Abstract
Background
Substantial acetabular cartilage damage is commonly present in patients suffering from femoral acetabular impingement (FAI). A better understanding of which patient is at risk of developing substantial cartilage damage is critical for establishing appropriate treatment guidelines.
Questions/Purposes
We asked: (1) Does the cam deformity severity in FAI as assessed by alpha angle predict acetabular cartilage delamination? And (2) what are the clinical and radiographic findings in patients with acetabular cartilage delamination?
Methods
One hundred sixty-seven patients (129 males, 38 females) with a mean age of 38 years (range, 17–59 years) underwent joint preservation surgery for cam-type FAI. All data were collected prospectively. We assessed center-edge angle and Tönnis grade on AP radiographs and alpha angle on specialized lateral radiographs. Acetabular cartilage damage was assessed intraoperatively using the classification of Beck et al., with Type 3 and greater qualifying as delamination.
Results
For all hips, mean alpha angle was 65.5° (range, 41°–90°), and mean center-edge angle was 33.3° (range, 21°–52.5°). Patients with an alpha angle of 65° or greater had an odds ratio (OR) of 4.00 (95% CI, 1.26–12.71) of having Type 3 or greater damage. Increased age (OR, 1.04; 95% CI, 1.01–1.07) and male sex (OR, 2.24; 95% CI, 1.09–4.62) were associated with Type 3 or greater damage, while this was the opposite for acetabular coverage as assessed by center-edge angle (OR, 0.94; 95% CI, 0.89–0.99).
Conclusions
Patients with cam-type FAI and an alpha angle of 65° or more are at increased risk of substantial cartilage damage while increasing acetabular coverage appears to have a protective effect.
Level of Evidence
Level III, prognostic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
The presence of acetabular cartilage damage at the time of femoroacetabular impingement (FAI) surgery is well documented, ranging from 44% to 75% [6, 9, 22]. More importantly, the pattern of cartilage damage is strongly influenced by the morphologic abnormality present. Pincer-type FAI demonstrates a more peripheral damage to the labrum, whereas cam-type primarily leads to acetabular cartilage damage leaving the labrum intact. In both pincer and cam FAI, the resulting damage to the cartilage of the hip is thought to be secondary to abnormal contact between the femoral head-neck and the anterosuperior acetabular rim [12]. For cam FAI, it has been postulated an outside-in damage leads to the avulsion of the acetabular cartilage from the labrum and subchondral bone, with Type 3 (cartilage debonded from the acetabular surface but no visible cleft) and Type 4 (same as Type 3 but with cleavage of the flap) [9] being of greater severity. Recent literature suggests the presence of a cam deformity (as quantified by the alpha angle) predicts the development of hip pain [1] and is an independent risk factor for the presence of acetabular cartilage delamination [3, 15]. Having said that, one recent study suggests 14% of the normal population will have morphology consistent with cam FAI without being symptomatic [13]. Consequently, understanding what clinical and radiographic variables put the patient at risk of developing such lesions is crucial in our understanding of the natural history of this morphologic abnormality and in the development of appropriate treatment guidelines.
We therefore (1) determined whether the severity of cam deformity as assessed by the alpha angle is predictive of acetabular cartilage delamination and (2) described the clinical (age, sex, BMI) and radiographic (Tönnis grade, acetabular coverage) characteristics of patients with cartilage delamination.
Patients and Methods
We prospectively followed all 176 patients (189 hips) with a diagnosis of cam FAI who underwent joint preservation surgery from September 2005 to August 2011. The indications for hip preservation surgery were (1) persistent hip pain for greater than 6 months, (2) labral tear on MRI, and (3) failed nonsurgical management including a course of antiinflammatory agents. The contraindications were (1) moderate hip arthritis of Tönnis Grade 2 or more and (2) age of greater than 60 years. Patients with a cam deformity but with a center-edge angle of less than 20° (n = 9) were excluded, as their hips were considered dysplastic, leaving us with 167 patients (180 hips). There were 129 males and 38 females, with a mean age of 38.4 years (range, 17.2–59.7 years) and a mean BMI of 26.9 (SD, 4.0). All patients consented to be entered into the study after institutional ethics approval.
