Abstract
Background
Isolated acetabular revisions using standard cups are at risk of dislocation. The introduction of a nonconstrained dual-mobility cup was designed to improve prosthetic stability without increasing loosening rates, but it is unclear whether the risk of dislocation is reduced.
Questions/purposes
We therefore determined: (1) if the rate of dislocation in isolated acetabular revisions is lower with a dual-mobility cup, (2) implant survival, (3) patient function, and (4) radiographic incidence of migration, loosening, and osteolysis.
Methods
We prospectively followed 33 selected patients who underwent isolated acetabular revisions with a minimum of 2 years’ followup (mean, 3 years; range, 2–5 years). In 24 patients a stainless steel dual-mobility cup was cemented into an antiprotrusio cage, whereas in nine we used a hyaluronan dual-mobility revision cup with a foramen hook and superior and posterior flanges screw fixations. We determined Harris hip (HHS) and WOMAC scores and examined radiographs for migration, loosening, and osteolysis.
Results
There were no dislocations. Survivorship rates of the femoral and acetabular components were 97% at 5 years; the rerevision rate for any reason was 3%. At last followup, the mean HHS increased from 48 points preoperatively to 86 points. No patients had progressive osteolysis, component migration, or loosening on radiographs.
Conclusion
In this select group of isolated acetabular revisions, our data suggest the use of a dual-mobility cup reduced the risk of dislocation without increasing loosening from 2 to 5 years.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Isolated acetabular revision is indicated when an acetabular implant is associated with pain, reduced function, instability, or loosening while the femoral implant is stable and in a satisfactory position [6, 22]. Approximately 15% of revision hip arthroplasties are performed for isolated failure of the acetabular component [9, 30]. However, isolated acetabular revisions reportedly have associated rates of postoperative dislocation ranging from 8% to 20% in part because the presence of the retained femoral component can limit the options available for head size, restoration of limb length, offset, and soft tissue tension [1, 14, 15, 25, 36, 38]. However, combined femoral and acetabular revision is associated with increased complication rate, surgical time, blood loss, and cost.
To address this risk, surgeons have developed jumbo femoral heads [3] or constrained acetabular liners [7, 16–18, 20, 29]. Although constrained liners have been used to treat recurrent dislocation and intraoperative instability, failure rates ranging from 40% to 100% have been reported [16, 31].
The dual-mobility concept was introduced in the mid-1970s to reduce the rate of postoperative dislocation in primary surgery. With the dual-mobility cup, the prosthetic head is mobile in a retentive polyethylene (PE), which is free to move in a metal-backed cup [21, 35]. The dual-mobility biomechanical concept is simple. The first motion occurs between the inner femoral head and the inner concave surface of the PE bearing, and the secondary motion occurs between the PE bearing and the acetabular cup when larger ROM is required. The bearing acts as a large femoral head articulating in the metal cup [35]. Advantages of dual mobility are greater ROM and increased stability of the implant. Philippot et al. [34] reported that the cumulative survival rate of the dual articulation acetabular cup, using surgical revision for aseptic loosening as the end point, was 95.9% ± 4.1% at 18 years postoperatively in primary cases. Although the dual-mobility concept is associated with a low rate of dislocation in primary THA, it is unclear whether this concept will reduce dislocations in isolated acetabular revision surgery.
We therefore determined: (1) if the rate of dislocation in isolated acetabular revisions is lower with a dual-mobility cup, (2) implant survival, (3) patient function, and (4) radiographic incidence of migration, loosening, and osteolysis.
