Abstract
Ectopic hepatocellular carcinoma (HCC) is a very rare clinical entity that is defined as HCC arising from extrahepatic liver tissue. This report presents a case of ectopic multiple HCC arising in the abdominal cavity. A 42-year-old otherwise healthy male presented with liver dysfunction at a general health checkup. Both HCV antibody and hepatitis B surface antigen were negative. Laboratory examination showed elevations in serum alpha-fetoprotein and PIVKA-II. Ultrasonography and computed tomography revealed multiple nodular lesions in the abdominal cavity with ascites without a possible primary tumor. Exploratory laparoscopy was performed, which revealed bloody ascites and multiple brown nodular tumors measuring approximately 10 mm in size that were disseminated on the perineum and mesentery. A postoperative PET-CT scan was performed but it did not reveal any evidence of a tumor in the liver. The tumors resected from the peritoneum were diagnosed as HCC. The present case of HCC was thought to have possibly developed from ectopic liver on the peritoneum or mesentery.
Key words: Hepatocellular carcinoma, Ectopic liver, Ectopic hepatocellular carcinoma, Abdominal cavity
Introduction
Ectopic liver tissue develops at various sites near the liver, such as the gallbladder, intra-abdominal ligaments, omentum, retroperitoneum and thorax [1, 2, 3]. The incidence of ectopic liver tissue has been reported to be 0.24–0.47% [3, 4]. Ectopic liver is a very rare entity, usually asymptomatic, but occasionally it causes unexpected problems such as intra-abdominal bleeding at the site of origin and hepatocarcinogenesis. Hepatocellular carcinoma (HCC) arising from ectopic liver is even more rare; only 26 cases have been reported in Japan. Multiple ectopic HCC arising in the abdominal cavity has been reported in only 3 cases, including the present case, and its PET-CT findings have never been reported. This report presents a case of HCC that disseminated in the abdominal cavity and probably developed from ectopic liver tissue present on the peritoneum.
Case Report