All patients had a well-centered AP radiograph controlling for rotation (tip of coccyx aligned with symphysis pubis) and tilt (distance between sacrococcygeal junction and symphysis between 3 and 4 cm). On the AP radiograph, the center-edge angle of Wiberg [28] was measured with a mean value of 33.3° (range, 21°–52.5°). Presence of acetabular retroversion was assessed using the crossover sign, with 45 of the 180 (25%) hips having a crossover sign. Tönnis grade [27] for osteoarthritis was assessed as follows: Grade 0, no signs of osteoarthritis; Grade 1, increased sclerosis of the head and acetabulum; Grade 2, small cysts in femoral head or acetabulum, increasing narrowing of joint space, and moderate loss of sphericity of femoral head; and Grade 3, large cysts, severe narrowing or obliteration of joint space, severe deformity of femoral head, and avascular necrosis. Seventy-four hips (41.1%) were Grade 0, 83 hips (46.1%) Grade 1, 23 hips (12.8%) Grade 2, and no hips Grade 3. One of us (PEB) independently measured the alpha angle [23, 26] on specialized lateral view radiographs (crosstable lateral with the leg in 15° of internal rotation or Dunn view) [21]. For all hips, the mean alpha angle was 65.5° (range, 41°–90°).
In addition, all patients underwent MRI with gadolinium arthrography (MRA) of their hips confirming a labral tear. An observer (PEB) viewed all radiographs and made measurements using a PACS system (Horizon Medical Imaging™; McKesson Medical Imaging, San Francisco, CA, USA). Previous studies describing the use of alpha angle measurement showed intra- and interobserver variations of ± 3% and ± 7%, respectively [23], and an interclass correlation coefficient of 0.810 and 0.796 on the axial and radial views, respectively [13].
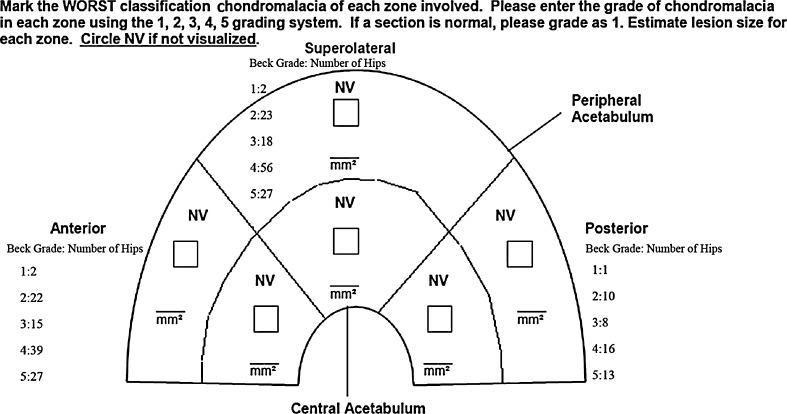
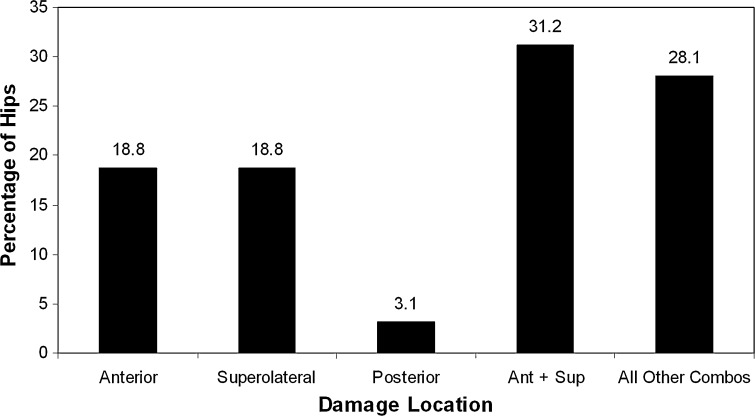
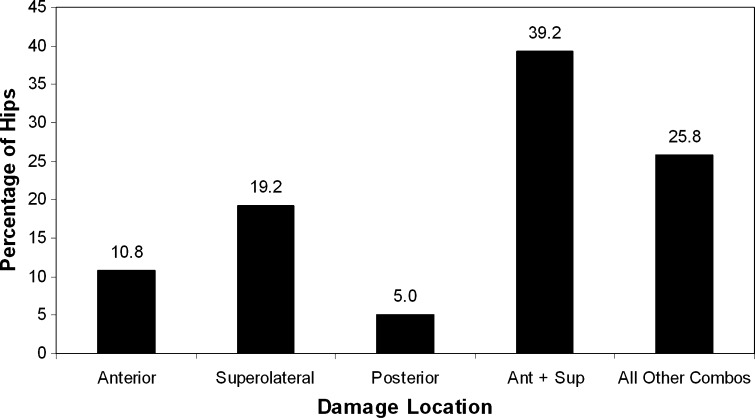
One surgeon (PEB) performed all surgeries and assessed acetabular cartilage damage using the classification of Beck et al. [9]: Type 1, normal cartilage; Type 2, malacia/fibrillation; Type 3, chondral delamination with no cleavage; Type 4, chondral delamination with cleavage; and Type 5, exposed subchondral bone. Twenty-two hips (12.2%) had Type 1, 32 hips (17.8%) Type 2, 26 hips (14.4%) Type 3, 64 hips (35.6%) Type 4, and 36 hips (20%) Type 5. The interobserver reliability for this classification has an intraclass coefficient of 0.88 [16]. The acetabular lesions were localized into the anterior, superolateral, and posterior quadrants (Fig. 1). For all damage types, 13.3% of hips had cartilage isolated to the anterior quadrant, 18.9% to the superolateral quadrant, and 6.7% to the posterior quadrant, with the remaining patients (61.1%) having damage in multiple quadrants (Types 1 and 2: Fig. 2; Types 3 and 4: Fig. 3).
