Abstract
Background:
The principles of treatment of congenital dislocation of hip in old children are different than those of infants and neonates. The purpose of this study is to evaluate the radiographic and functional results of one-stage treatment (open reduction, femoral shortening derotation, and Salter's osteotomy) of DDH in older children.
Materials and Methods:
Between January 2005 and June 2010, 25 patients (30 hips) underwent one-stage triple procedure of open reduction, femoral shortening derotation, and Salter's osteotomy for the treatment of DDH. Preoperatively, they were classified according to the Tönnis class. Clinical outcomes were assessed using the modified McKay's criteria to measure pain symptoms, gait pattern, Trendelenburg sign status, and the range of hip joint movement. Radiographic assessment was made using Severin's scoring method to measure the centre-edge angle and dysplasia.
Results:
The mean age at the time of operation was 3.9 years (range 1.6–8 years), and the average duration of followup was 4.1 years (range 2–7.6 years). The McKay's score was excellent in 13 hips, good in 14 hips, fair in 2, and poor in 1 hip. The Severin's class I and II was found in 25 (83.3%) hips at the time of final evaluation as compared to none at the time of presentation.
Conclusions:
Young children having DDH can safely be treated with an extensive one-stage triple procedure of open reduction, femoral shortening derotation, and Salter's osteotomy, without increasing the risk of AVN. Early diagnosis and intervention is the successful treatment of patients suffering from DDH.
Keywords: Developmental dysplasia, hip, femoral shortening, derotation, salter's osteotomy
INTRODUCTION
Developmental dysplasia of the hip (DDH) denotes a wide spectrum of pathologic conditions, ranging from subtle acetabular dysplasia to irreducible hip dislocation.1 It is a very common to suspect and diagnose hip dysplasia when the children start walking in india due to lack of screening programme. The principles of treatment of dislocated hip joint for an older child are quite different from those of a new born.2 In a child of walking age and beyond, achieving a concentrically reduced hip while minimizing complications is more challenging. In the older child the reduction of hip is difficult because of adaptive shortening of the extraarticular soft tissues, acetabular dysplasia, capsular constriction, increased femoral anteversion, fibrofatty tissue in the acetabulum, hypertrophied ligamentum teres, and fixed inversion of limbus. If left untreated, these dysplastic changes lead to osteoarthritis in early adulthood.3,4
Bracing, traction, closed reduction, open reduction, and femoral or pelvic osteotomies are the frequently used treatment modalities for older children.5–7 The incidence of osteonecrosis of the femoral head has been reduced by avoiding immobilization of the hip in extreme abduction and by using femur-shortening osteotomies when appropriate.8 Pelvic osteotomy continues to gain favor for the treatment of selected patients over 18 months of age.9,10
Traction has been used before reduction of a dislocated hip to decrease the risk of ischemia of the femoral head, but data supporting use of this treatment are inconsistent.11–13 Closed or open reduction without a bony realignment procedure is associated with residual dysplasia.14,15 Femoral shortening has been shown to facilitate reduction and does not appear to increase the prevalence of osteonecrosis of the femoral head.16,17 Many authors have reported success with a single-stage procedure consisting of open reduction, capsulorrhaphy, femoral shortening, and pelvic osteotomy.18–23
The one-stage surgical treatment for DDH, consisting of open reduction, femoral shortening, and pelvic osteotomy, is a demanding procedure, technically, than a staged procedure. We report retrospective analysis to evaluate the radiographic and functional results of one-stage triple operative procedure of open reduction, femoral shortening, and Salter's osteotomy in older children.
MATERIALS AND METHODS
Between January 2005 and June 2010, 25 patients (30 hips) underwent one-stage triple procedure of open reduction, femoral shortening derotation, and Salter's osteotomy for the treatment of DDH. The average age was 3.9 years (range 18 months – 8 yrs) at the time of open reduction. Only the patients with idiopathic congenital dislocation of the hip were included in the study.
