Abstract
Objective
The purpose of this study was to examine the relationship between shared decision-making (SDM) and satisfaction with decision (SWD) within a larger survey of patient decision-making in health care consultations.
Methods
A randomly selected age-proportionate national sample of adults (aged 21–70 years) stratified on race, ethnicity, and gender (N = 488) was recruited from a health research volunteer registry and completed an online survey with reference to a recent health consultation. Measures included the Shared Decision Making-9 questionnaire (SDM-Q-9), Satisfaction With Decision (SWD) scale, sociodemographic, health, and other standardized decision-making measures. Forward selection weighted multiple regression analysis was used to model correlates of SWD.
Results
After controlling for sociodemographic variables, SDM-Q-9 total score was associated with SWD, adjusted R2 = .368, p < .001. Three of nine SDM-Q-9 items accounted for significant proportions of variance in SWD.
Conclusion
SDM was positively associated with SWD and was strongest for three areas of SDM: patients being helped in a health care consultation with understanding information, with treatment preference elicitation, and with weighing options thoroughly.
Practice Implications
By identifying variables such as SDM that are associated with SWD, health care interventions can better target modifiable factors to enhance satisfaction and other outcomes.
Keywords: shared decision-making, satisfaction with decision, patient-provider communication
1. Introduction
A majority of adults routinely engage in health-related decision-making that has significant impact for personal health and well-being and broader public health outcomes. Recent national surveys in North America document the high prevalence of patient decision-making and associated unmet needs for decision-making support among patients who seek health care services (1, 2). Shared decision-making (SDM) is receiving increasing attention as a solution to better meet patient decision support needs by improving the quality of patient-provider health care decision-making processes. SDM can be broadly defined as an interactive, collaborative process between patients and health care providers that is used to make health care decisions, that is characterized by several features of the patient-provider interaction: (a) eliciting and acknowledging patients’ preferences for participation; (b) giving choices as to how the decision-making process will proceed; and, (c) mutually respecting and adhering to choices (3). SDM is advocated on premises that patients have a right of self-determination, as well as an expectation that patient involvement in shared decision-making can increase the likelihood of treatment adherence (4), in which adherence is conceptualized as the extent to which a patient continues to implement a previously-made treatment decision. Research on the relationship between SDM and adherence is important because patients themselves usually control the extent to which they adhere to health treatments, and adherence has significant impact on health and other outcomes.
Recently Stalmeier (2010) proposed a conceptual model to illustrate effects of decision aids on adherence behavior (4). The model posits researchable hypotheses (described as ‘hypothetical’ pathways in the model) for how processes of communication and deliberation in SDM can support treatment adherence. Specifically, decision aids are hypothesized to strengthen attitudes toward choices (options), which in turn can strengthen the relationship between attitudes and adherence behavior. Patient attitudes about options can be measured in multiple ways, including but not limited to strength and persistence of treatment preferences, and level of satisfaction with decisions. While there is as yet inconclusive empirical support for the hypothesized linkages of SDM, attitudes, and adherence, prior findings hold sufficient promise such that future studies are proposed to more definitely examine these relationships (4, 5). From a public health perspective, information about the association of shared decision-making and attitudes toward options is important because these are potentially-modifiable variables that can inform improved interventions to support treatment adherence, and improved adherence can lead to improved health outcomes.
1.1. Study purpose
The purpose of this study was to examine the relationship of patient perceptions of shared decision-making (SDM) and an attitude measure, satisfaction with decision (SWD) (6, 7), within a larger survey that was conducted to validate a newly-developed measure of SDM, the Shared Decision Making-9 questionnaire (SDM-Q-9), in a U.S. national sample (8, 9). The secondary analysis reported in this paper extends findings of prior national surveys (1, 2) by examining the association of SDM and SWD for a recently-made decision related to diagnosis, treatment, or referral for a personally-experienced health issue. The specific analysis reported in this paper and recency of recall of decision-making (decision made in the past 3 months) have not been addressed in prior national surveys which have used longer recall time periods; i.e., ever having made a complex health-related decision (2), or having made a medical decision within the past two years (1). Within the framework of the Stalmeier model (4), the overall hypothesis examined in the present study was that SDM would exhibit a positive relationship with SWD. Additional analyses were conducted to further explore: (a) the contribution of specific aspects of SDM to SWD; and, (b) the association of socio-demographic and other decision-making variables with SWD. To provide context about the decision-making circumstances of the respondents and to place our study results in context of other surveys of health-related decision-making (1, 2), we also summarized the types of reported health-related decisions (relating to diagnosis, treatment or referral for health concerns) and the specific categories of health concerns that were a focus of decision-making. We also were able to compare the socio-demographic characteristics of our obtained sample to the ResearchMatch population.