Fig. 1.
The diagram used to document acetabular cartilage damage intraoperatively is shown with Beck grade distribution for each quadrant. Adapted from the surgical data collection forms of the Academic Network of Conservational Hip Outcomes Research (ANCHOR).
Fig. 2.
A graph shows the distribution of Type 1 and 2 acetabular cartilage damage. Ant = anterior; sup = superolateral; combos = combinations.
Fig. 3.
A graph shows the distribution of Type 3 and 4 acetabular cartilage damage. Ant = anterior; sup = superolateral; combos = combinations.
During the study period, there was an evolution of the surgical techniques used to treat the patients where hip arthroscopy is now being used in the majority of cases and open surgical dislocation reserved for mixed deformities and large cam lesions extending posterolaterally [5]. One hundred thirty-seven of the patients underwent hip arthroscopy and 43 surgical dislocation for management of their FAI deformity (Table 1). Of the 13 bilateral patients, six had both procedures performed concurrently whereas the remaining had a mean time of 13.1 months (range, 3.87–21.97 months) between the two surgeries. Ten bilateral patients underwent surgical dislocation on both hips, two underwent hip arthroscopy with chondro-osteoplasty on both hips, and one patient underwent one of each procedure on each hip. At the time of surgery, all patients who had a surgical dislocation cases had chondro-osteoplasty of the femoral head-neck junction whereas 111 of the 137 patients (81.0%) were treated via chondroplasty. Eighteen patients also had acetabular rim trimming with labral refixation, 15 by means of surgical dislocation and three by means of hip arthroscopy. Compared to patients who underwent hip arthroscopy, those who underwent surgical dislocation were younger (34.0 versus 39.7 years; p = 0.001), were predominantly male (p < 0.001), had a higher mean alpha angle (69.1° versus 64.4°; p = 0.03), and had a higher median Tönnis grade (p = 0.007) (Table 1). In the hip arthroscopy group, patients who did not have a chondro-osteoplasty were older (47.1 versus 38.0 years; p < 0.001) and had a lower alpha angle (59.2° versus 65.6°; p = 0.003) (Table 2). All patients followed routine postoperative treatment consisting of toe-touch weightbearing for 6 weeks (surgical dislocation) or 50% weightbearing for 4 weeks (hip arthroscopy).
