Abstract
Background
Cam-type, pincer, and mixed femoroacetabular impingement (FAI) are accepted causes of labral and acetabular rim injury; however, the abnormal contact stresses associated with motion may damage other areas of the hip. Although cartilage damage to the femoral head has been reported previously in athletes, FAI-associated focal parafoveal chondral defects differ from previously reported lesions and represent a rare manifestation of the complex pathomechanics associated with FAI.
Questions/Purposes
We describe the clinical, radiographic, and surgical characteristics of a rare focal anterolateral parafoveal femoral chondral defect associated with FAI.
Methods
We retrospectively reviewed 10 patients with symptomatic FAI diagnosed with this unique focal defect confirmed at the time of surgical dislocation. Patients presented with hip pain, clinical findings of FAI, and, frequently, with an identifiable lesion on MRI arthrography. The minimum clinical followup was 12 months (mean, 29 months; range, 12–72 months).
Results
The consistent characteristics of these lesions associated with FAI differ from previously reported femoral chondral damage reported after hip dislocation or lateral impact in that there was no discrete injury such as a fall or dislocation/subluxation, no associated traumatic femoral lesion, and all were localized to the posterosuperior femoral head. Eight of 10 were diagnosed preoperatively using MR arthrography.
Conclusions
Despite radiographic similarities to findings of osteoarthritis and osteonecrosis, these FAI-associated femoral chondral defects were amenable to surgical reconstruction using first- or second-generation cartilage repair techniques during surgical treatment of impingement. The etiology of these lesions may be related to complex intraarticular forces generated by FAI-associated transient hip subluxation or forceful nonconcentric motion.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Osseous pathomorphologies, including femoral and acetabular deformity, that contribute to femoroacetabular impingement (FAI) are increasingly diagnosed [2]. Labral and acetabular damage caused by FAI is increasingly recognized as a source of pain and osteoarthritic changes in the hip [8]. Anatomic variations associated with FAI and premature osteoarthritis of the hip are established [13]. The mechanical consequence of FAI may be activity-specific affected by the direction and magnitude of force necessary to perform certain motions. Consequently, the specific chondral injury pattern associated with each unique anatomic deformity may differ between patients.
Damage to the acetabular labrum and the adjacent acetabular cartilage follows typical damage patterns of both cam and pincer FAI. Additionally, characteristic femoral chondral fibrocystic changes, today called impingement cysts [11], previously named herniation pits, are localized at the head-neck junction distal to the physis and frequently visible radiographically [11, 12, 15, 18]. Histologically these lesions consist of proliferative fibroblasts forming either dense fibrous tissue or gelatinous tissue.
Lamontagne et al. [10] have reported the mechanical consequence of cam-type FAI. Analysis of hip and pelvic motion during maximum squat demonstrates patients with cam-type FAI have less sagittal plane motion and decreased depth of squatting compared with nonimpinging hips. Similarly, Kennedy et al. [9] demonstrated decreased peak hip abduction, decreased frontal ROM, and attenuated pelvic roll in cam-type FAI compared with controls. In a novel motion capture analysis performed in a professional ballet dancer with normal hips, Charbonnier et al. [4, 5] demonstrated transient subluxation of the hip in certain ballet positions, especially those involving abduction and external rotation in maximum flexion. These findings suggest translational hip motion is associated with FAI. Translation depends on multiple factors including femoral and acetabular anatomy, activity-specific motions, force, direction, and momentum. We suggest impingement induces instability and translation by noncongruent hip motion. When the femur begins to rotate around an impingement point, this leads to translation between the femur and the acetabulum that induces complex pathologic forces leading to hyaline cartilage deformation that may produce the described femoral head cartilage lesions. Such high contact stresses associated with these abnormal motions may produce unique lesions.
In addition to using first-generation microfracture techniques, one of us recently reported a technique to treat focal defects using autologous matrix-induced chondrogenesis (AMIC), a second-generation bone marrow stimulation technique [14]. We found the AMIC technique was capable of restoring chondral tissue within femoral chondral defects associated with a variety of pathologic conditions.