2. Methods
2.1. Recruitment and sampling
The present study was based on a secondary analysis of data from a larger survey study that was conducted to validate the Shared Decision Making Questionnaire-9 (SDM-Q-9) (8) in a U.S. national sample. Recruitment for the study was done via ResearchMatch, a national health volunteer registry that was created by several academic institutions and supported by the U.S. National Institutes of Health as part of the Clinical Translational Science Award (CTSA) program. ResearchMatch has a large population of volunteers who have consented to be contacted by researchers about health studies for which they may be eligible. Review and approval for the study and all procedures was obtained from The Ohio State University Behavioral and Social Sciences Institutional Review Board.
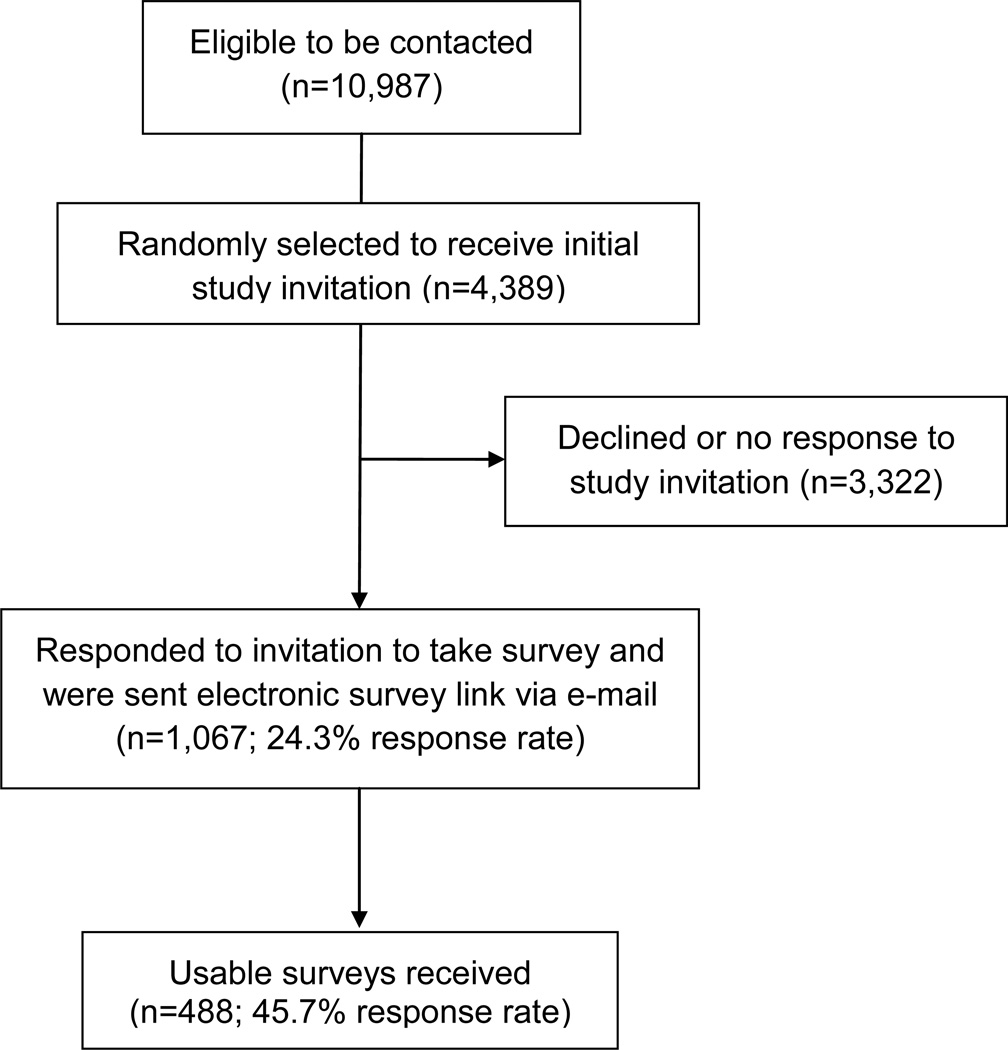
A stratified random sampling plan was created by state to reflect the gender,race, and ethnic distribution of the 2000 U.S. population census data for persons between the ages of 21 and 70. States were clustered into one of six geographic regions. Each region had an associated list of individuals aged 21–70 years to sample by state, within dichotomized strata of gender, race, and ethnicity. If a given state did not have enough ResearchMatch volunteers to reflect the sample needed to match the sampling plan, additional individuals were drawn from (a) larger state(s) within the same region. For states with more volunteers than needed to be sampled, a random number table was generated to select which individuals to contact. The study invitation was sent via ResearchMatch to the selected volunteers. The study flow diagram in Figure 1 shows the study recruitment, sampling, and survey processes.
