Abstract
Background
The acetabular cup should be properly oriented to prevent dislocation and to reduce wear. However, achieving proper cup placement is challenging with potentially large variations of cup position. We propose a new technique to position the acetabular cup.
Questions/Purposes
We used this technique, then determined actual cup position and subsequent dislocation rate.
Methods
We measured acetabular abduction (α°) and anteversion (β°) on preoperative CT scans in 46 patients (50 hips) scheduled for THA. During the operation, we identified the transverse acetabular notch (TAN) and anterior acetabular notch (AAN), a notch at the anterior acetabular margin. We then marked two reference points for 40° abduction at the acetabular rim: the superior point, which is opposite the TAN, and the inferior point at |α − 40| mm inside (when α was > 40°) or outside the TAN (when α was < 40°). We also marked two reference points for 15° anteversion: the posterior point opposite the AAN and the anterior point at |β − 15| mm inside (when β was < 15°) or outside the AAN (when β was > 15°). During cup insertion, we aligned cup abduction to the line between the superior and inferior points and cup anteversion to the line between the anterior and posterior points. We measured cup abduction and anteversion and evaluated the dislocation rate. One patient was lost to followup before 60 months; the minimum followup for the other 45 patients was 60 months (mean, 62.8 months; range, 60–65 months).
Results
The mean cup abduction was 40° (range, 32°–47°) and the mean cup anteversion was 17° (range, 8°–25°). No dislocation occurred postoperatively in 49 hips (45 patients) for a minimum of 5 years followup.
Conclusions
We obtained adequate cup position with our method and none of 45 patients (49 hips) had dislocation.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of level of evidence.
Introduction
Dislocation is the most common early complication after THA with a reported incidence ranging from 1% to 10% [3, 6, 7, 11, 29, 31–33, 38]. Among numerous influencing factors for dislocation, component malposition is an important factor under control of the surgeon [3, 6, 29, 31, 33].
Archbold et al. [1] used the transverse acetabular ligament as a landmark for acetabular cup positioning. However, another study criticized the method because the ligament was identified in only 47% during the operation and the cup position was not improved using the ligament for reference [10]. Mechanical guides and computer-assisted navigation systems have been designed to provide proper cup positioning [5, 34]. The use of mechanical guides still results in large variations of cup abduction and anteversion [5, 16, 24]. Clinical use of the hip navigation system is ongoing [4, 17, 28]. We therefore developed a simple, practical, and anatomically based alignment method to position the acetabular cup.
The purposes of this study were (1) to determine the accuracy of our method in cup abduction and anteversion; and (2) to evaluate the dislocation rate of THA after use of our method.
Patients and Methods
We enrolled the study subjects from 48 patients who underwent 52 THAs between January 2006 and April 2006. We excluded two patients with fused hips because the acetabular margin could not be defined on CT scans and our method could not be used. The remaining 46 patients (50 hips) were included in the study. The mean age of the 23 men and 23 women was 53.6 years (range, 19–78 years). The indication for THA was femoral head osteonecrosis in 28 hips: 16 had Stage III osteonecrosis and 12 had Stage IV osteonecrosis according to the Ficat classification [12]. Sixteen had osteoarthritis secondary to hip dysplasia, three had osteoarthritis secondary to septic arthritis, and three had rheumatoid arthritis. The mean preoperative Harris hip score (HHS) [14] was 51 points (range, 24–78 points). All 46 patients (50 hips) had postoperative 6-week and 3-month radiographs taken. One patient (one hip) was lost to followup before a minimum of 5 years. In the remaining 45 patients (49 hips), the minimum followup was 60 months (mean, 62.8 months; range, 60–65 months). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
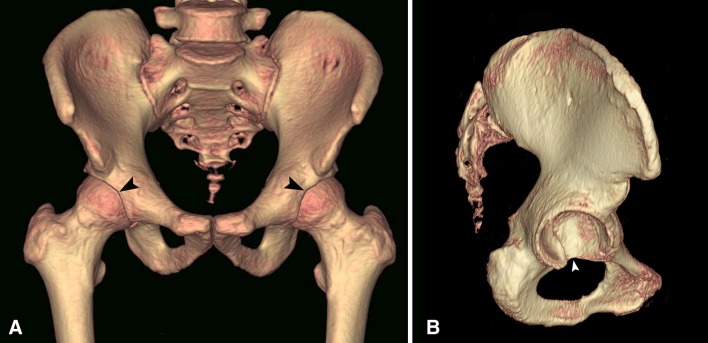
In the normal pelvis, there are two notches at the rim of the acetabulum. One is the transverse acetabular notch (TAN) at the lower margin and the other is at the anterior margin, which we named the anterior acetabular notch (AAN) (Fig. 1). To depict the relationships of the TAN to the acetabular inferior pole and the AAN to the acetabular anterior pole, we studied three-dimensional (3-D) CT images of the pelvis of 47 patients who underwent CT scanning between January 2005 and December 2005, 41 patients for preoperative evaluation of femoral head osteonecrosis and six patients for pelvic trauma. The scans were obtained with a 16-slice multidetector CT (Mx8000 IDT; Philips, Eindhoven, The Netherlands) using the standard acquisition of 16 × 1.5-mm beam collimation, 350-mm field of view, and reconstruction with 2.0-mm slice thickness and 1.0-mm increment. In the reconstructed 3-D images, the femur was deleted so as to expose the acetabulum and the pelvis was rotated to obtain an en facet view of the acetabulum.