A 42-year-old otherwise healthy male presented with liver dysfunction at a general health checkup. Although he had been aware of general fatigue recently, there was no other condition such as fever, diarrhea or appetite loss with nausea and vomiting. His medical history revealed no specific problems. We detected no significant changes in his feeding habits. He liked Japanese food and the amount of intake was normal. He had no history of alcohol abuse, and his family history was noncontributory. On admission, his abdomen was soft, without palpable masses. Both HCV antibody and hepatitis B surface antigen were negative. His laboratory results were generally unremarkable, including levels for CEA and CA19-9. However elevations in serum AST (117 U/I), ALT (254 U/I), alpha-fetoprotein (241 ng/ml) and PIVKA-II (69,349 mAU/ml) were shown. There were no specific findings in the gastrointestinal tract on endoscopic examination.
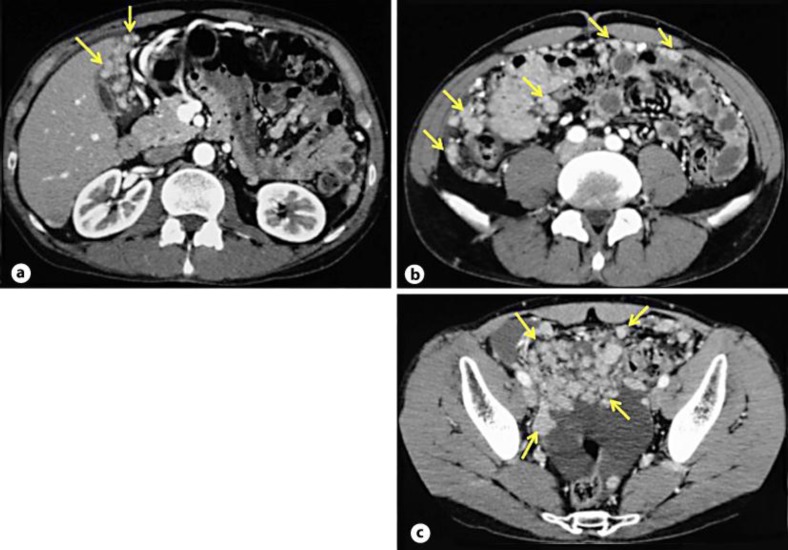
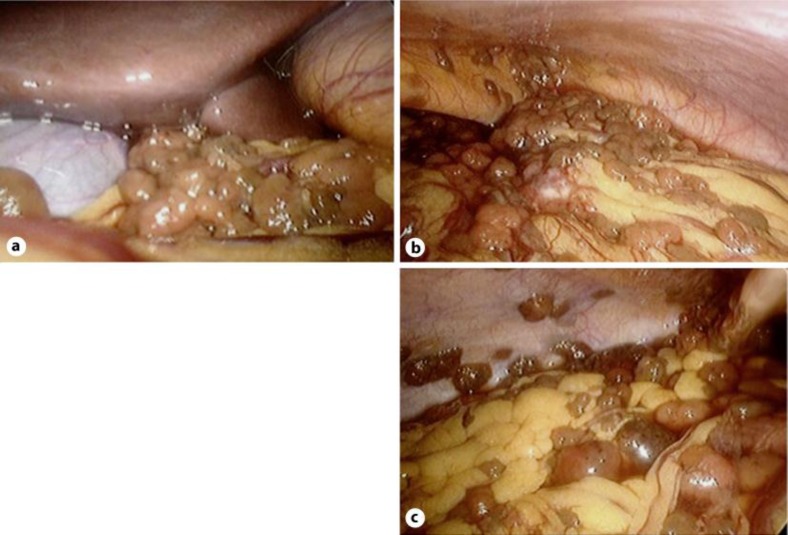
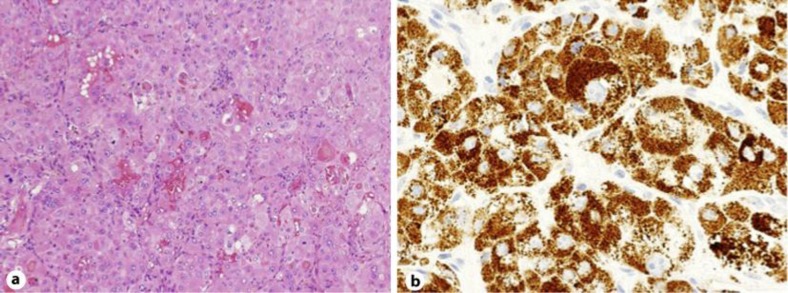
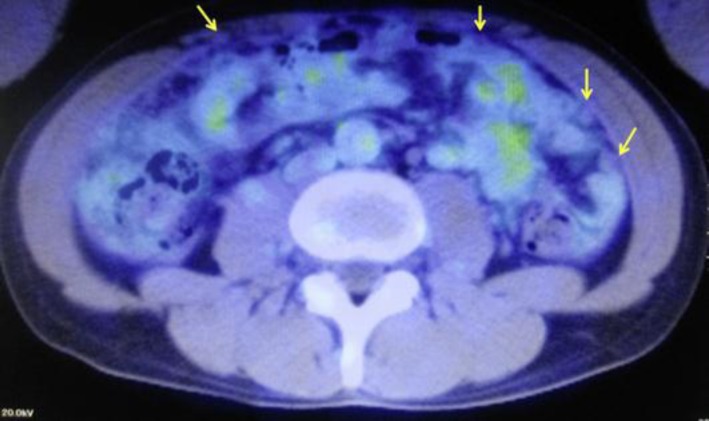
Computed tomography revealed multiple nodular lesions in the abdominal cavity with ascites but no other possible primary tumor (fig. 1). No lesion was found in the liver. For peritoneal dissemination of unknown primary lesion, exploratory laparoscopy was performed which revealed bloody ascites and multiple brown nodular tumors measuring approximately 10 mm in size that were disseminated on the peritoneum and mesentery (fig. 2). In microscopic examination, tumor cells resected from the peritoneum showed nodular lesion composed of atypical hepatocyte forming irregular trabecular or pseudoglandular structures with focal intraluminal or intracytoplasmic bile pigments. The atypical cells showed swollen and various-sized nuclei, distinct nucleoli and eosinophilic cytoplasm (fig. 3a). Immunohistochemical staining of the tumor cells revealed positive anti-human hepatocyte (fig. 3b). The final diagnosis was moderately differentiated HCC arising from ectopic liver tissue. A postoperative PET-CT scan was performed but it did not reveal any evidence of a tumor in the native liver (fig. 4). The patient is currently receiving chemotherapy for HCC.