Figure 1. Study Flow Diagram.
Of 10,987 ResearchMatch volunteers listed as being between 21 and 70 years of age, 4,389 were randomly selected to receive the initial study invitation. If a volunteer replied “YES” to the study invitation, the volunteer was sent a link to the online study survey. The survey consent procedure asked the respondent to confirm that s/he met study eligibility criteria by: (a) being between 21 and 70 years of age; and, (b) having had a consultation with a health care provider within the past 3 months for diagnosis, treatment, or referral related to a personally experienced health issue.
2.2. Measures
The survey consisted of measures of respondent characteristics and measures related to the process of decision-making. Decision-making questionnaires were completed with reference to a specific consultation each respondent confirmed had occurred with a health care provider within 3 months of participation in the survey. Respondents were asked to report age, race, gender, state of residence, ethnicity, employment status, health insurance status, marital status, and education level. They were asked to specify the reason for their visit to a health care provider in open text format, and to describe any diagnostic, treatment, or referral decisions made about their care at that visit. The final portion of the survey consisted of several widely-used, standardized self-report measures of decision-making: the Decisional Conflict Scale (DCS) (10), Autonomy Preference Scale (APS) (11), Shared Decision Making Questionnaire-9 (SDM-Q-9) (8), and Satisfaction with Decision (SWD) scale (6, 7). The standard 16-item version of the DCS was used to assess uncertainty in making a health-related decision, factors contributing to uncertainty, and perceptions of effective decision-making. Each item is rated on a 1 (strongly agree) to 5 (strongly disagree) scale. Higher scores indicate more decisional conflict. The Control (Autonomy) Preference Scale (APS) is a single-item measure of the extent to which the respondent wishes to exercise control in making a decision, rated on a 1 to 5 ordinal scale, with equally shared decision-making rated as a 3. A score of 1 indicates a preference for full patient autonomy in decision-making, while a score of 5 corresponds to preferring to have another make the entire decision. The SDM-Q-9 is a 9-item self-report measure assessing patient perceptions of the extent to which SDM occurred in a specific patient-provider consultation. The SDM-Q-9 is newly- validated and has been shown to have a unidimensional factor structure and high Cronbach alpha (α) internal consistency coefficients in German (.98) and U.S. (.94) populations. The items are rated on a 0 to 5 scale, with 0 indicating ‘completely disagree’ and 5 indicating ‘completely agree’. Higher scores indicate higher perceived levels of SDM during a patient-provider consultation. The SWD scale contains six items that assess patient satisfaction with a health care decision, rated on a 1–5 scale (1 strongly disagree; 5 strongly agree). Higher scores indicate higher satisfaction with decision. With the exception of the single-item APS measure, a raw sum score was computed for each decision-making measure, followed by transforming the raw sum scores to an in-common 0 to 100 scale for use in analyses.
