Abstract
Cryptococcosis is an invasive fungal infection, which is more common in immunocompromised patients. However, pulmonary cryptococcosis can occur in immunocompetent patients and should be considered on a differential diagnosis for nodular or mass-like lesions in chest radiograph. Recently, we experienced a patient with pulmonary cryptococcosis, successfully treated with oral fluconazole therapy. A 74-year-old female patient was referred for an evaluation of abnormal images, a large consolidative mass with multiple nodular consolidations and small nodules that mimics primary lung cancer with multiple lung to lung metastases. Computed tomography-guided lung biopsy confirmed the diagnosis of pulmonary cryptococcosis. The follow-up image taken after 4 months with oral fluconazole treatment showed marked improvement.
Keywords: Cryptococcosis, Lung Neoplasms, Multiple Pulmonary Nodules
Case Report
A 74-year-old woman was admitted to the hospital for the evaluation of abnormal chest radiograph taken at the private clinic for the routine check-up for her general weakness. She had been well except an essential hypertension diagnosed 20 years ago. Her family history was unremarkable. She was a housewife, working intermittently in the warehouse to make hay for cow feeding. She had no allergies. She did not smoke or drink. Her height was 151 cm and body weight was 67.7 kg. She appeared ill but her mental status was not impaired. She had no respiratory and neurologic symptom or sign. On physical examination, initial vital signs were as follows: blood pressure 159/90 mm Hg, pulse rate 65 beats per minute, body temperature 36.4℃, and respiratory rate 16 breaths per minute. Breathing sound was clear without crackle or wheezing on auscultation. Neurologic examination revealed no specific abnormal finding. Laboratory tests revealed hemoglobin 13.2 g/dL, hematocrit 38.2%, white blood cells 8,260/mm3 (neutrophils 44.3%, lymphocytes 40.8%, monocytes 10.3%, and eosinophils 3.5%), and platelet 255,000/mm3. The results of liver and renal function tests and serum electrolytes were normal. Serum C-reactive protein and erythrocyte sediment rate level was 0.09 mg/dL and 17 mm/hr, respectively. The sereologic tests for hepatitis B and C and human immunodeficiency virus were all negative. Sputum, blood, and urine culture did not reveal any bacterial pathogens. Electrocardiogram showed no abnormal findings.
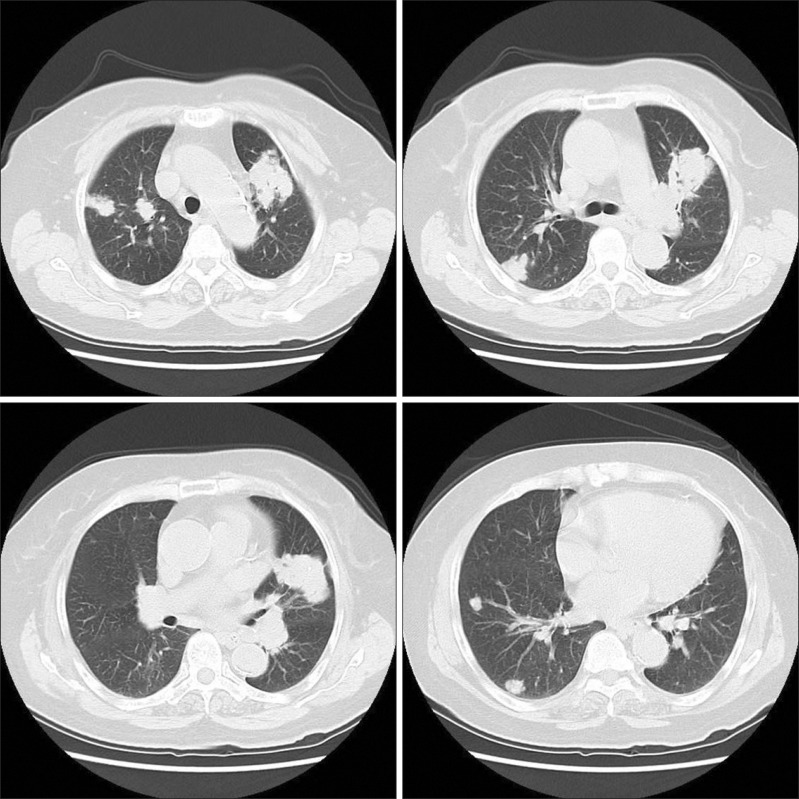
Chest radiograph showed a large irregular shaped mass-like lesion in left upper lobe with multiple nodular opacities in both lungs (Figure 1). Chest computed tomography (CT) revealed a large consolidative mass in left upper lobe (about 10 cm in longest diameter) and multiple nodular consolidations with small nodules, suggesting malignancy or granulomatous inflammation (Figure 2). Pulmonary function was within normal range.