Fig. 1.
Computed tomography revealed multiple nodular lesions (arrows) in the abdominal cavity with ascites. a Inferior surface of the liver. b Upper abdomen. c Lower abdomen.
Fig. 2.
Exploratory laparoscopy was performed which revealed the presence of bloody ascites and multiple brown nodular tumors measuring approximately 10 mm in size that were disseminated on the peritoneum and mesentery. a Inferior surface of the liver. b Upper abdomen. c Lower abdomen.
Fig. 3.
Microscopic examination of the tumor confirmed moderately differentiated HCC. a Tumor cells resected from the peritoneum showed nodular lesion composed of atypical hepatocyte forming irregular trabecular or pseudoglandular structures. HE stain, 100×. b Immunohistochemical staining of the tumor cells revealed positive anti-human hepatocyte. 400×.
Fig. 4.
A postoperative PET-CT scan was performed but it did not reveal any evidence of tumor in the native liver. The arrows indicate multiple nodular lesions (SUVmax: 1.5).
Discussion
Anomalous liver is classified into four types: accessory liver lobe, small accessory lobe, ectopic liver, and ectopic liver tissue. We distinguish between ectopic liver, which is outside the liver proper without any connection to it, and accessory liver, which is connected to the liver, often by a stalk [5]. Ectopic livers are islands of normal liver parenchyma separated from the main lobes of the liver and can occur at various sites near the liver, such as the gallbladder, intra-abdominal ligaments, omentum, retroperitoneum and thorax [1, 2, 3]. Ectopic liver is usually found incidentally, but it may also be found because of neoplastic change or compressive effects. Most ectopic livers seem to be more prone to hepatocarcinogenesis [6]. The common risk factors for HCC, such as infection with hepatitis B or C and cirrhosis, appear to be less implicated; only 32% of ectopic HCCs are reported to be associated with cirrhosis [7]. A diagnosis of ectopic HCC requires the identification of noncancerous liver parenchyma around the mass lesion [8]. It is possible that ectopic or accessory livers are subjected to specific additional carcinogenic factors, independent of the mother liver, as a result of their poor blood supply and biliary drainage secondary to their abnormal location [9]. Ectopic HCCs are surgically resected if possible, with a favorable prognosis. The resection of an ectopic HCC can be curative because the carcinogenetic potential of these tumors is usually limited to the ectopic liver itself [7].
A review of the pertinent literature suggests that approximately 21 cases of primary HCC in ectopic liver have been reported to date, and most of these case reports are from Japan [6, 7, 10, 11]. These case reports described the occurrence of HCC in the ectopic liver and one report described the occurrence of HCC within both the ectopic liver as well as the native liver [7]. HCC seems to evolve in ectopic liver tissue several years prior to that in the native liver because small ectopic liver tissue does not have a complete architecture and may be handicapped metabolically, which accelerates the carcinogenetic process [7]. Asymptomatic hepatitis B infection and excessive consumption of tobacco and/or alcohol are among the better-known predisposing factors for the development of primary HCC in the inhabitants of Asia [12]. The presence of these etiological factors might hasten the process of carcinogenesis within the ectopic liver tissue.
Ultrasonography and computed tomography revealed multiple nodular lesions in the abdominal cavity with ascites in the current patient, but no other possible primary tumor. Laboratory examination showed elevations in serum AST (117 U/I), ALT (254 U/I), alpha-fetoprotein (241 ng/ml) and PIVKA-II (69,349 mAU/ml). The present case was preoperatively diagnosed to have HCC that probably originated from an ectopic liver in the abdominal cavity. Exploratory laparoscopy was performed which revealed bloody ascites and multiple brown nodular tumors disseminated on the perineum and mesentery. The final diagnosis of the tumor resected from the peritoneum was moderately differentiated HCC. The tumors probably arose from ectopic liver on the peritoneum or mesentery, and thereafter became disseminated in the abdominal cavity. A postoperative search for primary malignancy within the mother liver was done with the help of a PET-CT scan but it did not reveal any evidence of tumor in the native liver.
