Abstract
Context:
Paralysis of quadriceps muscle leads to severe disability as the knee is unstable and cannot be fully extended and locked in extension, which results in giving way of the knee joint. Because of this, the patient tries to get stability of the knee by various means like hand to knee gait, extreme internal or external rotation of the affected limb to stabilize knee by support of medial or lateral collateral ligament, respectively, or by tilting pelvis. When there is concomitant weakness of gluteus maximus quadriceps and hamstrings (MRC muscle power less than grade III), patient may develop compensatory hyperlordosis of spine. Hamstring (H) transfer is a well-accepted procedure for patients with quadriceps (Q) weakness. For hamstring transfer, we have used a modified technique of anchoring of biceps femoris and semitendinosus tendon to patella. Instead of cutting the periosteum over the patella in an I-shaped manner, an osteoperisoteal flap was raised after two parallel incisions over the patella and both tendons were sutured under the flap with each other. We conducted a retrospective evaluation of the results of modified hamstring transfer in 267 patients of post polio residual paralysis with residual quadriceps paralysis.
Materials and Methods:
Two hundred and fifty young patients (100 male and 150 female patients) who had quadriceps paralysis due to polio were managed by hamstring transfer at a single center between 1984 and 1996 and were followed for a mean of 5 years (range 4–12 years). Age of patients ranged from 7 to 18 years in 238 patients and 12 patients were above the age of 18 years. All cases were followed periodically, and assessment of knee extension, extension lag, knee flexion, elimination of calliper, and avoidance of hand to knee gait was done.
Results:
One hundred and sixty two patients (65%) showed excellent results, 38 patients (15%) had good results, and 50 patients (20%) showed poor results. Ninety three patients had major complications like genu recurvatum, restricted knee flexion, and extension lag. Ten patients had minor complications like superficial infection and epidermal edge necrosis.
Conclusions:
H to Q transfer in the presence of quadriceps paralysis with good power in hamstring is a better alternative than supracondylar osteotomy because it is a dynamic correction and it produces some degree of recurvatum with increasing stability of knee in extension while walking. While inserting hamstring over patella the periosteum is not cut in an I-shaped fashion to create a flap which gives additional strength to new insertion and also patella act as a fulcrum during the extension of knee by producing the bowstring effect.
Keywords: Hamstring transfer, post polio residual paralysis, quadriceps paralysis
INTRODUCTION
Paralysis of quadriceps muscle results in severe disability as the knee is unstable and cannot be fully extended and locked in extension, which results in giving way of the knee joint. Because of this, the patient tries to get stability of knee by various means like hand to knee gait, extreme internal or external rotation of the affected limb to stabilize knee by support of medial or lateral collateral ligament, respectively, or by tilting pelvis. When there is concomitant weakness of gluteus maximus quadriceps and hamstrings power less than 3, patient may develop compensatory hyperlordosis of spine. To overcome the weakness of quadriceps, patient also tries to lock the knee with gastrocnemius contracting from down, leading to tendo achilles tightness which produces secondary equines deformity. Slight recurvatum produces stable knee if triceps surae is active. In bilateral quadriceps paralysis, patient has to crawl.
MATERIALS AND METHODS
We have operated 267 cases of quardriceps. We retrospectively reviewed the results of 267 operated cases of quadriceps paralysis. Only 250 could be followedup. Seventeen patients were lost to followup 66 patients had 2-3 years followup while 67 patients had 3-5 years followup and 199 patients had more than 5 years followup. There were 150 female and 100 male patients. 100 patients were between 7-10 years when operated while 38 between 11-12 years, 83 between 13-14 years and 17 between 15-18 years 12 patients were above the age of 18 years.
In all the patients in whom hamstring to quadriceps transfer was performed, the following prerequisites for successful transfer were considered. First, the power in biceps and semitendinosus must be more than grade 4 or more hip flexor and extensors must be good for clearing the ground without difficulty. Any flexion deformity of hip or knee valgus or varus was corrected. Knee flexors other than biceps and semitendinosus must be good and gastrocnemius must be active enough to perform knee flexion and prevent recurvatum. Biceps alone should not be transferred as this can lead to lateral displacement of patella. Triceps surae must be normal to prevent genu recurvatum and remain as an active knee flexor after surgery. Therefore, the equinus deformity should not be corrected by tendo achilles lengthening without seeing the result of hamstring transfer.
