Abstract
Aims
This study aimed to: 1) provide relative risk (RR) estimates between acute alcohol use and injuries from emergency departments in the Dominican Republic, Guatemala, Guyana, Nicaragua and Panama, and 2) test whether the RR differs if two control periods for the estimates were used.
Design
Case-crossover methodology was used to obtain estimates of the RR of having an injury within six hours after drinking alcohol, using a pair-matching design with control periods of the same time of day the day prior to injury, and the same time of day and day of week the week prior to injury.
Setting
Emergency departments(EDs).
Participants
2,503 injured patients from EDs were interviewed between 2010–2011, with a response rate of 92.6%.
Measurements
Number of drinks consumed within six hours prior to the injury and in the two control periods.
Findings
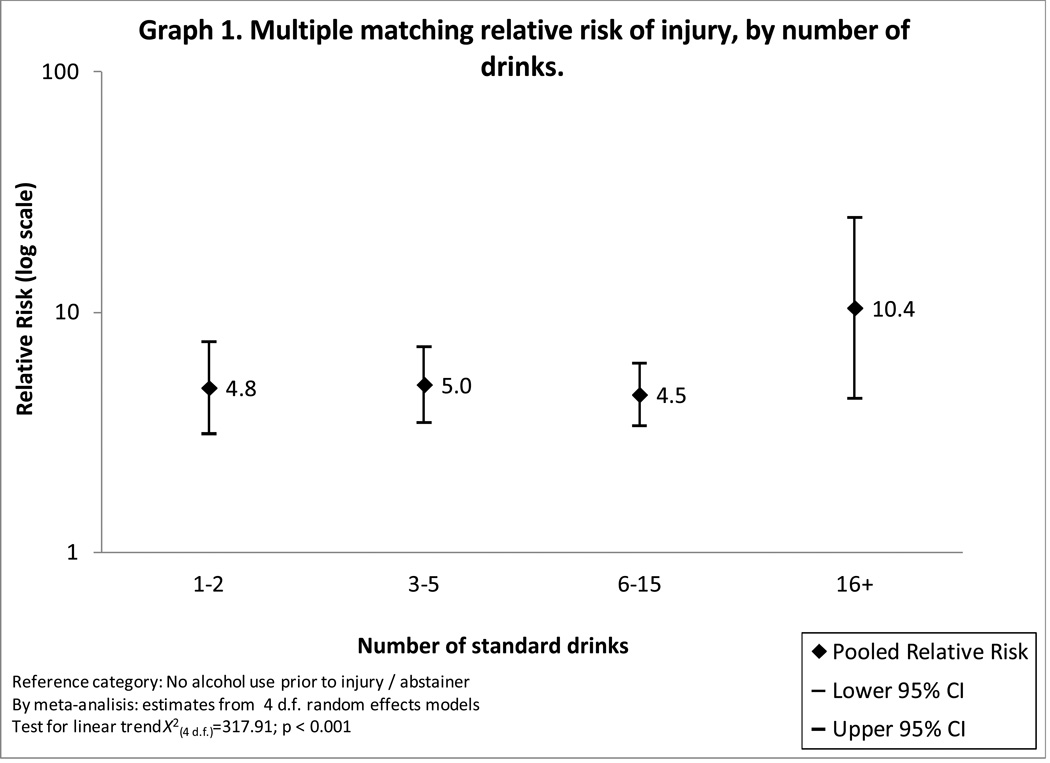
The RR of injury after drinking alcohol was 4.38 (95% confidence interval CI= 3.29–5.84) using as the control period the prior week, and 5.35 (CI=3.50–8.17) using as a control period the prior day. The RR was 5.08 (CI=4.15–6.23) in multiple matching. Those drinking 1–2 drinks had a RR of 4.85 (CI=3.12–7.54); those drinking 3–5 a RR of 5.00 (CI =3.47–7.18); those drinking 6–15 a RR of 4.54 (CI=3.36–6.14); and those drinking 16 or more a RR of 10.42 (CI=4.38–24.79).
Conclusions
As in other countries, alcohol drinking is a trigger for an injury in all five countries. The use of more than one control period give further strength to these findings from case-crossover analysis.