Clinical data regarding pain symptoms, gait pattern, range of hip joint motion and presence of Trendelenburg sign were recorded for each patient preoperatively and on the latest followup using the modified McKay's criteria.24 Tönnis classification system was used to assess the degree of dislocation of the femoral head.25 Radiographic evaluations included examination of preoperative and followup plain radiographs to classify patients according to the Severin's grading system.26 Avascular necrosis was assessed using Bucholz and Ogden's classification.27,28
Operative procedure
Open reduction followed the recommendations of Salter29 for the innominate osteotomy surgical technique and the femoral osteotomy was similar to that described by Predrag Klisic.30 The operative procedure started with the modified Smith-Petersen anterior approach (Bikini incision) [Figure 1a]. The muscles were reflected from the inner and outer aspects of the iliac crest and the hip joint was exposed [Figure 1b]. This was followed by the release of iliopsoas, excision of pulvinar, release of ligamentum teres, and incision of transverse acetabular ligament. Gentle traction was applied to the extremity to assess the degree of contracture of the muscles that crossed the hip joint. Due to the soft tissue contractures, the femoral head still was not reducible without applying excessive pressure.
Figure 1.
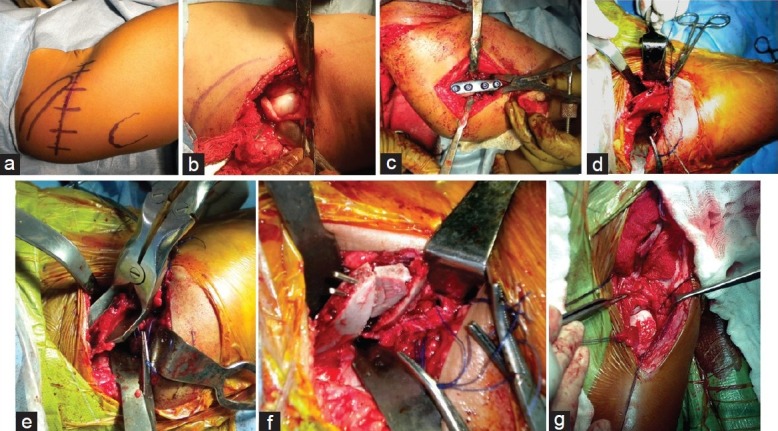
Peroperative photographs showing (a) Bikini incision; (b) exposure of the hip joint; (c) femoral osteotomy fixed with 4-hole small fragment plate; (d) pelvic osteotomy performed by using a Gigli saw; (e) bone graft taken from the proximal fragment of the ilium; (f) pelvic osteotomy fixed with a triangular bone graft and two K-wires; (g) reduction of the hip joint
Through a separate lateral approach, the proximal end of femur was exposed subperiosteally and a transverse osteotomy was made at the level of lesser trochanter. The amount of overlap in the femur was evaluated to determine the amount of femoral shaft to be resected. The osteotomy site was internally fixed with a four-hole small fragment plate [Figure 1c]. Shortening of 1–2 cm was found to be necessary to allow easy reduction of the femoral head while maintaining normal soft tissue tension across the hip.
At the time of open reduction femoral anteversion in excess of 60° as determined by forward angulation of the head and neck of femur with relation to the coronal plane of the femur is considered an indication for derotational osteotomy. Hip joint was reduced and held firmly in full internal rotation. Derotation was achieved by externally rotating the distal femoral fragment in relation to the proximal fragment until the patella pointed directly forward before applying the plate. It is important to avoid excessive derotation of femur as posterior instability may result if it is combined with Salter's innominate osteotomy.
At the time of initial reduction, if coverage of the femoral head was poor (which was assessed by the evidence of inadequate coverage of femoral head anteriorly with hip in extension and laterally with hip in adduction) or if the acetabulum was clearly maldirected, then we proceed for Salter's osteotomy. In this study all 25 patients (30 hips) required Salter's osteotomy for stabilization of the hip joint. A pelvic osteotomy was performed as described by Salter using a Gigli saw [Figure 1d]. A full-thickness bone graft was removed from the anterior part of the iliac crest and trimmed to the shape of a wedge; the base should correspond approximately to the distance between the anterior superior and inferior spines. After osteotomy, the distal segment of the innominate bone containing the entire acetabulum was shifted forward, downward, and outward so that the osteotomy site was opened anterolaterally. The bone graft was inserted on its edge into the osteotomy site and held with two K-wires [Figure 1e, f].