The purpose of this article is to describe the pathologic characteristics, MRI findings, and surgical management of a unique femoral-sided chondral lesion localized adjacent to the fovea found in a subcohort of young patients who perform activities that share hip motion associated with substantial force and rapid limb velocity. These cases provide further insight into the mechanical and pathologic sequelae of FAI and are differentiated from end-stage arthritic changes that are well-recognized radiographic and pathologic findings associated with hip arthritis.
Patients and Methods
Between January 2003 and December 2010 we treated approximately 600 patients with surgical hip dislocations for symptomatic FAI performed at two institutions by the authors. We excluded patients diagnosed with intraarticular synovial and neoplastic disorders, posttraumatic deformities, postinfectious etiology, and childhood-related disorders including slipped capital femoral epiphysis, Legg-Calve-Perthes disease, and epiphyseal dysplasia. Ten patients who presented for surgery to treat painful FAI had associated full-thickness parafoveal chondral lesions localized anterolateral to the fovea confirmed at the time of surgical dislocation. All patients had a component of cam-type FAI and eight of the 10 femoral lesions were diagnosed preoperatively by MRI arthrography (Table 1). There were seven males and three females (six US, four Switzerland). Three of these 10 patients were reported in another series [14] describing the use of AMIC to treat a variety of femoral chondral lesions associated with multiple pathologic conditions. The average age was 27 years ± 10 months with a range of 16 to 31 years. All the patients were either athletic or involved in a vocation requiring rapid or forceful hip flexion. The minimum followup was 12 months (mean, 29 months; range, 12–72 months). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
Table 1.
Patient characteristics, FAI-associated pathology, and management
| Patient number | Age (years) | Sex | Primary deformity | AP alpha angle | LCA | Lateral alpha angle | PW | Crossover | FAI pathology | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 19 | M | Cam | 56 | 29 | 49 | + | + | Chondral delamination | Débridement, FNO |
| 2 | 27 | M | Cam | 76 | 35 | 52 | + | + | Labral detachment | Partial labral débridement, FNO |
| 3 | 17 | F | Combined | 61 | 38 | 41 | − | − | Labral inflammation | FNO |
| 4 | 20 | M | Cam | 61 | 39 | 65 | + | + | Chondral delamination | Débridement, FNO |
| 5 | 17 | M | Cam | 45 | 33 | 46 | − | + | Labral detachment, chondral delamination | Débridement labrum and cartilage flap, FNO |
| 6 | 26 | M | Cam | 75 | 30 | 76 | + | + | Labral detachment | Partial labral débridement, FNO |
| 7 | 30 | M | Cam | 50 | 36 | 45 | + | + | Mild labral detachment | Débridement, AMIC, FNO |
| 8 | 22 | F | Cam | 38 | 26 | 57 | + | + | Labral detachment, inflammation | Débridement, AMIC, FNO |
| 9 | 30 | F | Combined | 46 | 33 | 57 | 0 | − | Labral detachment, synovitis | Débridement, drillings, FNO |
| 10 | 31 | M | Cam | 72 | 31 | 44 | 0 | − | Labral detachment, synovitis, scope | Débridement, AMIC, FNO |
FAI = femoroacetabular impingement; LCA = lateral center-edge angle; PW = posterior wall sign; M = male; F = female; FNO = femoral neck osteochondroplasty; AMIC = autologous matrix-induced chondrogenesis.
After obtaining the patients’ histories, we had routinely examined each patient clinically for ROM and hip positions that reproduced discomfort. With the patient in the supine position, hip flexion, internal and external in flexion and extension, and the anterior impingement sign were assessed. In all patients we obtained supine AP pelvis, false profile, Dunn lateral plain radiographs, and MR arthrography for each patient. The radiographs were assessed for femoral morphology, acetabular morphology, and the MRI arthrogram was reviewed for osseous morphology, labral damage, and the presence of femoral and acetabular chondral lesions. Standard acetabular and femoral radiographic indices including center-edge angle, crossover sign, posterior wall sign, and alpha angle were recorded.