Keywords: alcohol, emergency department, injury, epidemiology, case-crossover
INTRODUCTION
Alcohol is causally associated with a number of medical conditions and injuries [1], exerting a heavy burden to society [2]. Injuries are one of the largest contributors to this burden, and those related to violence, are a key component of the burden of disease in Latin America [3,4]. In this region, among all disability-adjusted life years associated with alcohol, 34% belong to unintentional injuries and 25% belong to intentional injuries [4]. It has also been estimated that 24% of the homicides, 11% of the suicides and 20% of traffic accidents is associated to alcohol [2], with a burden generally higher in the America region than that for other regions of the globe [4].
Despite the prominent role that alcohol has in the epidemiological profile of the region, few estimates of the relative risk (RR) for an injury after alcohol consumption are available for Latin American countries [5]. Estimates of the RR of an injury within six hours after alcohol consumption are available in the international literature using the case-crossover methodology, primarily with a pair-matching design in which the same day of the week, during the week prior to the injury, is used as the control period [6,7]. Since people tend to forget their drinking as time passes, this comparison period may be subject to recall bias and the use of other periods, more proximal to the injury period, such as the day prior to the injury, has been advocated [6,8,9,10]. A recent review [11] that provided meta-analyses for several types of injuries, but primarily focusing on traffic and violence related injuries, concluded that case–crossover studies of non-motor vehicle injury result in overall higher risks than case–control studies, further arguing for more studies using different control periods in case-crossover studies. This paper presents data on five recently completed studies on alcohol and injuries in emergency departments (EDs), sponsored by the Pan-American Health Organization (PAHO) and undertaken in five countries in the Latin American and Caribbean region. In countries of Latin America and the Caribbean, alcohol has been associated with aggression and injury [12] and more generally with partner violence [13], making ED studies particularly appealing. The goals of this study were to provide further evidence for the association between acute alcohol use and injury for Latin America and the Caribbean, and to test whether this association is different between RR estimates based on two different control periods: the day prior to the injury and the same day of the injury in the week before.
MATERIALS AND METHODS
Sample
Data from the PAHO study on alcohol and injuries were collected in 2010–2011 from EDs in the Dominican Republic, Guatemala, Guyana, Nicaragua and Panama. The methods used were similar to those used previously in ED studies from the World Health Organization (WHO) Collaborative Study on Alcohol and Injury [14]. Following the WHO standard protocol, probability samples were drawn from patients admitted within 6 hours of an injury at each site; each shift during each day of the week was represented equally in the sampling. The target sample size was 500 patients from each site. Patients were approached as soon as possible to obtain informed consent for participation in the study. The total sample size of participants aged 18 years or older was 2,503 patients, representing a 92.6% response rate. Interviewers were trained and supervised by study collaborators. Interviewers administered a standard 25-minute questionnaire. Further details on the general methodology, questionnaire development and training for the WHO study and the associated PAHO study can be found elsewhere [15,16]. Ethical approval was obtained from institutional review boards in each participating country, as well as by the PAHO Ethics Review Committee.
Interview and measures
The interview included questions on whether the participant reported drinking during the 6 hours before the injury, an estimate of the amount of alcohol consumed during this period and the same 6-hour period in the previous day and the previous week, and the usual quantity of alcohol consumed and frequency of use during the past year [8]. Questions on quantity and frequency of drinking were based on questionnaires used in a number of prior ED studies [17,16]. A binary variable for usual drinking of high quantities per occasion (binge drinking) was created, indicating whether the patient usually had 5 or more drinks on an occasion for men, and 4 or more drinks for women (5+/4+), based on the question: "when you drink wine, beer or hard liquor, how many drinks do you usually have at one time?". Participants were also asked the four questions that comprise the Rapid Alcohol Problems Screen (RAPS4), as a screening measure of alcohol dependence [18]. The type of injury was assessed with a single question, and categorized here as either unintentional (not related to violence) or intentional (related to violence).