The hip was reduced concentrically, and the stability was assessed with the limb in the weight-bearing position, i.e. in slight abduction and extension [Figure 1g]. Redundant capsule was excised when necessary and capsulorrhaphy performed with interrupted absorbable sutures. Throughout the operation, bleeding was controlled by packing and coagulation. The mean blood loss which is measured by weighing sponges and recording suction volumes is 220 ml (range 200- 250 ml). The average time for the combined operation of open reduction and osteotomy was 2.5 hours (range 2.25-2.75 hours).
Postoperatively, the hips were immobilized in a 1½ hip spica in position of slight flexion, abduction and internal rotation for 6 weeks. This was changed to an abduction splint for a further 4 weeks which allows non weight bearing flexion and extension mobilization of the hip joints. K-wires were removed after consolidation at the osteotomy site usually at 6–8 weeks. Partial weight bearing started after 10 weeks with crutches for 2 weeks, followed by full weight bearing. Patients with bilateral dysplasia (n=5) had the procedures on both hips at an interval of 3–6 months (mean 4.5 months) as per patient's convenience.
The patients were followed up in the outpatient clinic at 3 month intervals during the first 2 years after surgery and then at yearly intervals. They were evaluated clinically during each visit for the range of motion of the affected hip, the quality of gait, and the presence of any pain. Each patient's preoperative and postoperative radiographs were evaluated to determine the degree of displacement of the femoral head (the Tönnis grade), the acetabular index, C–E angle, the continuity of the Shenton's line, and the presence or absence of avascular necrosis. All the patients with a minimum follow up of two years were included in this study. So there were 30 hips available for evaluation.
RESULTS
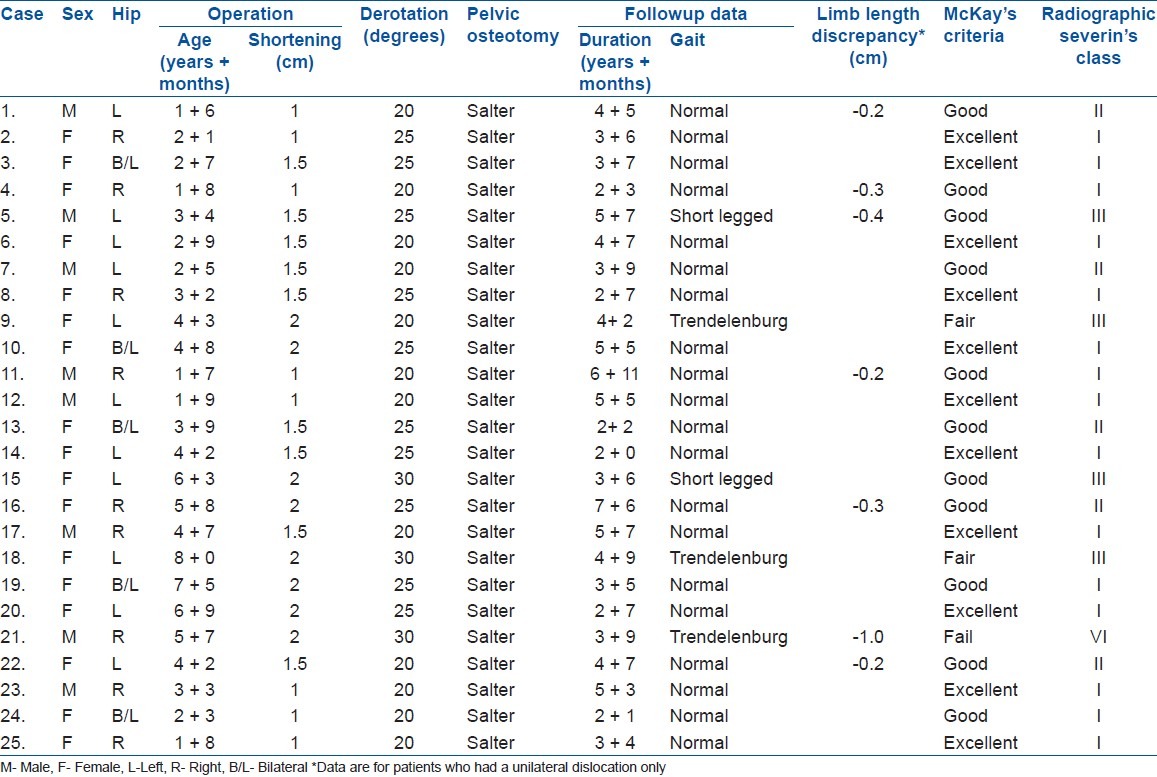
There were 17 girls and 8 boys [Table 1]. There were 20 unilateral dislocations (9 right unilateral dislocations, 11 left unilateral dislocations) and 5 bilateral dislocations. The average age at the time of operation was 3.9 years (range 1.6–8 years). The average duration of followup was 4.1 years (range 2–7.6 years). Immediate postoperative shortening of lower limb was 1–2 cm (average 1.5 cm) which improved to 0.2–1 cm (average 0.3 cm) during the latest followup examination. Femur derotated to an average of 23.2° (range 20°–30°) to correct the anteversion that was noted during the operation. Salter's osteotomy was necessary to stabilize the reduction in all cases.
