Abstract
The aim of this study was to compare safety and efficacy of 4 homogenous overlapping drug-eluting stents (DES) in acute myocardial infarction (AMI) patients. We selected 1,349 consecutive patients (62.1 ± 14.9 yr, 69.4% male) who received homogenous overlapping DESs in diffuse de novo coronary lesions from Korea Acute Myocardial Infarction Registry from April 2006 through September 2010. They were divided into 4 groups based on type of DES implanted - Paclitaxel (PES), Sirolimus (SES), Zotarolimus (ZES) and Everolimus (EES)-eluting stents. Primary endpoint was 12-month MACE. We also studied EES versus other DESs (PES + SES + ZES). Mean stent length was 26.2 ± 7.5 mm and mean stent diameter was 3.1 ± 0.4 mm. Average number of stents used per vessel was 2.2 ± 0.5. Incidence of major adverse cardiac events (MACE) in PES, SES, ZES, and EES groups were 9.5%, 9.2%, 7.5%, and 3.8%, respectively (P = 0.013). In EES group, overall MACE and repeat revascularization were lowest, and no incidence of stent thrombosis was observed. Non-fatal MI was highest in PES, almost similar in SES and EES with no incidence in ZES group (P = 0.044). Cox proportional hazard analysis revealed no differences in the incidence of primary endpoint (P = 0.409). This study shows no significant differences in 12-month MACE among 4 groups.
Keywords: Drug-Eluting Stents, Myocardial Infarction, Coronary Angioplasty
INTRODUCTION
Drug-eluting stents (DES) substantially reduce the risk of restenosis and target lesion revascularization (TLR) compared with bare metal stents (BMS), particularly in complex coronary disease (1). Long lesions account for approximately 10% of contemporary percutaneous coronary intervention (PCI) cases, and present specific challenges for stenting with DES. Data from randomized controlled trials and large observational registries highlight the increased risk of restenosis with longer lesions, and demonstrate a significant reduction in restenosis and target vessel revascularization (TVR) rates with DES use (2-5). As a result, use of DES in diffuse long lesions has become standard clinical practice, supported by international guidelines (6-9). Multiple overlapping stents are often unavoidable to treat long diffuse lesions owing to excessive lesion length, edge dissection, or incomplete stent coverage. At the present time there is limited information about the safety and efficacy of overlapping DES in treating acute myocardial infarction (AMI) patients with severe diffuse coronary lesions. Experimental studies raised concerns regarding the safety and efficacy of overlapping DES because of the increased density of polymer, drug, and stent material (10, 11). To further pursue this interesting subject we conducted this retrospective study to examine the clinical outcomes of overlapping DESs and compared 4 most commonly used types of homogenous DES - Paclitaxel-eluting stents (PES), Sirolimus-eluting stents (SES), Zotarolimus-eluting stents (ZES) and Everolimus-eluting stents (EES).
MATERIALS AND METHODS
This is a clinical analysis that was carried out in The Heart Center of Chonnam National University Hospital, Gwangju, Korea.
Ethics statement
The permission to carry out the study was obtained from the hospital authorities (Institutional Review Board number 05-49, I-2008-01-009) and written informed consent was taken from all patients.
Korea Acute Myocardial Infarction Registry
The Korea Acute Myocardial Infarction Registry (KAMIR) is a prospective, multicenter, observational registry designed to examine current epidemiology in hospital management and outcome of patients with AMI in Korea in commemoration of the 50th anniversary of the Korean Circulation Society. The registry included 52 community and university hospitals for primary PCI with 1-yr clinical follow up. Data was collected at each site by a well-trained study coordinator based on standardized protocol (12, 13).
Study population
Patients were enrolled in the registry after admission to participating hospitals with a suspected diagnosis of AMI. Patients' medical documents were used to note the demographic data, clinical characteristics and relevant laboratory results.
A total number of 14,329 patients with AMI (ST-segment elevation MI and non-ST segment elevation MI) undergoing PCI from April 2006 through September 2010 were assessed in this study. We selected 1,349 consecutive patients who received homogenous overlapping stents in diffuse de novo coronary lesions and studied their 12-month clinical outcomes (follow-up rate 76.6%). Patients who received BMSs or 2 different types of overlapping DESs were excluded from this study. We divided these patients into 4 groups based on the type of homogenous DESs implanted-Paclitaxel-eluting stents, PES group (Taxus, Boston Scientific Corporation, Natick, MA, USA), n = 247; Sirolimus-eluting stents, SES (Cypher, Cordis Corporation, Miami Lakes, FL, USA), n = 280; Zotarolimus-eluting stents, ZES (Endeavor, Medtronic Vascular, Santa Rosa, CA, USA), n = 412 and Everolimus-eluting stents, EES (Xience V/Promus Element), n = 410. The number of stents implanted, the type of DES used, and the degree of stent overlap were at the operator's discretion.
Study definitions and clinical endpoints
A final diagnosis of AMI was made according to the European Society of Cardiology/American College of Cardiology diagnostic criteria of AMI (14). Hypertension was defined as systolic blood pressure > 140 mmHg and/or diastolic blood pressure > 90 mmHg at rest, at repeated measurements or treatment with anti-hypertensive medications. Diabetes mellitus (DM) was defined as use of oral hypoglycaemic agent or insulin to lower blood glucose levels. Hyperlipidemia was defined as a total cholesterol level > 200 mg/dL or treatment with a lipid-lowering agent. CAD was defined as history of MI, revascularization procedure or obstructive CAD.
Peripheral blood samples were obtained using direct venipuncture. Blood samples were centrifuged and serum was removed and stored at a temperature of -70℃ until the assay could be performed for proteins and sugar. Absolute creatine kinase-MB levels were determined by radioimmunoassay (Dade Behring, Inc., Miami, FL, USA). Cardiac specific troponin I levels were measured by a paramagnetic particle, chemiluminescent immunoenzymatic assay (Beckham, Coulter, Inc. Fullerton, CA, USA). Twelve-hour fasting serum levels of total cholesterol, triglyceride, and low- and high-density lipoprotein cholesterol were measured by standard enzymatic methods. Blood samples for high-sensitivity C-reactive protein (hsCRP) were obtained on admission and analyzed turbidimetrically with sheep antibodies against human CRP; this has been validated against the Dade Behring method.
