Abstract
Background
High hip center reconstructions, used in revision and complex primary THAs, rely on pelvic bone stock at least 35 mm above the anatomic teardrop. However, the technique does not restore normal hip biomechanics and controversy exists regarding acetabular implant survival. Previous reports document a wide range of implant positioning above the teardrop. There is no anatomic guidance in the literature regarding the amount of bone stock available for initial implant stability in this area of the ilium.
Questions/purposes
We therefore determined the thickness of the human ilium and related it to acetabulum cup coverage in high hip center reconstructions.
Methods
We sectioned 16 cadaveric hips from the anterior superior iliac spine to the anatomic teardrop in 5-mm increments, then measured the thickness of the ilium for each cross section.
Results
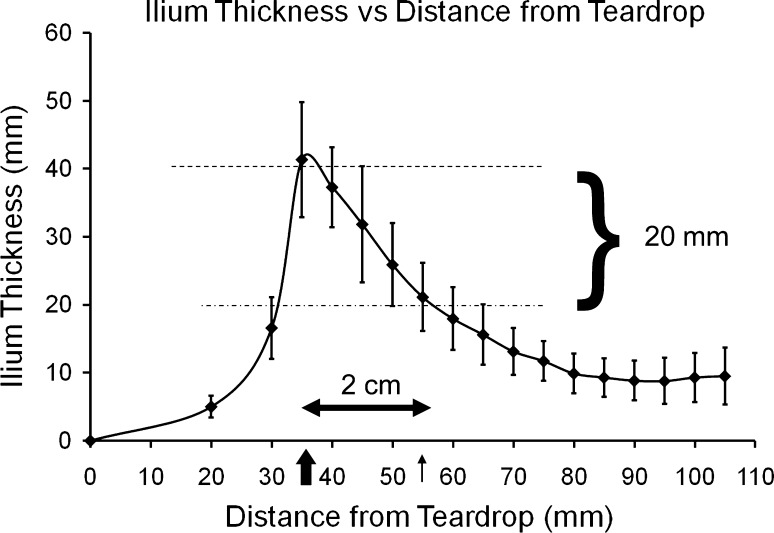
The maximum thickness of 42 ± 9 mm occurred at the dome of the acetabulum 35 ± 3 mm above the teardrop. At a distance of 1 cm above the dome, the ilium was reduced by 24%, to 32 ± 6 mm. At 2 cm above the dome, the ilium thickness was 22 ± 4 mm, a 48% reduction from its maximum.
Conclusion
There are substantial anatomic limitations to high hip reconstructions 2 cm above the acetabular dome.
Introduction
High hip center reconstructions place the hip center at least 35 mm above the anatomic teardrop. Complex primary and revision cases depend on adequate ilial bone above the dome for acetabular implant stability. The bony anatomy of the human pelvis has been well described in anatomic and surgical textbooks. Judet et al. discussed the columns of the acetabulum and operative techniques for fracture fixation [7]. They documented the anatomic features of complex acetabular fractures and the corresponding radiograph findings. They did not quantify any of their observations. Rubenstein et al. performed a descriptive anatomic study of a single human ilium [9]. They cross sectioned the ilium in 1-cm slices from the anterior superior iliac spine to the obturator foramen; correlating the anatomic landmarks to CT scan findings. No quantitative analysis was done. The only quantitative description of the human ilium, to our knowledge, was by Hauser et al. [5]. CT scans were used to measure periacetabular bone concentration and morphologic features. One hundred twenty-five healthy subjects were studied measuring acetabular depth, diameter, bone volume, and density. The acetabular diameter correlated with depth, bone density, and volume. Hauser et al. found no association between bone volume and sphericity but did find variability among subjects. However, the scans did not show the ilium above the acetabular dome as would be relevant for high hip reconstructions.
Doehring et al. reported biomechanical data unfavorable to high hip center placement [3, 4]. An experimental model calculated joint reaction forces of uncemented total hip implants at normal, 25 mm, and 37 mm above the hip center. Superior and lateral placement of the hip center resulted in an increase in the joint reaction forces, whereas superior placement alone did not [3]. Likewise, using the same biomechanical model, Doerhing et al. showed an increase in femoral component micromotion with superior and lateral component placement and normal head placement with leg lengthening [3].