Table 1.
Surgical and followup data
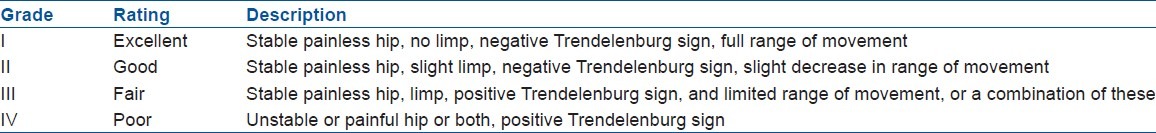
On the final clinical evaluation, the clinical results according to McKay's scoring system [Table 2] were also favorable. At preoperative evaluation, 23 hips (76.6%) were in fair condition and 7 hips (23.3%) were in poor condition. At the end of the study, there were 13 hips (43.3%) in excellent condition, 14 (46.6%) in good condition, 2 (6.6%) in fair condition, and 1(3.3%) in poor condition.
Table 2.
McKay's criteria for clinical evaluation
According to Severin's classification [Table 3] fourteen (46.6%) hips were Severin's class V and 16 (53.3%) were Severin's class IV prior to surgery. Postoperatively, 25 hips (83.3%) were rated class I (19 hips) and class II (6 hips). Five hips (16.6%) were rated class III (4 hips) and class VI (one hip) at the latest followup. Cases 17 and 20 are illustrative of excellent clinical and radiographic (class I) results [Figures 2a–c and 3a, b]. Cases 7, 13, and 16 showed good clinical and radiographic (class II) results [Figures 4a–c, 5a–c, and 6a–c]. Case 21 developed failure (class VI) 10 months after surgery.
Table 3.
Severin's classification for radiographic results
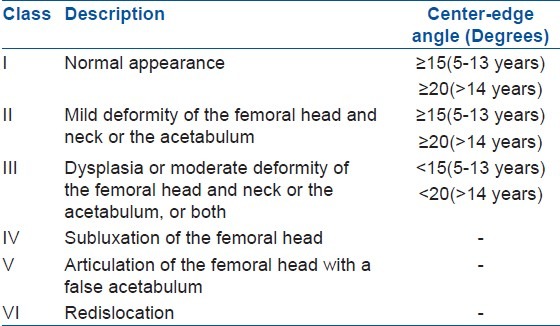
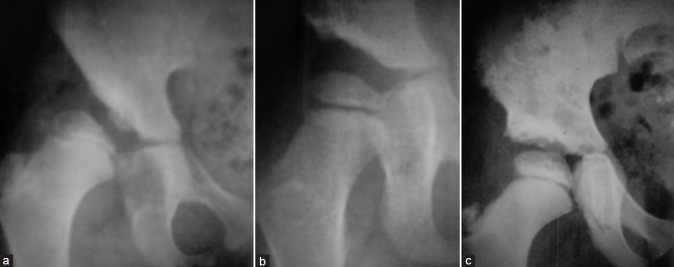
Figure 2.
A 4.7-year-old male child with A–P radiograph of right hip joint (Case 17) showing (a) dislocation; (b) adequate reduction at 8 months after surgery; (c) well-reduced hip joint within the remodeled acetabulum at 5.7 years followup
Figure 3.