Fig. 1A–B.
The (A) AAN is at the middle of the anterior rim (arrowhead) and the (B) TAN is at the lower margin of the cotyloid fossa (arrowhead).
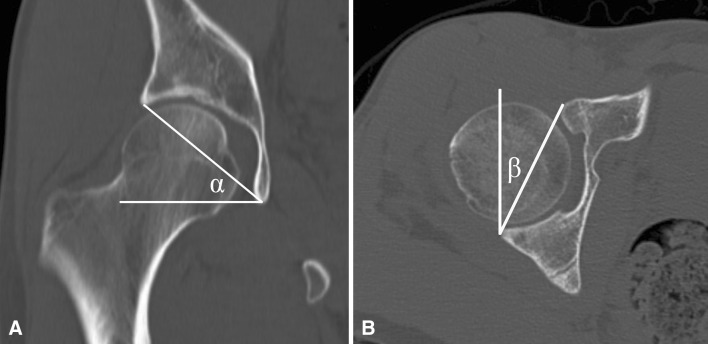
Two of us (YCH, JJY) measured the distance between the inferior pole of the acetabulum and the TAN and the distance between the anterior pole and the AAN. Two lines were drawn passing the center of the acetabulum, a parallel line and a perpendicular line with respect to the anterior pelvic plane. The crossing point of the parallel line and the lower margin of acetabulum was defined as the inferior pole and that of the vertical line and the anterior acetabular margin was the anterior pole. The distance between the inferior pole and the TAN ranged from 0 to 5 mm (mean, 1.7 mm) and that between the anterior pole and the AAN ranged from 0 to 3 mm (mean, 1.4 mm) (Fig. 2). Thus, we presumed the TAN, a proxy of the inferior pole, could be used as an intraoperatively identifiable landmark to align cup abduction and the AAN, a proxy of the anterior pole, as a landmark to align cup anteversion. To locate the TAN and AAN on the radiograph, we performed a study using a plastic pelvic model (Sawbones, Vashon, WA, USA). The TAN appeared at the lowest point of the teardrop and the AAN appeared at the middle of the anterior acetabular margin on the AP radiograph of the hip. Thus, we assumed the TAN appears as the teardrop in the midcoronal image of the reconstructed CT scan and the AAN at the anterior point in the midaxial image. Two of us (YKL, JYK) measured acetabular abduction and anteversion on preoperative CT scans, which were performed with the same scanner and the same acquisition protocol as described in the baseline study. Acetabular abduction was obtained on the midcoronal image by measuring the angle between a line drawn from the acetabular teardrop to the lateral acetabular margin and the interteardrop line (Fig. 3A) [36]. The acetabular anteversion was obtained on the midaxial image by measuring the angle between a line drawn from the anterior acetabular margin to the posterior acetabular margin and a line perpendicular to the line connecting the centers of both femoral heads (Fig. 3B) [36]. In osteoarthritic hips, osteophytes are present at the anterior rim of the acetabulum, which obscure the AAN, and the cotyloid fossa frequently is covered by a bony spur, a so-called central osteophyte [25], which obscures the TAN. We measured acetabular anteversion at the margin of the native acetabulum excluding the anterior osteophyte and acetabular abduction at the teardrop excluding the central osteophyte.
Fig. 2.
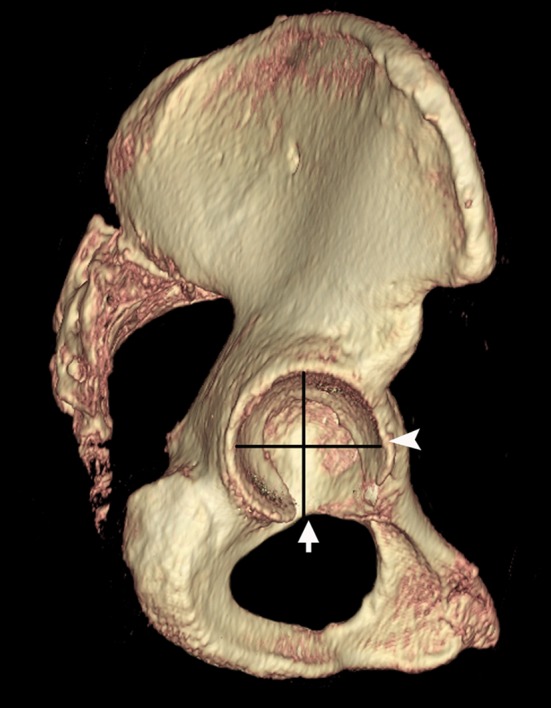
The AAN (arrowhead) is at the vicinity of the anterior pole of the acetabulum and the TAN (arrow) is at the vicinity of the inferior pole.
