Abstract
Background
The Bernese periacetabular osteotomy (PAO) can relieve pain and restore function in patients with symptomatic acetabular dysplasia. Accurate acetabular correction is fundamental to achieving these clinical goals and presumably enhancing survivorship of the reconstruction. Fluoroscopy is used by some surgeons to assess intraoperative acetabular correction but it is unclear whether the features observed by fluoroscopy accurately reflect those on postoperative radiographs.
Questions/Purposes
We therefore determined whether the parameters of acetabular correction of PAO correlated on intraoperative fluoroscopic imaging and postoperative radiography.
Methods
We retrospectively reviewed the imaging of 48 patients (50 hips) who underwent PAO. Intraoperative fluoroscopic AP and false profile images were obtained after final PAO correction. The intraoperative deformity correction as measured on the two fluoroscopy views was compared with the correction determined with postoperative standing plain AP pelvis and false profile radiographs using common measurements of acetabular position.
Results
Of all radiographic parameters, lateral center-edge angle had the highest correlation between intraoperative fluoroscopy and the postoperative radiograph with an intraclass correlation coefficient (ICC) of 0.80 (0.68–0.88). Similarly, acetabular inclination and anterior center-edge angle also correlated with ICCs of 0.76 (0.61–0.85) and 0.71 (0.54–0.82), respectively. Extrusion index and medial offset distance had lower correlations with ICCs of 0.66 (0.46–0.79) and 0.46 (0.21–0.65), respectively.
Conclusions
Intraoperative fluoroscopic assessment of PAO correction correlated with that from the postoperative radiographic assessment. Measurement of lateral center-edge angle shows the highest correlation with the fewest outliers. Acetabular inclination and anterior center-edge angle also correlated; extrusion index and medial offset distance should be used with more caution.
Introduction
Insufficient acetabular coverage of the femoral head in developmental dysplasia of the hip (DDH) is a major cause of hip pain, dysfunction, and secondary osteoarthritis [4, 7, 9, 10, 12, 21]. The Bernese periacetabular osteotomy (PAO) is commonly used for treating patients with symptomatic dysplasia. It helps restore normal hip biomechanics, decreases symptoms, improves function, and theoretically prolongs the longevity of the hip [20, 22, 25, 27, 33]. The PAO involves a series of osteotomies that allow for three-dimensional reorientation of the acetabulum. Precise reorientation is fundamental to achieving the clinical goals because normalizing acetabular inclination, extrusion index, and medial offset correlate with pain levels, physical function, and survivorship at 7 to 20 years after PAO [26, 27, 31]. Lateral center-edge angle of Wiberg and anterior center-edge angle of Lequesne are other radiographic parameters that are frequently used to judge acetabular reorientation [5].
To proficiently reorient the acetabulum, surgeons frequently rely on intraoperative plain radiographs or fluoroscopic imaging. Fluoroscopy can be used to evaluate each of the aforementioned measurements in an attempt to produce the desired correction. Moreover, radiographic parameters of acetabular position can be affected by pelvic rotation necessitating a very careful, systematic approach to the use of intraoperative imaging. Although intraoperative fluoroscopic imaging is time-efficient and convenient, it is unclear whether the corrections on intraoperative fluoroscopy correlate with those on postoperative radiographs.
We therefore assessed the correlation between intraoperative fluoroscopic imaging and postoperative radiography in assessing parameters of acetabular correction during PAO.
Patients and Methods
We retrospectively reviewed the radiographs from all 90 patients (99 hips) who underwent PAO for DDH between October 30, 2006, and January 31, 2011. Two surgeons (JCC and PLS) performed all surgeries. We excluded 49 of the hips (42 patients) operated on during this time because intraoperative fluoroscopic views were not archived in our electronic medical record and were unavailable for review. Intraoperative fluoroscopic AP and false profile images were obtained after final PAO correction and fixation of the remaining 50 hips (48 patients) that were included in our study for review. We used standing, weightbearing, followup AP, and false profile radiographs that were taken at an average of 11 weeks (range, 4–57 weeks) after surgery. We obtained prior internal review board approval.