At the time of surgical dislocation, performed through a modified Gibson approach using a trochanteric flip osteotomy as described by Ganz et al. [6], the femoral head was dislocated. In addition to treating the femoral and acetabular deformity and any associated cartilage damage, the femoral lesion was measured across its greatest diameter and its position relative to the fovea and the depth of injury were recorded. We also noted the method used to treat each deformity. The lesions were of varying size, but were all localized to the posterosuperior femoral head adjacent to the fovea capitis (Table 2). Seven of 10 patients were treated by microfracture alone and three were treated using a second-generation bone marrow stimulation technique [14] that included marrow cells contained by a bioresorbable membrane. Each patient underwent a femoral head or neck osteochondroplasty as well as either a labral repair or débridement depending on the discretion of the treating surgeon. No patient had an acetabular rim resection to treat impingement. The choice of cartilage restoration technique was dependent on the prevailing technique used at each author’s institution at the time of the surgical dislocation.
Table 2.
Characteristics and management of femoral chondral defects
| Patient number | Femoral quadrant location | Lesion area (mm2) | Lesion dimension (mm) | History of subluxation | MRI identified | MRI finding | Management | Primary activity | Followup | Tegner-Lysholm |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | ps | 165 | 15 × 11 | No | Yes | Defect | MF | Tennis | 72 months | 9 |
| 2 | ps | 120 | 10 × 12 | Yes | No | No | MF | Power lifter | 24 months | 6 |
| 3 | ps/as | 513 | 27 × 19 | Yes | No | No | MF | Hurdler | 38 months | 6 |
| 4 | ps | 96 | 8 × 12 | Yes | Yes | Defect, edema | MF | American football | 20 months | 9 |
| 5 | ps | 150 | 10 × 15 | Yes | Yes | Defect, edema | MF | American football | 41 months | 9 |
| 6 | ps | 112 | 8 × 14 | No | Yes | Defect, cystic, edema | MF | Hockey goal tender | 12 months | 5 |
| 7 | ps | 180 | 2 × 2 with large cyst underneath, after unroofing defect 12 × 15 mm | No | Yes | Large cyst under small defect | AMIC | Butcher | 2 years | 7 |
| 8 | ps | 300 | 20 × 15 | No | Yes | Defect, edema | AMIC | Karate | 1 year | 9 |
| 9 | ps | 48 | 12 × 4 | No | Yes | Defect | MF | Ice skater | 2 years | 6 |
| 10 | ps | 164 | 2 × 2 with cyst, after unroofing 12 × 14 mm | No | Yes | Defect | AMIC | Soccer | No followup, but 2 years | 8 |
ps = posterosuperior; as = anterosuperior; MF = microfracture; AMIC = autologous matrix-induced chondrogenesis.
After surgery, patients were mobilized as soon as possible depending on the time of day that the surgery was completed. Patients were limited to toe-touch weightbearing for approximately 6 weeks to permit time for the cartilage repair to mature and to allow the trochanter to heal. For the first 6 weeks, therapy consisted of passive or actively assisted hip ROM exercises. After 6 weeks and radiographic confirmation of trochanteric union, progressive weightbearing was encouraged and patients were instructed, under physiotherapy supervision, in gluteal, tensor fascia lata, and lower extremity strengthening. Patients were permitted to begin to return to sport once hip abductor strength was deemed sufficient.
The patients were reviewed postoperatively at 2 weeks, 6 weeks, 12 weeks, 6 months, and 1 year. At each visit patients were examined and AP pelvis radiographs were obtained. We evaluated healing of the trochanter as well as any evidence of measurable asymmetric joint space narrowing that would be visible on an AP view of the hip. Tegner and Lysholm activity scale assessment was completed at 1-year followup.