Two-dimensional echocardiography was performed in all patients and left ventricular ejection fraction (LVEF) was assessed using modified Simpson's biplanar method. The morphology in coronary angiography was classified according to the criteria of American College of Cardiology/American Heart Association (ACC/AHA) (15). Degree of coronary flow was classified by Thrombolysis In Myocardial Infarction (TIMI) score (16). Presence of left main coronary artery stenosis was defined as a luminal stenosis ≥ 50%. Multivessel disease was defined as the presence of a lesion with > 50% diameter stenosis in a non-infarct related coronary artery. Successful PCI was defined as TIMI flow 3 with residual stenosis ≤ 50% in the infarct related artery. In-hospital complications included any of atrio-ventricular block, bradycardia, ventricular tachycardia/ventricular fibrillation, atrial fibrillation, cardiogenic shock, no re-flow, dissection, acute renal failure, metabolic acidosis/lactic acidosis, cerebrovascular event, or infection/sepsis. All patients were administered loading doses of aspirin 325 mg and clopidogrel 300-600 mg before PCI. Anticoagulation during PCI was performed according to the routine practices of each hospital. After the procedure, aspirin 100-200 mg (1 time per day) was prescribed indefinitely. Clopidogrel was prescribed continuously for 1 yr.
The primary endpoint was major adverse cardiac events (MACE) which included all-cause death, non-fatal myocardial infarction (MI), TLR and TVR during 12-month follow-up. Non-fatal MI was defined as the presence of clinical symptoms, electrocardiographic change, or abnormal imaging findings of MI combined with an increase in creatine kinase - MB fraction or troponin T/I more than the 99th percentile of the upper normal limit that was not related to an interventional procedure. TVR was defined as clinically driven repeat revascularization of a lesion in the same epicardial vessel treated in the index procedure at 12 month follow-up. TLR was defined as any revascularization of the target lesion due to restenosis or re-occlusion within 5 mm proximal/distal to the stent. All data were recorded on a standardized, electronic, web based registry at http://www.kamir.or.kr.
Statistical analysis
SPSS 17.0 for Windows (SPSS, Inc., Chicago, IL, USA) was used for all analysis. Continuous variables were presented as mean ± SD; comparisons were conducted by one-way ANOVA. Discrete variables were presented as percentages and frequencies; comparisons were conducted by chi-square statistics or Fischer's exact test. A P value < 0.05 was considered statistically significant. Cox proportional hazard analysis was performed in a stepwise manner to identify a model with independent predictive factors with determination of a hazard ratio and its 95% confidence interval (CI) for each variable in the model. Survival time of each patient to perform Cox analysis was calculated from date of admission/first presentation to the emergency room to the date of follow-up. A cut off P value < 0.20 were selected for entry into the model. The results are presented as adjusted hazard ratios (HR) with 95% confidence intervals and P values.
RESULTS
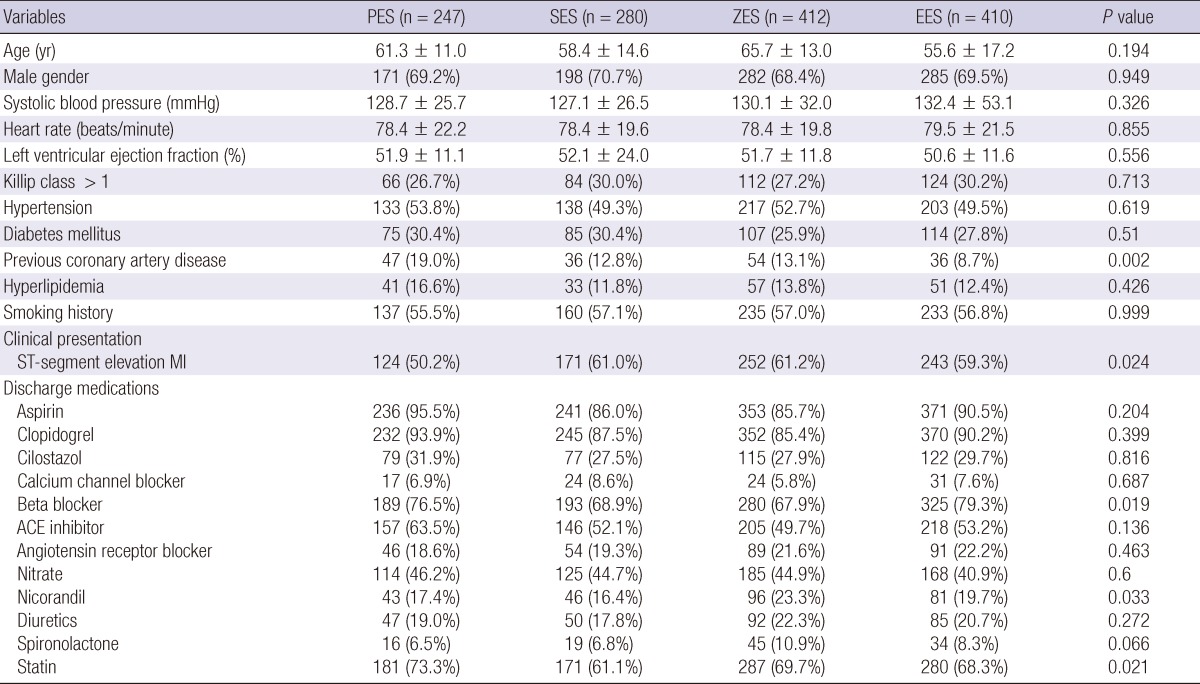
A total number of 1,349 consecutive patients with AMI undergoing PCI who received 2 or more homogenous overlapping DES in diffuse coronary lesions were included in the present study. These patients were divided into 4 groups based on the type of DESs implanted that is PES group, n = 247; SES group, n = 280; ZES group, n = 412 and EES group, n = 410. Mean age was 62.1 ± 14.9 yr and 69.4% were men. Mean stent length (including both stents) was 26.2 ± 7.5 mm and mean stent diameter was 3.1 ± 0.4 mm. Average number of stents used per vessel was 2.2 ± 0.5. Baseline clinical characteristics and concomitant medications of the 4 groups are presented in Table 1. Previous history of CAD was highest in PES group, followed by ZES, SES and lowest in EES group (P = 0.002). Clinical presentation with ST-segment elevation MI was found to be highest in ZES, followed by SES, EES and PES (P = 0.024). Use of beta blocker was highest in EES (P=0.019) and nicorandil in ZES (P=0.033) group. Use of statin was found to be highest in PES group, followed by ZES, EES and SES groups (P=0.021).