Figure 1.
Simple chest radiograph shows a large irregular mass-like lesion in the left upper lobe with multiple opacities in both lungs.
Figure 2.
Chest computed tomography reveals a large consolidative mass in the left upper lobe (about 10 cm in longest diameter) and multiple nodular consolidations with small nodules in both lungs.
Considering old age and multiple pulmonary nodules leaded us to rule out the possibility of primary lung cancer with lung to lung metastases.
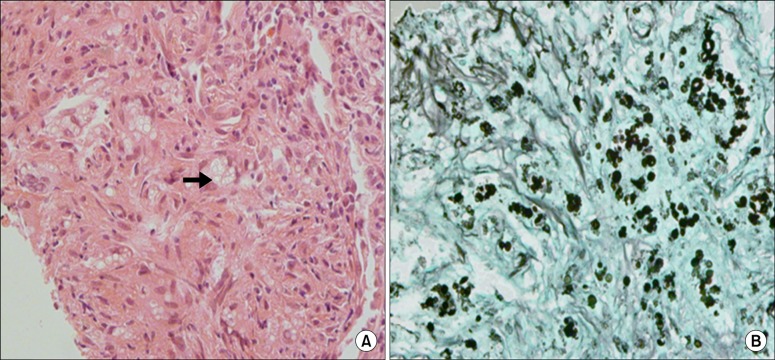
There was no endobronchial lesion on fiberoptic bronchoscopic examination. Microbiologic studies with bronchial washing fluid revealed no bacterial, fungal, or mycobacterial pathogen. For confirmative diagnosis, percutaneous CT-guided biopsy was performed at the mass in left upper lobe. Microscopic findings revealed granulomatous inflammation with multiple yeast forms, morphologically suggestive of cryptococcosis (Figure 3).
Figure 3.
Histologic findings of percutaneous computed tomography-guided biopsy from mass in the left upper lobe. (A) Many yeast-form fungal organisms (arrow) are observed on the hematoxylin and eosin stain (×200). (B) Multiple fungal colonies with some budding yeasts, strongly stained by Gomori's methenamine-silver stain (×200).