Results
The lesion size ranged from 96 mm2 to 513 mm2 with a mean of 184 mm2. The lesion was located in the posterosuperior femoral head lateral and slightly posterior to the fovea in all 10 patients. All of the patients had femoral head-neck morphology consistent with cam-type deformity as described by Beck et al. [2]. Two patients had potential combined femoral and acetabular deformity consistent with cam and pincer mechanics. The alpha angle measured on the AP radiograph ranged from 38° to 75° (mean, 58°). The lateral center-edge angle range was 26° to 39° (mean, 33°). The crossover sign was present in seven and the posterior wall sign was present in six of the 10 patients. All six patients who had a posterior wall sign had a crossover sign; one patient with a crossover did not have a posterior wall sign. The alpha angle observed on lateral radiographs ranged from 46° to 79° (mean, 53°).
The femoral chondral defect was diagnosed preoperatively using contrast-enhanced MR arthrography in eight of 10 patients. In the two patients in whom the lesion was not identified preoperatively, the articular cartilage was extensively delaminated but remained in continuity with the adjacent healthy articular cartilage (Fig. 1). The remaining patients had full-thickness defects with healthy-appearing surrounding cartilage (Fig. 2). The most consistent MRI finding was a defect in the articular cartilage visible as a result of pooling of intraarticular contrast agent within a filling defect of articular cartilage (Fig. 3). Subchondral edema noted on T2-weighted sequences was located at the base of the chondral defect in five patients (Fig. 3). Cystic changes were observed on the MRI arthrogram preoperatively and confirmed pathologically in two patients.
Fig. 1.
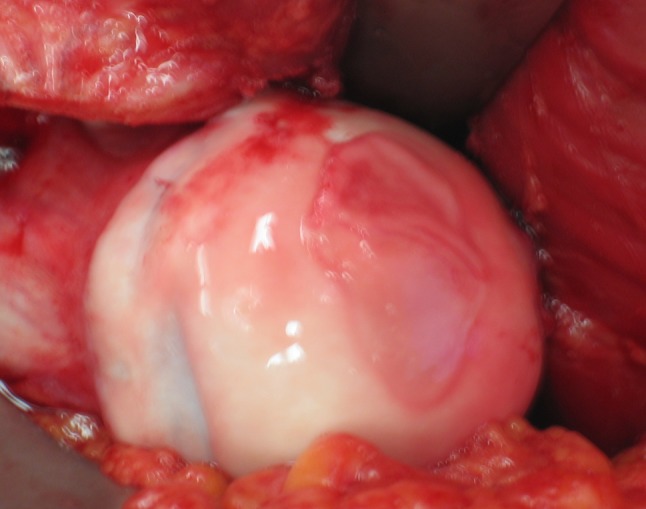
Left hip in patient 3, a 17 year old hurdler, shows extensively delaminated cartilage forming a blister. No pooling was noted on preoperative MRI-arthrogram. Note impingement trough at head neck junction.
Fig. 2.

Patient 4’s left parafoveal cartilage defect was diagnosed preoperatively by pooling present on MRI-arthrogram. Lesion is located anterosuperior to the fovea capitis. Note CAM morphology.
Fig. 3.
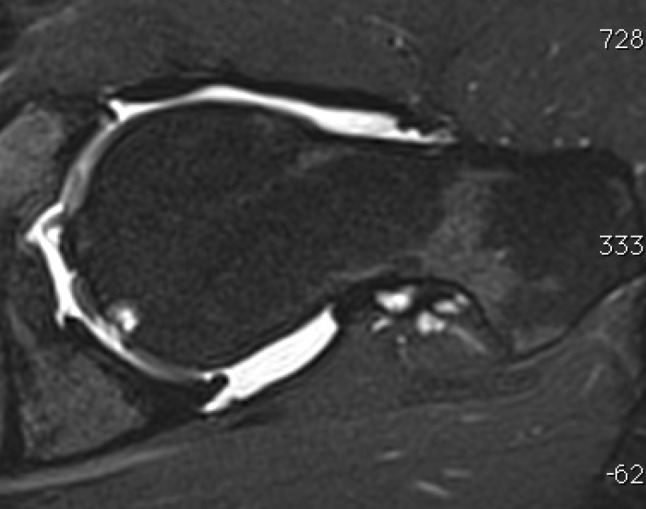
MRI of left hip in patient 6, a 26-year-old male goaltender, demonstrates articular defect and associated subchondral cyst formation.