Table 1.
Baseline clinical characteristics and concomitant medications
Data are expressed as mean ± SD or as number (percentage). ACE, Angiotensin-converting enzyme.
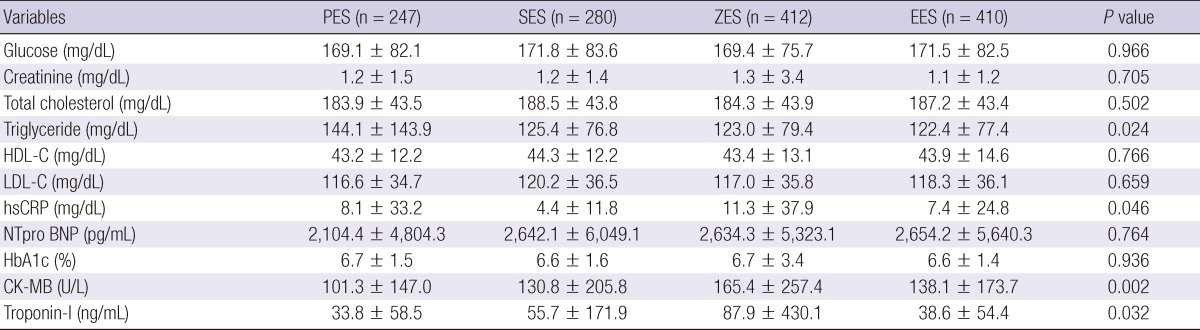
Laboratory findings of the 4 groups are presented in Table 2. Triglyceride showed an increasing trend from PES to SES to ZES to EES (P=0.024). Serum level of hsCRP was highest in ZES and lowest in SES group (P=0.046). CK-MB and troponin-I were highest in ZES group and lowest in PES group (P=0.002 and P=0.032, respectively).
Table 2.
Laboratory characteristics
Data are expressed as mean±SD. CK, Creatine kinase-MB; HbA1c, Hemoglobin A1c; HDL-C, High Density Lipoprotein Cholesterol; hsCRP, High-sensitivity C-Reactive Protein; LDL-C, Low Density Lipoprotein Cholesterol; NTpro BNP, N-Terminal pro-Brain Natrieuretic Peptide.
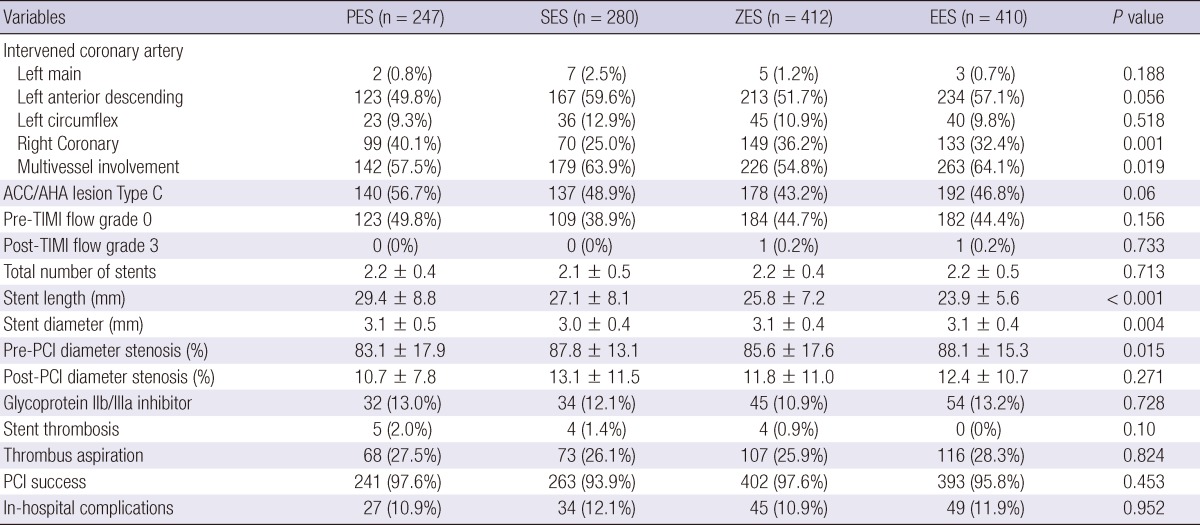
Coronary angiographic and procedural characteristics of 4 groups are presented in Table 3. Multivessel involvement was highest in EES group, followed by SES, PES and ZES (P=0.019). Right coronary involvement was highest in PES, then ZES, EES and SES (P=0.001). Percent diameter stenosis before PCI was highest in EES, followed by SES, ZES and PES (P=0.015). Mean stent length decreased from PES to EES groups (P<0.001). Mean stent diameter was found to be least in SES group and almost similar in other groups (P=0.004). Other angiographic characteristics did not show statistically meaningful differences among the groups.
Table 3.
Coronary angiographic and procedural characteristics
Data are expressed as mean±SD or as number (percentage). ACC/AHA, American College of Cardiology/American Heart Association; PCI, percutaneous coronary intervention; TIMI, Thrombolysis In Myocardial Infarction.