Operative procedure
The entire extremity was prepared and draped after the application of tourniquet and administration of appropriate anesthesia. An incision was made on posterolateral aspect of lower one-third of the thigh and extended distally up to the head of fibula. Biceps femoris tendon was dissected out taking care not to injure the lateral popliteal nerve which lies immediately behind the tendon and winds around the neck of fibula. Biceps tendon was divided distally along with thin chip of bone at its insertion on the lateral aspect of the head of fibula taking care not to damage the lateral ligaments of knee joint, which wind around the tendon, and muscle bellies are mobilized proximally as the entry of its nerve and blood supply will permit [Figure 1]. A second incision was made on the posteromedial aspect of lower one-third of the thigh to the medial aspect of the tibial condyle. About four-finger width distance was kept between both the incisions to prevent skin necrosis. Semitendinosus tendon, a cord-like round structure without muscle belly, is found lying behind the sartorius and gracilis muscles. It was divided from its insertion from tibia and mobilized as proximally as possible with blunt finger dissection. Take as much as length of tendon as possible [Figure 2]. The third incision was made vertically on the patella. Next two sharp cuts 8-10 mm apart were placed over periosteum of patella, parallel to each. With the help of sharp osteotome, thick osteoperiosteal flap was raised from one incision to another [Figure 3]. Then, oblique subcutaneous tunnel was made from the first to third incision in such a way that it could accommodate the whole biceps tendon and the tendon can glide freely. Similar type of tunnel was made between the second and third incision to pass semitendinosus tendon. The knee was kept at about 30° of