Patients and Methods
We prospectively followed 33 patients who had isolated acetabular revisions with a dual-mobility cup at our institution from June 2006 to March 2009. The indications for revision with the dual-mobility cup were: (1) isolated acetabular revision for aseptic loosening or malposition, and (2) a well-fixed and well-positioned femoral component. The contraindications were: (1) revision for septic loosening, and (2) revision required for both components. During this time, all patients needing isolated acetabular revision were treated with this technique. There were 18 (55%) women and 15 (45%) men and their average age at the time of the index revision was 69 years (range, 51.3–82.4 years). Twenty procedures were performed on the left side and 13 on the right side. The mean interval from THA to revision surgery was 9.4 years (range, 2–18 years). The mean American Society of Anesthesiologists score before the conversion procedure was 3.17 [32, 39]. The preoperative diagnoses were aseptic loosening in 32 hips and malposition of the acetabular component in one. Eleven had cemented acetabular components, 10 of which were all-polyethylene and one was metal-backed. All cemented components were revised for aseptic loosening. Twenty-two acetabular components were cementless (17 porous-coated, three hydroxyapatite-coated, and two threaded). Twenty-one of the cementless components were revised for aseptic loosening and one was malpositioned. The retained femoral components were 27 modular femoral components and six monolithic (monoblock) femoral components with a fixed head size and neck length; in four cases, the monoblock head was 22 mm, and in two cases it was 32 mm. The minimum followup was 2 years (mean, 3.3 years; range, 2–5 years). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
Acetabular bone deficiencies were classified according to the classification described by Paprosky and Magnus [33] using preoperative radiographs and the findings at surgery. Grade I deficiencies were found in one hip (3%), Grade II A in seven (21%), Grade II B in nine (28%), Grade II C in five (15%), Grade III A in seven (21%), and Grade III B in four (12%).
The direct lateral approach [12] was performed in 30 hips, whereas in three hips, an extensile anterior approach [10] was used to gain free access to the iliac bone. All acetabular cups, liners, and screws were removed. Pelvic bony defects were treated with fresh frozen morselized allograft in 30 (91%), whereas no bone augmentation was used in three (9%). The acetabular margins were defined and the cup always was positioned as close to the center of hip rotation as possible. In 24 cases, a stainless steel dual-mobility cup (Avantage®; Biomet, Warsaw, IN, USA) (Fig. 1) was cemented into an antiprotrusio cage screwed into the bone (Contour®; Smith & Nephew, Memphis, TN, USA) (Fig. 2) using antibiotic-loaded bone cement (Palacos with gentamicin; Merck, Darmstadt, Germany) (Fig. 3). In nine cases, we used an hydroxyapatite-coated stainless steel dual-mobility revision cup (Avantage® Revision; Biomet Warsaw, IN, USA) with three superior pelvic flanges for screw fixation and a foramen hook (Fig. 4).
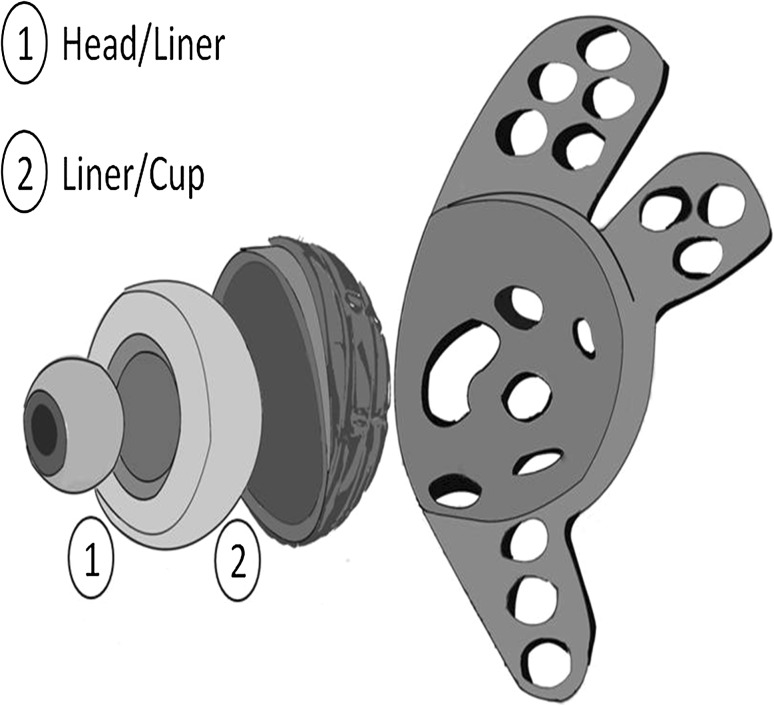
Fig. 1.

The stainless steel dual-mobility cup (Avantage®; Biomet, Warsaw, IN, USA) that is cemented in an antiprotrusio cage (Contour®; Smith & Nephew, Memphis, TN, USA) is shown.
Fig. 2.
The diagram of dual-mobility cup shows (1) articulation between the head and liner and (2) articulation between the liner and cup. The cup must be cemented into an antiprotrusio cage.