2.3. Content coding of decisions
The types of decisions and reasons for health care consultations were content-coded to be able to compare this research to previous surveys (1, 2). Coding was performed for the two open-ended questions for the specific decision being made by the respondent: (1) “Please indicate which health complaint/problem/illness the consultation was about,” and (2) “Please indicate which decision was made.” The lead researcher (K.G.), in collaboration with a second researcher (C.W.), developed the initial categories into which the content could be appropriately divided, and did the initial coding. If a respondent indicated several reasons for visiting a health care provider, only those that were associated with a clear decision in the consultation pertaining to diagnosis, treatment, or referral were coded. The initial categories were discussed and refined with other research team members. Next, the third researcher (J.O), using the categories devised by the primary researcher, performed a second independent coding of the data. The results of the two separate coding efforts were then compared for concordance between the three researchers, and the inter-rater reliability was calculated to determine the initial and final raw percentage agreement among the two primary coders (K.G., J.O.). The initial interrater raw percentage reliability was 83%. Discussion of the areas of content coding where the researchers did not agree took place with the third researcher (C.W.) who was not otherwise involved in the coding process and aided in reaching decisions on the appropriate content code. Most coding discrepancies involved a coder making an inference from the data that could not be fully supported based on the available information. The subset of ‘not codable’ responses was also reviewed within the larger research team to reconfirm the coding decisions that were made. All coding discrepancies were able to be resolved via the discussion process, resulting in a final interrater reliability of 100%.
2.4. Scoring and analysis
Forward selection multiple linear regression analysis was used to model correlates of SWD. IBM SPSS V19.0.0 was used to analyze the sample descriptive statistics. The regression analysis and results for the weighted modeling were performed with the SURVEYREG procedure in SAS 9.2. For the regression modeling, two sociodemographic measures, race and education level, were converted into dichotomous categories. Race was condensed from six original categories to “white” and “not white”, and education level (originally with 7 categories) was dichotomized as “less than high school education” and “high school education or greater.” For the decision questionnaires (DCS, SDM-Q-9, and SWD), total raw scores were linearly transformed to an in-common 0–100 scale. The APS scale was not transformed to a 0–100 scale as reasonable interpretation of the raw score is possible. The dependent variable, SWD sum total score, was treated as a continuous variable.
3. Results
3.1. Sample characteristics
Table 1 displays the overall sample characteristics for socio-demographic variables. Figure 1 presents the study flow diagram. The obtained sample had similarities and some differences compared to the overall ResearchMatch population. The sample was somewhat higher on proportion of white respondents, lower on African-American respondents, and higher on Hispanic respondents compared to ResearchMatch (82%, 10%, 5%, respectively). The obtained sample had similar percentages to ResearchMatch for Asian, American Indian/Alaskan Native, and other racial groups. The sample was more evenly distributed on gender (64.7% female, 35.3% male) compared to ResearchMatch (73.0% female, 27.0% male). The only groups that fully met the target sample sizes were white and non-white non-Hispanic females. There are larger sampling deficits for men of all races and ethnicities due to their underrepresentation in ResearchMatch.
Table 1.
Sociodemographic Characteristics (n=488)
| Characteristic | N | % |
|---|---|---|
| Age (in years) | ||
| Mean 41.4; SD 13.3 | ||
| Race | 482 | |
| White | 410 | 85.1 |
| Black/African Descent | 31 | 6.4 |
| Asian | 20 | 4.1 |
| Other | 18 | 3.7 |
| American Indian/Alaskan Native | 3 | 0.6 |
| Ethnicity | 479 | |
| Non-Hispanic | 439 | 91.6 |
| Hispanic | 40 | 8.4 |
| Gender | 485 | |
| Female | 314 | 64.7 |
| Male | 171 | 35.3 |
| Employment Status | 481 | |
| Employed | 363 | 75.5 |
| Unemployed | 118 | 24.5 |
| Marital Status | 483 | |
| Married | 300 | 62.0 |
| Not Married | 183 | 38.0 |
| Education Level | 485 | |
| Graduate/Professional Degree | 182 | 37.5 |
| College (completed degree) | 132 | 27.2 |
| Some Graduate/Professional | 80 | 16.5 |
| Some College/Technical Training | 73 | 15.1 |
| High School (12th grade) | 17 | 3.5 |
| Some High School (<12th grade) | 1 | 0.2 |
3.2. Content coding categories
The ‘reason for visit’ responses were placed into one of 15 reasons for consultations categories (Table 2a), with a total 522 non-mutually-exclusive reasons for health consultations reported. The most frequent reason for consultation was for a musculoskeletal issue, followed by neurological and infection. The ‘type of decision’ responses were coded as diagnosis, treatment, or referral (Table 2b). Of the 562 codable health care decisions reported by survey respondents, the large majority were treatment decisions.