We used a standardized fluoroscopic technique intraoperatively to standardize pelvic tilt and rotation. First, the fluoroscope was positioned approximately 6 inches above the patient such that both obturator foramina and the majority of the pelvic ring were visible on the fluoroscope. The fluoroscope was aligned perpendicular to the patient and adjusted in the coronal and sagittal planes until acceptable pelvic position was obtained. We did not consider an AP pelvis image acceptable until obturator foramina were symmetric from side to side, the coccyx was in line with the center of the pubic symphysis, the pubic symphysis was vertical, and the sacrococcygeal junction was 1 to 5 cm away from the pubic symphysis. After fluoroscopic calibration, at the midline, AP images of the operative hip were performed by directly translating the fluoroscope to a position centered over the right hip without adjusting the magnification, tilt, or rotation of the image. This allowed observation of the obturator foramen, the entire joint, the greater trochanter, and the majority of the periacetabular region of the ipsilateral hemipelvis. Similarly, for the intraoperative false profile view, we aligned the fluoroscope perpendicular to the patient, directly centered over the femoral head, and then rolled back over the patient to obtain a 65°-lateral projection [18]. Intraoperative deformity correction was analyzed subjectively with variable goals of correcting the hip to obtain a lateral center-edge angle of 20° to 35°, acetabular inclination of 0° to 15°, extrusion index of 10° to 25%, medial offset of 5 to 15 mm, and anterior center-edge angle of 20° to 30°. Nevertheless, definitive correction also was influenced by the degree of dysplasia preoperatively and the hip ROM at the time of acetabular correction. Specifically, acetabular reduction was adjusted to maintain at least 90° hip flexion.
The magnitude of corrections in our series averaged 18.7° for lateral center-edge angle, 8.4° for anterior center-edge angle, −13.2° for acetabular inclination, 24% for extrusion index, and −4.4 mm for medial offset.
We performed standing, weightbearing AP pelvis postoperative images using a standardized technique. They were obtained with the patient standing with their legs in 15° internal rotation with the crosshairs of the x-ray beam centered on a point midway between the superior border of the pubic symphysis and a line drawn connecting the anterosuperior iliac spines. We used an x-ray tube-to-film distance of 120 cm with the tube oriented perpendicular to the standing patient and cassette [5]. False profile radiographs were obtained with the patient in a standing position with the affected hip against the cassette and the pelvis rotated 65° in relation to the Bucky wall stand. The foot on the same side as the affected hip was positioned so that it was parallel to the cassette. We centered the central beam on the femoral head with a tube-to-film distance of approximately 40 inches (102 cm) [5].
Radiographic analysis was performed electronically in chronologic order by one author (CLL, not a treating surgeon) experienced in radiographic measurements of the prearthritic hip [8, 18, 24, 29, 34] using ImageJ software (National Institutes of Health, Bethesda, MD, USA). Analysis included measurement of the lateral center-edge angle, anterior center-edge angle, acetabular inclination, extrusion index, and medial offset distance. We repeated electronic measurements on 10 of the postoperative radiographic images used in our study to confirm intraobserver reliability. The intraclass correlation coefficients (ICCs) for intraobserver variability ranged from 0.82 to 1.0. Interobserver reliability has been established in multiple studies with ICCs for lateral center-edge angle ranging from 0.42 to 0.92, acetabular inclination from 0.45 to 0.85, extrusion index from 0.84 to 0.91, medial offset of 0.8, and anterior center-edge angle from 0.55 to 0.88 [1–3, 6, 19, 23, 28].
We compared the intraoperative fluoroscopic deformity correction with correction on postoperative plain AP pelvis and false profile images. Additionally, preoperative AP pelvis and false profile measurements were compared with postoperative measurements. We determined correlation between measurements of acetabular position made on intraoperative fluoroscopy and postoperative radiographs using the ICC. Additionally, for each radiographic parameter the percentage of cases with a relevant threshold (ie, 5°) is reported.