Table 1.
Demographics and clinical data in all hips and those with surgical dislocations or hip arthroscopies
| Variable | All hips (n = 180) | Hips with surgical dislocations (n = 43) | Hips with hip arthroscopies (n = 137) | p value |
|---|---|---|---|---|
| Demographics | ||||
| Age at surgery (years)* | 38.4 (9.9) (17–59) | 34.0 (8.2) (18–49) | 39.7 (10.0) (17–59) | 0.001 |
| Sex (number of males, females) | 129, 38 | 39, 1 | 90, 37 | < 0.001 |
| BMI* | 26.9 (4.0) (18.7–39.0) | 27.1 (4.1) (18.7–37.9) | 26.9 (3.9) (19.4–39.0) | 0.78 |
| Clinical data | ||||
| Alpha angle (°)* | 65.5 (10.8) (29.9–90.0) | 69.1 (12.4) (43.5–90.0) | 64.4 (10.0) (29.9–90.0) | 0.01 |
| Center-edge angle (°)* | 33.3 (6.6) (21.0–52.5) | 34.0 (7.1) (23.0–50.0) | 33.1 (6.5) (21.0–52.5) | 0.48 |
| Beck type† | 4 (2–4) (1–5) | 4 (3–5) (1–5) | 4 (2–4) (1–5) | 0.22 |
| Tönnis grade† | 1 (0–1) (0–2) | 1 (1–1) (0–2) | 1 (0–1) (0–2) | 0.007 |
* Values are expressed as mean, with SD and range in parentheses; values are expressed as median, with quartile and range in parentheses.
Table 2.
Demographics and clinical data in hip arthroscopies with or without chondroplasty (n = 137)
| Variable | Hips with chondroplasty (n = 111) | Hips without chondroplasty (n = 26) | p value |
|---|---|---|---|
| Demographics | |||
| Age at surgery (years)* | 38.0 (9.6) (17–59) | 47.1 (8.3) (24–58) | 0.001 |
| Sex (number of males, females) | 73, 28 | 17, 9 | 0.32 |
| BMI* | 26.8 (4.0) (19.4–39.0) | 27.1 (3.9) (21.5–33.8) | 0.73 |
| Clinical data | |||
| Alpha angle (°)* | 65.6 (9.8) (29.9–90.0) | 59.2 (9.6) (40.0–77.4) | 0.003 |
| Center-edge angle (°)* | 32.8 (6.1) (21.0–51.0) | 34.5 (7.7) (22.7–52.5) | 0.23 |
| Beck type† | 4 (2–4) (1–5) | 4 (2–5) (1–5) | 0.40 |
| Tönnis grade† | 1 (0–1) (0–2) | 1 (0–1) (0–2) | 0.10 |
* Values are expressed as mean, with SD and range in parentheses; values are expressed as median, with quartile and range in parentheses.
To assess the potential influence of alpha angle and other clinical/radiographic measures (eg, age, BMI, sex, UCLA activity score [2], center-edge angle) on cartilage delamination (Type 3 or greater), we performed univariate logistic regression analyses for each independent predictor. A subsequent multivariate analysis containing all significant (α = 0.05) univariate predictors (age, sex, center-edge angle, alpha angle) was then performed. To further assess the potential impact of alpha angle on cartilage delamination, we performed stratified logistic regression analyses with the following alpha angle subgroups: (1) less than 50° (reference group), (2) 50.0° to 64.9°, and (3) 65° or greater. In all cases, odds ratios (ORs) and corresponding 95% CIs were generated. Correlation between clinical/radiographic factors and Beck classification was assessed using Pearson’s r. All statistical analyses were performed using PASW® Statistics 17.0 (SPSS Inc, Chicago, IL, USA).