Fig. 3A–B.
Acetabular abduction (α) is measured on (A) a midcoronal CT image and acetabular anteversion (β) is measured on (B) a midaxial CT image.
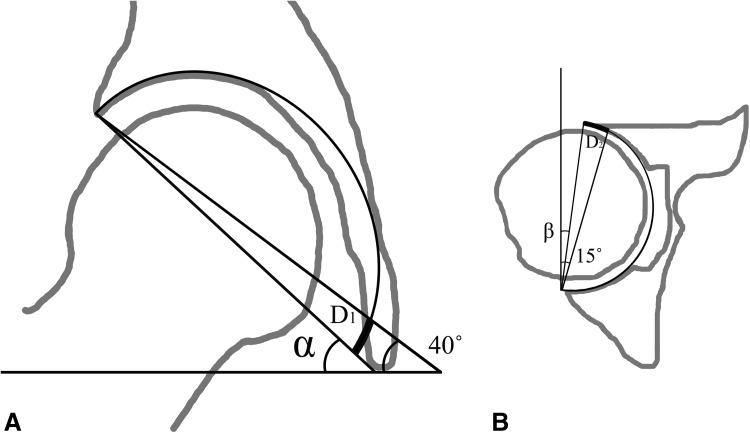
We set the goal of cup position at 40° abduction and 15° anteversion as suggested by Lewinnek et al. [23]. We used acetabular abduction as a reference to adjust cup abduction and acetabular anteversion as a reference to adjust cup anteversion. We determined four points to align cup position at the acetabular rim: the superior and inferior points of 40° abduction and the anterior and posterior points of 15° anteversion. The superior point was the opposite point of the TAN and posterior point was the opposite point of the AAN.
Murtha et al. [26] reported that the mean diameter of the normal acetabulum is 52 mm (range, 43.4–57.4 mm). A circumferential length of an arc (α) in a circle of a radius (R) can be calculated by the formula; 2 × π × R (α° ÷ 360°). When acetabular abduction is α°, the distance between the inferior point of 40° abduction and the TAN can be calculated by the formula:|2 × π × 52 mm (α° − 40°) ÷ 360°| = 0.91 × |α − 40| mm ≒ |α − 40| mm (Fig. 4A). Likewise, when acetabular anteversion is β°, the distance between the anterior point of 15° anteversion and the AAN is |β − 15| mm (Fig. 4B). When acetabular abduction was greater than 40°, the inferior point was inside the TAN and when less than 40°, it was outside the TAN. Likewise, when acetabular anteversion was greater than 15°, the anterior point was outside the AAN and when less than 15°, it was inside the AAN (Fig. 5). The size of cups used in our patients ranged from 46 to 54 mm. In this range, the difference of the distance (0.03–0.11 mm per 1°) according to the cup size in our calculation was negligible.
Fig. 4A–B.
(A) When acetabular abduction is α°, the distance between the inferior point of 40° abduction and the TAN (D1) is |2 × π × 52 mm × (α° − 40°) ÷ 360°| = |0.91 × (α − 40)| mm ≒ |α − 40| mm. (B) Likewise, when acetabular anteversion is β°, the distance between the anterior point of 15° anteversion and the AAN (D2) is |β − 15| mm.
Fig. 5.

When the acetabular abduction is 40° and anteversion is 15°, the cup is aligned to the native acetabular abduction and anteversion. The cup abduction is aligned to the superior point (black arrow) and the TAN (white arrow) and cup anteversion are aligned to the posterior point (black arrowhead) and the AAN (white arrowhead). When acetabular abduction is greater than 40°, the cup inferior point is inside the TAN and when less than 40°, it is outside the TAN. Likewise, when acetabular anteversion is greater than 15°, the cup anterior point is outside the AAN and when less than 15°, it is inside the AAN.
The mean acetabular abduction was 41.6° (SD, 3.8°; range, 32.7°–49.1°) and the mean acetabular anteversion was 16.0° (SD, 4.4°; range, 7.5°–26.5°). The distance between the TAN and the inferior point of 40° abduction ranged from 9.1 mm inside the TAN to 7.3 mm outside the TAN (mean, 1.6 mm inside the TAN). The distance between the AAN and the anterior point of 15° anteversion ranged from 7.5 mm inside the AAN to 11.5 mm outside the AAN (mean, 1.0 mm outside the AAN).