Results
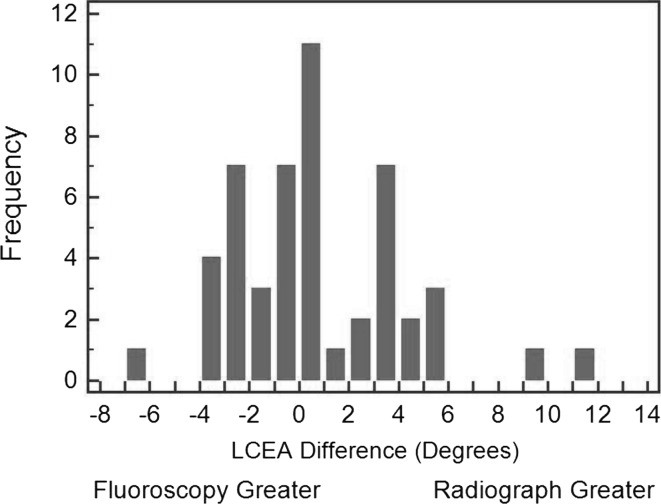
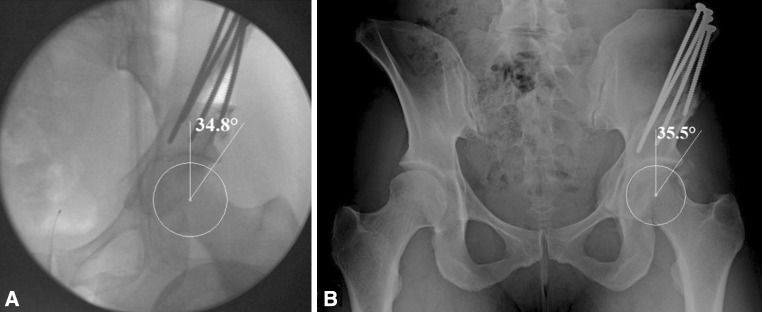
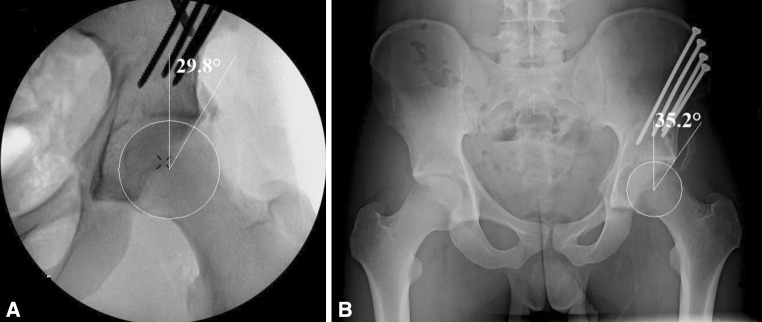
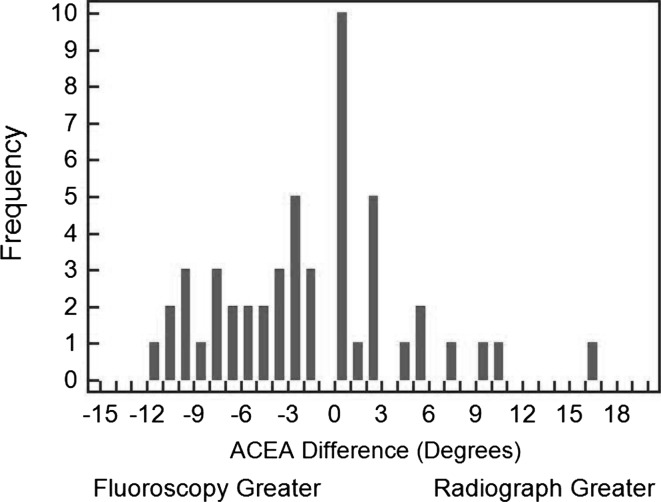
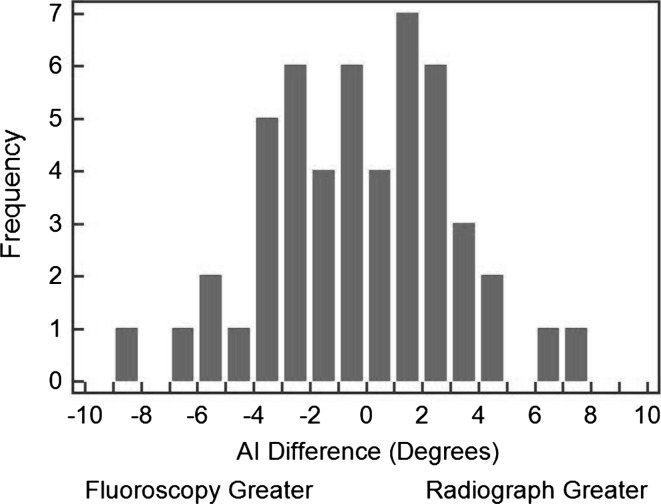
The mean measurements for intraoperative fluoroscopy and postoperative plain radiographs for lateral center-edge angle, center-edge angle, anterior center-edge angle, acetabular inclination,, extrusion index, and medial offset are shown (Table 1).When comparing intraoperative fluoroscopy with postoperative plain radiographs, the lateral center-edge angle showed an ICC of 0.80 (the highest correlation observed) (Table 2). In 88% of cases, intraoperative and postoperative lateral center-edge angle were within 5° (Fig. 1). Examples showing good agreement of lateral center-edge angle measurements between intraoperative fluoroscopy and the postoperative radiograph are shown (Fig. 2). In contrast, we also have provided examples that show poor agreement of lateral center-edge angle measurements between intraoperative fluoroscopy and postoperative radiographs (Fig. 3). Similarly, acetabular inclination, anterior center-edge angle, and extrusion index all showed a high amount of correlation but less than the lateral center-edge angle (Table 2). Intraoperative measurements for anterior center-edge angle were within 5° of postoperative measurements in 72% of