Results
A greater alpha angle was independently associated with (p = 0.01) increased odds of having Type 3 or greater cartilage damage (OR, 1.04; 95% CI, 1.01–1.08 (Table 3). Further, when stratifying for risk of Type 3 or greater cartilage according to alpha angle (Table 4), a value of 65° or greater had the greatest OR (OR, 4.00; 95% CI, 1.26–12.71; p = 0.02) when compared to our reference group (alpha angle < 50°).
Table 3.
Results of univariate and multivariate regression analyses
| Analysis/variable | Odds of having Beck Type 3 or greater | ||
|---|---|---|---|
| Odds ratio | 95% CI | p value | |
| Univariate | |||
| Age | 1.04 | 1.01–1.07 | 0.03 |
| BMI | 0.96 | 0.88–1.05 | 0.34 |
| Male sex | 2.24 | 1.09–4.62 | 0.03 |
| UCLA activity score | 1.02 | 0.88–1.17 | 0.82 |
| Alpha angle | 1.05 | 1.02–1.09 | 0.002 |
| Center-edge angle | 0.94 | 0.89–0.99 | 0.01 |
| Multivariate | |||
| Age | 1.04 | 1.01–1.08 | 0.02 |
| Male sex | 2.00 | 0.92–4.31 | 0.08 |
| Alpha angle | 1.04 | 1.01–1.08 | 0.01 |
| Center-edge angle | 0.94 | 0.89–0.99 | 0.03 |
Table 4.
Results of univariate regression analysis with alpha angle stratified into groups
| Alpha angle group | Odds of having Beck Type 3 or greater | ||
|---|---|---|---|
| Odds ratio | 95% CI | p value | |
| < 50° | 1.00 (reference) | ||
| 50°–64.9° | 1.44 | 0.45–4.59 | 0.53 |
| ≥ 65° | 4.00 | 1.26–12.71 | 0.02 |
Older age was independently associated with (p = 0.02) increased odds of having Type 3 or greater cartilage damage (OR, 1.04; 95% CI, 1.01–1.08) whereas the center-edge angle demonstrated a protective effect (OR, 0.94; 95% CI, 0.89–0.99; p = 0.03). Age (r = 0.14, p = 0.01) and alpha angle (r = 0.20, p = 0.04) were both weakly correlated with the type of acetabular cartilage damage. A weak correlation (r = 0.22, p = 0.002) was observed between Tönnis grade and damage type. There was no correlation (p = 0.89) between presence of crossover sign and cartilage damage.
Discussion
The treatment of prearthritic hip pain in young patients has evolved and grown tremendously in the last decade due to better diagnostic tools such as MRA and less invasive surgical techniques (ie, hip arthroscopy) [18, 19]. As such, our understanding of factors leading to cartilage damage in the hip has evolved from a purely labral origin of the pathology to a complex interaction of bony abnormalities, patient activity, and vascularity of the labral-chondral complex [10]. Initial investigations by McCarthy et al. [20] focused on the watershed lesion where it was believed the poor vascularity and deficient structure of the anterior-medial labral-chondral junction represented an at-risk area, which once damaged led to progressive damage to the acetabular and femoral cartilage. More recently, FAI has been proposed as the main mechanism of acetabular labral-chondral damage in patients suffering from prearthritic hip pain [7]. Consequently, the treatment focus has shifted from purely dealing with intraarticular pathology to surgical correction of either asphericity of the femoral head-neck junction (cam lesion), acetabular overcoverage (pincer), or both [5]. Although the presence of the cam deformity is believed to be the leading cause of acetabular cartilage damage, understanding the risk factors for these lesions is critical to developing appropriate treatment strategies. Consequently, we (1) determined whether the severity of cam deformity as assessed by the alpha angle is predictive of acetabular cartilage delamination and (2) described the clinical (age, sex, BMI) and radiographic (Tönnis grade, acetabular coverage) characteristics of patients with cartilage delamination.
