Abstract
Objective
To assess the effectiveness of intrauterine local anesthesia in reducing pain associated with outpatient gynecologic procedures.
Data Sources
We searched online databases PubMed or MEDLINE, Embase, Google Scholar, and Clinicaltrials.gov, and hand-searched reference lists from reviews evaluating pain control methods for gynecologic office procedures. We identified randomized controlled trials using intrauterine local anesthetic in gynecologic procedures.
Methods
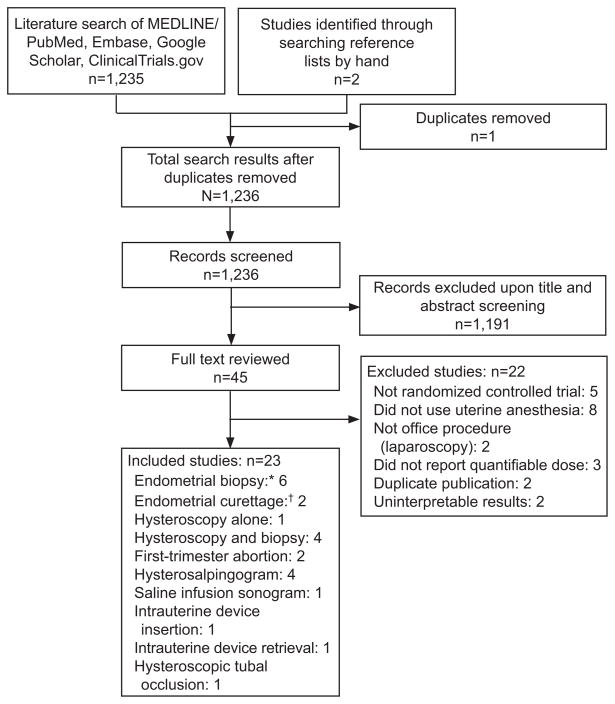
Titles and abstracts were screened for 1,236 articles. We identified 45 potential articles for inclusion. We excluded 22 of these studies because: 1) they were not randomized controlled trials; 2) they did not describe a quantifiable dose of medication used in the study; 3) they did not investigate an intrauterine anesthetic; 4) they did not study a potentially awake, outpatient procedure; and 5) they did not clearly report results or represented duplicate publication. Twenty-three articles were ultimately included for review.
Tabulation, Integration, and Results
Two authors independently reviewed full search results and assessed eligibility for inclusion, and independently abstracted data from all articles that met criteria for inclusion. Disagreements regarding eligibility or abstraction data were adjudicated by a third independent person. Our primary endpoint was reported effect of intrauterine local anesthesia on patient-reported pain scores. Due to heterogeneity in study methods, outcome measures, and reporting of outcomes, results could not be combined in a meta-analysis. Good evidence supports use of intrauterine anesthesia in endometrial biopsy and curettage, as five good-quality studies reported reduced pain scores while only one good-quality study reported negative results. We found moderate evidence to support intrauterine anesthesia in hysteroscopy, as one good-quality study and two fair or poor quality studies reported reduced pain scores, while two good-quality studies had negative results. Good evidence suggests that intrauterine anesthesia is not effective in hysterosalpingography; three good-quality studies reported that pain scores were not reduced, and no good quality studies showed beneficial effect in that procedure.
Evidence was insufficient concerning first-trimester abortion, saline-infusion sonogram, tubal sterilization, and intrauterine device insertion.
Conclusion
Intrauterine local anesthesia can reduce pain in several gynecologic procedures including endometrial biopsy, curettage, and hysteroscopy, and may be effective in other procedures as well.
INTRODUCTION
A major obstacle to the successful completion of outpatient gynecologic procedures is pain management. Most patients can tolerate pain to complete necessary procedures but studies show that pain scores are often high.. Cervical biopsy and cervical curettage are associated with visual analogue scale (VAS) pain scores ranging from four to six on a 10-point scale.(1, 2) Endometrial biopsies done have VAS scores of five to seven(3, 4). Pain with intrauterine device (IUD )insertion varies from two to seven, (5–8) and pain scores during laminaria insertions with paracervical block range from five to seven. Recent Cochrane reviews have evaluated the existing literature regarding pain control for hysteroscopy, first trimester abortion, IUD insertion and hysterosalpingography (HSG), and have concluded that optimal methods for pain control are unclear. (9–12)
Innervation of the uterus and cervix is complex. Major autonomic nerves arise from the S2–S4 roots and travel to the uterus in the lower portion of the broad ligament as the Frankenhauser plexus. (13) Interruption of this plexus is the basis of the paracervical block. However, the uterus is richly innervated with nerves that originate at other points as well. Alternative methods of local anesthesia targeting other nerve plexuses may improve pain management in procedures.