The Tegner-Lysholm score at latest followup ranged from 5 to 9 (mean, 7.4). All patients were able to return to their preoperative level of function with the exception of Patient 6 whose contralateral hip precluded participation. At most recent followup, there was no obvious asymmetric joint space narrowing visible on an AP pelvis view in any of the patients when comparing the medial with the lateral femoral-acetabular joint space.
Discussion
Since the introduction of FAI as a unified concept, there have been multiple reports after both open and arthroscopic procedures concerning the pathologic changes that occur within the labrum, chondrolabral junction, and peripheral acetabular articular cartilage as a result of abnormal contact between the acetabular rim and the femoral head-neck junction [2]. The changes produced by cam-type impingement include varying degrees of labral detachment and peripheral articular cartilage delamination that are believed to be caused by complex forces produced by inclusion of the femoral deformity, characterized by prominence extending from the anterolateral head-neck junction into the inside of the acetabulum that has a smaller unaccommodating orifice [1, 16, 19]. Although cartilage damage to the head of the femur has been reported previously in athletes after subluxation or dislocation events, focal chondral defects differ from what has been described in previous reports and represent a rare manifestation of the complex pathomechanics associated with FAI. We describe the pathologic characteristics, MRI findings, and surgical management of another femoral-sided unique chondral lesion localized adjacent to the fovea found in a subcohort of young patients who perform activities that share hip motion associated with substantial force and rapid limb velocity.
We note limitations to our study. First, these patients were collected retrospectively during a period when clinical experience diagnosing and managing patients with FAI was evolving. Consequently, we are unable to identify clinical factors that can be used to differentiate patients with femoral articular lesions from other patients with FAI. Second, inconsistent preoperative clinical scoring data were collected and the number of patients involved is insufficient to recommend any particular cartilage restoration treatment technique. Third, both surgeons working in separate institutions with similar MRI protocols but different magnets collected the data. Because both magnets were 3 T and the protocols similar in each institution, there would be very little difference between generated images. Some variation in radiologic interpretation may exist depending on the radiologist’s experience. Fourth, the treatment method for the chondral lesion was based on the prevailing technique at each author’s institution and it is not possible to determine whether treatment of the impingement, the chondral defect, or both led to clinical improvement. Fifth, because the number of patients with femoral chondral lesions is small, collected over a period of time of changing FAI treatment, and inconsistent preoperative and postoperative clinical outcome scores were collected, comparisons to other cohorts treated only for impingement is not possible. Nevertheless, knowledge that femoral chondral defects can occur in patients with FAI is important because it is not a sign of end-stage arthrosis and does not preclude successful treatment of FAI in the concentric joint.
Although the 10 patients described in this report participated in different activities and vocations, each share common attributes of rapid, forceful, repetitive hip flexion. Understanding kinematic attributes described by Lamontagne et al. [10], Kennedy et al. [9], and Charbonnier et al. [4, 5], it is conceivable that these motions, performed in hips with restricted flexion, can induce shear stresses on the femoral head that can produce the pathologic changes reported here. Whether the specified motions produce shear stresses by causing transient subluxation or forceful nonconcentric motion on the femoral head remains uncertain. Our clinical findings are consistent with two reports that suggest the probability that impingement-induced transient subluxation or dislocation generates shear stresses that produced the chondral damage. Weaver et al. [23] reported femoral head nonarthrogram MRI findings in 11 collegiate and professional athletes who presented with groin pain. These femoral lesions were high intensity on T2-weighted and low intensity on T1-weighted images. Three patients in their study who underwent arthroscopy had osteochondral defects in the superior femoral head. They proposed either impaction or transient subluxation as potential mechanisms of injury to explain the MRI findings. Although two patients in our study did not have MRI-identified lesions, these patients had chondral delamination that was still in continuity with the adjacent attached cartilage, similar to a dermal blister. This suggests osseous MRI findings probably do not develop until the subchondral bone is exposed to synovial fluid. Moreover, the cystic changes noted beneath the subchondral bone plate were found only in patients with chronic chondral defects. Consistent with these findings, Philippon et al. [17] reported the arthroscopic findings in 14 professional athletes who had traumatic hip dislocations. Eight patients had femoral chondral defects and nine evidence of FAI; however, the locations of the lesions were not specified. Whereas the patients in the report of Philippon et al. had documented evidence of dislocation, our patients had femoral head pathologic changes but no history of frank dislocation. We hypothesize that the lesions reported by Philippon et al. were different and secondary to acute trauma to the femoral head rather to repetitive injury. In addition, Byrd [3] described four patients with cartilage defects within the hip after lateral impact. One patient had a femoral chondral defect located above the fovea capitis that was caused by a fall on the lateral hip. The lesion was ultimately treated by arthroscopic fragment excision. With the available kinematic and clinical data, it is possible to deduce that motions capable of producing forces similar to those that are part of a hip dislocation may partially explain the observed pathologic changes reported in our patients.