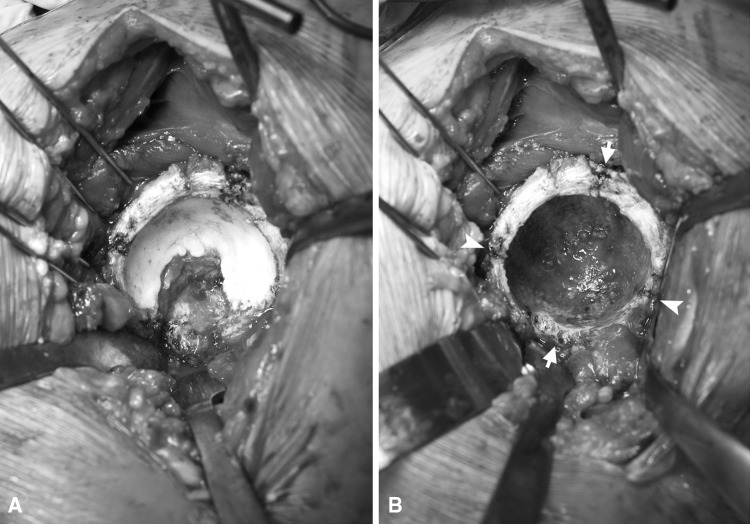
One surgeon (KHK) performed all operations using a posterolateral approach. To obtain complete exposure of the acetabular rim, we incised the superior and inferior portions of the capsule vertically and retracted the capsule flaps. We removed the labrum, transverse acetabular ligament, ligamentum teres, and pulvinar. During the operation, we removed the anterior osteophyte and central osteophyte with a gauge or osteotome (Fig. 6A). Reaming was started with the smallest size (40 mm) reamer, which was directed medially down to the cotyloid fossa. Subsequent reamers with 2-mm increments were directed in the same plane as the opening face of the acetabulum. After removal of cartilage, we identified the TAN and AAN and marked four points to obtain 40° cup abduction and 15° anteversion as described previously (Fig. 6B). A cementless acetabular cup (PLASMACUP® SC; Aesculap AG & Co, Tuttlingen, Germany), 28 mm-alumina liner (BIOLOX® forte; CeramTec AG, Plochingen, Germany), cementless stem (Bicontact®; Aesculap AG & Co), and 28-mm alumina femoral head (BIOLOX® forte; CeramTec AG) were used in all hips. The cup abduction was adjusted to the line between the superior and inferior points and the cup anteversion to the line between the anterior and posterior points. The cups were inserted by repeated tapping until obtaining a secure press-fit. During insertion, we repeatedly assessed and adjusted the cup alignment. After implantation, the hip capsule and short external rotators were repaired to restore soft tissue tension [37].
Fig. 6A–B.
(A) The acetabular labrum and transverse acetabular ligament are removed to obtain complete exposure of the acetabulum. (B) After reaming, the TAN (lower arrow) and AAN (right arrowhead) are identified. Then, four landmarks for cup alignment—the superior (upper arrow), inferior (lower arrow), anterior (right arrowhead), and posterior (left arrowhead) points are marked.
Postoperatively, patients were instructed to walk with the aid of two crutches for 4 weeks.
Clinical and radiologic followups were performed at 6 weeks; at 3, 6, 9, and 12 months; and every 6 months thereafter. We recorded instances of dislocation and the HHS [14]. To decrease the rate of lost or missed followups, we sent a text message to patients 1 week before the scheduled visits and patients who had not returned for the visits were contacted by telephone. Portions of the followups were performed by two nurses and local orthopaedic surgeons. In these instances, the followup form and radiographs were forwarded to our department.
We used postoperative 3-month radiographs to measure cup abduction and anteversion. Cup abduction was measured on the AP radiograph using the method of Engh et al. [8]. Various radiologic methods of measuring cup anteversion have been described. We used the method described by Woo and Morrey [40], which is reportedly easy, reliable, and valid [27], on the cross-table lateral radiograph. Scatterplots of the cup abduction and anteversion angles were made. The safe zone of the cup position was defined as 30° to 50° abduction and 5° to 25° anteversion as suggested by Lewinnek et al. [23].
Two of us (YKL, JYK) assessed fixation of the acetabular cup on the AP and cross-table lateral radiographs using the method of Latimer and Lachiewicz [21] and fixation of the femoral component using the methods of Engh et al. [9] and Kim and Kim [20]. The cup was considered loose when there was migration greater than 2 mm or a change of abduction greater than 4°. The stem was considered definitely loose when there was subsidence greater than 3 mm and possibly loose when there was a complete radiolucent line along the entire porous-coated surface on the AP and lateral radiographs. Postoperative 6-week radiographs were used as the baseline study and the final radiographic analysis was performed at the last followup. We assessed interobserver variability for acetabular abduction and anteversion using interclass correlation coefficients (ICCs). The mean cup abduction was 39.5° (SD, 2.50°; range, 31.6°–47.4°) and mean cup anteversion was 16.6° (SD, 4.19°; range, 7.7°–24.7°). ICCs for the acetabular abduction and anteversion were 0.853 and 0.832, respectively.