One promising form of anesthesia is intrauterine local anesthesia. As early as the 1970’s a report of the use of 1% lidocaine as an intrauterine anesthetic found that pain relief was satisfactory. (14) Since then, this technique has been investigated in multiple trials. We performed a systematic review of the current literature evaluating the effectiveness of intrauterine local anesthesia to reduce patient pain with common gynecologic office procedures.
SOURCES
We performed a comprehensive search of the PubMed or MEDLINE, Embase, Google Scholar, and ClinicalTrials.gov online databases for the years 1975–2012 for studies reporting use of intrauterine local anesthesia. The following search strategy using MeSH and non-MeSH terms was used to identify relevant human studies published in the English language: (analgesia OR anesthesia OR anesthetic OR anesthetic, local OR lidocaine OR bupivacaine OR mepivacaine OR pain measurement) AND (intrauterine OR intracervical OR intravaginal OR instillation, drug OR topical) AND (biopsy OR intrauterine device OR abortion, induced OR hysterosalpingography OR ultrasonography OR hysteroscopy OR curettage OR saline infusion sonogram OR sterilization, tubal OR endometrial ablation). In addition, we hand-searched reference lists from five review articles about pain management in gynecologic office procedures and reviewed any additional studies identified for eligibility.
STUDY SELECTION
We included studies confirmed to be randomized controlled trials which enrolled women undergoing gynecologic office procedures including endometrial biopsy, cervical biopsy, dilation and curettage, hysteroscopy, abortion, saline-infusion sonogram, hysterosalpingogram (HSG), IUD insertion or IUD removal. Studies investigated the use of liquid or gel local anesthetic instilled transcervically into the uterine cavity and compared this regimen to either placebo or another medication. The primary outcome of interest in each study was quantitative patient report of procedure-related pain using any standardized numeric scale. Studies did not have to be blinded for inclusion. We excluded studies that were not randomized trials, did not specify the dose of medications used, used general intravenous sedation while performing procedures, or involved a procedure not typically done in the outpatient office (such as laparoscopy).
Only studies published in English were included. If two publications seemed to be duplicate publication based on authors, institution and description of study population, only one of the studies was included. When publications represented an overlapping population (e.g. a large study which included patients from a previously reported smaller sample), only the larger study was included. Studies which reported results in an unclear manner, such that the study and statistical methods could not be understood, or that the stated conclusions could not be fully supported by the results as reported, were also excluded.
Our search identified 1237 potential studies for inclusion; after removal of duplicate studies, 1,236 remained for review. (Figure 1) Two authors independently reviewed search results, and all of these studies were screened by title and abstract review. We excluded 1,191 studies after screening. Full text was reviewed for 45 articles. When the two authors disagreed on inclusion, an independent third person reviewed the studies in question. Of the 45 full text articles, 22 were excluded. Twenty-three articles were ultimately included in our analysis.
Figure 1.
Summary of study selection. *Performed with Pipelle or Vabra device. †Sharp curettage with Sims curette.
Both authors independently assessed quality of included studies. Reports were evaluated for report and adequacy of randomization, allocation concealment, blinding of participants and providers, and quality of outcome measures. “Good” quality studies demonstrated adequate randomization, allocation concealment and blinding of all subjects and investigators, with minimal potential for bias. “Fair” quality studies lacked at least one of those factors, and had moderate potential for bias. “Poor” quality studies did not report allocation concealment and either participants or providers were unmasked as to treatment, with substantial potential for bias.
RESULTS
In the 23 studies included for analysis, pain control with intrauterine anesthetic was evaluated in several different procedures. (Figure 1) The studies were all similar in the described method of administering the local anesthetic, generally with a flexible plastic catheter inserted into the cervical canal. Most studies administered the drug two or three minutes before beginning the planned procedure.