The focal chondral defects noted in our patients, especially those whose lesions were associated with cystic subchondral changes, are similar to global clinical pathologic and radiologic findings associated with end-stage arthrosis [20]. Nevertheless, the mean Tegner-Lysholm score at 29-month followup was 7.4, representing the capacity to participate in competitive-level athletics. We postulate that high-level function after treatment depends on continued joint congruency and a concentric joint. In contrast to patients with Tönnis Grade 2 arthrosis [21] in whom degeneration of articular cartilage leads to joint space narrowing and loss of congruence, our patients maintained symmetric joint spaces and concentric motion despite focal cartilage defects and the presence of subchondral cystic change. Similar subchondral cystic changes are observed in osteonecrosis of the femoral head [22]. When localized to a defined geographic location, intertrochanteric redirectional osteotomy may be useful for altering weightbearing characteristics across the hip to prevent subchondral collapse [7]. Although our patients had localized femoral head lesions that were potentially amenable to redirectional treatment, the restricted motion of these hips does not permit flexion, varus, or valgus redirection without worsening movement. Moreover, the central location of these lesions would have required extensive reorientation that would not have been surgically feasible.
The pathologic focal femoral head chondral lesions in this cross-sectional study illustrate the complexity of abnormal hip mechanics and the spectrum of associated chondral damage. Furthermore, despite the MRI appearance of a femoral chondral defect with or without cystic change, normalization of hip mechanics by surgical correction of impingement morphology in addition to treatment of the chondral defect should be considered in appropriate patients as an alternative to total joint arthroplasty.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at William Beaumont Hospital, Royal Oak, MI, USA; and the Schulthess Klinik, Zurich, Switzerland.
References
- 1.Anderson LA, Peters CL, Park BB, Stoddard GJ, Erickson JA, Crim JR. Acetabular cartilage delamination in femoroacetabular impingement. Risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am. 2009;91:305–313. doi: 10.2106/JBJS.G.01198. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 3.Byrd JW. Lateral impact injury. A source of occult hip pathology. Clin Sports Med. 2001;20:801–815. doi: 10.1016/S0278-5919(05)70286-6. [DOI] [PubMed] [Google Scholar]
- 4.Charbonnier C, Kolo FC, Duthon VB, Magnenat-Thalmann N, Becker CD, Hoffmeyer P, Menetrey J. Assessment of congruence and impingement of the hip joint in professional ballet dancers: a motion capture study. Am J Sports Med. 2011;39:557–566. doi: 10.1177/0363546510386002. [DOI] [PubMed] [Google Scholar]
- 5.Charbonnier C, Magnenat-Thalmann N, Becker CD, Hoffmeyer P, Menetrey J. An integrated platform for hip joint osteoarthritis analysis: design, implementation and results. Int J Comput Assist Radiol Surg. 2010;5:351–358. doi: 10.1007/s11548-010-0422-y. [DOI] [PubMed] [Google Scholar]
- 6.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 7.Ito H, Kaneda K, Matsuno T. Osteonecrosis of the femoral head. Simple varus intertrochanteric osteotomy. J Bone Joint Surg Br. 1999;81:969–974. doi: 10.1302/0301-620X.81B6.10037. [DOI] [PubMed] [Google Scholar]