cases (Fig. 4). Intraoperative measurements for acetabular inclination were within 5° of postoperative measurements in 60% of cases (Fig. 5). Extrusion index was within 5% for 72% of cases. Medial offset was the least reliable measurement showing only moderate correlation with an ICC of 0.46. Measurement of medial offset between intraoperative fluoroscopy and postoperative radiographs was within 5 mm in 76% of cases.
Table 1.
Total correction obtained between preoperative radiographs, intraoperative fluoroscopy, and postoperative radiographs
| Radiographic measurement | Preoperative radiograph | Intraoperative fluoroscopy | Postoperative radiograph | Average correction (preoperative to postoperative radiograph) | Average difference (fluoroscopy to postoperative radiograph) |
|---|---|---|---|---|---|
| LCEA | 6.6° (−15.2°–29.3°) | 27.4° (18.7°–40.5°) | 25.3° (18.4°–40.7°) | 18.7° | 2.1° |
| ACEA | 15.1° (−27.7°–28.3°) | 30.3° (18.5°–46.5°) | 23.4° (13.8°–53.1°) | 8.4° | 6.9° |
| AI | 21.3° (5.2°–51.2°) | 7.8° (−4.8°–13.4°) | 8.1° (−4.8°–13.4°) | −13.2° | −0.3° |
| EI | 43% (19%–66%) | 27% (7%–33%) | 23% (9%–32%) | 24% | 4% |
| MO | 14.6 (5.8–32.5) mm | 8.7 (1.1–29.3) mm | 10.2 (–3.1, 19.3) mm | −4.4 mm | −1.5 mm |
LCEA = lateral center-edge angle; ACEA = anterior center-edge angle; AI = acetabular inclination; EI = extrusion index; MO = medial offset.