(a) X-ray pelvis including both hip shows DDH of left hip (Case 20) in a 6.9 year old girl (b) X-ray of same patient at 2.7 year followup shows concentric reduction with radiographic result Severin's class I
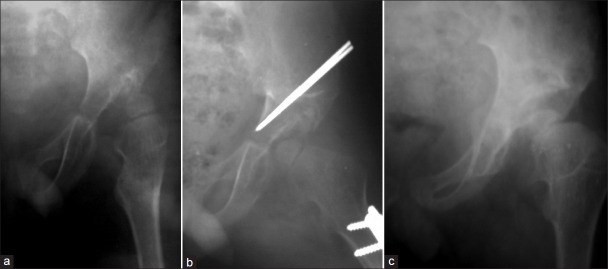
Figure 4.
A 2.5-year-old boy with untreated DDH of the left hip joint; postoperative X-ray left hip anteroposterior view (Case 7) showing (a) DDH of left hip (b) postoperative well reduced hip joint after single-stage triple procedure; (c) reduction maintained at 3.9 years after surgery
Figure 5.

Preoperative X-ray pelvis anteroposterior view of a 3.9 year old girl (Case 13) showing (a) bilateral DDH; (b) followup X-ray 2.2 years after surgery shows well-reduced hip joints; (c) well functional result with patient sitting cross legged
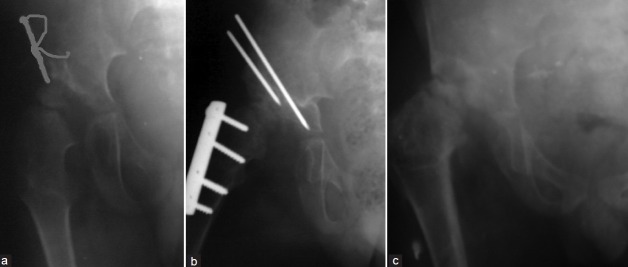
Figure 6.
Anteroposterior radiograph of a 5.8-year-old girl (case 16) showing (a) unilateral dislocation of the hip right side; (b) followup radiograph 7 months after surgery with adequate reduction; (c) followup radiograph after 7.6 years of surgery, with well-developed congruous hip joint
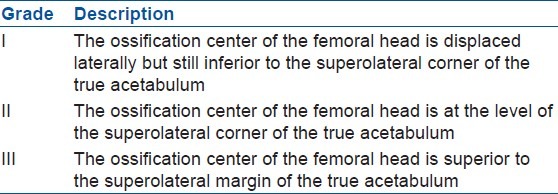
According to Tönnis classification [Table 4] of the degree of dislocation severity (preoperatively), there were 4 patients (13.3%) in grade I, 14 (46.6%) in grade II, and 12 (40%) in grade III, as compared to only 1 (3.3%) of grade II postoperatively.
Table 4.
Tönnis classification for severity of dislocation
The acetabular index was measured at each followup radiographs to assess acetabular development at the final followup. The average acetabular index was 23°±4.1°; it decreased from 42°±5° preoperatively to 21°±2° postoperatively. The average postoperative center-edge angle was 23.5° (range 21°–26°).
All radiographs were evaluated for evidence of avascular necrosis. One patient (Case 5) developed lateral physeal damage (type II classification of Bucholz and Ogden). At the latest followup, the clinical results were good, although the radiographic results were Severin's class III.
The hip was considered to be adequately reduced when the radiographs showed an intact Shenton's line, a center-edge angle of more then 15°, and an acetabular index of less then 28°. The adequacy of acetabular remodeling was evaluated by comparing the immediate postoperative radiograph with the latest followup radiograph. Improvement of the acetabular index by at least 8° and to 20° or less in the most recent radiographs was considered to be adequate correction.
Evaluation of gait revealed that three hips (Cases 9, 18, and 21) had a mild gluteus medius lurch and two (Cases 5 and 15) had a short legged gait. Subjectively, very few patients had any complaints. One patient had infrequent discomfort, and three noted weakness (a mild Trendelenburg limp). No patient or parent complained of a limb length discrepancy. In general, the subjective evaluation did not correlate with the objective findings; it was therefore of little value in assessing the end results.