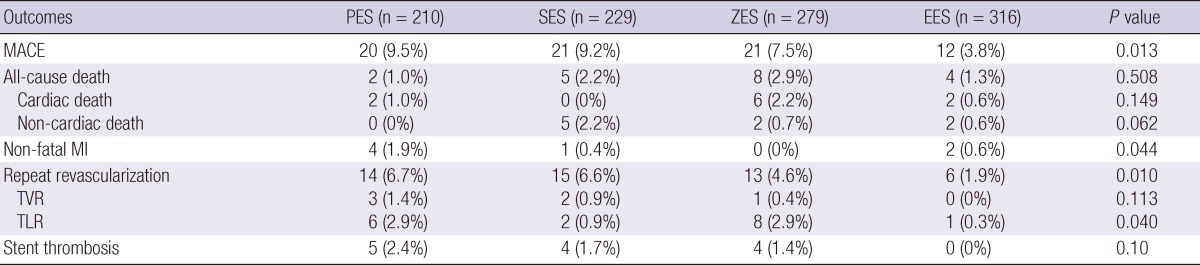
The rate of follow-up at 12 months was 76.6% (n=1,034). Twelve-month clinical outcomes are presented in Table 4. The incidence of MACE decreased from PES, SES, ZES to EES groups (9.5% vs 9.2% vs 7.5% vs 3.8%, P=0.013). Non-fatal MI was highest in PES group, almost similar in SES and EES groups with no incidence in ZES group (P=0.044). The occurrence of 12-month cardiac death was highest in ZES, followed by PES and EES with no incidence in SES group (P=0.149). Incidence of 12-month all-cause death and TVR were not statistically significant among the 4 groups. Repeat revascularization rate was found to be lowest in EES among 4 groups (P=0.01). There was no significant difference in non-cardiac death and stent thrombosis among the 4 groups (P=0.062 and P=0.10 respectively). Two acute events of stent thrombosis (1 in PES and 1 in ZES groups), 5 subacute stent thrombosis (3 in PES, 1 in SES and 1 in ZES groups), 3 late stent thrombosis (2 in SES and 1 in ZES groups) and 2 very late stent thrombosis (1 in PES and 1 in SES groups) occurred during the hospital stay. The average rate of PCI success was 97.9% (P=0.453).
Table 4.
Twelve-month clinical outcomes
Data are expressed as number (percentage). MACE, Major adverse cardiac events; MI, Myocardial Infarction; TVR, Target vessel revascularization; TLR, Target lesion revascularization.
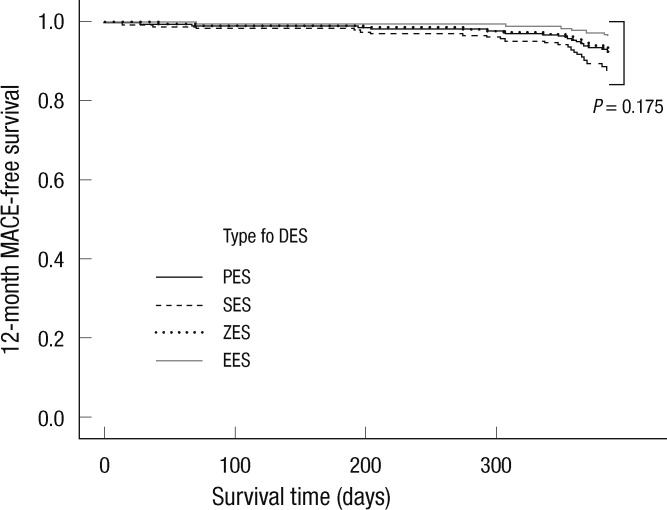
Cox proportional hazard analysis revealed no statistical differences in the incidence of MACE when adjusted for age and gender (P=0.826), and also when adjusted for multiple covariates (P=0.175) (Fig. 1). Table 5 shows details of multivariate analysis. ACC/AHA lesion type C (HR 0.431, CI 0.196 to 0.947, P=0.036) was found to be the only independent factor of the primary end point in this study. Covariates included in the model were age, gender, diameter stenosis before PCI, stent length and stent diameter, multivessel involvement, ACC/AHA lesion type C, pre-TIMI flow grade 0, clinical presentation ST-segment elevation MI, previous history of coronary artery disease (CAD), and statin use.
Fig. 1.
Cox model survival curves for 12-month major adverse cardiac events-free survival among 4 overlapping homogenous drug-eluting stents. DES, drug-eluting stent; PES, Paclitaxel-eluting stent; SES, Sirolimus-eluting stent; ZES, Zotarolimus-eluting stent; EES, Everolimus-eluting stent.
Table 5.