Table 2.
Intraclass correlation coefficients between intraoperative fluoroscopic and postoperative radiograph measurements
| Radiographic measurement | ICC | 95% CI |
|---|---|---|
| LCEA | 0.80 | 0.68–0.88 |
| ACEA | 0.71 | 0.54–0.82 |
| AI | 0.76 | 0.61–0.85 |
| EI | 0.66 | 0.46–0.79 |
| MO | 0.46 | 0.21–0.65 |
ICC = intraclass correlation coefficient; LCEA = lateral center-edge angle; ACEA = anterior center-edge angle; AI = acetabular inclination; EI = extrusion index; MO = medial offset.
Fig. 1.
The bar graph shows the difference in lateral center-edge angle (LCEA) between intraoperative fluoroscopy and postoperative AP radiographs.
Fig. 2A–B.
Examples of (A) an intraoperative fluoroscopy image and (B) postoperative radiograph show agreement between lateral center-edge angle measurements.
Fig. 3A–B.
Examples of (A) an intraoperative fluoroscopy image and (B) postoperative radiograph show low agreement between lateral center-edge angle measurements.
Fig. 4.
The difference in anterior center-edge angle (ACEA) between intraoperative fluoroscopy and postoperative AP images is shown.
Fig. 5.
The difference in acetabular inclination (AI) between intraoperative fluoroscopy and postoperative AP images is shown.
Discussion
PAO is a highly technical operation dependent on precise reorientation of the acetabulum to improve pain, restore function, and provide a durable reconstruction [15, 26, 27, 31]. We investigated the correlation of intraoperative fluoroscopy with postoperative plain radiographic assessment of acetabular reorientation. Correlation of intraoperative fluoroscopy is important because it is one method used intraoperatively by surgeons to determine parameters of acetabular correction. However, it is unclear whether the parameters measured on intraoperative fluoroscopy correlate to those measured on postoperative radiographs. We therefore assessed the correlation between intraoperative fluoroscopic imaging and postoperative radiography in assessing parameters of acetabular correction during PAO.
Our study has certain limitations. First, the fluoroscopic images were taken with the patient in the supine position, whereas the postoperative radiographs were taken with the patient standing, which can produce variances in pelvic tilt and rotation. Konishi and Mieno [14]showed the pelvis tilts approximately 5° posteriorly when radiographs are taken with the patient in a standing versus supine position. There are also patient-specific variances in pelvic tilt that were not reproduced exactly with our fluoroscopic examination. Kojima et al. [13] analyzed the effect of pelvic tilt on lateral center-edge angle in normal and dysplastic hips and found supine radiographs tend to overestimate the lateral center-edge angle by 1° to 2° when compared with standing radiographs. Similarly, Troelsen et al. [32]quantified the effect of supine versus standing radiographs on lateral center-edge angle, acetabular inclination, and medial offset. They found the measured lateral center-edge angle decreased by 1.3° to 1.6°, acetabular inclination increased by 1.6° to 2.3°, and medial offset decreased by 0.06 to 0.14 cm on standing radiographs. Lee et al. [17] analyzed the effect of pelvic tilt on radiographic projection of hip structure and showed changes in pelvic tilt as much as 20° did not have a substantial effect on lateral center-edge angle but did produce substantial changes in acetabular inclination. Although these studies confirm pelvic tilt does affect the radiographic projection of hip structure, the effects on the radiographic parameters analyzed in our study are relatively small. Second, the location of the center of the radiographic beam influences the projection of radiographic images [11]. An image centered on the hip will project differently than an image centered on the pelvis. Standard assessment of morphologic features of the acetabulum uses AP pelvis images, not AP hip images. This projection cannot be reproduced with fluoroscopy owing to the limited field of view. However, despite this theoretical limitation, we observed strong correlations between fluoroscopic images and postoperative radiographs. Therefore, the differences resulting from variances in radiographic projection between AP pelvis and AP hip images are likely small if both images are obtained with acceptable pelvic tilt and rotation. Another difference between fluoroscopy and plain radiographs is that fluoroscopic images have poorer resolution than plain radiographs potentially making it more difficult to find the necessary landmarks for measurement. In addition, intraoperative AP pelvis radiographs have limitations relative to pelvic position, projection, and image quality. Finally, in comparing our intraoperative and postoperative images, we are assuming there had been no migration of the acetabular fragment. We did not observe loss or change in the acetabular correction in any case; however, we acknowledge that small position changes are possible. We also recognize that correlations between intraoperative fluoroscopy and postoperative radiographs could be much lower if fluoroscopic images were rotated or magnified in ways other than the standardized technique described in this article.