Data analysis
Patients who reported drinking at any time within the 6 hours prior to injury were considered exposed cases. The volume of alcohol consumed during the 6-hour period was analyzed by converting the number and size of drinks of wine, beer, spirits and local beverages to pure ethanol, and summing across beverage types, using a standard drink size of 16 ml as a common volume measure across beverages. The pair-matching approach compared the reported use of alcohol of each patient during the 6 hours prior to injury with their respective use of alcohol during the same time period on the day prior to injury, and on the same day in the previous week. For alcohol use, during the 6 hours prior to injury, patients were asked: “In the 6 hours before and up to you having your injury/accident, did you have any alcohol to drink, even one drink?” (yes/no). Information on alcohol use at the same time in the previous week was elicited as follows: “In this next section, I am going to ask you about what you were doing exactly one week ago. Think about the time you had your accident (today) and remember the same time a week ago. Last week at the same time, did you have any alcohol to drink in the 6 hours leading up to this time?” (yes/no). Similar questions were asked to obtain data on alcohol use on the day prior to injury. These two control periods were combined for multiple (2:1) matching. The number of drinks consumed on each of the three occasions was obtained and transformed into a measure of volume, as described above. Conditional logistic regression was used to calculate matched-pair RRs and 95% confidence intervals (CI) [19]. Variation in the magnitude of the RR across levels of fixed characteristics, such as age, was examined using the χ2 test of homogeneity [20]. After obtaining the RR estimate for each study site, a pooled random RR was obtained across studies (Table 3 and 4). Meta-analysis was used to calculate those pooled RR, and further tests of homogeneity on the random effects RR were performed by possible effect modifiers [21]. We chose to report only random effects because the different countries sampled were regarded as exerting a random effect on all estimates. Linear trend and dose-response associations across categories of number of drinks were assessed examining the incremental risk ratios [22].
Table 3.
Distribution and association of alcohol use prior to injury and different control periods.
| Matched pairs distribution | Pooled estimate** | |||||
| Alcohol week prior* | RR | CI 95% | ||||
| Yes | No | |||||
|
Alcohol prior to injury* |
% | (n/N) | % | (n/N) | ||
| Yes | 24.48 | (118/482) | 75.52 | (364/482) | ||
| No | 4.36 | (82/1880) | 95.64 | (1798/1880) | ||
| Total | 8.47 | (200/2362) | 91.53 | (2162/2362) | 4.38 | (3.29–5.84) |
| Alcohol day prior* | ||||||
| Yes | No | |||||
| % | (n/N) | % | (n/N) | |||
| Yes | 24.65 | (122/495) | 75.35 | (373/495) | ||
| No | 3.72 | (70/1883) | 96.28 | (1813/1883) | ||
| Total | 8.07 | (192/2378) | 91.93 | (2186/2378) | 5.35 | (3.50–8.17) |
| Multiple matching*** | 5.08 | (4.15–6.23) | ||||
Self-report
By meta-analysis: estimates from 4 df random effects models
Multiple matching with both prior day and week as control periods
RR - Relative Risk; CI - Confidence Interval; df - degrees of freedom
Table 4.
Alcohol-related injury. Pooled multiple matching estimates, by relevant demographic and type of injury variables.
| Pooled estimate* | |||
|---|---|---|---|
| RR | CI 95% | ||
| Sex | |||
| Female | 5.75 | (3.10–10.66) | |
| Male | 5.02 | (4.06–6.22) | |
| Age | |||
| < 30 years | 5.26 | (3.98–6.95) | |
| >= 30 years | 4.91 | (3.34–7.23) | |
| Violence-related injury** | |||
| No | 3.96 | (3.03–5.18) | |
| Yes | 6.93 | (5.04–9.54) | |
| Positive RAPS | |||
| No | 4.94 | (3.71–6.59) | |
| Yes | 5.20 | (3.18–8.50) | |
By meta-analysis: estimates from 4 df random effects models
p < 0.05
RR - Relative Risk; CI - Confidence Interval; df - degrees of freedom
RESULTS
The total response rate was 92.6%, with a range of 84.7% to 98.6%. Table 1 presents socio-demographic and alcohol use characteristics across the five countries. In all sites, injured patients were predominately male and close to half or more were over the age of 30. The age range was 18–94 years. Educational attainment varied considerably, with Guyana showing the largest proportion with at least some college, and the Dominican Republic showing the lowest proportion with at least some college. Alcohol prior to the injury was similar across all countries, ranging from 19.3% to 21.5%.
Table 1.