Cox regression analysis
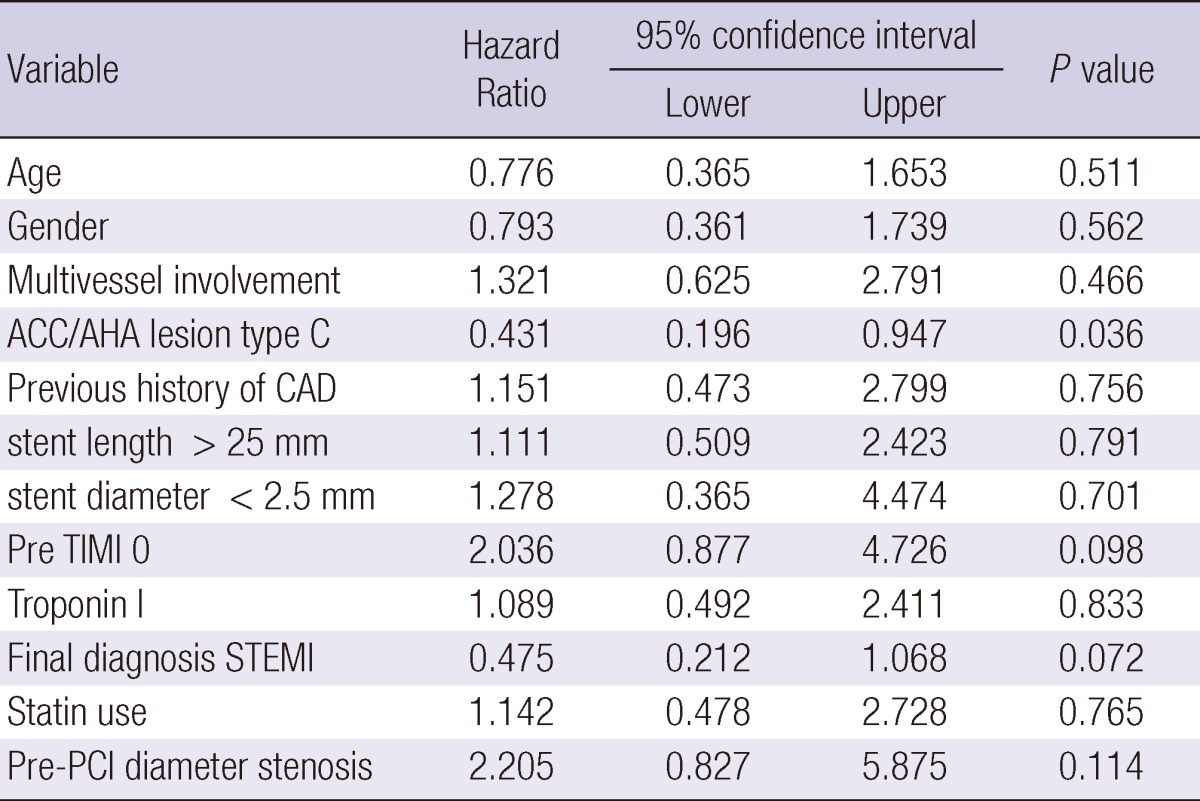
ACC/AHA, American College of Cardiology/American Heart Association; CAD, Coronary artery disease; STEMI, ST-segment elevation myocardial infarction; PCI, Percutaneous coronary intervention; TIMI, Thrombolysis In Myocardial Infarction.
In this study, EES showed a lower incidence of MACE at 12-months compared to other 3 types of DESs in uni-variate analysis as shown in Table 4. Conversely, in multivariate analysis after adjustment for multiple confounders the same difference does not reach statistical significance (Fig. 1). This could be due to the limited power of multivariate analysis with 4 sub-groups. The results on MACE are hypothesis-generating and warrant further long-term randomized evaluation.
DISCUSSION
The present study demonstrates no significant differences in safety and efficacy among 4 homogenous overlapping DESs in diffuse de novo coronary lesions in patients with AMI. Overlapping EES was found to have the lowest MACE rate and TLR-driven repeat revascularization rate with no reported events of stent thrombosis over the course of 12-month follow-up period in this cohort.
The development of DES, releasing anti-proliferative drugs into the vessel wall to inhibit neointimal hyperplasia, has revolutionized PCI dramatically reducing the incidence of ISR and TLR and permitting the treatment of more complex and extensive CAD, including diffuse or long lesions (17). The unique advantage of DES is that they allow higher local drug concentrations at lesion sites while avoiding systemic toxicity. DES showed signs of delayed arterial healing, more pronounced at the overlapping sites with increased inflammation and fibrin deposition. This leads to potential local toxicity caused by increased amounts of polymer and drug released at the overlapping stent site (10). The importance of a significant delay in endothelialization at sites of overlapping DES is underscored by the recent report of McFadden et al. involving 4 cases of human coronary thrombosis occurring >11 months after deployment of a single polymer-based PES or SES leading to more prolonged use of anti-platelet therapy (18). Lim et al.(19) studied porcine model and found that DESs inhibit neointimal hyperplasia, but inflammation and poor endothelization occur at the site of overlapping stents. Moreover, Munoz et al. found no significant quantitative changes in intravascular ultrasound measurements within overlapped segment (20).
More than 60% of DESs are used in the treatment of complex coronary lesions and 10% of them are overlapping (21, 22). However, there are sparse data available comparing 2 overlapping DESs, mainly PES and SES, with respect to important clinical outcomes such as death, MI, ST, TVR or TLR. This is the first clinical study comparing 4 types of overlapping homogenous DESs for diffuse long lesions in an established large interventional registry of AMI patients with prospective follow-up.
The impact of overlap of DES on clinical and angiographic outcomes is not well established. The Prospective, Randomized MultiCenter Comparison of the Cypher Sirolimus-Eluting and the Taxus Paclitaxel-Eluting Stent System (REALITY) Study (23), a 1,353-patient trial, demonstrated that binary restenosis rate, death, MI, TLR and TVR were similar between SES and PES systems; whereas Sirolimus-eluting and Paclitaxel-eluting Stents for Coronary Revascularization (SIRTAX) Study (24), a 1,012-patient trial, showed a favorable result in the SES arm in terms of TLR, late lumen loss, and binary restenosis.
In a 3-yr follow-up of SIRTAX trial, Raber et al.(22) demonstrated that patients with DES overlap are at greater risk of experiencing MACEs, particularly in needs of repeat revascularization and ischemic adverse events. Kastrati et al.(25) in a meta-analysis of 6 randomized trials compared clinical and angiographic outcomes of SES and PES. In this study subjects who received SES had a significantly lower risk of TVR and restenosis compared to PES. Shishehbor et al.(26) reported that overlapping SES are comparable with PES for early and late composite end points of death, ST, MI, and TLR; however those that received overlapping SES had a trend towards lower TLR. Degertekin et al.(27) demonstrated that overlapping SES implantation is safe and effective for very long coronary lesions. In their study, they used ≥2 overlapping stents at a minimum length of 41 mm to treat native coronary lesion. Their TLR, TVR, and MACE rates were compatible with our findings.
