Inflammation has long been a well-known symptom of many infectious diseases, but molecular and epidemiological research increasingly suggests that it is also intimately linked with a broad range of non-infectious diseases, perhaps even all of them. Although these insights might not lead to a unified theory of disease, the crucial role of inflammatory processes makes possible the development of a new generation of drugs to treat conditions including cancers, autoimmune disorders and infectious diseases.
…humans with colitis-associated cancer have elevated TLR4 levels, which raises the possibility of using this highly conserved receptor as a therapeutic target
It is hard to pinpoint a specific advance or paper that heralded this new understanding of inflammation and disease in the genomic era, but one seminal development was the 2004 discovery that the ras cancer gene plays a role in inflammation [1]. This insight was followed by a spate of papers identifying a role for chronic inflammation in many cancers at various stages of their progression, in some cases identifying possible targets for therapeutic intervention.
Maria Abreu's research group at the University of Miami's Miller School of Medicine in the USA found that the incidence of colon cancer was linked directly to expression of the Toll-like receptor 4 (TLR4) gene [2]. TLRs are crucial in alerting the immune system to microbial infection, triggering acute inflammatory responses that clear invading pathogens. However, TLR4 can also maintain chronic inflammation, for example by responding to commensal bacteria in the gut. As such bacteria are constantly replenished through food intake, and therefore cannot be permanently cleared by the immune system, this can lead to persistent chronic infection maintained by TLRs. Abreu's work suggests that TLR4 not only plays a role in setting up chronic inflammation—which seems to trigger cancer formation—but also promotes subsequent tumorigenesis. She found that suppressing the TLR4 gene protects mice from colon cancers that usually arise from chronic inflammation, and that overexpression of TLR4 increases susceptibility to colon cancer. Interestingly, humans with colitis-associated cancer have elevated TLR4 levels, which raises the possibility of using this highly conserved receptor as a therapeutic target.
Rosana Risques, a specialist in inflammatory processes at the University of Washington in Seattle, USA, said that it is becoming clear that chronic inflammation is implicated at every level of tumorigenesis. This includes initiation, promotion, malignant conversion, invasion and final metastasis. Risques explained that the initial process involves DNA damage caused by reactive oxygen species that are produced by immune cells. The role of inflammation in the subsequent processes that lead to terminal cancer is less clear, and presumably involves signalling and cross-talk between the tumour cells and the host immune system. Indeed, a study from the Istituto Clinico Humanitas in Milan, Italy, suggests that an inflammatory microenvironment is essential for all cancers [3], although the causal mechanisms have yet to be established.
…environmental factors that trigger both oncogenic changes and inflammation are probably particularly potent causes of cancer; this certainly seems to be the case for tobacco smoke
According to Maija Kohonen-Corish from the Garvan Institute of Medical Research, Sydney, Australia, chronic inflammation causes cancer through tissue destruction and scarring, and reshaping of the tissue architecture, as well as contributing to changes in gene expression that sustain tumorigenesis. The permanent presence of inflammatory proteins also maintains an environment in which tumour cells can proliferate. “In a nutshell, it is believed that inflammatory mediators such as cytokines and chemokines, when persistent in the inflamed tissue, can induce proliferation, survival and growth of cells and modify their differentiation status, 'forcing' them to undergo transformation,” Kohonen-Corish explained. In some cases, cancer might arise in the absence of inflammation—as a result of an oncogenic change caused by an environmental exposure, for example—but even in those cases, low-level inflammation is crucial in sustaining the processes of tumorigenesis. Thus, environmental factors that trigger both oncogenic changes and inflammation are probably particularly potent causes of cancer; this certainly seems to be the case for tobacco smoke. In addition to the established role of tobacco smoke in tumour initiation, owing to its high concentration of carcinogens, research shows that smoking also promotes lung cancer by causing chronic inflammation [4].