There are several limitations to our study. First, we used plain radiographs (crosstable or Dunn view) to quantify the alpha angle, which may have underestimated in some circumstances the severity of the deformity and missed the deformity due to the use of a two-dimensional measurement to assess a three-dimensional deformity [8]. This is well illustrated by the eight patients who had a normal alpha angle on plain radiographs but had a recognized cam deformity at the time of surgery. Although alpha angle measurements on plain radiographs have a diagnostic accuracy of 70% to 90% in diagnosing cam FAI [4], future work should focus on a more three-dimensional quantification of the deformity to better predict risk of cartilage damage. Second, cartilage damage evaluation was limited to a macroscopic evaluation using the classification of Beck et al. [9] where we focused on Type 3 and 4 damage, which has been most commonly noted in patients with cam-type FAI. Recent work has suggested microscopic evaluation using high-resolution quantification MRI techniques can detect early depletion of proteoglycan content in asymptomatic individuals with a cam deformity [24]. Consequently, we may have underestimated cartilage damage in some patients who did not demonstrate Type 3 or 4 damage. Finally, other factors may have played a role in the development of the cartilage lesions, such as pelvic mobility [17]. These may have accentuated or diminished the degree of impingement and individual biologic susceptibility to cartilage damage, as variations in subchondral bone density affecting cartilage nutrition may also have a strong influence on the development and/or severity of cartilage damage [10].
Our observations suggest cam deformity (as assessed by the alpha angle) predicted cartilage damage, with an alpha angle of 65° or greater having an OR of 4.00. Our findings are similar to those of two previously published retrospective studies. In a series of 102 hips, Johnston et al. [15] reported the alpha angle measured on crosstable lateral views was higher in patients with full-thickness delamination (60° versus 51°). Similarly, Nepple et al. [22] found an alpha angle of greater than 50° measured on frog leg lateral views had an OR of 2.8 to be associated with substantial acetabular cartilage delamination. Some of the discrepancies in the alpha angle values associated with cartilage damage among the three studies reflect the different types of lateral radiographs used to quantify the alpha angle (crosstable, Dunn, and frog leg lateral views). Because of the three-dimensional nature of the cam deformity, it is likely the maximum area of deformity may not be visualized on certain radiographic projections. The mounting evidence that a gradient of severity for the cam deformity exists is important in demonstrating the causality between cam FAI and hip arthritis. Using presence of hip pain as a function of alpha angle in patients with cam FAI, Allen et al. [1] showed an alpha angle of greater than 60° had an OR of 2.54 to be associated with hip pain in the contralateral hip. Although the cutoff value of the alpha angle between this study and that of Allen et al. [1] is different, this is not unexpected as hip pain is not necessarily associated with substantial acetabular cartilage damage, and one would expect the alpha angle associated with cartilage damage is greater than that associated with hip pain. The only other study looking at the risk of cartilage delamination was that of Anderson et al. [3] where they developed a femoral risk score with 1 point given for each of the following radiographic findings: pistol grip deformity, femoral bump, and femoral cyst. They found each additional point increased the risk of delamination; however, the reliability of this assessment was not provided.
When looking at the clinical and radiographic presentations, male sex, advanced age, and Tönnis grade were factors associated with Type 3 and higher cartilage damage. This again is consistent with previous studies and related to the higher prevalence and greater severity of the cam deformity in males [13]. Although the reasons for this are still being investigated, recent work by Siebenrock et al. [25] showed intense activity level in males predisposes to the development of the cam deformity. Having said that, when performing the multivariate analysis, male sex was no longer significant, again highlighting the importance of the size of the deformity. In contrast, advanced age remained significant in the multivariate analysis in regard to greater cartilage damage, which implies a temporal sequence in the degeneration of the hip, which was also observed in hip dysplasia [14] and has important clinical implications in the timing of surgical correction of the cam deformity since degree of cartilage damage has a considerable impact on clinical outcome [11]. In regard to radiographic findings, our study showed an increased center-edge angle was protective of cartilage damage with an OR of 0.94 (Fig. 4). Previously, Anderson et al. [3] found a similar trend, with a center-edge angle of more than 40° being protective. This suggests increased acetabular coverage is protective in the presence of cam FAI, and therefore performing an acetabular rim trimming to correct the overcoverage without correcting the cam deformity may actually be detrimental to the hip. More importantly, acetabular retroversion had no relationship to cartilage damage. This is consistent with the paper of Allen et al. [1], which could not find an association between pincer deformity and hip pain in patients with cam FAI. This also illustrates the complexity of this dynamic deformity where pelvic tilt during motion is difficult to predict, which may have a strong influence on the etiology of cartilage damage. More importantly, the treatment of mixed deformities in FAI remains controversial, with current data suggesting the cam deformity represents the driving force in the etiology of acetabular cartilage damage and excessive acetabular rim trimming potentially putting the hip at risk of hip instability.