The studies differed in many other aspects (Tables 1–4). Studies varied in the type of local anesthetic used, dose of anesthetic, number of study arms, overall design (parallel or factorial), and what comparator was used, whether placebo, other local block, or systemic oral medication. Studies also differed in both measurement and report of primary outcome. Multiple outcome scales were used (10cm VAS, 20cm VAS, and 4, 5, 6 or 7 point verbal response scales). Pain measurements were taken a different times across studies, ranging from one measurement during the procedure to a total of seven measurements prior, during, and after procedures. The studies also reported the outcome of pain differently. While most compared difference in mean or median pain score between intervention and control groups, several instead compared proportions of patients who reported pain above a pre-defined cut-point. Due to this heterogeneity in methods and reporting, results could not be accurately combined in a meta-analysis.
Table 1.
Intrauterine Anesthesia in Endometrial Biopsy or Curettage
| Study | Procedure | Patients (n) | Intrauterine Medication, Dose | Comparator | Reduced Pain? | Pain Difference | Study Quality | Comments |
|---|---|---|---|---|---|---|---|---|
| Trolice 200023 | Endometrial biopsy | 41 | 2% lidocaine 5mL | Saline | Yes | 50 mm 200mmVAS |
Good | |
| Dogan 200424 | Endometrial biopsy | 120 | 2% lidocaine 5mL |
* Saline placebo * Oral NSAID |
Yes | 25 mm 100mm VAS |
Fair | Significant reduction in pain between double medication and double placebo. Pain reduced with only intrauterine lidocaine alone compared to double placebo, but not significant |
| Guney 200626 | Endometrial biopsy | 107 | 2% lidocaine 5mL | Saline placebo | Yes | 24% reduction in pain score 100mmVAS |
Good | All patients received 200mcg misoprostol; if tenaculum used, 5mL lidocaine also injected in anterior lip of cervix. Only reported exact numeric pain scores for subgroup analysis |
| Hui 200627 | Endometrial aspiration | 200 | 2% lidocaine 5mL | Saline placebo | Yes | 19 mm 100mmVAS |
Good | Reduced pain during suction procedure, not at other time points |
| Api 201029 | Endometrial curettage | 111 | 2% lidocaine 5mL |
* Saline placebo * Oral NSAID |
Yes | 28 mm 100mmVAS |
Good | Reduced pain between all interventions and double placebo. Intrauterine lidocaine alone did not reduce pain more than NSAID alone |
| Rattanachaiyonont 200530 | Endometrial curettage | 70 | 2% lidocaine 5mL | Yes | 25% fewer reported moderate/severe pain 100mmVAS |
Good | All patients received paracervical block. Reduced pain during endocervical curettage and uterine curettage. Reported as proportion of patients reporting pain score greater than 4. | |
| Einarsson 200525 | Endometrial biopsy | 88 | 20% benzocaine spray† | Saline placebo | No | Good | Dosed as “1/2 second spray”; equivalent to 60mg. 60mg applied to lip of cervix, 60mg sprayed in endocervical canal. | |
| Kozman 200128 | Endometrial aspiration | 328 | 2% lidocaine gel 10 mL | Inert gel placebo | No | Fair | Reported results as proportion of patients with pain score greater than 6 on 10pt scale |
VAS, visual analog scale; NSAID, nonsteroidal anti-inflammatory drugs.
Factorial design.
Benzocaine spray is currently not recommended for use in outpatient settings due to risk of methemoglobenemia
Table 4.
Intrauterine Anesthetic in Abortion and Contraceptive Procedures
| Study | Procedure | Patients (n) | Intrauterine Medication, Dose | Comparator | Reduced Pain? | Pain Difference | Study Quality | Comments |
|---|---|---|---|---|---|---|---|---|
| Edelman 200441 | First- trimester abortion | 80 | 1% lidocaine 10mL | Saline placebo | No | Good | All patients received oral NSAID and some received oral benzodiazepine; rates of sedative use similar in both groups | |
| Edelman 200642 | First- trimester abortion | 80 | 4% lidocaine 5mL | Saline placebo | Yes | 28 mm 100mmVAS | Good | All patients received oral NSAID and some received oral benzodiazepine; rates of sedative use similar in both groups. More side effects seen in intervention group, no adverse events or toxicity. |
| Oloto 199743 | IUD insertion | 103 | 2% lidocaine gel 1.5mL | Saline placebo*, None* | YES | †23% fewer reported moderate or severe pain† | Fair | Dose varied between patients, 1mL to 1.5mL of gel used. Results reported as proportion of patients with moderate or severe pain. Significant reduction in pain when placebo and no-intervention groups combined |
| Guney 200644 | IUD retrieval | 68 | 2% lidocaine gel 5mL | Saline placebo | Yes | 20 mm 100mmVAS | Good | Intrauterine medication instilled 10 minutes before procedure |
| Isley 201245 | Hysteroscopic tubal occlusion | 58 | 4% lidocaine 5mL | Saline placebo | No | Good | All patients received paracervical block, oral NSAID and oral benzodiazepine |
NSAID, nonsteroidal anti-inflammatory drugs; VAS, visual analog scale IUD, intrauterine device.