flexion with the help of a wooden triangle or some other device at this stage of surgery [Figure 4]. Now the tendon of biceps was passed through the osteoperiosteal flap, and tendon was sutured near the lower incision on patella and infrapatellar portion of ligamentum patellae. Then, the remaining long portion slit was made in biceps femoris proximal to the previously sutured area for osteoperiosteal flap. Finally, semitendinosus was sutured back on its own proximal portion [Figures 5–7]. It is always advisable to take two sutures with biceps femoris and semitendinosus to keep the direction of the pull on the patella in the midline. To know about the tension over the patella, the thigh was raised passively to allow knee to go under 30 degrees of flexion and there should not be any giving way of the sutures. Any restrictions of knee flexion postoperatively was prevented by this precaution. After coagulation of bleeders, the wound was closed over negative suction drain. Postoperatively groin to toe posterior slab was given without any flexion at hip and knee joints.
Figure 1.
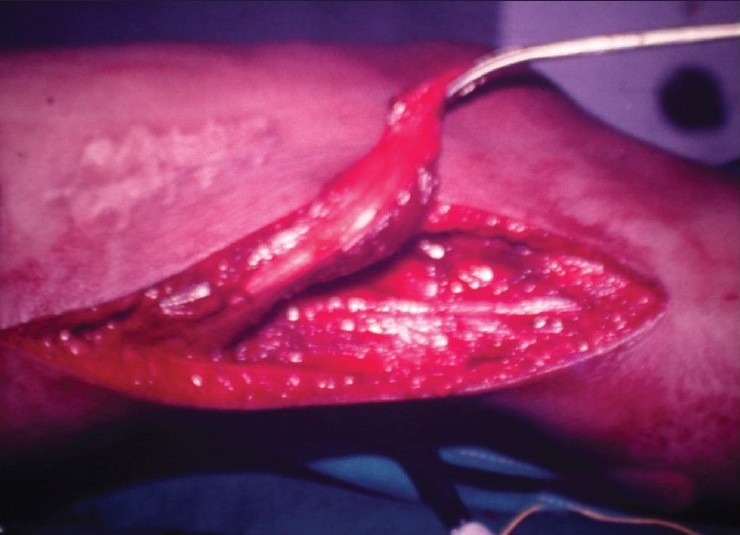
Peroperative photograph showing lateral incision with detached biceps tendon
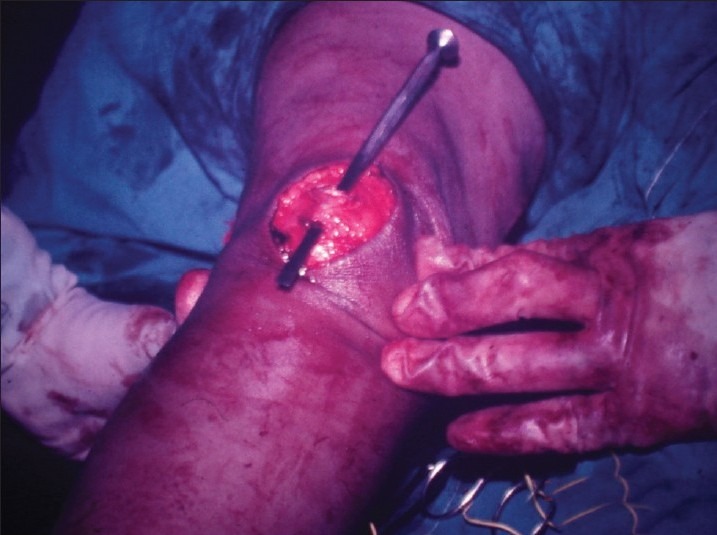
Figure 2.

Peroperative photograph showing posteromedial incision with separated semitendinosus tendon
Figure 3.
Peroperative photograph showing raised osteoperiosteal flap over patella
Figure 4.
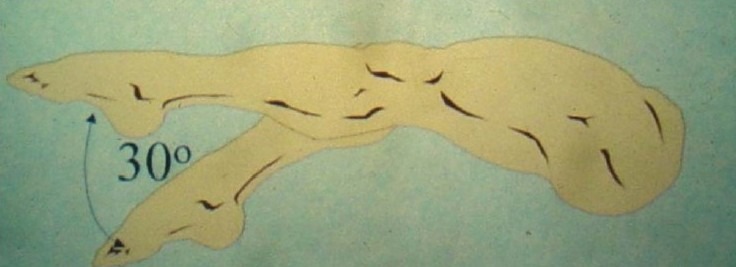
Optimum tension at 30° flexion
Figure 5.
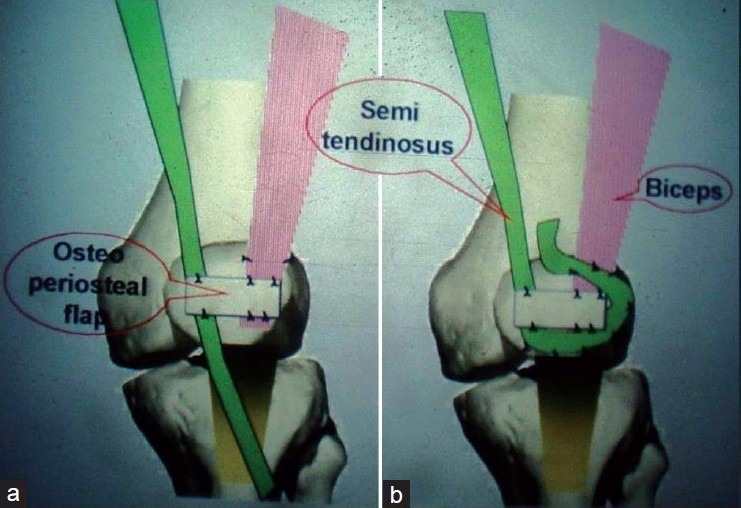
Schematic diagram showing (a) Tendon of biceps was passed through the osteoperiosteal flap, (b) tendon was sutured near the lower incision on patella and infrapatellar portion of ligamentum patellae
Figure 7.

Peroperative photograph showing suturing of biceps tendon with semitendinosus
Figure 6.