The design and protocol of this prospective study were approved by the institutional review board in our hospital, and all patients were informed that his or her medical data could be used in a scientific study and each provided consent preoperatively.
Results
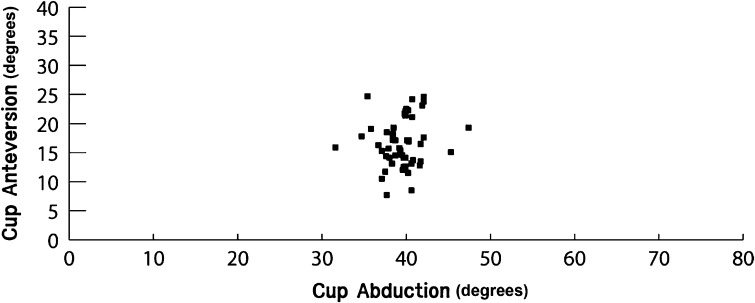
The mean cup abduction was 40° (range, 32°–47°) and the mean cup anteversion was 17° (range, 8°–25°).The mean error of cup abduction compared with the target abduction of 40° was 1.76° (SD, 1.84°; range, 0.0°–8.4°) and the mean error of cup anteversion compared with the target anteversion of 15° was 3.47° (SD, 2.83°; range, 0.1°–8.8°) (Fig. 7) (Table 1). In the scatterplot, cup abduction and anteversion of all 50 hips were within the safe zone (Fig. 8).
Fig. 7A–E.
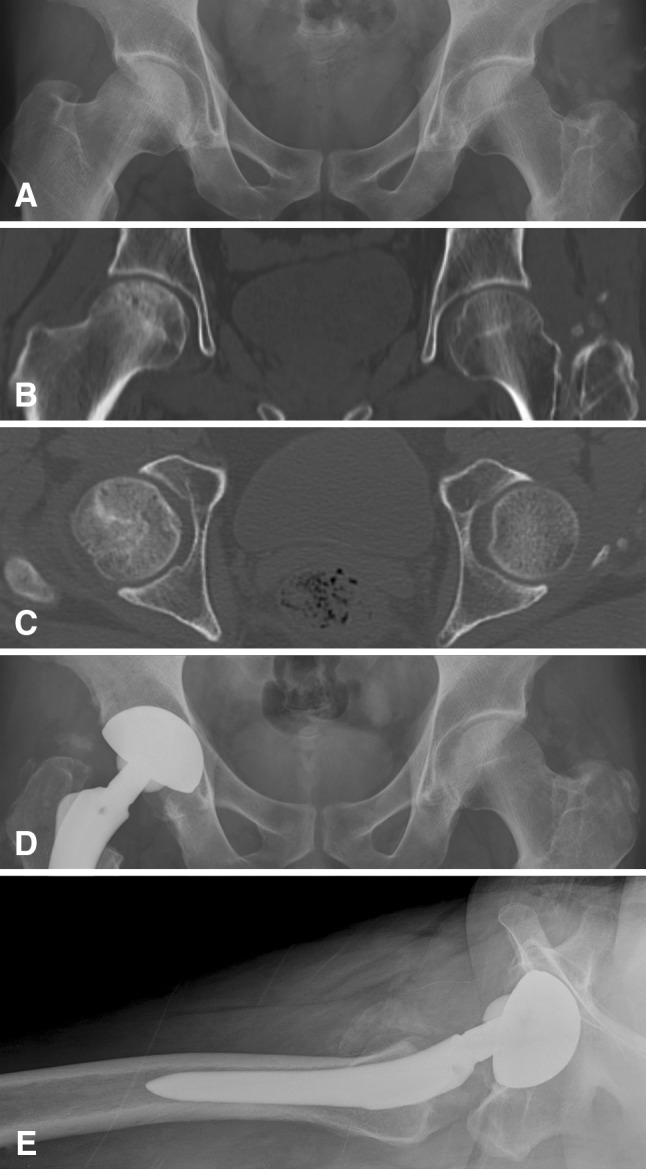
A 36-year-old man had osteonecrosis in the right femoral head as seen on his (A) preoperative AP radiograph. (B) The acetabular abduction is 44.6° as measured on the preoperative midcoronal CT scan. (C) On the preoperative midaxial CT scan, the acetabular anteversion is 13.7°. (D) The 6-week postoperative AP radiograph shows the cup abduction is 37.1°. (E) On the lateral radiograph, the cup anteversion is 14.4°.
Table 1.