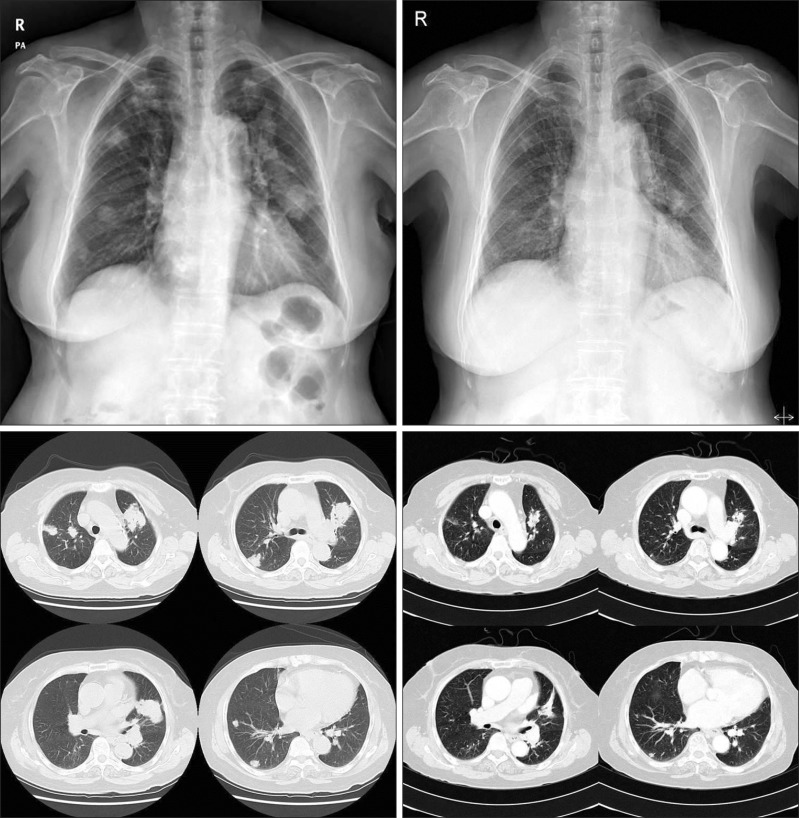
Serum cryptococcal antigen (Ag) was reactive. Lumbar puncture revealed normal cerebrospinal fluid (CSF) opening pressure of 10 cm H2O. CSF microscopy showed no cells and no bacteria or fungus. CSF cryptococcal Ag was non-reactive. The patient was treated with oral fluconazole 400 mg daily according to the recent guidelines. Four months later, she became well without any symptom or sensation of weakness. Follow-up imaging studies showed a marked improvement of previously noted lesions (Figure 4).
Figure 4.
After treatment with oral fluconazole for 4 months, chest radiographs shows significant decrease in size of the consolidative pulmonary mass in the left upper lobe and multiple nodular consolidations with small nodules in both lungs.
Discussion
Cryptococcosis is an invasive fungal infection, caused predominantly by Cryptococcus neoformans or Cryptococcus gattii1. It is an opportunistic infection that was recently estimated at 1 million cases and >600,000 deaths annually2. Cryptococcosis is more common in immune compromised patients. The infection is most often associated with human immunodeficiency virus infection. The other predisposing factors are patients with hematologic malignancies, chronic corticosteroid or immunosuppressive drugs, recipients of solid organ transplants. Cryptococcal infection is acquired by inhalation of aerosolized particles. The clinical presentation of cryptococcal infection varies along a spectrum from asymptomatic pulmonary colonization to severe pneumonia with respiratory failure and life threatening meningitis3. In immunocompromised patients, pulmonary cryptococcosis can be severe and rapidly progressive. However, the disease in immunocompetent patients may be asymptomatic and tends to remain confined to the lung as pulmonary nodules, although some patients develop serious meningitis and disseminated infection4,5.
Symptoms are nonspecific and characterized by cough, fever, dyspnea, chest pain, hemoptysis, malaise, or weight loss6. Many cases are discovered incidentally during the work-up of an abnormal chest radiograph. The most common CT finding in immunocompetent patients is pulmonary nodule, well defined with smooth margin. Multiple nodules are more common than solitary nodule. Consolidation, lymphadenopathy, pleural effusion, and cavitation can occur in the immunocompromised patients7-9.
Diagnosis of pulmonary cryptococcosis requires direct evidence of the presence of cryptococcus in sputum, bronchial washing or bronchoalveolar lavage fluid or lung tissue. Cryptococcal Ag titer can be measured in serum or CSF. Although high titer suggests invasive disease, negative titer does not rule out the diagnosis. The changes in cryptococcal Ag titer reliably reflect the response to therapy10.
The treatment of cryptococcosis depends on the immune status of the host and the site of infection. Pulmonary cryptococcosis in the immunocompetent patient sometimes resolves spontaneously. However, recent guidelines suggest treating even those who are asymptomatic, because dissemination of infection to central nervous system (CNS) in healthy host can occur and low toxicity therapy with fluconazole is availalbe. Mild to moderate disease limited to the respiratory system is usually treated with oral fluconazole in both immunocompetent and immunocompromised hosts (400 mg per day for 6~12 months). Patients with severe disease, CNS involvement, or any other evidence of dissemination are treated with intravenous amphotericin B and flucytosine during induction phase, which is followed by prolonged therapy with oral fluconazole during consolidation phase. Immunocompromised patients remain on lifelong oral fluconazole until their immune impairment resolves or improves11.