Our data indicate intraoperative fluoroscopy is reliable for predicting postoperative acetabular position. The fluoroscopic measurement with the greatest correlation with postoperative radiographic correction was lateral center-edge angle. Similarly, acetabular inclination, anterior center-edge angle, and extrusion index also had substantial reliability, whereas medial offset was the least reliable. In one of the earlier series of PAOs published, Siebenrock et al. [26] showed that cases in which postoperative acetabular inclination correction was not within the 0° to 10° range correlated with worse Postel and Merle D’Aubigné scores (worse pain, decreased ability to ambulate) at an average of 11 years followup Similarly, Troelsen et al. [31] found a medial offset greater than 2 cm correlated with poor 9-year survivorship of PAO. At 20 years followup, Steppacher et al. [27] found a postoperative extrusion index of 20% or greater correlated with poor survivorship of PAO. At an average followup of 9-years Matheney et al. [20] observed an age older than 35 years and poor preoperative congruency predicted poor results defined as either conversion to THA or having a pain score greater than 10 on the WOMAC pain score. These studies showed acetabular inclination, medial offset, and extrusion index correlate with clinical outcomes at 9 to 20 years, but do not show a direct correlation between lateral center-edge angle and anterior center-edge angle and clinical outcomes at 9 to 20 years. These studies reinforce the concept that radiographic measurements are an important marker of correct acetabular position and correlate to clinical outcomes. However, the small differences we found in the measurements between intraoperative fluoroscopy and postoperative radiographs would likely not be large enough to alter the long-term outcome. Thus, fluoroscopy seems to be an acceptable tool in allowing the surgeon to accurately assess the degree of correction of the osteotomy intraoperatively.
Kuhnel et al. [16] recently evaluated the reliability of intraoperative fluoroscopy in comparison to postoperative radiographs on 22 consecutive patients. They calculated kappa values of 0.65 for acetabular inclination and 0.55 for lateral center-edge angle for agreement between intraoperative fluoroscopy and postoperative plain radiographs. Unlike Kuhnel et al., we found acetabular inclination and lateral center-edge angle to be more reliable for producing the desired correction. Troelsen [30] reported the reliability of a novel device that can be used intraoperatively in conjunction with fluoroscopy for determining angular correction. The device involves securing intraoperative pins in bilateral anterosuperior iliac spines to which a radiopaque measurement device can be centered over the femoral head and attached. Using this device, he found fluoroscopic measurements were within ± 5% in 95% of postoperative measurements for lateral center-edge angle and acetabular inclination in 35 hips. Similar to the study by Troelsenl, we found measurements of lateral center-edge angle and acetabular inclination can be used on intraoperative fluoroscopy to reliably produce the desired amount of correction on postoperative plain radiographs. In addition to the studies by Kuhnel et al. and Troelsen, we expanded our measurements by analyzing the anterior center-edge angle, extrusion index, and medial offset. We found these measurements to be less reliable than lateral center-edge angle and acetabular inclination.
Our study suggests intraoperative fluoroscopy is an acceptable tool for assessing acetabular correction in PAO. Measurements of lateral center-edge angle, acetabular inclination, and anterior center-edge angle show the greatest correlation with postoperative plain radiographs. Extrusion index and medial offset should be used with more caution when making intraoperative decisions regarding acetabular correction. Intraoperative fluoroscopy continues to be our preferred imaging modality for assessing acetabular deformity correction in PAO.