Another major group of diseases in which chronic inflammation has been implicated are disorders that involve progressive and irreversible damage to the central nervous system. Work in this field has already led to clinical trials for a drug to treat amyotrophic lateral sclerosis (ALS), a common and fatal motor neuron disease. The drug was developed by Arturo Zychlinsky and colleagues at the Max Planck Institute for Infection Biology in Berlin, Germany, who suspected that in addition to a combination of inherited and environmental factors that cause ALS, inflammatory processes might also be involved in causing the death of neurons. They discovered that the signalling molecule interleukin-1 is integral to the pathogenesis of ALS and showed that, by blocking its production, they could enhance the motor performance and increase the lifespan of mice suffering from a disease similar to ALS. Their results suggested that the same blocking agent might work in ALS patients [5]. “[T]ogether with the ALS clinic at the Charité, we have started a clinical trial,” Zychlinsky explained. The team is optimistic that the patients will have enhanced motor performance, even if it is still too early to say whether they will also live longer.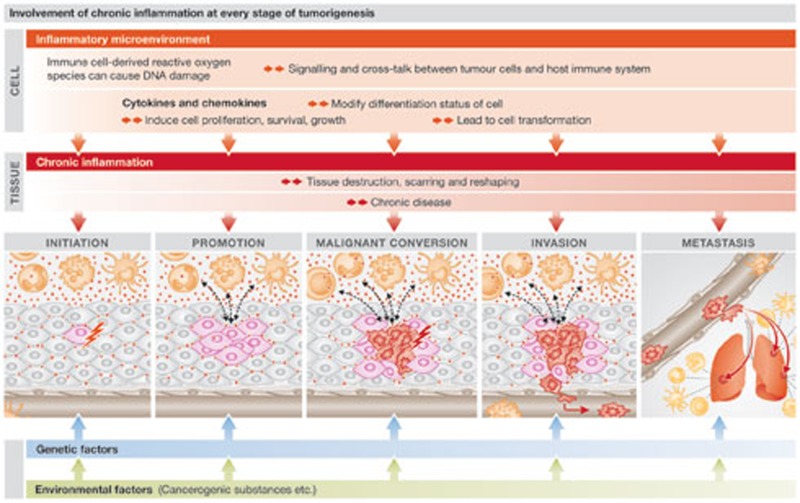
If chronic inflammation does underlie so many diseases, it would make sense to recognize it as a condition that should be treated in its own right as a preventative therapy. One problem with promoting this approach, however, is that chronic inflammation does not always cause disease; it requires additional genetic and environmental factors. As such, attempts to alleviate chronic inflammation are confined to cases where it is already clear that disease has resulted.
…attempts to alleviate chronic inflammation are confined to cases where it is already clear that disease has resulted
This is the case for severe asthma, which Peter Barnes and colleagues at Imperial College in London, UK, have shown is associated with insensitivity to the action of corticosteroids [6]. Corticosteroids are effective in treating most patients suffering from mild or moderate asthma, but Barnes has found that 5–10% of patients retain severe symptoms even after treatment with high doses of corticosteroids. This group of patients accounts for about 50% of total healthcare cost for asthma in the UK. Barnes and his team have found that the reduced responsiveness to corticosteroids is associated with reduced nuclear translocation and hyperphosphorylation of the glucocorticoid receptor. Normally, corticosteroids bind to glucocorticoid receptors that then translocate to the nucleus to regulate the expression of genes involved in immune responses. Barnes and colleagues have identified a mechanism by which the administration of long-acting adrenergic agonists restores the activity of the glucocorticoid receptor in severe asthma patients, by inhibiting phosphorylation and increasing nuclear translocation. The result is improved sensitivity to corticosteroids, opening up a potential treatment for severe asthma.
In some cases, existing drugs with anti-inflammatory effects are being found to be effective against a variety of diseases resulting from chronic inflammation. The long-term use of aspirin to reduce the risk of cardiovascular disease is well known, but a study at the John Radcliffe Hospital in Oxford, UK, found that people taking aspirin over long periods also had a lower incidence of death from cancer [7].
Another anti-inflammatory drug that holds promise is omeprazole, normally prescribed to reduce acid reflux in the stomach. In its new role, it is being used to treat cancers induced by colitis, which is associated with inflammation in the bowel. Omeprazole is a proton pump inhibitor that blocks the hydrogen/potassium adenosine triphosphatase enzyme system involved in the final stage of gastric acid secretion, but also has significant anti-inflammatory, anti-oxidative and anti-mutagenic activities that help prevent colitis-induced carcinogenesis [8]. “I think Proton Pump Inhibitors can be applied successfully for cancer treatment,” said Ki Baik Hahm, one of the authors. “We are also planning to do some clinical trials.”
Clinical evidence suggests that some traditional remedies, such as curcumin—an active component of turmeric, the yellow spice used widely in Indian cuisine—are effective against inflammatory bowel disease (IBD). A study from the Father Muller Medical College in Karnataka, India, reported that several experimental models of IBD responded to curcumin, which seems to work by scavenging free radicals, increasing anti-oxidants and influencing multiple signalling pathways [9]. The authors recommend the initiation of large-scale clinical investigations to determine the potential for the oral use of curcumin to treat IBD.