Pagnano et al. showed unfavorable long-term clinical results regarding high center reconstructions in Crowe Type II hips [8]. One hundred seventeen cemented hips were analyzed and the acetabular position was used to correlate with survival. Cups positioned 15 mm above the center of the femoral head with and without lateral displacement had increased rates of loosening and revision. Yoder et al. had similar conclusions studying 116 cemented hips [11]. At 9 years, the risk of loosening was four times greater if the hip center was raised 30 mm above the teardrop. However, there are some long-term clinical data to support high hip center reconstructions [1, 2, 6, 10]. Russotti and Harris reported greater than 90% survival of cemented cups with hip centers 43 ± 7 mm above the teardrop at 10 years [10]. Likewise, using cementless cups, Dearborn and Harris reported a similar survival with hip centers 44.5 ± 9.5 above the teardrop [2]. These cohorts of patients were followed for a minimum of 10 years and later reported at 16.8 years. They emphasized the importance of medialization of the cup for better coverage and optimum hip biomechanics. They advocated high hip center positioning, using smaller cup sizes, if adequate initial stability could be achieved with screws; their mean cup diameter was 55 mm (range, 40–74 mm). Christodoulou et al. analyzed survival and polyethylene wear rates of 34 uncemented high hip reconstructions compared with 70 normal positioned cups at 8 years followup [1]. There was no difference in polyethylene wear or survival. There were four failures of the acetabulum in the high hip center group. The average hip center height was 40 mm above the teardrop (range, 31–60 mm); the heights of the failures were not reported.
Given the questions raised by the various studies above, we determined the thickness of the human ilium from the anatomic teardrop to the iliac crest, using a thin transverse section; and related this thickness to acetabular cup coverage using a mathematical model.
Materials and Methods
We obtained eight full pelvic specimens from three male and five female cadavers (16 hips) from the Anatomical Services Division at the University of Maryland School of Medicine. Only the cause of death and age were known for each. We debulked the pelvic specimens of soft tissue and placed them in a detergent solution for dissolution of the remaining soft tissues. AP radiographs of the pelvis were made of each specimen to rule out any anatomic abnormalities; no specimens were excluded on this basis. We obtained 16 separate ilium specimens by detachment from the sacrum in each pelvis.
After soft tissue debulking, we placed a Steinmann pin at the superior-most aspect of the cotyloid fossa (Fig. 1) and directed it between the inner and outer tables of the ilium, to a point on the iliac crest 1/3 of the distance from the anterior superior iliac spine to the posterior superior iliac spine. This point on the iliac crest was constant in each specimen; it represented the cephalad extent of the thickened ilium supporting the acetabulum, and allowed for standardization of anatomic measurements. We then removed the Steinmann pin and passed a thin, methylene blue-dyed, wooden stick through the pinhole, marking a track in the ilium for its entire vertical length (Fig. 2). The ilium then was sectioned with a band saw in 5-mm increments perpendicular to the path of the pin tract; the sectioning started proximally, 1 cm below the anterior superior iliac spine, and proceeded distally toward the teardrop with subsequent sections parallel to the first. The anatomic teardrop was the floor of the acetabulum, just above the obturator foramen. We measured the thickness of the ilium in millimeters at the level of the methylene blue mark in the medial to lateral direction (Fig. 3). The most distal section of each specimen was made at the midpoint of the quadrilateral plate.
Fig. 1.