Parallel design.
7-point verbal scale.
Eight studies evaluated pain control in endometrial biopsy or curettage without hysteroscopy. (Table 1) Four studies involved biopsy with a biopsy cannula,(15–18) two used biopsy with a vacuum aspirator,(19, 20) and two reported on curettage with a sharp Sims curette.(21, 22) All studies used a saline placebo comparator. Six studies involved two groups (IU anesthetic and placebo) while two studies had four groups, comparing lidocaine, saline, oral non-steroidal anti-inflammatory drugs and oral placebo in a factorial design. Six studies were rated as good quality and two were fair quality.
Overall, six studies enrolling a total of 649 patient reported a significant reduction in pain score during biopsy or curettage with intrauterine anesthesia; of these, five were good quality. The fair quality study did not describe techniques for allocation concealment or blinding, so potential for bias was difficult to assess. The two studies with indeterminate results differed in exact procedure (cannula biopsy and vacuum aspiration) and medication used (100mg of lidocaine and 60mg benzocaine); both were of good quality.
Five studies evaluated pain control in hysteroscopy (Table 2). Only one studied hysteroscopy alone;(23) the remainder evaluated hysteroscopy with endometrial biopsy or aspiration.(24–27) These studies were similar in outcome measure used (100mm VAS), but differed in number and timing of pain score measurements. They were also heterogeneous in the type and dose of medication studied (mepivacaine and lidocaine). One study pre-medicated all subjects with 400 mcg of misoprostol, but no adjunctive medications were used in the other studies.
Table 2.
Intrauterine Anesthesia in Hysteroscopy
| Study | Procedure | Patients (n) | Intrauterine Medication, Dose | Comparator | Reduced Pain? | Pain Difference | Study Quality | Comments |
|---|---|---|---|---|---|---|---|---|
| Soriano 200031 | Hysteroscopy alone | 121 | 5% lidocaine spray, 3 metered doses | Placebo spray | Yes | 15 mm 100mmVAS |
Good | Total dose 30mg per manufacturer label; sprayed on cervical surface and then endocervical canal. |
| Gupta 201034 | Hysteroscopy, biopsy | 49 | 2% lidocaine 5mL | None | Yes | 15 mm 100mmVAS |
Poor | Compared lidocaine to oral naproxen. Pain reduced during hysteroscopy, not at other times. All patients received misoprostol 400mcg prior to hysteroscopy. |
| Zupi 199532 | Hysteroscopy, biopsy | 45 | 2% mepivacaine 5mL | Saline placebo | Yes | 40mm 200mmVAS |
Fair | Subgroup analysis of patients with hysteroscopy alone or hysteroscopy plus biopsy; pain reduced in both groups, most significantly with hysteroscopy alone |
| Cicinelli 199733 | Hysteroscopy, biopsy | 80 | 2% mepivacaine 2mL | Saline placebo | No | Good | ||
| Lau 200035 | Hysteroscopy, biopsy | 89 | 2% lidocaine 5mL | Saline placebo | No | Good |
VAS, visual analog scale.
Results were mixed. As shown in Table 2, three studies with a total of 215 subjects reported significant reduction in pain score during hysteroscopy with the use of intrauterine anesthesia, but only one was of good quality. The fair-quality study did not clearly report on allocation concealment and blinding, and the poor quality study was did not have blinding of either patients or providers, so both had some potential for bias. Two good-quality studies reported no significant reduction in pain between intervention and placebo groups.