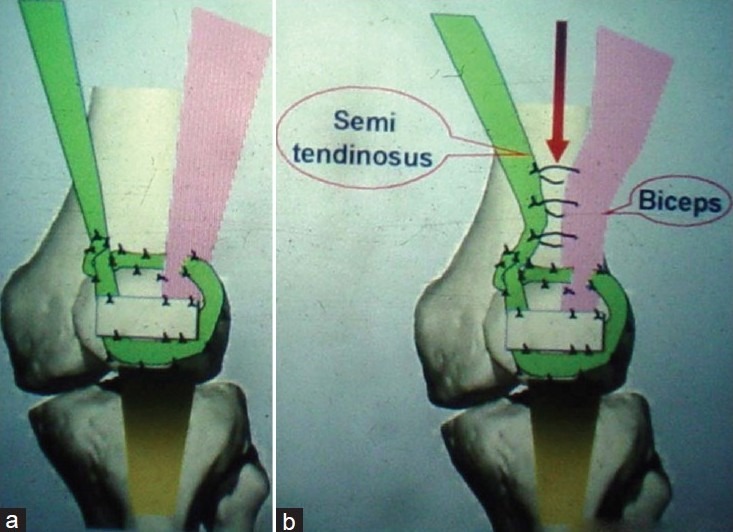
Schematic diagram showing (a) Semitendinosus tendon after passing from biceps, sutured on its own proximal portion of tendon. (b) Few sutures taken between semitendinosus and biceps to bring the pull of tendon in the center
The foot end of the bed was raised to prevent edema in the limb. One should not put anything under the leg to elevate, to avoid tension over the hamstring. After suture removal, groin to toe plaster was given for 3–4 weeks. This was followed by physiotherapy to get knee extension. When good extension was achieved, slowly knee flexion exercise were started. Weight bearing was permitted when the patient was able to do full extension and atleast 90° flexion.
Technical tips
We used continuous incision on the posteromedial aspect of the thigh, instead of interrupted incision to dissect out semitendinosus tendon, to get good exposure and to be able to mobilize freely up to adequate length. We could reroute the tendon in a direct line between its origin and new insertion. We did not cut periosteum in an I-shaped manner rather raised thick osteoperiosteal flap from patella and passed tendon through it so that we could give as much as tension as necessary for that particular case without fear of breakage of thick flap. This thick osteoperiosteal flap also adds to the strength of fixation of tendon and patella would act as fulcrum during extension of knee joint by producing bowstring effect. Semitendinosus tendon also passes through osteoperiosteal flap and is sutured with ligamentum patellae, and then encircling the biceps tendon, it is sutured back on its own proximal portion. Few stitches are made where semitendinosus tendon was encircling the biceps tendon, for additional strength. Thus, new insertion was securely fixed. In certain cases where medial hamstring was so powerful and it was fixed within with quadriceps, it not only acted as check rein but also helped in getting powerful extension. Too much tension while anchoring the tendon patella should be avoided, which otherwise can lead to restriction of knee flexion. Because of bony tissue of osteoperiosteal flap, tendons would unite with patella, and thus would provide a rigid new bony insertion to the transferred tendons.
RESULTS
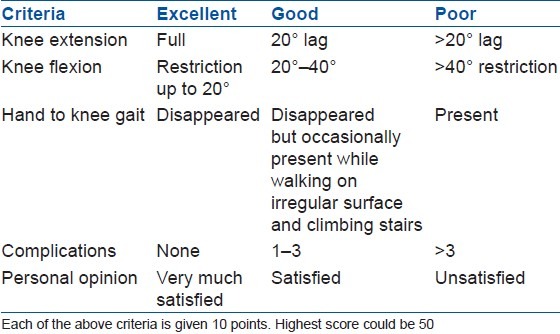
All 250 patients were followed for 2–10 years. For assessment of the outcome of the surgery, we had considered the criteria [Table 1].
Table 1.
Outcome assessment criteria
One hundred and sixty two patients (65%) had excellent results, 38 patients (15%) showed good results and 50 patients (20%) had poor results [Figure 8].
Figure 8.