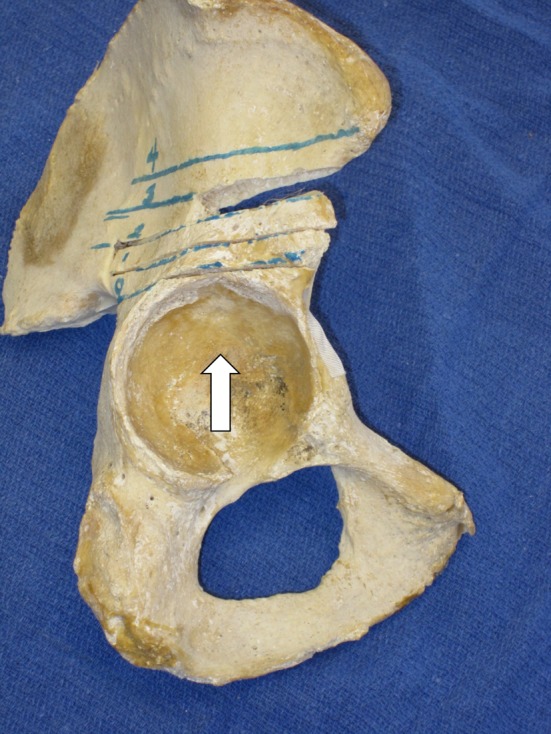
A pan ilium model is shown in this photograph. The lines represent levels where cross sections were taken in each specimen. The arrow is the entry site of the Steinmann pin at the cotyloid fossa.
Fig. 2A–B.
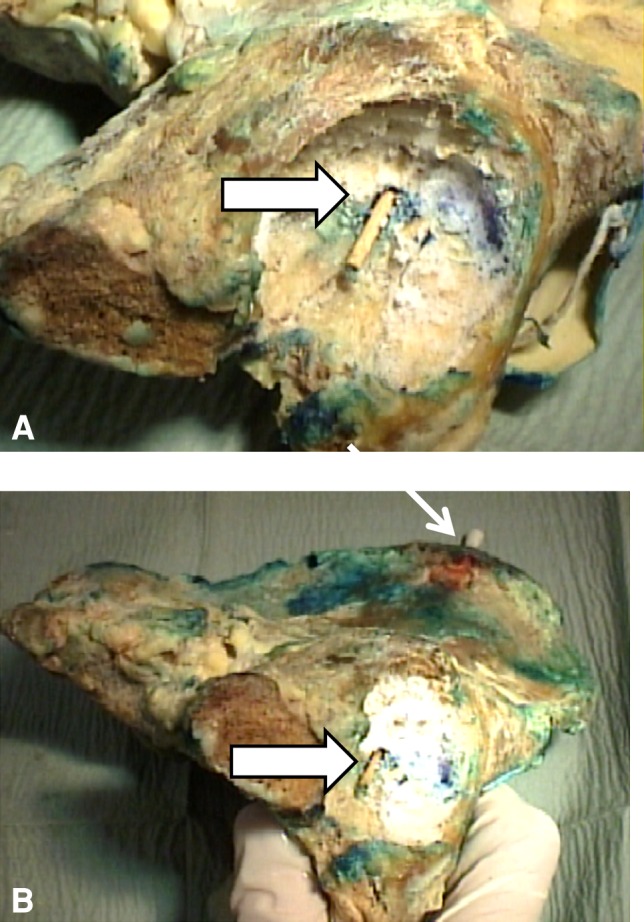
(A) A Q-tip, dyed in methylene blue (arrow) was inserted through the cotyloid fossa into the Steinmann pin tract. (B) The Q-tip (arrow) was started in the acetabulum and directed proximally between the inner and outer tables.
Fig. 3.

Cross-sections of the ilium oriented from cephalad to caudad are shown. The numbers correspond to distance above the teardrop in millimeters. The pin tract is marked by the blue dot (arrows). Greater than 55 mm above the teardrop, the ilium is thicker posterior to the pin tract (“x”).
To ascertain acetabular cup coverage at different levels above the teardrop, we developed a mathematical calculation to estimate the bony coverage of 40-mm, 50-mm, and 60-mm acetabular shells: linear acetabular cup coverage = (ilium thickness at any level above the teardrop/pie × diameter of acetabular shell/2) × 100. We calculated this at 1 cm and 2 cm above the acetabular dome. This number gives an approximate mathematical estimate of acetabular cup coverage above the teardrop using our ilium thickness cross-sectional measurements.