- 8.Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004;429:262–271. doi: 10.1097/01.blo.0000144861.11193.17. [DOI] [PubMed] [Google Scholar]
- 9.Kennedy MJ, Lamontagne M, Beaulé PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait. Walking biomechanics of FAI. Gait Posture. 2009;30:41–44. doi: 10.1016/j.gaitpost.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 10.Lamontagne M, Kennedy MJ, Beaulé PE. The effect of cam FAI on hip and pelvic motion during maximum squat. Clin Orthop Relat Res. 2009;467:645–650. doi: 10.1007/s11999-008-0620-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leunig M, Beck M, Kalhor M, Kim YJ, Werlen S, Ganz R. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005;236:237–246. doi: 10.1148/radiol.2361040140. [DOI] [PubMed] [Google Scholar]
- 12.Leunig M, Mast NH, Impellizerri FM, Ganz R, Panaro C. Arthroscopic appearance and treatment of impingement cysts at femoral head-neck junction. Arthroscopy. 2012;28:66–73. doi: 10.1016/j.arthro.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 13.Leunig M, Podeszwa D, Beck M, Werlen S, Ganz R. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;418:74–80. doi: 10.1097/00003086-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Leunig M, Tibor LM, Naal FD, Ganz R, and Steinwachs R. Surgical Technique. Second-generation bone marrow stimulation via surgical dislocation to treat hip cartilage lesions. Clin Orthop Relat Res. 2012. In press. [DOI] [PMC free article] [PubMed]
- 15.Panzer S, Augat P, Esch U. CT assessment of herniation pits: prevalence, characteristics, and potential association with morphological predictors of femoroacetabular impingement. Eur Radiol. 2008;18:1869–1875. doi: 10.1007/s00330-008-0952-7. [DOI] [PubMed] [Google Scholar]
- 16.Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778–785. doi: 10.1148/radiol.2403050767. [DOI] [PubMed] [Google Scholar]
- 17.Philippon MJ, Kuppersmith DA, Wolff AB, Briggs KK. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy. 2009;25:169–174. doi: 10.1016/j.arthro.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Pitt MJ, Graham AR, Shipman JH, Birkby W. Herniation pit of the femoral neck. AJR Am J Roentgenol. 1982;138:1115–1121. doi: 10.2214/ajr.138.6.1115. [DOI] [PubMed] [Google Scholar]
- 19.Pollard TC, McNally EG, Wilson DC, Wilson DR, Mädler B, Watson M, Gill HS, Carr AJ. Localized cartilage assessment with three-dimensional dGEMRIC in asymptomatic hips with normal morphology and cam deformity. J Bone Joint Surg Am. 2010;92:2557–2569. doi: 10.2106/JBJS.I.01200. [DOI] [PubMed] [Google Scholar]
- 20.Taljanovic MS, Graham AR, Benjamin JB, Gmitro AF, Krupinski EA, Schwartz SA, Hunter TB, Resnick DL. Bone marrow edema pattern in advanced hip osteoarthritis: quantitative assessment with magnetic resonance imaging and correlation with clinical examination, radiographic findings, and histopathology. Skeletal Radiol. 2008;37:423–431. doi: 10.1007/s00256-008-0446-3. [DOI] [PubMed] [Google Scholar]
- 21.Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. New York, NY, USA: Springer; 1987. [Google Scholar]
- 22.Watson RM, Roach NA, Dalinka MK. Avascular necrosis and bone marrow edema syndrome. Radiol Clin North Am. 2004;42:207–219. doi: 10.1016/S0033-8389(03)00166-0. [DOI] [PubMed] [Google Scholar]
- 23.Weaver CJ, Major NM, Garrett WE, Urbaniak JE. Femoral head osteochondral lesions in painful hips of athletes: MR imaging findings. AJR Am J Roentgenol. 2002;178:973–977. doi: 10.2214/ajr.178.4.1780973. [DOI] [PubMed] [Google Scholar]