Although there are many case reports of pulmonary cryptococcosis in immunocompetent hosts, it is very rare that a huge consolidative mass like our case diagnosed as pulmonary cryptococcosis in a review of literatures12.
In conclusion, we presented a case of 74-year-old patient with pulmonary cryptococcosis mimicking primary lung cancer with multiple lung to lung metastases. Although more common in immunocompromised patients, pulmonary cryptococcosis can occur in immunocompetent patients and should be considered on the differential diagnosis for nodular or mass-like lesions in chest radiograph.
References
- 1.Brizendine KD, Baddley JW, Pappas PG. Pulmonary cryptococcosis. Semin Respir Crit Care Med. 2011;32:727–734. doi: 10.1055/s-0031-1295720. [DOI] [PubMed] [Google Scholar]
- 2.Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23:525–530. doi: 10.1097/QAD.0b013e328322ffac. [DOI] [PubMed] [Google Scholar]
- 3.Hung MS, Tsai YH, Lee CH, Yang CT. Pulmonary cryptococcosis: clinical, radiographical and serological markers of dissemination. Respirology. 2008;13:247–251. doi: 10.1111/j.1440-1843.2007.01202.x. [DOI] [PubMed] [Google Scholar]
- 4.Nadrous HF, Antonios VS, Terrell CL, Ryu JH. Pulmonary cryptococcosis in nonimmunocompromised patients. Chest. 2003;124:2143–2147. doi: 10.1016/s0012-3692(15)31671-8. [DOI] [PubMed] [Google Scholar]
- 5.Goldman JD, Vollmer ME, Luks AM. Cryptococcosis in the immunocompetent patient. Respir Care. 2010;55:1499–1503. [PubMed] [Google Scholar]
- 6.Mylonakis E, Muse VV, Mino-Kenudson M. Case records of the Massachusetts General Hospital. Case 28-2011. A 74-year-old man with pemphigus vulgaris and lung nodules. N Engl J Med. 2011;365:1043–1050. doi: 10.1056/NEJMcpc1102201. [DOI] [PubMed] [Google Scholar]
- 7.Lindell RM, Hartman TE, Nadrous HF, Ryu JH. Pulmonary cryptococcosis: CT findings in immunocompetent patients. Radiology. 2005;236:326–331. doi: 10.1148/radiol.2361040460. [DOI] [PubMed] [Google Scholar]
- 8.Song KD, Lee KS, Chung MP, Kwon OJ, Kim TS, Yi CA, et al. Pulmonary cryptococcosis: imaging findings in 23 non-AIDS patients. Korean J Radiol. 2010;11:407–416. doi: 10.3348/kjr.2010.11.4.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choe YH, Moon H, Park SJ, Kim SR, Han HJ, Lee KS, et al. Pulmonary cryptococcosis in asymptomatic immunocompetent hosts. Scand J Infect Dis. 2009;41:602–607. doi: 10.1080/00365540903036212. [DOI] [PubMed] [Google Scholar]
- 10.Chang WC, Tzao C, Hsu HH, Lee SC, Huang KL, Tung HJ, et al. Pulmonary cryptococcosis: comparison of clinical and radiographic characteristics in immunocompetent and immunocompromised patients. Chest. 2006;129:333–340. doi: 10.1378/chest.129.2.333. [DOI] [PubMed] [Google Scholar]
- 11.Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010;50:291–322. doi: 10.1086/649858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garrett L, Marr K, West S, Allada G. 74-year-old man from the pacific northwest with fever and a lung mass. Chest. 2011;140:814–817. doi: 10.1378/chest.10-2964. [DOI] [PubMed] [Google Scholar]