Socio-demographic and drinking characteristics. Emergency Department Collaborative study on alcohol and injuries. Pan American Health Organization, 2010–2011.
| Socio-demographic variables* | ||||||
|---|---|---|---|---|---|---|
| Country | N | Males % |
Age >= 30 years old % |
Some college or above % |
Alcohol use before injury** % |
|
| Guatemala | 513 | 69.4 | 53.6 | 8.4 | 21.1 | |
| Guyana | 485 | 72.4 | 56.8 | 36.8 | 21.0 | |
| Nicaragua | 518 | 69.1 | 46.8 | 16.9 | 21.5 | |
| Panama | 490 | 68.4 | 58.4 | 16.0 | 20.8 | |
| Dominican Republic | 497 | 80.8 | 46.9 | 8.0 | 19.3 | |
| Total | 2,503 | 71.9 | 52.4 | 17.1 | 20.8 | |
Missing values: gender (n=8), age (n=24), education (n=90) and alcohol use (n=42) distributed across countries
Self-report of alcohol use six hours prior to injury
Close to a third of this sample were admitted to the ED due to a violent-related injury (Table 2), with higher prevalence of violence among males. Patients that entered the ED for a violence-related injury tended to be younger (mean age 30 years) compared to non-violence injured patients (mean age 36 years) (data not showed in table). Alcohol use was common, with almost two-thirds of the sample being a current drinker (reporting drinking in the last 12 months), and 20.8% reporting drinking prior to the injury event. A little over a quarter of the patients (26.4%) were positive on the RAPS4 (reporting one or more of the four items in the last year) and 35.2% reported consuming 5 or more drinks (males; 4 or more for females) on at least one occasion during the last year.
Table 2.
Violence and alcohol use distribution in the Emergency Department, by gender.
| Gender | Total | |||||
|---|---|---|---|---|---|---|
| Female | Male | |||||
| % | (n/N) | % | (n/N) | % | (n/N) | |
| Violence-related injury | 23.4 | (161/688) | 31.7 | (558/1760) | 29.4 | (719/2448) |
| Current drinkers* | 38.7 | (266/687) | 75.0 | (1315/1754) | 64.8 | (1581/2441) |
| Alcohol use before injury** | 7.8 | (54/692) | 26.0 | (457/1761) | 20.8 | (511/2453) |
| Usual high quantity*** | 17.2 | (115/667) | 42.6 | (691/1621) | 35.2 | (806/2288) |
| Positive RAPS**** | 11.1 | (76/685) | 32.4 | (566/1747) | 26.4 | (642/2432) |
Missing values: gender (n=8), violence (n=47), current drinkers (n=54), alcohol use (n=42), usual high quantity (n=207), RAPS (n=63), distributed across countries
Patients who had at least one drink of any alcoholic beverage in the last 12 months
Self-report of alcohol use six hours prior to injury
Defined as usual five or more drinks for men and four or more drinks for women
A positive answer in any of the four RAPS items: Remorse, Amnesia ('blackouts'), Perform or Starter ('eye-opener')
Table 3 presents the distribution of alcohol consumption within six hours prior to the injury by consumption during the same six-hour period the week prior and the day prior to the injury. Based on drinking the week prior as the control period, the pooled random estimate of the RR of injury was 4.38 (95% CI=3.29–5.84), while the pooled random estimate of RR, based on the prior day as the control period, was 5.35 (CI=3.50–8.17).Based on multiple matching, in which both control periods are taken into account, the pooled random effect RR was 5.08 (CI=4.15–6.23).
RRs were then estimated separately, using the multiple matching approach, for several possible effect modifiers (Table 4). As seen in Table 4, the only variable that produced a significant effect modification was type of injury, with those with a violent-related injury having a higher RR (6.93) compared to those with a non-violent injury (RR=3.96) (χ2=6.90, p=0.009).
Multiple matching was also used to estimate a dose-response relationship between the number of drinks consumed and the RR of an injury (Figure 1), using again a random effects model from meta-analyses. We selected those drinking cut-points based on a data driven approach, trying to estimate associations for low level of drinks while keeping sample sizes under consideration. Those consuming 1–2 drinks had a RR of 4.85 (CI =3.12–7.54), those consuming 3–5 had RR of 5.00 (CI = 3.47–7.18), those consuming 6–15 had RR of 4.54 (CI= 3.36–6.14) and 16 or more, a RR of 10.42 (CI=4.38–24.79). The chi-squared test for a linear trend was significant (<0.001), but a conservative inspection of the incremental risk ratios across categories in Figure 1 suggested no monotonic dose-response, with those in the middle drinking categories showing similar RRs compared to those in the lowest level of drinking, but a larger RR was apparent for those in the highest level of drinking.
Figure 1.