Clinical photograph with longest followup of 24 years after hamstring transfer showing (a) full extension and near full flexion (b)
The major complications seen were genu recurvatum (more than 15°), restricted flexion, and extension lag. The minor complications noted were epidermal edge necrosis and superficial infection. Fifty patients (20%) were noticed to have genu recurvatum, who had bilateral affection of lower limbs. Because of good results of hamstring transfer, patient had discarded calliper from the opposite side and started walking with full weight bearing on the operated side. So, ultimately strain on the operated side leg led to recurvatum. From this observation, we infer that bilateral polio weakness is major cause of this complication of genu recurvatum. Another 30 patients had restricted knee flexion [Figure 9], while 22 patients had more than 20° extension lag. Patients who had restricted flexion had difficulty in squatting on the ground. Ten patients had epidermal necrosis on the posterior medial incision, of whom one got superficial infection which was treated successfully with antibiotics and repeated dressing. Other complications of lateral displacement of patella, lateral popliteal nerve palsy, and unstable knee gait were not seen in this series.
Figure 9.

Clinical photograph showing restriction of knee flextion postoperatively
DISCUSSION
In any tendon transfer, the transferred muscle must be strong enough to do reasonably well what paralyzed muscle did or support the power of partially paralyzed muscle. The transferred tendon must be mobilized enough for free gliding movements and should be routed in comparatively direct line between its origin and insertion. Because of medial continuous incision, it is possible to reroute the semitendinosus tendon and dissect out its adequate length to reinforce the new insertion over the patella, and its line of pull will be almost straight from the origin to its new insertion. As far as possible, we try to do the same procedure for biceps tendon. With the modified technique of raising the osteoperiosteal flap of patella, it is possible to give as much as tension as necessary and fixation of both tendons is very strong on patella. As the periosteum is not cut in an I-shaped fashion, the flap gives additional strength to new insertion. Patella will act as a fulcrum during the extension of knee by producing the bowstring effect [Figure 10].
Figure 10.
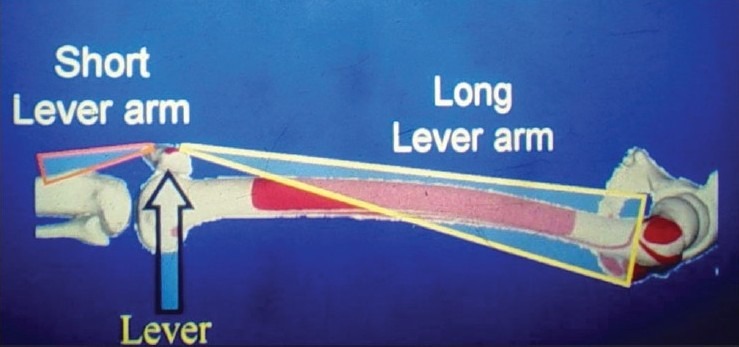
The line diagram shows patella (arrow) acting as a fulcrum during extension of the knee
In many cases, we found very strong semitendinosus muscle, which not only acts as check rein but is also helpful in getting powerful extension and preventing lateral subluxation of the patella. Hamstrings to quadriceps transfer not only improves the balancing power of patients, but also improves gait and removes the fear of falling down while walking. It also produces desired recurvatum and out of four muscle of knee flexion only two muscles are transferred in front of the knee joint.
Various authors have reported results by using different muscles available for transfer, alone or in combinations. Wray1 used only hamstrings for transfer. Of the 51 transfers in 47 patients, 46.5% were rated good, 14% were fair, and 39.5% were unsatisfactory. The complications seen were lateral dislocation of patella and genu recurvatum. In another review of series by Crego and Fischer,2 biceps tendon alone was used for transfer in 100 patients, 29 patients had bilateral dislocation of patella, 16 patients had genu recurvatum, and few had lateral instability of the knee. In another group of patients of the same review, who had transfer of both biceps and semitendinosus, none developed lateral dislocation of patella, but seven had recurvatum, one had lateral knee instability, and one had failed reconstruction.