Table 2.
| a Content coding for the question, “Please indicate which health complaint/problem/illness the consultation was about” | ||
|---|---|---|
| Reason for Visit | N | % |
| Musculoskeletal | 91 | 18.6 |
| Neurological | 70 | 14.3 |
| Infection | 64 | 13.1 |
| Cardiovascular | 55 | 11.2 |
| Psychological | 51 | 10.4 |
| Gastrointestinal | 38 | 7.8 |
| Endocrinological | 34 | 7.0 |
| Dermatology | 33 | 6.8 |
| Reproductive | 22 | 4.5 |
| Pulmonary | 15 | 3.1 |
| Cancer | 13 | 2.7 |
| Weight Issue | 12 | 2.5 |
| Allergies | 11 | 2.3 |
| Urinary | 10 | 2.0 |
| Prevention | 3 | < 1.0 |
| b Content coding for the question, “Please indicate the decision made” | ||
|---|---|---|
| Type of Decision | N | % |
| Treatment | 402 | 82.4 |
| Diagnosis | 122 | 25 |
| Referral | 38 | 7.8 |
Ns are > 488 due to some participants reporting multiple reasons for consultations; percentage denominator is 522
Ns are > 488 due to some participants reporting multiple decisions; percentage denominator is 562
3.3. Descriptive statistics for standardized measures
Table 3 summarizes the total scores for the four standardized decision-making measures included in the survey. The majority (65.6%) indicated that their autonomy preference was a 2 on the 1 to 5 rating scale, corresponding with the response option, “I should make the decision on my own, but take others’ opinions into account.” The average SDM-Q-9 score showed that the mean of the sample was above the midpoint of the scale in their perceptions of the extent to which shared decision-making was present in their index health care consultation. The SWD total score was relatively high, reflecting that the average respondent was satisfied with rated health care decisions.
Table 3.
Descriptive Statistics for Decision-making Measures (n=488)
| Measure | N | Mean | SD |
|---|---|---|---|
| Autonomy Preference (APS)a | 462 | 2.3 | .62 |
| Decisional Conflict Scale (DCS) Total Scoreb | 472 | 37.1 | 31.0 |
| Shared Decision Making (SDM-Q-9) Total Scorec | 479 | 67.6 | 26.6 |
| Satisfaction with Decision (SWD) Total Scored | 473 | 76.7 | 19.6 |
1 – 5 ordinal scale:1 = preference for complete autonomy, 3 = preference for equally shared decision; 5 = preference for others to make the decision
0 – 100 scale; higher scores indicate higher decisional conflict
0 – 100 scale; higher scores indicate higher perceived shared decision-making
0 – 100 scale; higher scores indicate higher decision satisfaction
3.4. Regression modeling
Variables in addition to the SDM-Q-9 measure that were included in the initial linear regression model were: dichotomized race, gender, ethnicity, education level, marital status, and age, autonomy preference (APS), and standardized total scores for decisional conflict (DCS). Non-modifiable respondent characteristics (race, gender, ethnicity, education level, marital status, age, and APS) were controlled for by grouping them together in a block. DCS and SDM-Q-9 were conceptualized as potentially modifiable variables, and were added to the model after controlling for the non-modifiable variables.
The linear regression model (Table 4) revealed that total SDM-Q-9 score was a statistically significant predictor of SWD, p < 0.001. DCS total score approached statistical significance with a p-value of 0.09. While DCS displayed the expected negative relationship with SWD, i.e., higher decisional conflict was associated with lower decision satisfaction, the relatively small effect size was unexpected, and may be due to the negatively skewed distribution of DCS scores. Variance inflation factor (VIF) values for all variables in the model were at or around 1, suggesting little collinearity between them. The adjusted R2 value indicated that 36.8% of the variation in SWD was explained by the variables included in the model, and primarily by SDM-Q-9 score.
Table 4.