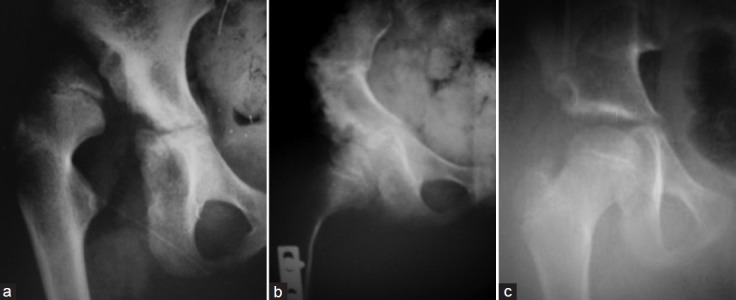
One patient (Case 21) had an open reduction and innominate osteotomy performed in a false acetabulum. Most recent followup shows Severin's radiographic rating class VI [Figure 7a–c]. Postoperative stiffness of the hip occurred in one patient. Repeat arthrotomy at the time of plate removal disclosed extensive scarring but no other intraarticular obstruction or pathology.
Figure 7.
Anteroposterior ratiograph of right hip joint of a 5.7-year-old male child (case 21) showing (a) untreated DDH (b) immediate postoperative X-ray with residual dislocation; (c) Severin's class VI at the latest followup, 3.9 years after surgery
DISCUSSION
The primary goal of treatment of congenital dislocation of hip is concentric reduction. Failure to treat at an early age may lead to gait abnormalities, limitation of motion of the hip, joint pain, and osteoarthritis. However, the age beyond which surgical treatment is contraindicated has been the subject of debate due to the risk of serious complications. Concentric reduction in older children may be a challenge, more so when the femoral head is flattened or when the acetabulum is dysplastic. Reduction may be hindered by soft tissue contracture with undue pressure on the femoral head. This may result in poor development of hip joint and avascular necrosis of the femoral head.
Femoral osteotomy, including shortening, derotation osteotomy, combined with open reduction, capsulorrhaphy, and pelvic osteotomy, is an extensive procedure that can safely be undertaken in one stage. This one stage procedure which has been used in older children is the method of choice in the treatment of late diagnosed congenital dislocation of the hip. With femoral shortening as the fundamental step, this method can be applied in high dislocations to prevent undue pressure on the femoral head, which is the main cause of avascular necrosis, joint stiffness, and failures.
There have been numerous reports discussing the merits of a more aggressive surgical approach that includes a single procedure combining an open reduction with a femoral or pelvic osteotomy. Salter and Dubos showed 93.6% good to excellent results in children of younger age group.31 Klisic and Jankovic (n=60) reported 63% excellent to good results in the age group of 5–15 years.30 Karakaş et al. operated on 47 patients (55 hips), who were 4 years and more, with 67% good or excellent clinical results and 65% good or excellent radiological results.32 Ryan et al. showed 92% excellent to good results clinically and 72% radiologically.33 Vallamshetla et al. operated on 15 patients (18 hips), who were 4 years and more, with 100% good or excellent clinical results (McKay's criteria) and 100% Severin's classification class I (10) and II (8).34 Umer et al. have reported 86.2% good to excellent clinical results and 51.7% Severin's class I at final evaluation.35 The results of the Salter's osteotomy for treatment of DDH in 30 hips treated beyond 18 months of age were reviewed. Salter's osteotomy was found to be useful for stabilizing hips after open reduction. The results of the study showed a significant improvement in the radiological features of the operated hip joints according to Severin's classification. At the followup none of the patient had class V severity compared to 14 hips (46.6%) prior to surgery. There was only one hip in class IV post operatively as compared to 16 hips (53.3%) preoperatively. Notably 83.3% of hips achieved an improvement of class I (19 hips) and class II (6 hips) at followup compared to none before surgery. Similarly, favorable results were also observed when clinical parameters were compared before and after surgery. At final followup, excellent to good results were noted in 27 hips (89.9%) compared to none before surgery. Only 1 (3.3%) hip joint demonstrated poor condition at followup compared to 7 (23.3%) prior to surgery. Principle of preserving the shape and capacity of the acetabulum by Salter's innominate osteotomy is important for the future function and development of the joint as compared to Pemberton osteotomy which alters the shape of acetabulum and decreases its capacity.