DISCUSSION
Findings here show that about 20% of the patients across these countries reported drinking within six hours prior to the injury that brought them to the ED, with the likelihood of sustaining an injury elevated more than four-fold (RR=4.38), based drinking during the same time the prior week, and over five-fold (RR=5.35), based on drinking during the same time the day prior, and a summary RR of 5.08 combining both control time periods. The only variable that acted as an effect modifier for this relationship was intentionality of the injury, with intentional injuries showing a significantly elevated RR compared to unintentional injuries. Patients who consumed more, especially at the very high-end level of drinking, had a much higher RR of sustaining an injury than those drinking more modest quantities.
The prevalence of drinking prior to the injury was within the range of previous similar studies in the ED, which have ranged from 6.3% to 46.4% [7]. Analysis of three Latin American countries from the WHO Collaborative Study found that the prevalences of drinking six hours prior to the injury were of: 27.8% in Argentina, 12.8% in Brazil and 17.2% in Mexico [7]. Prevalences reported here appear to be at the upper-end of this spectrum compared to other countries in the Americas region. The RR, based on the week prior compared to the estimates based on the same time period in the 12-country WHO Collaborative Study [14] was similar, with an RR of 5.7 in that study. In addition, this study found that those with a violent-related injury had a RR of 6.9, considerably lower than the RR of 15.0 reported for Argentina, Brazil and Mexico [5]; while the RR for non-violent injuries in the current study was 3.96, quite similar to the RR of 4.2 for the same group of countries. This research, alone, cannot elucidate the reasons for these differences in RR for cases of violent-related injury. However, another study across a number of countries on the differences between violent and non-violent injury cases found that the larger RR for violence, and the lack of homogeneity across countries was explained, in part, by the level of detrimental drinking pattern in a country, which is based on heavy drinking occasions, drinking with meals, and drinking in public places in a country [23]. Future research on a larger number of countries in the Latin American and Caribbean region with emergency department data may shed further light on the heterogeneity of RR among countries for violent-related injuries.
Overall, the RR estimate from the pooled sample using as a control period the same day of the week, during the week prior (RR of 4.38), and the RR estimate using the day prior as the control group (RR of 5.35) point in the same direction and are remarkably close to each other. This finding is basically similar to what was previously reported in Mexico for three different control periods [14], as well to a similar research in 1995 [6], and more recently for a group of cases of myocardial infarction [9], but not by others [24]. Since there is no acceptable way to define a gold standard as a control time period for case-crossover studies, the most advisable conclusion would be to work with as many control periods as possible and to produce a multiple matching estimate. This multiple matching is not only more precise; but it also combines possible upward and downward unidentifiable biases to produce a single estimate. Quantifying similarities and differences from multiple methodological approaches seems a more reasonable strategy [11,25,26,27] than just pursuing some undefined and supposedly unbiased time-control period.
Some estimates of dose-response from case-crossover studies for acute alcohol use are reported in the literature. Estimates here suggest that the risk is high at low levels of consumption (1–2 drinks), and remains relatively stable until high levels of consumption are reached (16 or more drinks), where the risk increases sharply. Pooled data from the WHO Collaborative Study [25] suggest risk remains relatively stable up to six drinks, and then increases sharply, but sharper increases for violent-related injuries have been reported for other countries in the Americas [14]. Reports of both smooth and sharp increases have also been reported elsewhere [5]. Regardless of the shape of the curve, these studies and a meta-analyses [6,26] show similarities; even the low levels of drinking are associated with increases in risk for injury. Future studies from our group, using a larger number of EDs across the globe, will provide a larger sample size to more fully address the important issue on the shape of the curve for the relationship between number of drinks and injury, as this has important implications for public health. Overall, our results suggest that public health messages in the region should include all drinkers, not only high-level drinkers.
Limitations
This study is limited to analysis of data from patients with non-fatal injuries who attended specific EDs. Although the study design provides a representative sample of patients from each facility, patients may not be representative of other facilities in the city or the country. Additionally, as is common with other studies conducted in EDs, cases cannot be assumed to be representative of other individuals who were injured but did not seek medical attention. All analyses reported here are based on the patient’s reported alcohol consumption across different times, and it is possible that participants were more likely to recall their consumption more accurately immediately before an injury than during any previous period, thereby producing an overestimate of the association between alcohol and injury. Prior case-crossover research on alcohol consumption and injury has used other control periods [11] ranging from a day to a year, and findings of relative risk have been found to vary. Legal or other issues, however, may encourage patients to minimize their reports of drinking prior to an injury, as in the case of drivers in motor vehicle accidents. On the other hand, it is also possible that patients may overestimate their drinking. For example, those with violence-related injuries may over-report alcohol consumption to excuse behavior that would otherwise be viewed as socially unacceptable [6,26,8,28]. Clearly, more research on the validity of methods for eliciting alcohol use in case-crossover analyses is needed. Despite the fact that case-crossover studies are well suited to control for between-person confounders, they do not remove the possibility that within-person confounders may exist, for example that acute alcohol use followed an acute episode of cocaine use. Because we lack measures of other variables that vary over time, such as cocaine use, and that could be considered possible confounders of the relationship between acute alcohol use and injury, we are not able to adjust for these potential biases.