Five studies evaluated intrauterine anesthesia in radiographic procedures: one study of saline-infusion sonogram(28) and four of HSG (29–32). (Table 3) Most used the same outcome scale of a 100mm VAS, though one used a 200mm VAS. Different doses and medications were used in all studies. Four studies compared to placebo, but one used no placebo and compared intrauterine lidocaine to oral naproxen only. In one study all subjects received topical lidocaine spray to the cervix, and in two studies all subjects received oral naproxen prior to procedures.
Table 3.
Intrauterine Anesthetic in Sonography and Hysterosalpingogram
| Study | Procedure | Patient s (n) | Intrauterine Medication, Dose | Comparator | Reduced Pain? | Pain Difference | Study Quality | Comments |
|---|---|---|---|---|---|---|---|---|
| Guney 200736 | Saline infusion sonogram | 106 | 2% lidocaine 5mL | Saline placebo | Yes | 24% reduction in pain score 100mmVAS | Good | Only reported exact numeric pain scores for subgroup analysis, overall reduction reported for whole population. |
| Costello 200237 | Hysterosalpingogram | 110 | 2% lidocaine 5mL | Saline placebo | No | Good | Increased pain post-procedure in lidocaine group. All patients had topical lidocaine applied to anterior cervix prior to tenaculum and naproxen prior to procedure. | |
| Frishman 200438 | Hysterosalpingogram | 64 | 2% lidocaine 3mL | Saline placebo | No | Good | All patients received oral NSAID prior to procedure. Similar levels of moderate or severe pain in both | |
| Gupta 200839 | Hysterosalpingogram | 100 | 1% lidocaine 5mL | None | No | Poor | No placebo; compared lidocaine to oral naproxen. No difference in pain between 2 groups | |
| Kafali 200340 | Hysterosalpingogram | 86 | 2% lidocaine gel 2.5mL | Placebo gel | No | Good | Slight reduction in pain 30 min after HSG, but at most times and on average, no difference |
VAS, visual analog scale; NSAID, nonsteroidal anti-inflammatory drugs; HSG, hysterosalpingogram.
The single study of saline-infusion sonogram reported a significant reduction in pain score with intrauterine anesthetic; this was a good-quality study. All four studies of HSG, with at total of 360 subjects, reported no significant reduction in pain score with intrauterine anesthetic. One study reported an increased post-procedure pain score in the group receiving intrauterine lidocaine. Of the four studies reporting no reduction in pain, three were good quality. One was poor quality with unclear allocation concealment and no blinding of patients or providers.
Two studies evaluated intrauterine anesthesia in first-trimester abortion. (Table 4) Both studies were similar in methods, but differed in dose of lidocaine used. In both studies all patients received oral non-steroidal anti-inflammatory drugs, and some patients received oral benzodiazepine prior to the procedure. One study using 10 mL of 1% lidocaine showed no significant reduction in pain score(33). A follow-up study which used the higher dose of 5mL of 4% lidocaine did show a significant reduction in pain score with intrauterine lidocaine.(34) Both were of good quality.
One study evaluated intrauterine anesthesia in IUD insertion,(35) one in IUD retrieval,(36) and one study in hysteroscopic tubal sterilization.(37) (Table 4) The study of IUD insertion compared lidocaine gel to placebo or no intervention and reported pain score as the proportion of patients reporting high pain scores (>5 on a 7-point scale). The authors reported reduced pain score with intrauterine lidocaine gel when the placebo and no-intervention groups were combined. This study was of fair quality, as allocation concealment is unclear, and providers were not blinded overall due to the inclusion of the no-intervention group.
The study of IUD retrieval with a Novak curette compared lidocaine to placebo gel and showed a significant reduction in pain score in the lidocaine group; this was a good quality study. The single study of intrauterine lidocaine in hysteroscopic tubal sterilization was of good quality. The investigators used multiple adjunctive medications in all patients (paracervical block, oral non-steroidal anti-inflammatory drugs and oral benzodiazepine) and showed no significant reduction in pain score.
CONCLUSION
Intrauterine anesthesia is an effective method of pain management for some gynecologic office procedures, but not for all. This review found good evidence to support its use in endometrial biopsy, moderate evidence to support use in hysteroscopy, and insufficient evidence to recommend for or against use in IUD insertion, IUD removal, saline-infusion sonogram, hysteroscopic tubal sterilization or first-trimester abortion. Good evidence indicates that intrauterine anesthesia is not effective in HSG.