In conclusion, this report presents a rare case of multiple ectopic HCCs arising in the abdominal cavity. The patient is currently receiving chemotherapy for HCC.
References
- 1.Kawahara E, Kitamura T, Ueda H, Ogino T, Mai M, Ooi A, Nakanishi I. Hepatocellular carcinoma arising in the abdominal cavity. An autopsy case of ectopic liver origin. Acta Pathol Jpn. 1988;38:1575–1581. doi: 10.1111/j.1440-1827.1988.tb02297.x. [DOI] [PubMed] [Google Scholar]
- 2.Leone N, De Paolis P, Carrera M, Carucci P, Musso A, David E, Brunello F, Fronda GR, Rizzetto M. Ectopic liver and hepatocarcinogenesis: report of three cases with four years’ follow-up. Eur J Gastroenterol Hepatol. 2004;16:731–735. doi: 10.1097/01.meg.0000131044.05434.f7. [DOI] [PubMed] [Google Scholar]
- 3.Watanabe M, Matsura T, Takatori Y, Ueki K, Kobatake T, Hidaka M, Hirakawa H, Fukukmoto S, Shimada Y. Five cases of ectopic liver and a case of accessory lobe of the liver. Endoscopy. 1989;21:39–42. doi: 10.1055/s-2007-1012892. [DOI] [PubMed] [Google Scholar]
- 4.Kanzaki R, Yamada T, Gotoh K, Takahashi H, Ohigashi H, Ishikawa O. Ectopic hepatocellular carcinoma arising in the left triangular ligament of the liver. Case Rep Gastroenterol. 2010;4:138–143. doi: 10.1159/000314042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collan Y, Hakkiluoto A, Hastbacka J. Ectopic liver. Ann Chir Gynaecol. 1978;67:27–29. [PubMed] [Google Scholar]
- 6.Kim KA, Park CM, Kim CH, Choi SY, Park SW, Hong SJ, Seol HY, Cha IH. Hepatocellular carcinoma in an ectopic liver: CT findings. Eur Radiol. 2003;13((suppl 4)):L45–L47. doi: 10.1007/s00330-003-1908-6. [DOI] [PubMed] [Google Scholar]
- 7.Arakawa M, Kimura Y, Sakata K, Kubo Y, Fukushima T, Okuda K. Propensity of ectopic liver to hepatocarcinogenesis: case reports and a review of the literature. Hepatology. 1999;29:57–61. doi: 10.1002/hep.510290144. [DOI] [PubMed] [Google Scholar]
- 8.Takayasu K, Itabashi M, Moriyama N. Case report: ectopic hepatocellular carcinoma arising from the left diaphragm. Clin Radiol. 1994;49:579–581. doi: 10.1016/s0009-9260(05)82944-7. [DOI] [PubMed] [Google Scholar]
- 9.Caygill CP, Gatenby PA. Ectopic liver and hepatocarcinogenesis. Eur J Gastroenterol Hepatol. 2004;16:727–729. doi: 10.1097/01.meg.0000131037.92864.df. [DOI] [PubMed] [Google Scholar]
- 10.Lasser A, Wilson GL. Ectopic liver tissue mass in the thoracic cavity. Cancer. 1975;36:1823–1826. doi: 10.1002/1097-0142(197511)36:5<1823::aid-cncr2820360537>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 11.Algin C, Yaylak F, Olgun EG, Caglikulekci M. Laparoscopic removal of an incidental ectopic liver: short report of a case. Case Rep Gastroenterol. 2008;2:134–137. doi: 10.1159/000121283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raoul JL. Natural history of hepatocellular carcinoma and current treatment options. Semin Nucl Med. 2008;38:S13–S18. doi: 10.1053/j.semnuclmed.2007.10.004. [DOI] [PubMed] [Google Scholar]