Late-diagnosed congenital dislocation of the hip with one-stage open reduction, femoral shortening, capsulorrhaphy, and pelvic osteotomy corrects associated femoral and acetabular deformities. This operation improves the cover of the femoral head and provide stability in the weight-bearing position. This procedure can be done safely, with reliable results and without an increase in the risk of avascular necrosis.
The limitation of this study is that all the patients were not followed to skeletal maturity. The presence of residual hip dysplasia and problems relating to subluxation, trochanteric overgrowth and avascular necrosis if any should be recognized early and treated appropriately to ensure optimum results.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Klisic PJ. Congenital dislocation of the hip. A misleading term: Brief report. J Bone Joint Surg Br. 1989;71:136. doi: 10.1302/0301-620X.71B1.2914985. [DOI] [PubMed] [Google Scholar]
- 2.Beaty JH. Congenital and developmental anomalies of hip and pelvis. In: Canale ST, editor. Campbell's operative orthopedics. 11th ed. Philadelphia: Mosby; 2007. pp. 1180–220. [Google Scholar]
- 3.Berkeley ME, Dickson JH, Cain TE, Donovan MM. Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. J Bone Joint Surg Am. 1984;66:412–20. [PubMed] [Google Scholar]
- 4.Wedge JH, Wasylenko MJ. The natural history of congenital disease of the hip. J Bone Joint Surg Br. 1979;61:334–8. doi: 10.1302/0301-620X.61B3.158025. [DOI] [PubMed] [Google Scholar]
- 5.Ashley RK, Larsen LJ, James PM. Reduction of dislocation of the hip in older children: A preliminary report. J Bone Joint Surg Am. 1972;54:545–50. [PubMed] [Google Scholar]
- 6.Morel G. The treatment of congenital dislocation and subluxation of the hip in the older child. Acta Orthop Scand. 1975;46:364–99. [PubMed] [Google Scholar]
- 7.Weinstein SL, Mubarak SJ, Wenger DR. Developmental hip dysplasia and dislocation: Part II. Instr Course Lect. 2004;53:531–42. [PubMed] [Google Scholar]
- 8.Zionts LE, MacEwen GD. Treatment of congenital dislocation of the hip in children between the ages of one and three years. J Bone Joint Surg Am. 1986;68:829–46. [PubMed] [Google Scholar]
- 9.Salter RB. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Am. 1961;43:518–39. [PubMed] [Google Scholar]
- 10.Vitale MG, Skaggs DL. Developmental dysplasia of the hip from six months to four years of age. J Am Acad Orthop Surg. 2001;9:401–11. doi: 10.5435/00124635-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Gage JR, Winter RB. Avascular necrosis of the capital femoral epiphysis as a complication of closed reduction of congenital dislocation of the hip. A critical review of twenty years experience at Gillette Children's Hospital. J Bone Joint Surg Am. 1972;54:373–88. [PubMed] [Google Scholar]
- 12.Schoenecker PL, Strecker WB. Congenital dislocation of hip in the children. Comparison of the effects of femoral shortening and of skeletal traction in the treatment. J Bone Joint Surg Am. 1984;66:21–7. [PubMed] [Google Scholar]
- 13.Harrold AJ. Problems in congenital dislocation of the hip. Br Med J. 1977;1:1071–3. doi: 10.1136/bmj.1.6068.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lindstrom JR, Ponseti IV, Wenger DR. Acetabular development after reduction in congenital dislocation of the hip. J Bone Joint Surg Am. 1979;61:112–8. [PubMed] [Google Scholar]
- 15.Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am. 1994;76:1777–92. doi: 10.2106/00004623-199412000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Browne RS. The management of late diagnosed congenital dislocation and subluxation of the hip. with special reference to femoral shortening. J Bone Joint Surg Br. 1979;61:7–12. doi: 10.1302/0301-620X.61B1.422637. [DOI] [PubMed] [Google Scholar]
- 17.Wenger DR. Congenital hip dislocation: techniques for primary open open reduction including femoral shortening. Instr Course Lect. 1989;38:343–54. [PubMed] [Google Scholar]