The effectiveness of intrauterine anesthetic is related to the origin and pathways of uterine innervation. While the Frankenhauser plexus in the lower broad ligament is the most well known nervous pathway, the uterus, cervix and fallopian tubes receive nerve supply from other sources as well. Sympathetic innervations from the T-10 to L1 roots enter the uterus with the utero-ovarian vessels and follow a variable course, with branches following the anastamoses of the uterine artery. (38, 39) Well defined nerve plexuses lie in the endometrium and along the mucosal surface of the cervix, and are fed by both the ascending and descending roots; the precise pattern of innervation varies with pathologic processes such as endometriosis and adenomyosis. (40) The limited efficacy of the paracervical block in many gynecologic procedures is likely due to its inability to block these nerves of other origins. Intrauterine anesthesia may reach these nerves more effectively and, alone or in conjunction with paracervical block, provide more global uterine anesthesia.
The overall safety of intrauterine anesthesia is an important consideration if it is to be widely incorporated into office gynecology. Twenty of the twenty-three included studies used lidocaine as the intrauterine anesthetic, and ample evidence supports its safety when administered by this route. Higher doses (exceeding 200mg total of lidocaine) may lead to increased frequency of minor side effects, (34) but several studies have documented no significantly increased serum levels in the toxic range, even in symptomatic patients.(22, 34, 41). One study measured serial blood samples at five, 15, 30, and 60 minutes following insertion of 11ml of 2% lidocaine gel in 10 patients. All patients had peak serum lidocaine levels well below the threshold for toxicity.(41) Mepivicaine was used in 2 studies, and no significant adverse reaction occurred in any patients in either study; it is reasonable to assume its safety profile is similar to that of lidocaine at equivalent doses. One included study used benzocaine spray, and found it did not reduce pain scores. (17) Specific safety concerns have been raised about the anesthetic benzocaine in its spray formulation with a known link to methemoglobinemia. (42) Until more safety data is available, lidocaine or mepivicaine should be considered preferred anesthetics for intrauterine use, and benzocaine spray should be avoided.
Our review has both strengths and weaknesses. It is strengthened by a comprehensive search strategy which revealed a substantial body of research on this topic. Prior reviews of pain control in gynecologic practice have tended to focus on a single given procedure and assess the evidence supporting the use of various pain control methods (oral non-steroidal anti-inflammatory drugs, paracervical block, etc) for that procedure. By focusing on the anesthetic technique across the full range of office procedures, we were able to assess how this technique may be applied to general gynecologic practice.
Our study’s main weakness is the inconsistent quality of the studies we have reviewed. Many were of fair or poor quality, with moderate to substantial risk of bias. This lack of quality compromises the interpretation of study results overall. The review is also limited by the small numbers of studies for several procedures including IUD insertion, first-trimester abortion, hysteroscopic tubal sterilization, and saline-infusion sonogram. When only one study is available, even if that study is of good quality, the strength of evidence is overall weak. The heterogeneity of the studies also limited our conclusions. For clarity in interpretation, we stratified our analysis by specific procedures. However, even for single procedures, the studies varied in medication type, dosing, and measurement of pain score. Different dose effects and outcome measurements complicate comparison and interpretation of the results as a whole.
It is unclear why intrauterine anesthesia has not been more widely adopted especially for endometrial biopsy and hysteroscopy. Many factors may prevent clinicians from adopting potentially beneficial practices. Providers may be unaware of new practices; they may lack of awareness of the need for new practices; they may overestimate the potential safety concerns or perceive difficulty of incorporating new methods into established work-flow patterns. Each of these may be involved in the failure of clinicians to adopt intrauterine anesthesia. It is the authors’ subjective experience that most clinicians are unaware of the technique and unfamiliar with the literature published on the topic. Research assessing provider familiarity with the technique could provide further insight into this question
Administering intrauterine anesthesia prior to an office procedure is an effective, low-cost, and low risk intervention. Administration is generally simple, and seems less painful for patients than injection of a paracervical block. Good effect on pain seems is most consistently seen with doses at or equivalent to 100mg–200mg of lidocaine. No studies included in this review reported any adverse outcomes. One study has clearly demonstrated that the use of intrauterine lidocaine does not impact the quality or reliability of pathology specimens in procedures where it is used.(15) Good evidence supports its use in endometrial biopsy, and moderate evidence supports use at doses above 100mg in hysteroscopy. Clinicians should consider adopting intrauterine anesthesia for endometrial biopsy and hysteroscopy in order to improve their patients’ comfort during these procedures. Provider education regarding the frequently unmet need for pain control and demonstrating the efficacy of this technique could help support its adoption.