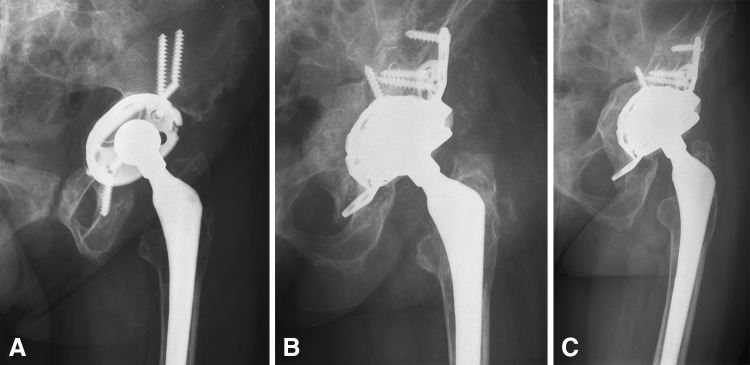
Fig. 3A–C.
A 65-year-old woman had loosening of an oval cementless cup. (A) Her preoperative AP view shows the massive acetabular defect. (B) The immediate postoperative AP view shows the revision THA with an antiprotrusio cage and a cemented dual-mobility cup. (C) A radiograph taken 4 years after revision shows excellent bone ingrowth without evidence of loosening.
Fig. 4.

An hydroxyapatite-coated stainless steel dual-mobility revision cup (Avantage® Revision; Biomet Warsaw, IN, USA) is shown.
In case of monoblock femoral components, the dual-mobility cup was assembled in situ (Fig. 5). Femoral component version was noted at the time of revision, and revision acetabular components were positioned to obtain a total of approximately 40° anteversion. Intraoperatively, stability was examined by observing for dislocation while the hip was put through the full ROM possible and by observing for displacement while applying traction to the limb.
Fig. 5A–C.
A 73-year-old woman had loosening of a Charnley cemented cup. (A) Her preoperative AP view is shown. (B) An intraoperative photograph shows how the polyethylene of the dual-mobility cup was assembled in situ. (C) A postoperative AP view taken 2 years after revision is shown.
Postoperative management included bed rest for 5 days with the leg in abduction and then, depending on intraoperative bone quality and the resulting reconstruction of the acetabulum, the patients were allowed to walk with partial weightbearing using crutches or a walker, with full weightbearing after 2 months. Antibiotic prophylaxis (15 mg/kg vancomycin every 6 hours) was discontinued at 72 hours. Subcutaneous low-molecular-weight heparin was used as a routine preventive measure for thromboembolic problems until the patients were fully mobile.
Routine clinical and radiographic examinations were performed preoperatively, and postoperatively at 3 and 6 weeks, 3 and 6 months, 1 year, and then annually. The clinical evaluation was performed using the Harris hip score (HHS) [13] and WOMAC score [19]. Complications were recorded according to the classification of Dindo et al. [8]. Instability of the hip was defined as a dislocation or a subluxation. Subluxation was defined as perception by the patient of an abnormal hip movement accompanied by an audible thud or clunk of the hip often associated with pain.
Two of the authors (RC, CC) evaluated all radiographs for osteolysis, inclination of the acetabular component, stability of the acetabular and femoral components, and hip center correction. The interobserver measurements errors of osteolysis, hip center of rotation, and degree of inclination of the cup were 2%, 3%, and 2%, respectively. Loosening of the socket was defined as cup migration exceeding 3 mm, angular rotation exceeding 3°, or a continuous radiolucent line wider than 2 mm. Measurement of preoperative and postoperative center of hip rotation was estimated by measuring the position of the implant with respect to fixed pelvic landmarks. Two reference lines were drawn: one horizontal reference line between the inferior margins of the teardrops was used to evaluate vertical position and migration and a perpendicular line tangential to the medial aspect of the teardrop was drawn to measure medial position and migration [28]. Parameters investigated on the femoral side included progression of radiolucent lines according to the seven zones described by Gruen et al. [11] and subsidence of the stem. Loosening of the stem was defined according to the criteria of Barrack et al. [2]. Definite, probable, and potential evidence of loosening were considered in this study. Periprosthetic cystic or scalloped lesions exceeding 2 mm in diameter that had not been noted on the immediate postoperative radiograph were defined as osteolysis. Heterotopic ossification was evaluated at the last followup and classified according to Brooker et al. [5].