Multiple linear regression (dependent variable = SWD)
| Variable | β | SE(β) | t | Sig. (p) |
|---|---|---|---|---|
| (constant) | 49.520 | 6.151 | 8.05 | <.001 |
| Gender | 0.427 | 1.474 | 0.29 | 0.772 |
| Race (White/Non-White) | 0.598 | 2.199 | 0.27 | 0.786 |
| Employment (Employed/Not Employed) | 1.061 | 1.855 | 0.57 | 0.568 |
| Education Level (Less than High School/High School or greater) | 2.13 | 1.886 | 1.13 | 0.259 |
| Marital Status ( Married/Not Married) | 0.244 | 1.671 | 0.15 | 0.884 |
| Ethnicity (Hispanic/non-Hispanic) | −1.517 | 2.775 | −0.55 | 0.585 |
| Age (in years) | 0.032 | 0.062 | 0.51 | 0.612 |
| Autonomy Preference (APS) | −1.60 | 1.311 | −1.22 | 0.223 |
| Decisional Conflict Scale (DCS) Total Score | −0.042 | 0.025 | −1.71 | 0.089 |
| Shared Decision Making (SDM-Q–9) Total Score | 0.429 | 0.034 | 12.60 | <.001 |
Note: R2= .368
Because SDM-Q-9 total score was significantly associated with SWD, a second model was run on an exploratory basis to ascertain which items of the SDM-Q-9 were more or less strongly associated with SWD. This second model held all other variables and procedures the same as the previous model, except for the substitution of each of the nine individual item scores comprising the SDM-Q-9 questionnaire (Table 5). DCS was again marginally significant (p = 0.09) and displayed the expected negative association with SWD (Table 5). Of the 9 SDM-Q-9 items, 3 displayed significant, positive correlations: (a) Item 5 (“My doctor helped me understand all the information”), (b) Item 6 (“My doctor asked me which treatment I prefer”), and, (c) Item 7 (“My doctor and I thoroughly weighed the different treatment options”). The SDM-Q-9 individual items were somewhat collinear with VIF values ranging from 1.4 to 4.7, but not markedly increased over the initial model. Collinearity of the remaining variables remained low. In this exploratory model, p-values were examined only to quantify the potential strength of statistical significance and not as a strict testing exercise. In a formal testing event, only Item 5 (p < .001) would remain statistically significant based on a Bonferroni adjustment.
Table 5.
Multiple linear regression with individual SDM-Q-9 items (dependent variable = SWD)
| Variable | β | SE(β) | t | Sig. (p) |
|---|---|---|---|---|
| (constant) | 50.551 | 6.399 | 7.90 | <.001 |
| SDM-Q-1: My doctor made clear that a decision needs to be made |
0.177 | 0.652 | 0.27 | 0.787 |
| SDM-Q-2: My doctor wanted to know exactly how I wanted to be involved in making the decision |
−0.884 | 0.822 | −1.08 | 0.283 |
| SDMQ-3: My doctor told me that there are different options for treating my medical condition |
−1.049 | 0.665 | −1.58 | 0.115 |
| SDMQ-4: My doctor precisely explained the advantages and disadvantages of the treatment options |
−0.028 | 0.886 | −0.03 | 0.975 |
| SDMQ-5: My doctor helped me understand all of the information |
3.554 | 1.075 | 3.31 | 0.001 |
| SDMQ-6: My doctor asked me what treatment option I prefer |
2.063 | 0.982 | 2.10 | 0.036 |
| SDMQ-7: My doctor and I thoroughly weighed the different treatment options |
2.435 | 1.186 | 2.05 | 0.041 |
| SDMQ-8: My doctor and I selected a treatment option together |
0.514 | 0.956 | 0.54 | 0.591 |
| SDMQ-9: My doctor and I reached an agreement on how to proceed |
1.756 | 1.075 | 1.63 | 0.103 |
Note: R2= .410
4. Discussion and Conclusion
4.1. Discussion
As hypothesized, SDM-Q-9 score was positively associated with SWD. By identifying factors such as SDM that may increase satisfaction with decisions, this can support improved intervention approaches to encourage patients to be involved in their own care, including collaboration on health management plans that they will be more likely to follow if they are satisfied with their decisions. Although there are many factors that contribute to whether or not patients are satisfied with their care, one aspect of satisfaction with a health care experience is clearly the quality of interaction during decision-making with the health care provider. If SDM can improve the quality of that interaction, the result of this study is consistent with the premise that SWD may lead to improved adherence by increasing overall satisfaction with care.