Conclusions
In spite of these limitations, this study suggests that, in these five countries, as in other regions and countries, alcohol is a trigger for an injury. The use of more than one control period, with similar findings, provides additional strength to prior findings of the risk of injury from alcohol, using the case-crossover design. These findings have important implications for Latin America and the Caribbean: patients should be encouraged to abstain or decrease their drinking, in order to avoid possible injuries, especially those related to violence. Alcohol policies aimed at reducing overall consumption would decrease the prevalence of alcohol-related injuries among both men and women.
Acknowledgements
Funding for this study comes from the Pan American Health Organization and Generalitat Valenciana, Spain, and in part by a grant from the U.S. National Institute on Alcohol Abuse and Alcoholism (RO1 2 AA013750-04).
Footnotes
Declaration of interest
No authors have financial interests or potential conflicts of interests to report.
REFERENCES
- 1.Rehm J, Baliunas D, Borges G, Graham K, Irving H, Kehoe T, et al. The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction. 2010;105:817–843. doi: 10.1111/j.1360-0443.2010.02899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Room R, Babor T, Rehm J. Alcohol and public health. Lancet. 2005;365:519–530. doi: 10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- 3.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerewattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 4.Rehm J, Monteiro M. Alcohol consumption and burden of disease in the Americas: implication for alcohol policy. Rev Panam Salud Publica. 2005;18:241–248. doi: 10.1590/s1020-49892005000900003. [DOI] [PubMed] [Google Scholar]
- 5.Borges G, Orozco R, Cremonte M, Buzi-Figlie N, Cherpitel C, Poznyak V. Alcohol and violence in the emergency department: a regional report from the WHO collaborative study on alcohol and injuries. Salud Publica Mex. 2008;50:S6–S11. doi: 10.1590/s0036-36342008000700003. [DOI] [PubMed] [Google Scholar]
- 6.Vinson D, Mabe N, Leornard L, Alexander J, Becker J, Boyer J, et al. Alcohol and injury. A case-crossover study. Arch Fam Med. 1995;4:505–511. doi: 10.1001/archfami.4.6.505. [DOI] [PubMed] [Google Scholar]
- 7.Borges G, Cherpitel C, Orozco R, Bond J, Ye Y, Macdonald S, et al. Acute alcohol use and the risk of non-fatal injury in sixteen countries. Addiction. 2006;101:993–1002. doi: 10.1111/j.1360-0443.2006.01462.x. [DOI] [PubMed] [Google Scholar]
- 8.Borges G, Cherpitel C, Mondragón L, Poznyak V, Peden M, Gutierrez I. Episodic alcohol use and risk of nonfatal injury. Am J Epidemiol. 2004;159:565–571. doi: 10.1093/aje/kwh073. [DOI] [PubMed] [Google Scholar]
- 9.Gerlich M, Rehm J. Recall bias in case-crossover designs studying the potencial influence of alcohol consumption. Journal of Studies on Alcohol and Drugs. 2010;71 doi: 10.15288/jsad.2010.71.619. 619-author reply 620-1. [DOI] [PubMed] [Google Scholar]
- 10.Thornley S, Kool B, Robinson E, Marshall R, Smith G, Ameratunga S. Alcohol and risk of admission to hospital for unintentional cutting or piecing injuries at home: a population based case-crossover study. Public Health. 2011;11:852. doi: 10.1186/1471-2458-11-852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor B, Irving H, Kanteres F, Room R, Borges G, Cherpitel C, et al. The more you drink, the harder you fall: a systematic review and meta-anlysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend. 2010;110:108–116. doi: 10.1016/j.drugalcdep.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Monteiro MG, Telles-Dias P, Inglez-Dias A. Epidemiología del uso del alcohol y otras sustancias psicoactivas en América Latina y el Caribe. In: Monteiro MG, Telles-Dias P, Inglez-Dias A, editors. Epidemiolog a de los trastornos mentales en América Latina y el Caribe. Washington, D.C: Organización Panamericana de la Salud; 2009. pp. 177–193. [Google Scholar]