Acknowledgments
We thank Debbie Long for help in preparation of the manuscript for submission.
Footnotes
The institution of one of the authors (JCC) received funding from the Curing Hip Disease Fund (St. Louis, MO, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Anderson LA, Gililland J, Pelt C, Linford S, Stoddard GJ, Peters CL. Center edge angle measurement for hip preservation surgery: technique and caveats. Orthopedics. 2011;34:86. doi: 10.3928/01477447-20101221-17. [DOI] [PubMed] [Google Scholar]
- 2.Carlisle JC, Zebala LP, Shia DS, Hunt D, Morgan PM, Prather H, Wright RW, Steger-May K, Clohisy JC. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J. 2011;31:52–58. [PMC free article] [PubMed] [Google Scholar]
- 3.Carroll KL, Murray KA, MacLeod LM, Hennessey TA, Woiczik MR, Roach JW. Measurement of the center edge angle and determination of the Severin classification using digital radiography, computer-assisted measurement tools, and a Severin algorithm: intraobserver and interobserver reliability revisited. J Pediatr Orthop. 2011;31:e30–e35. doi: 10.1097/BPO.0b013e31821adde9. [DOI] [PubMed] [Google Scholar]
- 4.Clohisy JC, Beaule PE, O’Malley A, Safran MR, Schoenecker P. AOA symposium. Hip disease in the young adult: current concepts of etiology and surgical treatment. J Bone Joint Surg Am. 2008;90:2267–2281. doi: 10.2106/JBJS.G.01267. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clohisy JC, Carlisle JC, Trousdale R, Kim YJ, Beaule PE, Morgan P, Steger-May K, Schoenecker PL, Millis M. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467:666–675. doi: 10.1007/s11999-008-0626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hasegawa Y, Iwata H, Mizuno M, Genda E, Sato S, Miura T. The natural course of osteoarthritis of the hip due to subluxation or acetabular dysplasia. Arch Orthop Trauma Surg. 1992;111:187–191. doi: 10.1007/BF00571474. [DOI] [PubMed] [Google Scholar]
- 8.Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32:767–778. [PubMed] [Google Scholar]
- 9.Jacobsen S, Sonne-Holm S. Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology (Oxford). 2005;44:211–218. doi: 10.1093/rheumtology/keh436. [DOI] [PubMed] [Google Scholar]
- 10.Jingushi S, Ohfuji S, Sofue M, Hirota Y, Itoman M, Matsumoto T, Hamada Y, Shindo H, Takatori Y, Yamada H, Yasunaga Y, Ito H, Mori S, Owan I, Fujii G, Ohashi H, Iwamoto Y, Miyanishi K, Iga T, Takahira N, Sugimori T, Sugiyama H, Okano K, Karita T, Ando K, Hamaki T, Hirayama T, Iwata K, Nakasone S, Matsuura M, Mawatari T. Osteoarthritis hip joints in Japan: involvement of acetabular dysplasia. J Orthop Sci. 2011;16:156–164. doi: 10.1007/s00776-011-0025-7. [DOI] [PubMed] [Google Scholar]
- 11.Kakaty DK, Fischer AF, Hosalkar HS, Siebenrock KA, Tannast M. The ischial spine sign: does pelvic tilt and rotation matter? Clin Orthop Relat Res. 2010;468:769–774. doi: 10.1007/s11999-009-1021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim YJ, Jaramillo D, Millis MB, Gray ML, Burstein D. Assessment of early osteoarthritis in hip dysplasia with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. J Bone Joint Surg Am. 2003;85:1987–1992. doi: 10.1302/0301-620X.85B2.13289. [DOI] [PubMed] [Google Scholar]
- 13.Kojima A, Nakagawa T, Tohkura A. Simulation of acetabular coverage of femoral head using anteroposterior pelvic radiographs. Arch Orthop Trauma Surg. 1998;117:330–336. doi: 10.1007/s004020050260. [DOI] [PubMed] [Google Scholar]