The regression model in which the individual items of the SDM-Q-9 were used instead of the total score was done on an exploratory basis, to examine if some items were more associated with SWD than others. While only three of the nine items on the SDM-Q-9 were significantly correlated with SWD, it is of interest that the nine items have such a wide range of association with SWD, including some that were not significantly associated with SWD. The significant association of SWD with these three SDM-Q-9 items is consistent with prior research, linking understanding of what matters to the patient for their overall satisfaction with their health care encounter. However, the statistical modeling accomplished in this study is a more explicit examination of the relationship of these individual aspects of SDM to SWD compared to previous research. The reported results allow a deeper look into what patients perceive makes SDM a desirable approach in health care consultations. The implication from the data is that some aspects of SDM may be more highly valued than others. Interestingly, the highest correlation with SWD was with “doctor helped to understand information.” The two other significant items: patient’s preference of treatment option, and weighing different options together, had significant associations with SWD, while “selecting a treatment option together” and “reaching an agreement” did not. This seems to suggest that once patients understand the information, having the ability to choose increases their SWD, while making decision together with the health provider does not. Perhaps in the future, a shorter version of the SDM-Q-9 questionnaire might be developed that retains strong psychometric properties and effectiveness in predicting health care outcomes. More research regarding how each of the nine items relate to a broader range of outcomes is recommended.
The analysis of the decision content coding demonstrates the diversity of the type of decisions being made, which is consistent with prior North American national surveys (1, 2). This study provides detail about specific elements of shared decision-making that were perceived as present by examining the individual components of the SDM-Q-9 scale. In addition, a more recent timeframe for decision-making was examined (past 3 months), which is substantially briefer compared to prior national surveys.
There were several limitations to this study. Although not central to the purpose of the study, the relationship between SDM and adherence was not assessed in the larger cross-sectional survey study to validate the SDM-Q-9 scale in a U.S. population. A more definitive test of a causal relationship between SDM and adherence would require a longitudinal experimental design. Self-reported adherence for the timeframe of the study recall period (past 3 months) could be challenging to analyze due to the wide variety of decisions and acute and chronic health conditions contexts reported by respondents. Recall bias could have influenced survey responses otherwise, as respondents were asked to retrospectively recall a health-related decision. However, this window of time is relatively small, and is substantially briefer compared to two previous national surveys (1, 2). Lastly, the sample was relatively well-educated and 95% reported having at least some health insurance. These variables could account in part for the relatively high overall level of satisfaction with health decisions reported in this study and show that the sample was not fully representative of the total U.S. population. Because ResearchMatch is an online database, the ability to participate and learn about studies is limited to those who can access an Internet-equipped computer. There may also be a selection bias of the population based on their interest in medical research that could explain the relatively high percentage of SWD. ResearchMatch is being implemented at a number of academic medical institutions nationwide, but some states and regions contain many more volunteers than others. Nonetheless, the obtained sample represents users of health care services for whom research on shared decision-making is relevant. Results are similar to prior national surveys in terms of the extent to which respondents reported being involved in decision-making, and in the wide range of decisions and health care issues represented in their survey responses. Thus, although the study population may not be representative of the U.S. as a whole, the results still provide valuable insights on the relationship between SDM and SWD, and are relevant to populations that seek health care services.
4.2. Conclusion
The statistical modeling strategy identified factors correlated with SWD, especially SDM and specific aspects of the SDM questionnaire. These findings are consistent with the adapted model, in that we were able to document a hypothesized relationship between SDM and SWD. More research on the effects of shared decision-making on patient satisfaction is encouraged, as is research on the relationship between shared decision-making and adherence (via attitudes), for both chronic and acute conditions, and for a wide variety of individuals and populations.
4.3. Practice implications
By identifying variables such as SDM that are significantly associated with satisfaction in a health care decision, the public health and broader health care communities can better target potentially modifiable variables to enhance decision satisfaction and clinical outcomes.