Studies of acetabular cup position after THA
| Study | Study type | Number of hips | Cup abduction (°) | Cup anteversion (°) | Outliers (%) | Dislocation rate | Followup |
|---|---|---|---|---|---|---|---|
| Digioia et al. [5] | Navigation | 74 | 44 | 18 | 78 | NR | NR |
| Haaker et al. [13] | Comparison of manual and navigation | 69 (manual) | 45.7 (manual) | 28.5 (manual) | 28 | NR | NR |
| 98 (navigation) | 43 (navigation) | 22.2 (navigation) | 7 | ||||
| Parratte and Argenson [30] | Comparison of manual and navigation | 30 (manual) | 34 (manual) | 16.2 (manual) | 57 | NR | NR |
| 30 (navigation) | 34 (navigation) | 14.4 (navigation) | 20 | ||||
| Current study | Anatomic study | 50 | 39.5 | 16.6 | 0 | 0 | 5 years |
NR = not reported.
Fig. 8.
The cup abduction and anteversion are within the safe zone of 35° to 45° abduction and 10° to 20° anteversion in all 50 THAs.
During the followup, no hip dislocated and no hip showed radiographic signs of component loosening. The mean HHS was 94 points (range, 86–100 points) at the latest followup.
Discussion
Proper positioning of the acetabular cup has been a challenging issue of THA [3, 6, 29, 31, 33]. Many efforts have been made to provide surgeons with more accurate knowledge of cup alignment during THA. Mechanical intraoperative guides have been used to align the cup with respect to the longitudinal and coronal planes of the patient. However, these devices do not consider individual variations in a patient’s anatomy or the change of pelvic orientation during the operation. High percentages of inadequate cup orientations outside the desired alignment have been reported after the use of mechanical guides [4, 31, 32]. Digioia et al. [5] showed a mechanical guide was inadequate in achieving the desired anteversion angle and, to a lesser extent, the abduction angle; among 74 impacted press-fit cups using the guide, 78% had an unacceptable acetabular alignment. The first hip navigation system was developed in 1992. The system requires a preoperative CT scan and registration of anatomic landmarks so the computer can determine where the pelvis lies in space [19]. There has been criticism of the navigation systems including the extra costs, additional radiation exposure, time-consuming preoperative planning, and intraoperative matching procedures [34]. Jolles et al. [17], using computer-assisted cup placement techniques, reported 20% of the press-fit cups were outside the desired cup alignment. We therefore developed a simple, practical, and anatomically based alignment method to position the acetabular cup. The purposes of this study were (1) to determine the accuracy of our method in cup abduction and anteversion; and (2) to evaluate the dislocation rate of THA after use of our method.
We acknowledge limitations of our study. First, our method necessitates preoperative CT scanning to measure acetabular abduction and anteversion; these scans are costly and associated with a risk of radiation exposure. Usually preoperative plans for THA are made using AP radiographs. Acetabular abduction can be measured using AP radiographs of the hip by obtaining the angle between a line drawn from the acetabular teardrop to the lateral acetabular margin and the interteardrop line. In the normal pelvis, acetabular anteversion also can be measured on the AP radiograph [18] using the method described by Widmer [39]. However, the anterior wall margin of the acetabulum is not clearly seen on AP radiographs. In 39 of 50 hips in our study, the anterior acetabular margin was not evident on radiographs. Second, our method is not applicable when the acetabulum is not identifiable, such as with a fused hip. Third, our patients were operated on by one surgeon using a posterolateral approach. Accordingly, we could not determine whether the surgical approach affected cup alignment and intraoperator and interoperator variation could not be evaluated. However, we used bony landmarks in the acetabular rim to align the cup position. If the rim were completely exposed, there might be little difference in cup positioning regardless of the approach method. Fourth, to use our method, the surgeon should identify the landmarks, measure and mark the calculated distances, and then align the cup to the marks, which necessitates a learning curve. Fifth, our study was not a randomized clinical trial and we had no control group. However, our dislocation rate was zero, comparable or better than rates reported using a mechanical guide [28, 31, 32] or computer-assisted cup placement method [5, 11, 21, 36]. Sixth, our method might not be applicable in severely dysplastic hips with excessive acetabular abduction. However, we could position the cup properly using the method in our patients with hip dysplasia who had acetabular abduction of 46° to 49°. Seventh, we measured cup anteversion on postoperative radiographs. This measurement is inaccurate compared with CT scan measurement. Thus, we measured cup anteversion using the method of Woo and Morrey [40], which is reportedly reliable and valid [27]. Finally, our sample size was small. Because our study was not a case-control study, we could not calculate the sample size. The study design was reviewed by our institutional review board, which restricted the case number because of the radiation hazard and cost of CT scans.
Our alignment method needs no additional tools such as a numerical table, specific formula, or mathematical function. The method uses anatomic landmarks of the acetabulum, which are easily identified during THA, as guidance for cup alignment. In our study, all acetabular cups were positioned within the safe zone described by Lewinnek et al. [23], and the clinical results were satisfactory [13, 30] (Table 1). We used a target of 40° abduction and 15° anteversion. However, there is controversy in ideal cup positioning and some surgeons prefer different abduction and anteversion [2, 15, 35]. Sometimes the target position should be changed according to the patient’s limb length, kypholordotic deformity of the spine, and pelvic tilt [22]. In such situations, the target angles of 40° and 15° in the calculation formula should be changed.