Acknowledgments
Rebecca J. Mercier is supported by an NIH T-32 grant for clinical research (Grant # T32 HD 40672-11) and the North Carolina Translational and Clinical Sciences Institute. The Institute is supported by grants UL1RR025747, KL2RR025746, and TLRR025745 from the NIH National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health.
Footnotes
Financial Disclosure: The authors did not report any potential conflicts of interest.
References
- 1.Naki MM, Api O, Acioglu HC, Uzun MG, Kars B, Unal O. Analgesic Efficacy of Forced Coughing versus Local Anesthesia during Cervical Punch Biopsy. Gynecol Obstet Invest. 2011 May 21; doi: 10.1159/000320842. [DOI] [PubMed] [Google Scholar]
- 2.Oyama IA, Wakabayashi MT, Frattarelli LC, Kessel B. Local anesthetic reduces the pain of colposcopic biopsies: a randomized trial. American journal of obstetrics and gynecology. 2003 May;188(5):1164–5. doi: 10.1067/mob.2003.290. [DOI] [PubMed] [Google Scholar]
- 3.Crane JCC, Dawson L, O’Grady T, Bartellas E, Hutchens D. Randomized trial of oral misoprostol before endometrial biopsy. J Obstet Gynaecol Can. 2009;31(11):1054–9. doi: 10.1016/S1701-2163(16)34351-1. [DOI] [PubMed] [Google Scholar]
- 4.Leclair CM, Zia JK, Doom CM, Morgan TK, Edelman AB. Pain experienced using two different methods of endometrial biopsy: a randomized controlled trial. Obstetrics and gynecology. 2011 Mar;117(3):636–41. doi: 10.1097/AOG.0b013e31820ad45b. [DOI] [PubMed] [Google Scholar]
- 5.Hubacher D, Reyes V, Lillo S, Zepeda A, Chen PL, Croxatto H. Pain from copper intrauterine device insertion: randomized trial of prophylactic ibuprofen. American journal of obstetrics and gynecology. 2006 Nov;195(5):1272–7. doi: 10.1016/j.ajog.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 6.Dijkhuizen K, Dekkers OM, Holleboom CA, de Groot CJ, Hellebrekers BW, van Roosmalen GJ, et al. Vaginal misoprostol prior to insertion of an intrauterine device: an RCT. Hum Reprod. 2011 Feb;26(2):323–9. doi: 10.1093/humrep/deq348. [DOI] [PubMed] [Google Scholar]
- 7.Edelman AB, Schaefer E, Olson A, Van Houten L, Bednarek P, Leclair C, et al. Effects of prophylactic misoprostol administration prior to intrauterine device insertion in nulliparous women. Contraception. 2011 Sep;84(3):234–9. doi: 10.1016/j.contraception.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 8.Saav I, Aronsson A, Marions L, Stephansson O, Gemzell-Danielsson K. Cervical priming with sublingual misoprostol prior to insertion of an intrauterine device in nulliparous women: a randomized controlled trial. Hum Reprod. 2007 Oct;22(10):2647–52. doi: 10.1093/humrep/dem244. [DOI] [PubMed] [Google Scholar]
- 9.Tangsiriswatthana TS, US, Lumbiganon P, Loapaiboon M. Paracervical local anaesthesia for cervical dilation and uterine intervention. Cochrane Database Syst Rev. 2009;(1):Art. No.: CD005056. doi: 10.1002/14651858.CD005056.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Ahmad DD, JMN, O’Flynn H, Watson A. Pain Relief in hysterosalpingography. Cochrane Database Syst Rev. 2007;(2):Art. No.: CD006106. doi: 10.1002/14651858.CD006106.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Allen RHGDH D, O’Brien P. Interventions for pain with intrauterine device insertion. Cochrane Database Syst Rev. 2009;(2):Art. No.:CD006106. doi: 10.1002/14651858.CD006106.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Renner RM, Jensen JT, Nichols MD, Edelman AB. Pain control in first-trimester surgical abortion: a systematic review of randomized controlled trials. Contraception. 2010 May;81(5):372–88. doi: 10.1016/j.contraception.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Butler CRC, Dennis C. Turk Bonica’s management of pain. 3. Philadelphia: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 14.Hasson HM. Topical uterine anesthesia: a preliminary report. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 1977;15(3):238–40. doi: 10.1002/j.1879-3479.1977.tb00683.x. [DOI] [PubMed] [Google Scholar]