Acknowledgements
The authors thank Drs. Amy Ferketich and Randi Foraker of The Ohio State University College of Public Health for their reviews of earlier drafts of this manuscript. The results reported in this manuscript were used in the lead author’s Master of Public Health (MPH) Culminating Project, completed in partial fulfillment of requirements for the MPH degree. Portions of the results were presented at the June 2011 International Shared Decision Making Conference in Maastricht, The Netherlands. The project was supported by the resources of Award Number UL1RR025755 to the Ohio State University Center for Clinical Translational Science from the U.S. National Center for Research Resources. The content is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. National Center for Research Resources of the National Institutes of Health.
The authors confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Katherine Elizabeth Glass, The Ohio State University, 1585 Neil Avenue, Columbus, OH 43210. Telephone: 614.292.4524. FAX: 614.292.7976..
Celia E. Wills, Associate Professor & Sills Professor in Interdisciplinary Behavioral Health Nursing, The Ohio State University College of Nursing, Columbus, Ohio U.S.A. wills.120@osu.edu
Christopher Holloman, Auxiliary Associate Professor, The Ohio State University Department of Statistics, Columbus, Ohio U.S.A.
Jacklyn Olson, Honors Baccalaureate Student in Nursing, The Ohio State University College of Nursing, Columbus, Ohio U.S.A..
Catherine Hechmer, Master’s Student in Clinical Social Work, The Ohio State University College of Social Work, Columbus, Ohio U.S.A.
Carla K. Miller, Associate Professor, The Ohio State University Department of Human Nutrition, Columbus, Ohio U.S.A.
Anne-Marie Duchemin, Research Scientist, Associate Professor Adjunct, The Ohio State University Department of Psychiatry, Columbus, Ohio U.S.A.
References
- 1.Zikmund-Fisher BJ, Couper MP, Singer E, Levin CA, Fowler FJ, Ziniel S, et al. The DECISIONS study: a nationwide survey of United States adults regarding 9 common medical decisions. Med Dec Making. 2010;30:20S–34S. doi: 10.1177/0272989X09353792. [DOI] [PubMed] [Google Scholar]
- 2.O'Connor AM, Drake ER, Wells GA, Tugwell P, Laupacis A, Elmslie T. A survey of the decision-making needs of Canadians faced with complex health decisions. Health Expect. 2003;6:97–109. doi: 10.1046/j.1369-6513.2003.00215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes two to tango) Soc Sci Med. 1997;44:681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 4.Stalmeier PFM T. Adherence and decision aids: a model and a narrative review. Med Dec Making. 2010;31:121–9. doi: 10.1177/0272989X10370487. [DOI] [PubMed] [Google Scholar]
- 5.Stacey D, Bennett CL, Barry MJ, Col NF, Eden KB, Holmes-Rovner M, et al. Decision aids for people facing health treatment or screening decisions. Coch Database Syst Rev. 2011;(10) doi: 10.1002/14651858.CD001431.pub3. [DOI] [PubMed] [Google Scholar]
- 6.Holmes-Rovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML, et al. Patient satisfaction with health care decisions: the Satisfaction With Decision Scale. Med Dec Making. 1996;16:58–64. doi: 10.1177/0272989X9601600114. [DOI] [PubMed] [Google Scholar]
- 7.Wills CE, Holmes-Rovner M. Preliminary validation of the satisfaction with decision scale with depressed primary care patients. Health Expect. 2003;6:149–59. doi: 10.1046/j.1369-6513.2003.00220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kriston L, Scholl I, Holzel L, Simon D, Loh A, Harter M. The 9-item shared decision making questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Pat Educ Couns. 2010;80:94–99. doi: 10.1016/j.pec.2009.09.034. [DOI] [PubMed] [Google Scholar]
- 9.Wills CE, Glass KE, Holloman C, Hechmer C, Olson J, Miller C, et al. Validation of the shared decision-making questionnaire-9 (SDM-Q-9) in a stratified, age-proportionate U.S. sample. International Shared Decision-Making (ISDM) Conference; The Netherlands: Maastricht; 2011. [Google Scholar]
- 10.O'Connor A. Validation of a decisional conflict scale. Med Dec Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 11.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Can J Nsg Res. 1997;29(3):21–43. [PubMed] [Google Scholar]