et al. Timing of antiretroviral therapy for HIV-1 infection and tuberculosis. N Engl J Med. 2011;365:1482–91. doi: 10.1056/NEJMoa1013607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blanc F-X, Sok T, Laureillard D, et al. Earlier versus later start of antiretroviral therapy in HIV-infected adults with tuberculosis. N Eng J Med. 2011;365:1471–81. doi: 10.1056/NEJMoa1013911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nanteza MW, Mayanja-Kizza H, Charlebois E, et al. A randomized trial of punctuated antiretroviral therapy in Ugandan HIV-seropositive adults with pulmonary tuberculosis and CD4+ T-cell counts of ≥350 cells/μL. J Infect Dis. 2011;204:884–92. doi: 10.1093/infdis/jir503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Getahun H, Kittikraisak W, Heilig CM, et al. Development of a standardized screening rule for tuberculosis in people living with HIV in resource-constrained settings: individual participant data meta-analysis of observational studies. PLoS Med. 2011;18:e1000391. doi: 10.1371/journal.pmed.1000391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grant AD, Charalambous S, Fielding KL, et al. Effect of routine isoniazid preventive therapy on tuberculosis incidence among HIV-infected men in South Africa. JAMA. 2005;293:2719–25. doi: 10.1001/jama.293.22.2719. [DOI] [PubMed] [Google Scholar]
- 42.Mwaungulu FBD, Floyd S, Crampin AC, et al. Cotrimoxazole prophylaxis reduces mortality in human immunodeficiency virus-positive tuberculosis patients in Karonga District, Malawi. Bull World Health Organ. 2004;82:354–63. [PMC free article] [PubMed] [Google Scholar]
- 43.Siegfried N, Uthman OA, Rutherford GW. Optimal time for initiation of antiretroviral therapy in asymptomatic, HIV-infected, treatment-naive adults. Cochrane Database Syst Rev. 2010;3 doi: 10.1002/14651858.CD008272.pub2. March 17:CD008272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lawn SD, Ayles H, Egwaga S, et al. Potential utility of empirical tuberculosis treatment for HIV-infected patients with advanced immunodeficiency in high TB-HIV burden settings. Int J Tuberc Lung Dis. 2011;15:287–95. [PubMed] [Google Scholar]
- 45.World Health Organization, World Health Organization African Regional Office, US Centers for Disease Control and Prevention, American Society for Clinical Pathology. Consultation on technical and operational recommendations for clinical laboratory testing harmonization and standardization: helping to expand sustainable quality testing to improve the care and treatment of people infected with and affected by HIV/AIDS, TB, and malaria. Maputo, Mozambique: World Health Organization; 2008. p. 20. World Health Organization. [Google Scholar]