Fig. 4A–B.
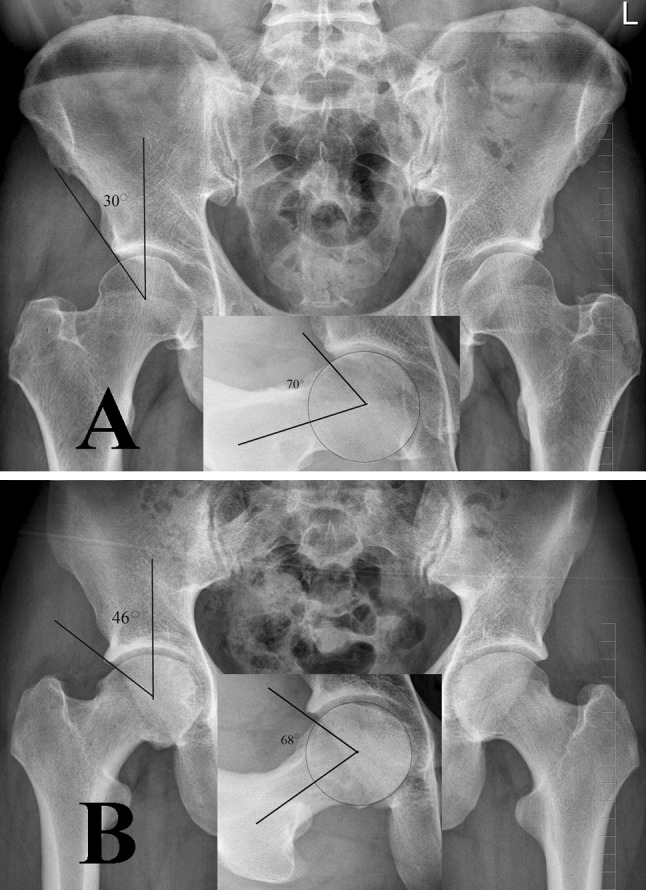
(A) An AP pelvis radiograph shows the hips of a 56-year-old man with Type 4 acetabular cartilage damage. The center-edge angle is 33°, and the alpha angle is 70° on the Dunn view (inset). (B) An AP pelvis radiograph shows the hips of a 25-year-old man with Type 1 acetabular cartilage damage. The center-edge angle is 41°, and the alpha angle is 66° on the Dunn view (inset).