- 18.Shih CH, Shih HN. One-stage combined operation of congenital dislocation of the hips in older children. J Pediatr Orthop. 1988;8:535–9. doi: 10.1097/01241398-198809000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Galpin RD, Roach JW, Wenger DR, Herring JA, Birch JG. One-stage treatment of congenital dislocation of the hip in older children, including femoral shortening. J Bone Joint Surg Am. 1989;71:734–41. [PubMed] [Google Scholar]
- 20.Dimitriou JK, Cavadias AX. One-stage surgical procedure for congenital dislocation of the hip in older children: Long-term results. Clin Orthop Relat Res. 1989;246:30–8. [PubMed] [Google Scholar]
- 21.Olney B, Latz K, Asher M. Treatment of hip dysplasia in older children with a combined one-stage procedure. Clin Orthop Relat Res. 1998;347:215–23. [PubMed] [Google Scholar]
- 22.El-Sayed MM. Single-stage open reduction, Salter innominate osteotomy, and proximal femoral osteotomy for the developmental dysplasia of the hip in children between the ages of 2 and 4 years. J Pediatr Orthop B. 2009;18:188–96. doi: 10.1097/BPB.0b013e32832bf618. [DOI] [PubMed] [Google Scholar]
- 23.Forlin E, Munhoz da Cunha LA, Figueiredo DC. Treatment of developmental dysplasia of the hip after walking age with open reduction, femoral shortening, and acetabular osteotomy. Orthop Clin North Am. 2006;37:149–60. doi: 10.1016/j.ocl.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 24.McKay DW. A comparison of the innominate and pericapsular osteotomy in the treatment of congenital dislocation of the hip. Clin Orthop Relat Res. 1974;98:124–32. doi: 10.1097/00003086-197401000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Tönnis D. An evaluation of conservative and operative methods in the treatment of congenital hip dislocation. Clin Orthop Relat Res. 1976;119:76–88. [PubMed] [Google Scholar]
- 26.Severin E. Congenital dislocation of the hip; development of the joint after closed reduction. J Bone Joint Surg Am. 1950;32:507–18. [PubMed] [Google Scholar]
- 27.Bucholz RW, Ogden JA. The hip. Proceedings of the Sixth Open Scientific Meeting of The Hip Society. St. Louis: The C.V. Mosby Company; 1978. Patterns of ischemic necrosis of the proximal femur in nonoperatively treated congenital hip disease; pp. 43–63. [Google Scholar]
- 28.Thomas CL, Gage JR, Ogden JA. Treatment concepts for proximal femoral ischemic necrosis complicating congenital hip disease. J Bone Joint Surg Am. 1982;64:817–28. [PubMed] [Google Scholar]
- 29.Salter RB. Role of innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip in the older child. J Bone Joint Surg Am. 1966;48:1413–39. [PubMed] [Google Scholar]
- 30.Klisic P, Jankovic L. Combined procedure of open reduction and shortening of the femur in treatment of congenital dislocation of the hips in older children. Clin Orthop Relat Res. 1976;119:60–9. [PubMed] [Google Scholar]
- 31.Salter RB, Dubos JP. The first fifteen year's personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop Relat Res. 1974;98:72–103. doi: 10.1097/00003086-197401000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Karakaş ES, Baktir A, Argün M, Türk CY. One-stage treatment of congenital dislocation of the hip in older children. J Pediatr Orthop. 1995;15:330–6. doi: 10.1097/01241398-199505000-00014. [DOI] [PubMed] [Google Scholar]
- 33.Ryan MG, Johnson LO, Quanbeck DS, Minkowitz B. One-stage treatment of management of congenital dislocation of the hip in children three to ten years old: Functional and radiographic results. J Bone Joint Surg Am. 1998;80:336–44. doi: 10.2106/00004623-199803000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Vallamshetla VR, Mughal E, O’Hara JN. Congenital dislocation of the hip. A re-appraisal of the upper age limit for treatment. J Bone Joint Surg Br. 2006;88:1076–81. doi: 10.1302/0301-620X.88B8.17592. [DOI] [PubMed] [Google Scholar]
- 35.Umer M, Nawaz H, Kasi PM, Ahmed M, Ali SS. Outcome of triple procedure in older children with developmental dysplasia of hip (DDH) J Pak Med Assoc. 2007;57:591–5. [PubMed] [Google Scholar]