Kandzari et al.(28) in a prospective randomized trial studied comparison of the clinical efficacy, safety and angiographic outcomes among patients treated with ZES and SES, treatment with ZES was associated with increased neointimal hyperplasia resulting in greater angiographic late lumen loss. Patients treated with EES rather than PES experienced significantly improved event-free survival at a 2-yr follow-up in the SPIRIT III trial.(29) Serruys et al.(30) found ZES to be non-inferior to EES at 13-months follow-up. There is no data on safety of overlapping ZES and EES with regard to clinical outcomes. In our study cohort, EES appears to be relatively safe among overlapping DESs with lowest MACE and TLR-driven repeat revascularization rates, and no incidence of stent thrombosis. The higher rate of cardiac death in ZES group on univariate analysis could be attributable to high rates of several known predictors of mortality: higher prevalence of old age and ST-elevation myocardial infarction. They also had higher serum levels of baseline hs-CRP, CK-MB and troponin I, which indicates that the area of infarction was broader in the ZES group.
The risk of compromising the flow in the side branches originating from the main coronaries could have resulted in statistically significant non-fatal myocardial infarction. The patients in our study group received dual anti-platelet therapy (87.9%) for 1 yr after DES implantation according to ACC/AHA/Society for Cardiovascular Angiography and Interventions guidelines for PCI (7) which may have remarkably reduced the rate of stent thrombosis. Lowest MACE rate in EES group could be attributable to longer duration of dual antiplatelet therapy, better stent technique with different delivery system and different polymer. Moreover, the mean length of stents used was smallest in the EES group with highest percentage of pre-procedure diameter stenosis.
The present study is limited due to its retrospective and non-randomized nature, even though it was partially compensated for by adjustment in multivariable analysis. Our patients were analyzed in the short-term (12 months), and the follow-up rate was relatively low (76.6%). However, the number of follow-up patients at 12-months was substantial in this cohort of patients (n=1,033). This study lacks systemic angiographic follow-up data and possible complications (restenosis or aneurysm) at the site of overlapping could not be ascertained due to registry limitation. There could be bias due to rapid evolution in DES strategies considering the duration of 4 yr for patient enrollment (SES might be used frequently in the early days of this study, whereas EES might be so in the late phase) and its pharmaco-therapeutic management in the recent years. The reason for using overlapping DES is based on the operator's discretion which is prone to bias. Nevertheless, inclusion of relatively large number of patients and comparison of 4 most commonly used overlapping DES with appropriate method of statistical analysis is the strength of this study.
In conclusion this study demonstrates that any of the 4 types of overlapping homogenous DES (PES, SES, ZES, or EES) is acceptable to treat AMI patients and there are no significant differences in their 12-month MACEs. Overlapping EES was found to have the lowest MACE rate and TLR-driven repeat revascularization rate with no reported events of stent thrombosis over the course of 12-month follow-up period. This is an important study comparing overlapping DESs where incidence of overall MACE, including TLR and TVR was quite low. We suggest further long-term randomized evaluation to establish the safety of our study findings.
Appendix: Korea Acute Myocardial Infarction Registry (KAMIR) Study Group of Korean Society of Cardiology
Myung Ho Jeong, MD (Chonnam National University Hospital), Youngkeun Ahn, MD (Chonnam National University Hospital), Shung Chull Chae, MD (Kyungpook National University Hospital), Jong Hyun Kim, MD (Busan Hanseo Hospital), Seung Ho Hur, MD (Keimyung University Dongsna Hospital), Young Jo Kim, MD (Yeungnam University Hospital), In Whan Seong, MD (Chungnam National University Hospital), Dong Hoon Choi, MD (Yonsei University Severance Hospital), Jei Keon Chae, MD (Chonnbuk University Hospital), Taek Jong Hong, MD (Pusan National University Hospital), Jae Young Rhew, MD (Chonju Presbyterian Hospital), Doo Il Kim, MD (Inje University Hospital), In Ho Chae, MD (Seoul National University Hospital), Jung Han Yoon, MD (Wonju Christian Hospital), Bon Kwon Koo, MD (Seoul National University Hospital), Byung Ok Kim, MD (Inje University Hospital), Myoung Yong Lee, MD (Dankuk University Hospital), Kee Sik Kim, MD (Daegu Catholic University Hospital), Jin Young Hwang, MD (Gyeongsang National , Myeong Chan Cho, MD (Chungbuk National University Hospital), Seok Kyu Oh, MD (Wonkwnag University Hospital), Nae Hee Lee, MD (Suncheonhyang University Hospital), Kyoung Tae Jeong, MD (Eulji University Hospital), Seung Jea Tahk, MD (Ahju University Hospital), Jang Ho Bae, MD (Keonyang University Hospital), Seung Woon Rha, MD (Korea University Hospital), Keum Soo Park, MD (Inha University Hospital), Chong Jin Kim, MD (Kyunghee University Hospital), Kyoo Rok Han, MD (Hanlym University Hospital), Tae Hoon Ahn, MD (Gacheon University Gill Hospital), Moo Hyun Kim, MD (Dong University Hospital), Ki Bae Seung, MD (Catholic University Hospital), Wook Sung Chung, MD (Catholic University Hospital), Ju Young Yang, MD (Ilsan Hospital), Chong Yun Rhim, MD (Hanllym University Hospital), Hyeon Cheol Gwon, MD (Samsung Medical Center), Seong Wook Park, MD (Asan Medical Center), Young Youp Koh, MD (Chosun University Hospital), Seung Jae Joo, MD (Cheju University Hospital), Soo Joong Kim, MD (Kyung Hee University Hospital), Dong Kyu Jin, MD (Suncheonhyang University Hospital), Jin Man Cho, MD (Kyung Hee University Hospital), Byung Ok Kim, MD (Inje University Hospital), Sang-Wook Kim, MD (Chungang University Hospital), Jeong Kyung Kim, MD (Daejon Sun Hospital), Tae Ik Kim, MD (Busan Maryknoll Hospital), Deug Young Nah, MD (Dongkuk University Hospital), Si Hoon Park, MD (Ihwa University Hospital), Sang Hyun Lee, MD (Mokpo Hankuk Hospital), Seung Uk Lee, MD (Kwangju Christian Hospital), Hang-Jae Chung, MD (Pohang Seonrin Hospital), Jang Hyun Cho, MD (Suncheon Carollo Hospital), Seung Won Jin, MD (Daejon Hankuk Hospital), Yang Soo Jang, MD (Yeonsei University Severance Hospital), Jeong Gwan Cho, MD, and Seung Jung Park, MD (Asan Medical Center).