- 13.Pan American Health Organization. Unhappy hours: alcohol and partner aggression in the Americas. Washington, D.C: PAHO; 2009. [Google Scholar]
- 14.Borges G, Cherpitel C, Orozco R, Bond J, Ye Y, Macdonald S, et al. Multicentre study of acute alcohol use and non-fatal injuries: data from the WHO collaborative study on alcohol and injuries. Bull World Health Organ. 2006;84:453–460. doi: 10.2471/blt.05.027466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Management of substance abuse. [Accessed 2011-12-5];Alcohol and injuries. 2011 Nov 20; URL: http://www.who.int/substance_abuse/publications/en/AlcoholInjuriesFactSheet.pdf. (Archived by WebCite® at http://www.webcitation.org/64q6AuNdG)
- 16.Cherpitel C, Ye Y, Bond J, Rehm J, Rehm J, Poznyak V, et al. Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) and the WHO Collaborative Study on Alcohol and Injuries. Multi-level analysis of alcohol-related injury among emergency department patients: a cross-national study. Addiction. 2005;100:1840–1850. doi: 10.1111/j.1360-0443.2005.01257.x. [DOI] [PubMed] [Google Scholar]
- 17.Cherpitel C. Drinking patterns and problems associated with injury status in emergency room admissions. Alcohol Clin Exp Res. 1988;12:105–110. doi: 10.1111/j.1530-0277.1988.tb00141.x. [DOI] [PubMed] [Google Scholar]
- 18.Cherpitel C. A brief screening instrument for problem drinking in the emergency room: the RAPS4 Rapid Alcohol Problem Screen. J Stud Alcohol. 2000;61:447–449. doi: 10.15288/jsa.2000.61.447. [DOI] [PubMed] [Google Scholar]
- 19.Maclure M. The case-crossover desing: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133:144–153. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- 20.Rothman K, Greenland S. Modern Epidemiology. 2nd edn. Philadelphia: Lippincott-Raven; 1998. [Google Scholar]
- 21.Sutton A, Abrams K, Jones D, Sheldon T, Song F. Methods for Meta-Analysis in Medical Research. Chichester, UK: John Wiley and Sons; 2000. [Google Scholar]
- 22.Maclure M, Greenland S. Test for trend and dose response: misinterpretations and alternatives. Am J Epidemiol. 1992;135:96–104. doi: 10.1093/oxfordjournals.aje.a116206. [DOI] [PubMed] [Google Scholar]
- 23.Cherpitel C, Ye Y. Alcohol and violene-related injuries among emergency room patients in an international perspective. J Am Psychiatr Nurses Assoc. 2010;16:227–235. doi: 10.1177/1078390310374876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gmel G, Daeppen J. Recall bias for seven-day recall measumerement of alcohol consumption among emergency department patients: implications for case-crossover designs. Journal of Studies on Alcohol and Drugs. 2007;68:303–310. doi: 10.15288/jsad.2007.68.303. [DOI] [PubMed] [Google Scholar]
- 25.Vinson D. Studying associations between alcohol and acute events: problems and promise [Letter to the editor] J Stud Alcohol Drugs. 2010;71:622–623. doi: 10.15288/jsad.2010.71.622. [DOI] [PubMed] [Google Scholar]
- 26.Vinson D, Maclure M, Reidinger C, Smith G. A population-based case-crossover and case-control study of alcohol and the risk of injury. J Stud Alcohol. 2003;64:358–366. doi: 10.15288/jsa.2003.64.358. [DOI] [PubMed] [Google Scholar]
- 27.Wacholder S, Silverman D, McLaughlin J, Mandel J. Selection of controls in case-control studies II. Types of controls. Am J Epidemiol. 1992;135:1029–1041. doi: 10.1093/oxfordjournals.aje.a116397. [DOI] [PubMed] [Google Scholar]
- 28.Borges G, Cherpitel C, Mittlelman M. Risk of injury after alcohol consumption: a case-crossover study in the emergency department. Soc Sci Med. 2004;58:1191–1200. doi: 10.1016/s0277-9536(03)00290-9. [DOI] [PubMed] [Google Scholar]