Caldwell,3 using Durham technique of biceps femoris transfer in 39 patients, obtained good results in 15% of patients, 70% showed fair and 15% showed poor results, and 15% had lateral dislocation of patella. Two patients had recurvatum because of weak triceps and medial hamstrings. Transplantation of adductor longus was used in one patient by Kleinberg4 and very satisfactory immediate results were obtained. Transfer of sartorius and tensor fascia lata muscle, though theoretically more satisfactory, is usually insufficient because these muscles are not strong enough to replace the quadriceps. Kleinberg4 in 1957 had transferred adductor longus muscle including its neurovascular pedicle to supplement the quadriceps. Riska5 used transfer of iliotibial band with part of gluteus maximus muscle in 63 patients and could get improvement for stability in 85% patients and power of extension. With this combination of muscle transfers, good conversion of hamstring activity from swing phase to stance phase has been seen by Sutherland6 and this is the advantage of surgery.
Another small series of 15 patients in 1996 with average followup of 48 months showed excellent results in only 13.5% patients, and it was noted that lack of active terminal knee flexion prohibiting comfortable floor sitting was the main limitation of the surgery.7
Mukherjee8 in a series of 40 patients in 1980 showed that 50% had good to satisfactory improvement in knee extension and gait following hamstring to quadriceps transfer. Remaining 50% had poor results attributed to faulty technique, infection, flexion contracture, or inadequate postoperative management.
In bilateral affection, it is possible that patients may get undesired recurvatum on the operated side because with good results on the operated side, patient was able to walk without calliper on the unoperated side, leading to more strain on the operated limb, and thus unwanted recurvatum at the knee. Even in cases of gross extension lag, patients were able to lock the knee in extension while standing and walking. It also eliminates the hand to knee gait. Transfer of biceps and semitendinosus acts from lateral and medial sides of patella, so it keeps patella in its position and this muscle provides long lever arm acting on short lever arm, so with less effort patient gets better extension after this transfer.
CONCLUSION
H to Q transfer in the presence of quadriceps paralysis with good power in hamstring is a better alternative than supracondylar osteotomy because it is a dynamic correction and it produces some degree of recurvatum with increasing stability of knee in extension while walking. In modified technique as the periosteum is not cut in an I-shaped fashion, the flap gives additional strength to new insertion. Patella will act as a fulcrum during the extension of knee by producing the bowstring effect.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Wray JB. Hamstring transfer in management of paralysis of the quadriceps due to poliomyelitis. 1955 Mar [Google Scholar]
- 2.Cergo CH, Jr, Fischer J. Transplantation of the biceps femoris for the relief of the quadriceps femoris paralysis in residual poliomyelitis. J Bone Joint Surg Am. 1931;13:515. [Google Scholar]
- 3.Caldwell GD. Transplantation of the biceps femoris to the patella by the medial route in poliomyelitic quadriceps paralysis. J Bone Joint Surg Am. 1955;37:347–53. [PubMed] [Google Scholar]
- 4.Kleinberg S. The transplantation of the adductor longus in its entirety to supplement the quadriceps femoris. Bull Hosp Joint Dis. 1957;18:117–22. [PubMed] [Google Scholar]
- 5.Riska EB. Transposition of the tractusiliotibialis to the patella as a treatment of Quadricpes paralysis and certain deformities of the lower extremity after poliomyelitis. Acta Orthop. Scand. 1962;32:140–58. doi: 10.3109/17453676208989569. [DOI] [PubMed] [Google Scholar]
- 6.Sutherland David H, Bost Frederic C, Schottstaedt Edwin R. Electromyographic study of transplanted muscles about the knee in poliomyelitis patients. J Bone Joint Surg Am. 1960;42:919. [Google Scholar]
- 7.Shahcheraghi GH, Javid M, Zeighami B. Hamstring tendon transfer for quadriceps femoris paralysis. J Pediatr Orthop. 1996;16:765–8. doi: 10.1097/00004694-199611000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Mukherjee PK, Chaudhury AK, Chaudhury KC, Das AK. Hamstring transfer in Quadricpes paralysis following Poliomyelitis in children. Indian J Ortho. 1980;14:13–9. [Google Scholar]