Footnotes
This study was performed with the support of the Korean Society of Circulation in the memorandum of the 50th Anniversary of the Korean Society of Circulation and Korea Ministry of Health and Welfare (A084869), Republic of Korea.
References
- 1.Stettler C, Wandel S, Allemann S, Kastrati A, Morice MC, Schömig A, Pfisterer ME, Stone GW, Leon MB, de Lezo JS, et al. Outcomes associated with drug-eluting and bare-metal stents: a collaborative network meta-analysis. Lancet. 2007;370:937–948. doi: 10.1016/S0140-6736(07)61444-5. [DOI] [PubMed] [Google Scholar]
- 2.Kaltoft A, Jensen LO, Maeng M, Tilsted HH, Thayssen P, Bøttcher M, Lassen JF, Krusell LR, Rasmussen K, Hansen KN, et al. 2-year clinical outcomes after implantation of sirolimus-eluting, paclitaxel-eluting, and bare-metal coronary stents: results from the WDHR (Western Denmark Heart Registry) J Am Coll Cardiol. 2009;53:658–664. doi: 10.1016/j.jacc.2008.09.058. [DOI] [PubMed] [Google Scholar]
- 3.James SK, Stenestrand U, Lindback J, Carlsson J, Scherstén F, Nilsson T, Wallentin L, Lagerqvist B SCAAR Study Group. Long-term safety and efficacy of drug-eluting versus bare-metal stents in Sweden. N Engl J Med. 2009;360:1933–1945. doi: 10.1056/NEJMoa0809902. [DOI] [PubMed] [Google Scholar]
- 4.Eisenberg MJ, Konnyu KJ. Review of randomized clinical trials of drug-eluting stents for the prevention of in-stent restenosis. Am J Cardiol. 2006;98:375–382. doi: 10.1016/j.amjcard.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 5.Roukoz H, Bavry AA, Sarkees ML, Mood GR, Kumbhani DJ, Rabbat MG, Bhatt DL. Comprehensive meta-analysis on drug-eluting stents versus bare-metal stents during extended follow-up. Am J Med. 2009;122:581.e1–581.e10. doi: 10.1016/j.amjmed.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 6.Ramcharitar S, Hochadel M, Gaster AL, Onuma Y, Gitt A, Serruys PW. An insight into the current use of drug eluting stents in acute and elective percutaneous coronary interventions in Europe. A report on the EuroPCI Survey. EuroIntervention. 2008;3:429–441. doi: 10.4244/a78. [DOI] [PubMed] [Google Scholar]
- 7.King SB, 3rd, Smith SC, Jr, Hirshfeld JW, Jr, Jacobs AK, Morrison DA, Williams DO, Feldman TE, Kern MJ, O'Neill WW, et al. 2005 WRITING COMMITTEE MEMBERS. 2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee. Circulation. 2008;117:261–295. doi: 10.1161/CIRCULATIONAHA.107.188208. [DOI] [PubMed] [Google Scholar]
- 8.Marroquin OC, Selzer F, Mulukutla SR, Williams DO, Vlachos HA, Wilensky RL, Tanguay JF, Holper EM, Abbott JD, Lee JS, et al. A comparison of bare-metal and drug-eluting stents for off-label indications. N Engl J Med. 2008;358:342–352. doi: 10.1056/NEJMoa0706258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Messori A, Trippoli S. Drug-eluting stents for the treatment of coronary artery disease: NICE technology appraisal guidance. Heart. 2009;95:847. [PubMed] [Google Scholar]
- 10.Finn AV, Kolodgie FD, Harnek J, Guerrero LJ, Acampado E, Tefera K, Skorija K, Weber DK, Gold HK, Virmani R. Differential response of delayed healing and persistent inflammation at sites of overlapping sirolimus-or paclitaxel-eluting stents. Circulation. 2005;112:270–278. doi: 10.1161/CIRCULATIONAHA.104.508937. [DOI] [PubMed] [Google Scholar]
- 11.Wilson GJ, Polovick JE, Huibregtse BA, Poff BC. Overlapping paclitaxel-eluting stents: long-term effects in a porcine coronary artery model. Cardiovasc Res. 2007;76:361–372. doi: 10.1016/j.cardiores.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Lee SR, Jeong MH, Ahn YK, Chae SC, Hur SH, Kim YJ, Seong IW, Chae JK, Hong TJ Korea Acute Myocardial Infarction Registry Investigators. Clinical safety of drug-eluting stents in the Korea acute myocardial infarction registry. Circ J. 2008;72:392–398. doi: 10.1253/circj.72.392. [DOI] [PubMed] [Google Scholar]
- 13.Sim DS, Jeong MH, Kang JC. Current management of acute myocardial infarction: experience from the Korea Acute Myocardial Infarction Registry. J Cardiol. 2010;56:1–7. doi: 10.1016/j.jjcc.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Apple FS, Wu AH, Jaffe AS. European Society of Cardiology and American College of Cardiology guidelines for redefinition of myocardial infarction: how to use existing assays clinically and for clinical trials. Am Heart J. 2002;144:981–986. doi: 10.1067/mhj.2002.124048. [DOI] [PubMed] [Google Scholar]
- 15.Kini AS. Coronary angiography, lesion classification and severity assessment. Cardiol Clin. 2006;24:153–162. doi: 10.1016/j.ccl.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 16.Manginas A, Gatzov P, Chasikidis C, Voudris V, Pavlides G, Cokkinos DV. Estimation of coronary flow reserve using the Thrombolysis In Myocardial Infarction (TIMI) frame count method. Am J Cardiol. 1999;83:1562–1565. doi: 10.1016/s0002-9149(99)00149-6. [DOI] [PubMed] [Google Scholar]