- 14.Konishi N, Mieno T. Determination of acetabular coverage of the femoral head with use of a single anteroposterior radiograph: a new computerized technique. J Bone Joint Surg Am. 1993;75:1318–1333. doi: 10.2106/00004623-199309000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Kralj M, Mavcic B, Antolic V, Iglic A, Kralj-Iglic V. The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7–15-year follow-up of 26 hips. Acta Orthop. 2005;76:833–840. doi: 10.1080/17453670510045453. [DOI] [PubMed] [Google Scholar]
- 16.Kuhnel SP, Kalberer FA, Dora CF. Periacetabular osteotomy: validation of intraoperative fluoroscopic monitoring of acetabular orientation. Hip Int. 2011;21:303–310. doi: 10.5301/HIP.2011.8389. [DOI] [PubMed] [Google Scholar]
- 17.Lee YK, Chung CY, Koo KH, Lee KM, Kwon DG, Park MS. Measuring acetabular dysplasia in plain radiographs. Arch Orthop Trauma Surg. 2011;131:1219–1226. doi: 10.1007/s00402-011-1279-4. [DOI] [PubMed] [Google Scholar]
- 18.Lequesne M, de Seze. [False profile of the pelvis: a new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies][in French]. Rev Rhum Mal Osteoartic. 1961;28:643–652. [PubMed]
- 19.Mast NH, Impellizzeri F, Keller S, Leunig M. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res. 2011;469:188–199. doi: 10.1007/s11999-010-1447-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the bernese periacetabular osteotomy and predictors of clinical outcome: surgical technique. J Bone Joint Surg Am. 2010;92(suppl 1 pt 2):115–129. doi: 10.2106/JBJS.J.00646. [DOI] [PubMed] [Google Scholar]
- 21.Mavcic B, Iglic A, Kralj-Iglic V, Brand RA, Vengust R. Cumulative hip contact stress predicts osteoarthritis in DDH. Clin Orthop Relat Res. 2008;466:884–891. doi: 10.1007/s11999-008-0145-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murphy S, Deshmukh R. Periacetabular osteotomy: preoperative radiographic predictors of outcome. Clin Orthop Relat Res. 2002;405:168–174. doi: 10.1097/00003086-200212000-00021. [DOI] [PubMed] [Google Scholar]
- 23.Nelitz M, Guenther KP, Gunkel S, Puhl W. Reliability of radiological measurements in the assessment of hip dysplasia in adults. Br J Radiol. 1999;72:331–334. doi: 10.1259/bjr.72.856.10474491. [DOI] [PubMed] [Google Scholar]
- 24.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 25.Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239–245. [PubMed] [Google Scholar]
- 26.Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20. doi: 10.1097/00003086-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26:1199–1205. doi: 10.1002/jor.20653. [DOI] [PubMed] [Google Scholar]
- 29.Tönnis D, editor. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Heidelberg, Germany: Springer; 1987. [Google Scholar]
- 30.Troelsen A. Surgical advances in periacetabular osteotomy for treatment of hip dysplasia in adults. Acta Orthop Suppl. 2009;80:1–33. doi: 10.1080/17453690610046585. [DOI] [PubMed] [Google Scholar]
- 31.Troelsen A, Elmengaard B, Soballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179. doi: 10.2106/JBJS.H.00994. [DOI] [PubMed] [Google Scholar]
- 32.Troelsen A, Jacobsen S, Romer L, Soballe K. Weightbearing anteroposterior pelvic radiographs are recommended in DDH assessment. Clin Orthop Relat Res. 2008;466:813–819. doi: 10.1007/s11999-008-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995;77:73–85. doi: 10.2106/00004623-199501000-00010. [DOI] [PubMed] [Google Scholar]
- 34.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(suppl 58):28–38. [Google Scholar]