We computed averages and standard deviations of all measurements.
Results
The inner to outer table thickness of the ilium attained its maximum of 42 mm (± 9 mm) at a point 35 mm (± 3 mm) above the anatomic teardrop, corresponding to the acetabular dome (Fig. 4). At 1 cm above the acetabular dome, the thickness of the ilium was 32 mm (± 6 mm) (a 25% reduction), whereas at 2 cm above the dome, the thickness decreased to 22 mm (± 4 mm) (a 48% reduction). At 2 cm or greater above the acetabular dome, only posterior displacement of the acetabulum toward the sacroiliac joint provided any increase in transcortical thickness of the ilium (Fig. 3).
Fig. 4.
The average ilium thickness versus the distance from the teardrop is shown with standard deviations. The maximum thickness was 42 ± 9 mm at 35 mm above the teardrop, which decreased by 50% at 54 mm above the teardrop.
The mathematical linear acetabular cup coverage for 40-, 50-, and 60-mm hemispheric shells, were 67%, 54%, and 45% at the acetabular dome, 51%, 41%, and 33% 1 cm above the dome, and 35%, 28%, and 23% 2 cm above the dome, respectively.
Discussion
High hip center reconstructions have been advocated as a compromise in treating complex acetabular revisions and congenital hip dislocations. It is difficult from the literature to discern if there is a threshold for the amount of distance from the teardrop. Reconstructions within 2 cm of the dome have a good chance of survival, in terms of cup coverage, however any higher leaves little anatomic room for coverage. None of the studies, to our knowledge, recorded the height of each failure. We believe this is why there is discrepancy in the literature. The bony anatomy of the human ilium has been well described from a qualitative perspective, however there are little quantitative data [5, 7, 9]. High hip center reconstructions use this anatomy for initial stability and long-term survival. There are biomechanical and clinical data against these reconstructions [3, 4, 8, 11]. However, there are intermediate and long-term clinical studies to support this technique [1, 2, 6, 10]. Concerns regarding implant stability and durability, given the small amount of ilial bone, are the main reasons against this technique. We therefore quantified the thickness of the human ilium from the anatomic teardrop to the iliac crest using thin transverse sections, and relate it to acetabular cup coverage using a mathematical model.
Readers should be aware of limitations of our study. First, there was specimen size variability that we could not control; specifically, the height and weight of each specimen were unknown. Despite this our standard deviations were relatively small and the relative behavior of the ilium was fairly consistent. Second, it was at times technically difficult to reproduce precise bone cuts at each level in each specimen, however this could account for only minimal variability in observed measurements. Future anatomic studies combining CT scans with gross anatomic specimens would optimize data point accuracy. Nevertheless, we found a consistent relationship between ilium thickness and distance from the teardrop that was useful in predicting acetabular implant coverage, and therefore initial stability, in nonanatomic acetabular component placement in complex revisions. Third, the mathematical calculation of cup coverage is a linear estimation of acetabular perimeter coverage in two dimensions; three-dimensional thickness of the ilium contributed to stability of the hemispheric component, but our data were able to address only linear thickness of the iliac wing. Despite systematic limitation, linear cup coverage substantially decreased relative to the same calculation performed at the anatomic location of the normal acetabular dome. Future studies with CT and MRI would provide three-dimensional coverage of the cup. These data could add to computer navigation technology by adding acetabular coverage in addition to cup orientation and leg length.
Regardless of the beneficial biomechanical effects of hip center medialization, our data do not support the empiric recommendation that in acetabular reconstructions using high hip centers, the cup should be moved as medial as possible to improve acetabular component coverage [2, 6, 10]. The ilium thickness reached its peak 35 mm above the teardrop, approximately at the acetabular dome, and quickly decreased to approximately ½ its thickness in 2 cm as the anatomy progressed proximally. At that height above the dome, a 50-mm cup would have only 28% coverage by our mathematical calculation. Greater than 2 cm from the acetabular dome, only posterior displacement toward the sacroiliac joint provided a modest increase in transcortical iliac thickness. According to our data, a 50-mm cup had only 28% linear perimeter coverage at 2 cm above its normal position compared with 53% linear coverage in an anatomic location. Therefore, strategic screw positioning to achieve secure adjunct fixation would seem to be necessary to obtain initial cup stability in such a proximal location.