A Kaplan-Meier survival analysis was performed to calculate the survival curve of the dual-mobility cup. The Wilcoxon signed rank test was used to compare preoperative versus postoperative values in nonparametric values as the HHS, WOMAC score, and hip center of rotation. All statistical analyses were performed using StataTM Version 6.0 (College Station, TX, USA).
Results
There were no acute postoperative complications and early or late dislocations.
The survivorship rate of the femoral and acetabular components was 97% at 5 years (95% CI, 82%–98%). Revision arthroplasty was performed in one hip for infection at 6 months, treated with successful two-stage resection and reimplantation with a porous tantalum cup (Zimmer, Warsaw, IN, USA) and a modular tapered revision stem (MP, Waldemar Link, Hamburg, Germany).
At last followup, the average HHS improved (p = 0.002) from 48 preoperatively (range, 32–68) to 86 (range, 66–95) postoperatively. The average total WOMAC score improved (p ≤ 0.001) from 79 (range, 41–96) to 19 (range, 8–37) postoperatively.
The vertical distance of hip center from the interteardrop line was 33 mm (range, 12–53 mm) preoperative and 18 mm (range, 3–33 mm) postoperative (p = 0.001). The horizontal distance was 17 mm (range 3–29 mm) lateral to the medial aspect of the teardrop preoperative and 34 mm (range 21–41 mm) lateral to the same landmark postoperative (p = .0009). The preoperative existing vertical and medial migration of the center of rotation of the surgically treated hip was substantially corrected after surgery. Of the acetabular components, 18 (55%) had no radiolucent line, seven (21%) had a radiolucent line in Zone I, five (15%) in Zone III, and three (9%) in Zones I and III. In all these hips, the radiolucent lines were less than 1 mm in thickness and were nonprogressive. The 32 (97%) femoral components that were not revised were well fixed, and there was no potential or pending revision. We did not identify any patients with progressive femoral osteolysis, component migration, or loosening.
Discussion
Controversy exists regarding whether to remove a well-fixed femoral component at the time of revision of a failed acetabular component [9, 22]. Obvious advantages of isolated acetabular revisions include shorter surgical time, less blood loss, and fewer complications. Disadvantages of leaving a stable femoral component in place are a more technically challenging operation owing to limitations of exposure associated with an intact femoral component and an increased rate of postoperative dislocations, because retention of the femoral component is associated with difficulty in balancing the soft tissues and decreases the ability to construct a stable hip. We therefore determined: (1) if the rate of dislocation in isolated acetabular revisions is lower with a dual-mobility cup, (2) implant survival, (3) patient function, and (4) radiographic incidence of migration, loosening, and osteolysis.
There are limitations to this study. First, we had a small number of patients (33). There are few series of isolated acetabular revisions reported in the literature and their numbers are similar to ours, ranging from 13 to 95 patients [4, 6, 26, 27]. Second, we had relatively short-term followup after revision surgery. However, when analyzing dislocation in hip revision, it must be considered that approximately 90% of the dislocations occur within 3 months of surgery [4]. Third, we used two types of acetabular cups. However, although different in anchoring to the bone, the two implants share the same geometry and biomechanics of the dual-mobility system.
We observed no dislocations using this technique in isolated acetabular revisions. There are several reports which documented a higher incidence of dislocation compared with revision of both components (Table 1). One series of 211 hip revisions [36] had a dislocation rate of 20% after isolated acetabular revisions compared with an 8% rate after revision of both components. Similarly another series of 63 isolated acetabular revisions followed for a minimum of 60 months had a dislocation rate of 8% [14]. Recently Schneider et al. [37] had 10 cases of dislocation (10.4%) in a series of 96 revisions with a reconstruction cage and a cemented dual-mobility cup. Langlais et al. [21] reported a dislocation rate of 1.1% at 5 years after revising both components (Table 2). Massin and Besnier [27] prospectively followed 23 THA revisions involving acetabular component replacement with the use of a cementless dual-mobility cup. At last followup (range, 2–10 years), there was one isolated dislocation and one recurrent dislocation associated with a loose greater trochanter nonunion. Leiber-Wackenheim et al. [23], in 59 recurrent THA dislocations treated by a cementless dual-mobility cup, reported a dislocation rate of 1.7% with a minimum followup of 6 years (mean, 8 years; range, 6–11 years) without loosening or migration. Levine et al. [24], using a similar tripolar construct, concluded that it was effective in eliminating or preventing instability in 93% of the complex cases treated.