The entire field of inflammation and disease has reached a point where large controlled studies are needed to identify specific targets for therapeutic intervention
There is growing evidence that diseases with an inflammatory component can be treated through physical exercise, rather than pharmacology. The positive effect of exercise on inflammatory processes has long been known, but there was little evidence of a direct link with specific conditions. This year, however, a multi-agency US study looked in detail at 45 articles published between 1950 and 2011 that relate physical activity, cancer survival and biomarkers potentially relevant to cancer [10]. Although the data were inconclusive for most cancers, there was consistent evidence from 27 of the studies that physical activity reduced mortality from breast and colon cancers of all causes. Furthermore, the authors pointed out that randomized controlled trials designed to correlate exercise with specific biomarker endpoints suggest that physical activity might beneficially change the circulating levels of insulin, insulin-related pathways, inflammation and, possibly, immunity.
The entire field of inflammation and disease has reached a point where large controlled studies are needed to identify specific targets for therapeutic intervention. There is also hope of establishing a common framework for understanding a variety of conditions previously considered to be unrelated, through the underlying inflammatory mechanisms. One study at Carnegie Mellon University in the USA attempted to link stress, inflammation and the risk of infectious disease by looking at glucocorticoid receptor resistance, which is known to have a role in other inflammation-related diseases such as asthma. The study, led by Sheldon Cohen, Director of the university's Laboratory for the Study of Stress, Immunity and Disease, focused on the common cold to assess the link between chronic psychological stress and the risk of contracting upper respiratory infections in general. The researchers found that reduced glucocorticoid receptor sensitivity leads to increased levels of circulating leukocytes and neutrophils, triggered by the increased release of pro-inflammatory cytokines. The authors concluded that this same inflammatory process upregulates immunity to the cold virus and is responsible for well-known cold symptoms such as increased mucus production in the nose. The implication is that stress does not necessarily increase the probability of infection, but it does amplify the symptoms. This suggests that anti-inflammatory rather than anti-viral mechanisms might constitute the most effective remedy for many upper respiratory infections. Cohen pointed out that these findings were consistent with the viral-challenge theory, which suggests a positive association between pro-inflammatory cytokine levels and the expression of symptoms.
More fundamentally, Cohen argued that this model might help to understand the development of many other conditions associated with prolonged stress, including cardiovascular disease, diabetes, autoimmune conditions and even clinical depression. It might also lead to a new and better understanding of the interplay between the immune system, inflammation and infectious disease, and how they trigger chronic inflammation leading to other conditions.
Footnotes
The author declares that he has no conflict of interest.
References
- Liu J et al. (2004) A genetically defined model for human ovarian cancer. Cancer Res 64: 1655–1663 [DOI] [PubMed] [Google Scholar]
- Fukata M et al. (2007) Toll-like receptor-4 promotes the development of colitis-associated colorectal tumors. Gastroenterology 133: 1869–1881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454: 436–444 [DOI] [PubMed] [Google Scholar]
- Takahashi H, Ogata H, Nishigaki R, Broide DH, Karin M (201) Tobacco smoke promotes lung tumorigenesis by triggering IKKbeta- and JNK1-dependent inflammation. Cancer Cell 17: 89–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meissner F, Molawi K, Zychlinsky A (2010) Mutant superoxide dismutase 1-induced IL-1beta accelerates ALS pathogenesis. Proc Natl Acad Sci USA 107: 13046–13050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercado N, Hakim A, Kobayashi Y, Meah S, Usmani OS, Chung KF, Barnes PJ, Ito K (2012) Restoration of corticosteroid sensitivity by p38 mitogen activated protein kinase inhibition in peripheral blood mononuclear cells from severe asthma. PLoS ONE 7: e41582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Algra AM, Rothwell PM (2012) Effects of regular aspirin on long-term cancer incidence and metastasis: a systematic comparison of evidence from observational studies versus randomised trials. Lancet Oncol 13: 518–527 [DOI] [PubMed] [Google Scholar]
- Kim YJ, Lee JS, Hong KS, Chung JW, Kim JH, Hahm KB (2010) Novel application of proton pump inhibitor for the prevention of colitis-induced colorectal carcinogenesis beyond acid suppression. Cancer Prev Res 3: 963–974 [DOI] [PubMed] [Google Scholar]
- Baliga MS, Joseph N, Venkataranganna MV, Saxena A, Ponemone V, Fayad R (2012) Curcumin, an active component of turmeric in the prevention and treatment of ulcerative colitis: preclinical and clinical observations. Food Funct [Epub ahead of print] doi:; DOI: 10.1039/C2FO30097D [DOI] [PubMed] [Google Scholar]
- Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM (2012) Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review. J Natl Cancer Inst 104: 815–840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, Turner RB (2012) Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci USA 109: 5995–5999 [DOI] [PMC free article] [PubMed] [Google Scholar]