In conclusion, patients with cam-type FAI and an alpha angle of 65° or more are at increased risk of substantial cartilage damage. With advancing age, the degree of cartilage damage also increases. Increased acetabular coverage (as measured by center-edge angle) appears protective of cartilage damage by limiting the outside-in damage of the cam deformity. This knowledge provides additional information in the development of guidelines for the treatment of FAI and evidence to support the hypothesis of cam FAI as a cause of osteoarthritis.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Allen DJ, Beaule PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91:589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip: a comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 3.Anderson LA, Peters CL, Park BB, Stoddard GJ, Erickson JA, Crim JR. Acetabular cartilage delamination in femoroacetabular impingement: risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am. 2009;91:305–313. doi: 10.2106/JBJS.G.01198. [DOI] [PubMed] [Google Scholar]
- 4.Barton C, Salineros MJ, Rakhra KS, Beaule PE. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469:464–469. doi: 10.1007/s11999-010-1624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beaule PE, Allen DJ, Clohisy JC, Schoenecker P, Leunig M. The young adult with hip impingement: deciding on the optimal intervention. J Bone Joint Surg Am. 2009;91:210–221. doi: 10.2106/JBJS.H.00802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beaule PE, LeDuff MJ, Zaragoza EJ. Quality of life outcome of femoral head/neck offset correction for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 7.Beaule PE, O’Neill M, Rakhra K. Acetabular labral tears. J Bone Joint Surg Am. 2009;91:701–710. doi: 10.2106/JBJS.H.00802. [DOI] [PubMed] [Google Scholar]
- 8.Beaule PE, Zaragoza EJ, Motamedic K, Copelan N, Dorey J. Three-dimensional computed tomography of the hip in the assessment of femoro-acetabular impingement. J Orthop Res. 2005;23:1286–1292. doi: 10.1016/j.orthres.2005.03.011.1100230608. [DOI] [PubMed] [Google Scholar]
- 9.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement. Part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. doi: 10.1097/00003086-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Brandt KD, Radin EL, Dieppe PA, Putte L. Yet more evidence that osteoarthritis is not a cartilage disease. Ann Rheum Dis. 2006;65:1261–1264. doi: 10.1136/ard.2006.058347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res. 2010;468:555–564. doi: 10.1007/s11999-009-1138-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hack K, Diprimio G, Rakhra K, Beaule PE. Prevalence of cam type femoroacetabular impingement in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436–2444. doi: 10.2106/JBJS.J.01280. [DOI] [PubMed] [Google Scholar]
- 14.Jessel RH, Zurakowski D, Zilkens C, Burstein D, Gray ML, Kim YJ. Radiographic and patient factors associated with pre-radiographic osteoarthritis in hip dysplasia. J Bone Joint Surg Am. 2009;91:1120–1129. doi: 10.2106/JBJS.G.00144. [DOI] [PubMed] [Google Scholar]
- 15.Johnston TL, Schenker ML, Briggs KK, Philippon MJ. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24:669–675. doi: 10.1016/j.arthro.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 16.Konan S, Rayan F, Meermans G, Witt J, Haddad FS. Validation of the classification system for acetabular chondral lesions identified at arthroscopy in patients with femoroacetabular impingement. J Bone Joint Surg Br. 2011;93:332–336. doi: 10.2106/JBJS.J.01587. [DOI] [PubMed] [Google Scholar]
- 17.Lamontagne M, Kennedy MJ, Beaule PE. The effect of cam FAI on hip and pelvic motion during maximum squat. Clin Orthop Relat Res. 2009;467:645–650. doi: 10.1007/s11999-008-0620-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616–622. doi: 10.1007/s11999-008-0646-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lubowitz JH, Poehling GG. Hip arthroscopy: an emerging gold standard. Arthroscopy. 2006;22:1257–1259. doi: 10.1016/j.arthro.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 20.McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The watershed labral lesion: its relationship to early arthritis of the hip. J Arthroplasty. 2001;16:81–87. doi: 10.1054/arth.2001.28370. [DOI] [PubMed] [Google Scholar]
- 21.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 22.Nepple JJ, Carlisle JC, Nunley RM, Clohisy JC. Clinical and radiographic predictors of intra-articular hip disease in arthroscopy. Am J Sports Med. 2011;39:296–303. doi: 10.1177/0363546510384787. [DOI] [PubMed] [Google Scholar]
- 23.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 24.Pollard TC, McNally EG, Wilson DC, Wilson DR, Madler B, Watson M, Gill HS, Carr AJ. Localized cartilage assessment with three-dimensional dGEMRIC in asymptomatic hips with normal morphology and cam deformity. J Bone Joint Surg Am. 2010;92:2557–2569. doi: 10.2106/JBJS.I.01200. [DOI] [PubMed] [Google Scholar]
- 25.Siebenrock KA, Ferner F, Noble PC, Santore RF, Werlen S, Mamisch TC. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res. 2011;469:3229–3240. doi: 10.1007/s11999-011-1945-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tannast M, Siebenrock KA, Anderson S. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 27.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 28.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(suppl 58):1–135. [Google Scholar]