Our observations provided no anatomic basis to believe that increased medialization of the cup resulted in improved bony coverage in cephalad locations. Only posterior movement of the elevated acetabulum toward the sacroiliac joint offered any increase in thickness of the ilium, but such displacement of the hip center would likely have resulted in other problems related to component impingement and did not seem advisable. However, we do concur that medialization of the acetabular component to the extent possible remains a prudent theoretical strategy to reduce overall joint reaction forces.
We described the human ilium in a clinically relevant context referencing the anatomically constant acetabular teardrop. A predictable and rapid decrease in thickness of the ilium occurred with proximal migration above the normal anatomic location of the acetabulum. Within 2 cm of the intact acetabular dome, the width of the ilium decreased to approximately 50% of its maximum thickness. The resulting bicortical iliac thickness of approximately 21 mm covered only approximately 25% of the linear perimeter of a 50- to 60-mm acetabular component, as typically used in revision arthroplasty. With a complex acetabular reconstruction, a working knowledge of available iliac bone stock is important in establishing initial implant coverage and stability. There are substantial anatomic limitations to high hip center acetabular reconstructions, particularly 2 cm above the dome.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Christodoulou NA, Dialetis KP, Christodoulou AN. High hip center technique using a biconical threaded Zweymuller cup in osteoarthritis secondary to congenital hip disease. Clin Orthop Relat Res. 2010;468:1912–1919. doi: 10.1007/s11999-009-1203-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dearborn J, Harris W. High placement of an acetabular component inserted without cement in a revision total hip arthroplasty: results after a mean of ten years. J Bone Joint Surg Am. 1999;81:469–480. doi: 10.2106/00004623-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Doehring TC, Rubash HE, Dore DE. Micomotion measurements with hip center and modular neck length alterations. Clin Orthop Relat Res. 1999;362:230–239. doi: 10.1097/00003086-199905000-00032. [DOI] [PubMed] [Google Scholar]
- 4.Doehring TC, Rubash HE, Shelly FJ, Schwendeman LJ, Donaldson TK, Navalgund YA. Effect of superior and superolateral relocations of the hip center on hip joint forces: an experimental and analytical analysis. J Arthroplasty. 1996;11:693–703. doi: 10.1016/S0883-5403(96)80008-8. [DOI] [PubMed] [Google Scholar]
- 5.Hauser DL, Fox JC, Sukin D, Mudge B, Coutts RD. Anatomic variation of structural properties of periacetabular bone as a function of age: a quantitative computed tomographs study. J Arthroplasty. 1997;12:804–811. doi: 10.1016/S0883-5403(97)90012-7. [DOI] [PubMed] [Google Scholar]
- 6.Hendricks KJ, Harris WH. High placement of noncemented acetabular components in revision total hip arthroplasty a concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg Am. 2006;88:2231–2236. doi: 10.2106/JBJS.E.00247. [DOI] [PubMed] [Google Scholar]
- 7.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46:1615–1646. [PubMed] [Google Scholar]
- 8.Pagnano W, Hanssen AD, Lewallen DG, Shaughnessy WJ. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am. 1996;78:1004–1014. doi: 10.2106/00004623-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Rubenstein J, Kellam J, McGonigal D. Cross-sectional anatomy of the adult bony acetabulum. J Can Assoc Radiol. 1982;33:137–138. [PubMed] [Google Scholar]
- 10.Russotti GM, Harris WH. Proximal placement of the acetabular component in total hip arthroplasty. J Bone Joint Surg Am. 1991;73:587–592. [PubMed] [Google Scholar]
- 11.Yoder SAA, Brand RA, Pederson DR, Gorman TW. Total hip acetabular component position affects component loosening rates. Clin Orthop Relat Res. 1988;228:79–87. [PubMed] [Google Scholar]