Table 1.
Isolated acetabular revision
| Study | Number of revisions | Followup (years)* | Cup | HHS* | Dislocation | Aseptic loosening cup | Pelvic osteolysis | Survival |
|---|---|---|---|---|---|---|---|---|
| Jamali et al. [14] | 95 | 10.8 (5–17.3) | NC | 81 (31–100) | 8% | 5 % | 4% | 90.5% at 10 years |
| Jones and Lachiewicz [15] | 69 | 6 (1–18) | NC | 83 (31–100) | 20% | 2% | 7% | 95% at 12 years |
| Poon and Lachiewicz [36] | 38 | 4 (2–10) | NC | 88 (NA) | 8% | 0% | NA | 95% at final followup |
| Lawless et al. [22] | 42 | 6.4 (2–13) | NC | 80 (40–99) | 0% | 7.3% | 2% | 88% at final followup |
| Della Valle et al. [7] | 55 | 3.6 (2–6.7) | C | NA | 16% | 0% | NA | NA |
| Khan et al. [17] | 34 | 3 (2.2–4.8) | C | 69 | 3% | 8.4% | NA | 88.2% at final followup |
| Current study | 33 | 3.3 (2–5) | DM | 86 (66–95) | 0% | 0% | 0% | 97% at 5 years |
* Ranges shown in parentheses; NC = Nonconstrained; C = Constrained; DM = Dual-mobility; HHS = Harris hip score; NA = not available.
Table 2.
Dual-mobility cup in total hip revisions
| Study | Number of revisions | Cup | Type of revision | Followup (years)* | Dislocation |
|---|---|---|---|---|---|
| Langlais et al. [21] | 85 | Medial Cup DMC | Total 85 | 3 (2–5) | 1 of 85 (1.1%) |
| Massin and Besnier [27] | 23 | Collégia™ cup | Total 16 Isolated 7 | 4.5 (2–10) | 2 of 23 (8.7%) |
| Leiber-Wackenheim et al. [23] | 59 | Novae-1™ cup | Isolated 59 | 8 (6–11) | 1 of 59 (1.7%) |
| Schneider et al. [37] | 96 | Novae-1™ cup | NA | 3.4 (1 month to 8.4 years) | 10 of 96 (10.4%) |
| Current study | 33 | Avantage® | Isolated 33 | 3.3 (2–5) | 0 (0%) |
* Ranges shown in parentheses; NA = not available.
The survivorship rates of our femoral and acetabular components were 97% at 5 years with a rerevision rate for any reason of 3%. Langlais et al. [21] reported a cup survival rate of 94.6% in 85 cemented dual-mobility cups for THA revisions in patients at high risk of dislocation (Table 2). In their followup of 2 to 5 years, the cemented dual-mobility cup had better survival than constrained cups in hips at risk of dislocation and with recurrent loosening. Schneider et al. [37] reported a survival rate of 95.6% at 8 years with 10 cases of dislocation (10.4%) in a series of 96 revisions with a reconstruction cage and a cemented dual-mobility cup.
In the study group as a whole, there were symptomatic relief and functional improvement after revision and the HHS increased by a mean of 38 points to a mean of 86 points. This compares with a range of 69 to 88 reported in previous studies (Table 1).
We found no patients with osteolysis, migration, or loosening. Comparing our data with published data, the incidence of aseptic loosening for the acetabular cup has reported ranges from 0% to 8.4% and the incidence of pelvic osteolysis ranges from 0% to 7% (Table 1).