Our method might not seem easy or practical because it requires comprehensive knowledge of acetabular anatomy, CT imaging, a functional pelvic plane, and mathematical formulas. However, the method can be summarized in four steps for practical use: (1) measure acetabular abduction (α°) and anteversion (β°) on preoperative CT scans; (2) calculate α − 40 and β − 15; (3) during the operation, locate the TAN and AAN and mark four reference points at the rim of the acetabulum: superior point; the opposite point of TAN, inferior point; |α − 40| mm inside (when α was > 40°) or outside the TAN(when α was < 40°), posterior point; the opposite point of AAN, and anterior point; |β − 15| mm inside (when β was < 15°) or outside the AAN (when β was > 15°); and (4) during press-fitting of the cup, adjust the cup abduction to the line between the superior and inferior points and cup anteversion to the line between the anterior and posterior points.
We believe our method using the TAN and AAN as landmarks for cup alignment can aid positioning of the acetabular component of a THA. It defines abduction and anteversion of the acetabulum and acetabular cup without the need for additional instrumentation and is independent of the position of the patient. Further studies are required to verify the accuracy and reproducibility of our method.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Seoul National University College of Medicine, Seoul, South Korea.
References
- 1.Archbold HA, Mockford B, Molloy D, McConway J, Ogonda L, Beverland D. The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement: a preliminary study of 1000 cases investigating postoperative stability. J Bone Joint Surg Br. 2006;88:883–886. doi: 10.1302/0301-620X.88B7.17577. [DOI] [PubMed] [Google Scholar]
- 2.Charnley J. Total hip replacement by low-friction arthroplasty. Clin Orthop Relat Res. 1970;72:7–21. [PubMed] [Google Scholar]
- 3.Daly PJ, Morrey BF. Operative correction of an unstable total hip arthroplasty. J Bone Joint Surg Am. 1992;74:1334–1343. [PubMed] [Google Scholar]
- 4.DiGioia AM, Jaramaz B, Blackwell M, Simon DA, Morgan F, Moody JE, Nikou C, Colgan BD, Aston CA, Labarca RS, Kischell E, Kanade T. The Otto Aufranc Award: image guided navigation system to measure intraoperatively acetabular implant alignment. Clin Orthop Relat Res. 1998;355:8–22. doi: 10.1097/00003086-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Digioia AM, 3rd, Jaramaz B, Plakseychuk AY, Moody JE, Jr, Nikou C, Labarca RS, Levison TJ, Picard F. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002;17:359–364. doi: 10.1054/arth.2002.30411. [DOI] [PubMed] [Google Scholar]
- 6.Dorr LD, Wolf AW, Chandler R, Conaty JP. Classification and treatment of dislocations of total hip arthroplasty. Clin Orthop Relat Res. 1983;173:151–158. [PubMed] [Google Scholar]
- 7.Eftekhar NS. Dislocation and instability complicating low friction arthroplasty of the hip joint. Clin Orthop Relat Res. 1976;121:120–125. [PubMed] [Google Scholar]
- 8.Engh CA, Griffin WL, Marx CL. Cementless acetabular components. J Bone Joint Surg Br. 1990;72:53–59. doi: 10.1302/0301-620X.72B1.2298795. [DOI] [PubMed] [Google Scholar]
- 9.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 10.Epstein NJ, Woolson ST, Giori NJ. Acetabular component positioning using the transverse acetabular ligament: can you find it and does it help? Clin Orthop Relat Res. 2011;469:412–416. doi: 10.1007/s11999-010-1523-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Etienne A, Cupic Z, Charnley J. Postoperative dislocation after Charnley low-friction arthroplasty. Clin Orthop Relat Res. 1978;132:19–23. [PubMed] [Google Scholar]
- 12.Ficat RP. Idiopathic bone necrosis of the femoral head: early diagnosis and treatment. J Bone Joint Surg Br. 1985;67:3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 13.Haaker RG, Tiedjen K, Ottersbach A, Rubenthaler F, Stockheim M, Stiehl JB. Comparison of conventional versus computer-navigated acetabular component insertion. J Arthroplasty. 2007;22:151–159. doi: 10.1016/j.arth.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 14.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 15.Harris WH. Advances in surgical technique for total hip replacement: without and with osteotomy of the greater trochanter. Clin Orthop Relat Res. 1980;146:188–204. [PubMed] [Google Scholar]