- 17.Kirtane AJ, Gupta A, Iyengar S, Moses JW, Leon MB, Applegate R, Brodie B, Hannan E, Harjai K, Jensen LO, et al. Safety and efficacy of drug-eluting and bare metal stents: comprehensive meta-analysis of randomized trials and observational studies. Circulation. 2009;119:3198–3206. doi: 10.1161/CIRCULATIONAHA.108.826479. [DOI] [PubMed] [Google Scholar]
- 18.McFadden EP, Stabile E, Regar E, Cheneau E, Ong AT, Kinnaird T, Suddath WO, Weissman NJ, Torguson R, Kent KM, et al. Late thrombosis in drug-eluting coronary stents after discontinuation of antiplatelet therapy. Lancet. 2004;364:1519–1521. doi: 10.1016/S0140-6736(04)17275-9. [DOI] [PubMed] [Google Scholar]
- 19.Lim SY, Jeong MH, Hong SJ, Lim DS, Moon JY, Hong YJ, Kim JH, Ahn Y, Kang JC. Inflammation and delayed endothelization with overlapping drug-eluting stents in a porcine model of in-stent restenosis. Circ J. 2008;72:463–468. doi: 10.1253/circj.72.463. [DOI] [PubMed] [Google Scholar]
- 20.Muñoz JS, Abizaid A, Mintz GS, Albertal M, Abizaid AS, Feres F, Centemero M, Staico R, Mattos LA, Pinto I, et al. Intravascular ultrasound study of effects of overlapping sirolimus-eluting stents. Am J Cardiol. 2004;93:470–473. doi: 10.1016/j.amjcard.2003.10.047. [DOI] [PubMed] [Google Scholar]
- 21.Farb A, Boam AB. Stent thrombosis redux--the FDA perspective. N Engl J Med. 2007;356:984–987. doi: 10.1056/NEJMp068304. [DOI] [PubMed] [Google Scholar]
- 22.Raber L, Juni P, Loffel L, Wandel S, Cook S, Wenaweser P, Togni M, Vogel R, Seiler C, Eberli F, et al. Impact of stent overlap on angiographic and long-term clinical outcome in patients undergoing drug-eluting stent implantation. J Am Coll Cardiol. 2010;55:1178–1188. doi: 10.1016/j.jacc.2009.11.052. [DOI] [PubMed] [Google Scholar]
- 23.Morice MC, Colombo A, Meier B, Serruys P, Tamburino C, Guagliumi G, Sousa E, Stoll HP REALITY Trial Investigators. Sirolimus- vs paclitaxel-eluting stents in de novo coronary artery lesions: the REALITY trial: a randomized controlled trial. JAMA. 2006;295:895–904. doi: 10.1001/jama.295.8.895. [DOI] [PubMed] [Google Scholar]
- 24.Windecker S, Remondino A, Eberli FR, Jüni P, Räber L, Wenaweser P, Togni M, Billinger M, Tüller D, Seiler C, et al. Sirolimus-eluting and paclitaxel-eluting stents for coronary revascularization. N Engl J Med. 2005;353:653–662. doi: 10.1056/NEJMoa051175. [DOI] [PubMed] [Google Scholar]
- 25.Kastrati A, Dibra A, Eberle S, Mehilli J, Suárez de Lezo J, Goy JJ, Ulm K, Schömig A. Sirolimus-eluting stents vs paclitaxel-eluting stents in patients with coronary artery disease: meta-analysis of randomized trials. JAMA. 2005;294:819–825. doi: 10.1001/jama.294.7.819. [DOI] [PubMed] [Google Scholar]
- 26.Shishehbor MH, Amini R, Raymond RE, Bavry AA, Brener SJ, Kapadia SR, Whitlow PL, Ellis SG, Bhatt DL. Safety and efficacy of overlapping sirolimus-eluting versus paclitaxel-eluting stents. Am Heart J. 2008;155:1075–1080. doi: 10.1016/j.ahj.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 27.Degertekin M, Arampatzis CA, Lemos PA, Saia F, Hoye A, Daemen J, Tanabe K, Lee CH, Hofma SJ, Sianos G, et al. Very long sirolimus-eluting stent implantation for de novo coronary lesions. Am J Cardiol. 2004;93:826–829. doi: 10.1016/j.amjcard.2003.12.018. [DOI] [PubMed] [Google Scholar]
- 28.Kandzari DE, Leon MB, Popma JJ, Fitzgerald PJ, O'Shaughnessy C, Ball MW, Turco M, Applegate RJ, Gurbel PA, Midei MG, et al. Comparison of zotarolimus-eluting and sirolimus-eluting stents in patients with native coronary artery disease: a randomized controlled trial. J Am Coll Cardiol. 2006;48:2440–2447. doi: 10.1016/j.jacc.2006.08.035. [DOI] [PubMed] [Google Scholar]
- 29.Stone GW, Midei M, Newman W, Sanz M, Hermiller JB, Williams J, Farhat N, Caputo R, Xenopoulos N, Applegate R, et al. Comparison of everolimus-eluting and paclitaxel-eluting stents: two-year clinical follow-up from the Clinical Evaluation of the Xience V Everolimus Eluting Coronary Stent System in the Treatment of Patients with de novo Native Coronary Artery Lesions (SPIRIT) III trial. Circulation. 2009;119:680–686. doi: 10.1161/CIRCULATIONAHA.108.803528. [DOI] [PubMed] [Google Scholar]
- 30.Serruys PW, Silber S, Garg S, van Geuns RJ, Richardt G, Buszman PE, Kelbaek H, van Boven AJ, Hofma SH, Linke A, et al. Comparison of zotarolimus-eluting and everolimus-eluting coronary stents. N Engl J Med. 2010;363:136–146. doi: 10.1056/NEJMoa1004130. [DOI] [PubMed] [Google Scholar]