In this select group of isolated acetabular revisions, our 2- to 5-year data suggest the use of a dual-mobility cup was successful to reduce the risk of dislocation by increasing functional diameter of the head without increasing loosening and that acetabular revision could be performed without removing or revising a stable, well-fixed femoral component.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
References
- 1.Amstutz HC, Duff MJ, Beaule PE. Prevention and treatment of dislocation after total hip replacement using large diameter balls. Clin Orthop Relat Res. 2004;429:108–116. doi: 10.1097/01.blo.0000150310.25603.26. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Mulroy RD, Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty: a 12-year radiographic review. J Bone Joint Surg Br. 1992;74:385–389. doi: 10.1302/0301-620X.74B3.1587883. [DOI] [PubMed] [Google Scholar]
- 3.Beaule PE, Schmalzried TP, Udomkiat P, Amstutz HC. Jumbo femoral head for the treatment of recurrent dislocation following total hip replacement. J Bone Joint Surg Am. 2002;84:256–263. doi: 10.2106/00004623-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Blom AW, Astle L, Loveridge J, Learmonth ID. Revision of an acetabular liner has a high risk of dislocation. J Bone Joint Surg Br. 2005;87:1636–1638. doi: 10.1302/0301-620X.87B12.16349. [DOI] [PubMed] [Google Scholar]
- 5.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 6.Chen XD, Waddell JP, Morton J, Schemitsch EH. Isolated acetabular revision after total hip arthroplasties: results at 5–9 years of follow up. Int Orthop. 2005;29:277–280. doi: 10.1007/s00264-005-0674-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Della Valle CJ, Chang D, Sporer S, Berger RA, Rosenberg AG, Paprosky WG. High failure rate of a constrained acetabular liner in revision total hip arthroplasty. J Arthroplasty. 2005;20(7 suppl 3):103–107. doi: 10.1016/j.arth.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fukui K, Kaneuji A, Sugimori T, Ichiseki T, Kitamura K, Matsumoto T. Should the well-fixed, uncemented femoral components be revised during isolated acetabular revision? Arch Orthop Trauma Surg. 2011;131:481–485. doi: 10.1007/s00402-010-1152-x. [DOI] [PubMed] [Google Scholar]
- 10.Glassman AH. Exposure for revision: total hip replacement. Clin Orthop Relat Res. 2004;420:39–47. doi: 10.1097/00003086-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Gruen TA, McNeice GM, Amstutz HC. Modes of failure of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 12.Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br. 1982;64:17–19. doi: 10.1302/0301-620X.64B1.7068713. [DOI] [PubMed] [Google Scholar]
- 13.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 14.Jamali AA, Dungy DS, Mark A, Schule S, Harris WH. Isolated acetabular revision with use of the Harris-Galante cementless component. J Bone Joint Surg Am. 2004;86:1690–1697. doi: 10.2106/00004623-200408000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Jones CP, Lachiewicz PF. Factors influencing the longer-term survival of uncemented acetabular components used in total hip revisions. J Bone Joint Surg Am. 2004;86:342–347. doi: 10.1302/0301-620X.86B6.15000. [DOI] [PubMed] [Google Scholar]
- 16.Khan RJ, Fick D, Alakeson R, Haebich S, Cruz M, Nivbrant B, Wood D. A constrained acetabular component for recurrent dislocation. J Bone Joint Surg Br. 2006;88:870–876. doi: 10.1302/0301-620X.88B7.17644. [DOI] [PubMed] [Google Scholar]
- 17.Khan RJ, Fick D, Alakeson R, Li MG, Nivbrant B, Wood D. The constrained acetabular component for hip instability. J Arthroplasty. 2007;22:377–382. doi: 10.1016/j.arth.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 18.Khoury JI, Malkani AL, Adler EM, Markel DC. Constrained acetabular liners cemented into cages during total hip revision arthroplasty. J Arthroplasty. 2010;25:901–905. doi: 10.1016/j.arth.2009.08.012. [DOI] [PubMed] [Google Scholar]
- 19.Klassbo M, Larsson E, Mannevik E. Hip disability and osteoarthritis outcome score. An extension of the Western Ontario and McMaster Universities Osteoarthritis Index. Scand J Rheumatol. 2003;32:46–51. doi: 10.1080/03009740310000409. [DOI] [PubMed] [Google Scholar]