- 16.Hassan DM, Johnston GH, Dust WN, Watson G, Dolovich AT. Accuracy of intraoperative assessment of acetabular prosthesis placement. J Arthroplasty. 1998;13:80–84. doi: 10.1016/S0883-5403(98)90079-1. [DOI] [PubMed] [Google Scholar]
- 17.Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res. 2004;426:174–179. doi: 10.1097/01.blo.0000141903.08075.83. [DOI] [PubMed] [Google Scholar]
- 18.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis : a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelley TC, Swank ML. Role of navigation in total hip arthroplasty. J Bone Joint Surg Am. 2009;91(suppl 1):153–158. doi: 10.2106/JBJS.H.01463. [DOI] [PubMed] [Google Scholar]
- 20.Kim YH, Kim VE. Uncemented porous-coated anatomic total hip replacement: results at six years in a consecutive series. J Bone Joint Surg Br. 1993;75:6–13. doi: 10.1302/0301-620X.75B1.8421036. [DOI] [PubMed] [Google Scholar]
- 21.Latimer HA, Lachiewicz PF. Porous-coated acetabular components with screw fixation: five to ten-year results. J Bone Joint Surg Am. 1996;78:975–981. doi: 10.2106/00004623-199607000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Legaye J. Influence of the sagittal balance of the spine on the anterior pelvic plane and on the acetabular orientation. Int Orthop. 2009;33:1695–1700. doi: 10.1007/s00264-008-0702-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 24.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty: causes and prevention. Clin Orthop Relat Res. 1990;261:159–170. [PubMed] [Google Scholar]
- 25.Mofidi A, Shields JS, Stubbs AJ. Central acetabular osteophyte (saber tooth sign), one of the earlist signs of osteoarthritis of the hip joint. Eur J Orthop Surg Traumatol. 2011;21:71–74. doi: 10.1007/s00590-010-0663-z. [DOI] [Google Scholar]
- 26.Murtha PE, Hafez MA, Jaramaz B, DiGioia AM., 3rd Variations in acetabular anatomy with reference to total hip replacement. J Bone Joint Surg Br. 2008;90:308–313. doi: 10.1302/0301-620X.90B3.19548. [DOI] [PubMed] [Google Scholar]
- 27.Nho JH, Lee YK, Kim HJ, Ha YC, Suh YS, Koo KH. Reliability and validity of measuring version of the acetabular component. J Bone Joint Surg Br. 2012;94:32–36. doi: 10.1302/0301-620X.94B1.27621. [DOI] [PubMed] [Google Scholar]
- 28.Nogler M, Kessler O, Prassl A, Donnelly B, Streicher R, Sledge JB, Krismer M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop Relat Res. 2004;426:159–163. doi: 10.1097/01.blo.0000141902.30946.6d. [DOI] [PubMed] [Google Scholar]
- 29.Ohlin A, Balkfors B. Stability of cemented sockets after 3–14 years. J Arthroplasty. 1992;7:87–92. doi: 10.1016/0883-5403(92)90037-Q. [DOI] [PubMed] [Google Scholar]
- 30.Parratte S, Argenson JN. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty: a prospective, randomized, controlled study. J Bone Joint Surg Am. 2007;89:494–499. doi: 10.2106/JBJS.F.00529. [DOI] [PubMed] [Google Scholar]
- 31.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 32.Pellicci PM, Salvati EA, Robinson HJ. Mechanical failures in total hip replacement requiring reoperation. J Bone Joint Surg Am. 1979;61:28–36. [PubMed] [Google Scholar]
- 33.Ritter MA. A treatment plan for the dislocated total hip arthroplasty. Clin Orthop Relat Res. 1980;153:153–155. [PubMed] [Google Scholar]
- 34.Schlenzka D, Laine T, Lund T. [Computer-assisted spine surgery: principles, technique, results and perspectives][in German] Orthopade. 2000;29:658–669. doi: 10.1007/s001320050508. [DOI] [PubMed] [Google Scholar]
- 35.Seki M, Yuasa N, Ohkuni K. Analysis of optimal range of socket orientations in total hip arthroplasty with use of computer-aided design simulation. J Orthop Res. 1998;16:513–517. doi: 10.1002/jor.1100160418. [DOI] [PubMed] [Google Scholar]
- 36.Stem ES, O’Connor MI, Kransdorf MJ, Crook J. Computed tomography analysis of acetabular anteversion and abduction. Skeletal Radiol. 2006;35:385–389. doi: 10.1007/s00256-006-0086-4. [DOI] [PubMed] [Google Scholar]
- 37.Suh KT, Park BG, Choi YJ. A posterior approach to primary total hip arthroplasty with soft tissue repair. Clin Orthop Relat Res. 2004;418:162–167. doi: 10.1097/00003086-200401000-00026. [DOI] [PubMed] [Google Scholar]
- 38.Turner RS. Postoperative total hip prosthetic femoral head dislocations: incidence, etiologic factors, and management. Clin Orthop Relat Res. 1994;301:196–204. [PubMed] [Google Scholar]
- 39.Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004;19:387–390. doi: 10.1016/j.arth.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 40.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]