- 20.Lachiewicz PF, Kelley SS. The use of constrained components in total hip arthroplasty. J Am Acad Orthop Surg. 2002;10:233–238. doi: 10.5435/00124635-200207000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Langlais FL, Ropars M, Gaucher F, Musset T, Chaix O. Dual mobility cemented cups have low dislocation rates in THA revisions. Clin Orthop Relat Res. 2008;466:389–395. doi: 10.1007/s11999-007-0047-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lawless BM, Healy WL, Sharma S, Iorio R. Outcomes of isolated acetabular revision. Clin Orthop Relat Res. 2010;468:472–479. doi: 10.1007/s11999-009-1104-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leiber-Wackenheim F, Brunschweiler B, Ehlinger M, Gabrion A, Merl P. Treatment of recurrent THR dislocation using of a cementless dual-mobility cup: a 59 cases series with a mean 8 years’ follow-up. Orthop Traumatol Surg Res. 2011;97:8–13. doi: 10.1016/j.otsr.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 24.Levine BR. Della Valle CJ, Deirmengian CA, Breien KM, Weeden SH, Sporer SM, Paprosky WG. The use of a tripolar articulation in revision total hip arthroplasty. J Arthroplasty. 2008;23:1182–1188. doi: 10.1016/j.arth.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 25.Livermore J, Ilstrup D, Morrey B. Effect of femoral head size on wear of the polyethylene acetabular component. J Bone Joint Surg Am. 1990;72:518–528. [PubMed] [Google Scholar]
- 26.Manning DW, Ponce BA, Chiang PP, Harris WH, Burke DW. Isolated acetabular revision through the posterior approach: short-term results after revision of a recalled acetabular component. J Arthroplasty. 2005;20:723–729. doi: 10.1016/j.arth.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 27.Massin P, Besnier L. Acetabular revision of total hip arthroplasty using a press-fit dual mobility cup. Orthop Traumatol Surg Res. 2010;96:9–13. doi: 10.1016/j.otsr.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 28.Massin P, Schmidt L, Engh CA. Evaluation of cementless acetabular component migration: an experimental study. J Arthroplasty. 1989;4:245–251. doi: 10.1016/S0883-5403(89)80020-8. [DOI] [PubMed] [Google Scholar]
- 29.McCarthy JC, Lee JA. Constrained acetabular components in complex revision total hip arthroplasty. Clin Orthop Relat Res. 2005;441:210–215. doi: 10.1097/01.blo.0000194069.15086.1b. [DOI] [PubMed] [Google Scholar]
- 30.Moskal JT, Shen FH, Brown TE. The fate of stable femoral components retained during isolated acetabular revision: a six-to-twelve-year follow-up study. J Bone Joint Surg Am. 2002;84:250–255. doi: 10.2106/00004623-200202000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Noble PC, Durrani SK, Usrey MM, Mathis KB, Bardakos NV. Constrained cups appear incapable of meeting the demands of revision THA. Clin Orthop Relat Res. 2011 Dec 17. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 32.Owens WB, Felts JA, Spritznagel EL. ASA physical status classification: a study of consistency of ratings. Anaesthesiology. 1978;49:239–243. doi: 10.1097/00000542-197810000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Paprosky WG, Magnus RE. Principles of bone grafting in revision total hip arthroplasty: acetabular technique. Clin Orthop Relat Res. 1994;298:147–155. [PubMed] [Google Scholar]
- 34.Philippot R, Camilleri JF, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009;33:927–932. doi: 10.1007/s00264-008-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Philippot R, Farizon F, Camilleri JP, Boyer B, Derhi G, Bonnan J, Fessy MH, Lecuire F. [Survival of dual mobility socket with a mean 17 years follow-up] [in French] Rev Chir Orthop Reparatrice Appar Mot. 2008;94:43–48. doi: 10.1016/j.rco.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 36.Poon ED, Lachiewicz PF. Results of isolated acetabular revisions: the fate of the unrevised femoral component. J Arthroplasty. 1998;13:42–49. doi: 10.1016/S0883-5403(98)90074-2. [DOI] [PubMed] [Google Scholar]
- 37.Schneider L, Philippot R, Boyea B, Farizon F. Revision total hip arthroplasty using a reconstruction cage device and a cemented dual mobility cup. Orthop Traumatol Surg Res. 2011;97:807–813. doi: 10.1016/j.otsr.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 38.Tanzer M, Drucker D, Jasty M. Revision of the acetabular component with an uncemented Harris-Galante porous-coated prosthesis. J Bone Joint Surg Am. 1992;74:987–994. [PubMed] [Google Scholar]
- 39.Wolters U, Wolf T, Stutzer H, Schroder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996;77:217–222. doi: 10.1093/bja/77.2.217. [DOI] [PubMed] [Google Scholar]