- 15.Trolice MP, Fishburne C, Jr, McGrady S. Anesthetic efficacy of intrauterine lidocaine for endometrial biopsy: a randomized double-masked trial. Obstetrics and gynecology. 2000 Mar;95(3):345–7. doi: 10.1016/s0029-7844(99)00557-8. [DOI] [PubMed] [Google Scholar]
- 16.Dogan E, Celiloglu M, Sarihan E, Demir A. Anesthetic effect of intrauterine lidocaine plus naproxen sodium in endometrial biopsy. Obstetrics and gynecology. 2004 Feb;103(2):347–51. doi: 10.1097/01.AOG.0000109519.74229.30. [DOI] [PubMed] [Google Scholar]
- 17.Einarsson JI, Henao G, Young AE. Topical analgesia for endometrial biopsy: a randomized controlled trial. Obstetrics and gynecology. 2005 Jul;106(1):128–30. doi: 10.1097/01.AOG.0000165272.62416.61. [DOI] [PubMed] [Google Scholar]
- 18.Guney M, Oral B, Mungan T. Intrauterine lidocaine plus buccal misoprostol in the endometrial biopsy. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2007 May;97(2):125–8. doi: 10.1016/j.ijgo.2006.11.017. [DOI] [PubMed] [Google Scholar]
- 19.Hui SK, Lee L, Ong C, Yu V, Ho LC. Intrauterine lignocaine as an anaesthetic during endometrial sampling: a randomised double-blind controlled trial. BJOG : an international journal of obstetrics and gynaecology. 2006 Jan;113(1):53–7. doi: 10.1111/j.1471-0528.2005.00812.x. [DOI] [PubMed] [Google Scholar]
- 20.Kozman E, Collins P, Howard A, Akanmu T, Gibbs A, Frazer M. The effect of an intrauterine application of two percent lignocaine gel on pain perception during Vabra endometrial sampling: a randomised double-blind, placebo-controlled trial. BJOG : an international journal of obstetrics and gynaecology. 2001 Jan;108(1):87–90. doi: 10.1111/j.1471-0528.2001.00005.x. [DOI] [PubMed] [Google Scholar]
- 21.Api O, Ergen B, Api M, Ugurel V, Emeksiz MB, Unal O. Comparison of oral nonsteroidal analgesic and intrauterine local anesthetic for pain relief in uterine fractional curettage: a randomized, double-blind, placebo-controlled trial. American journal of obstetrics and gynecology. 2010 Jul;203(1):28, e1–7. doi: 10.1016/j.ajog.2010.02.029. [DOI] [PubMed] [Google Scholar]
- 22.Rattanachaiyanont M, Leerasiri P, Indhavivadhana S. Effectiveness of intrauterine anesthesia for pain relief during fractional curettage. Obstetrics and gynecology. 2005 Sep;106(3):533–9. doi: 10.1097/01.AOG.0000172424.09992.3e. [DOI] [PubMed] [Google Scholar]
- 23.Soriano D, Ajaj S, Chuong T, Deval B, Fauconnier A, Darai E. Lidocaine spray and outpatient hysteroscopy: randomized placebo-controlled trial. Obstetrics and gynecology. 2000 Nov;96(5 Pt 1):661–4. doi: 10.1016/s0029-7844(00)00984-4. [DOI] [PubMed] [Google Scholar]
- 24.Zupi E, Luciano AA, Valli E, Marconi D, Maneschi F, Romanini C. The use of topical anesthesia in diagnostic hysteroscopy and endometrial biopsy. Fertil Steril. 1995;63(2):414–6. [PubMed] [Google Scholar]
- 25.Cicinelli E, Didonna T, Ambrosi G, Schonauer LM, Fiore G, Matteo MG. Topical anaesthesia for diagnostic hysteroscopy and endometrial biopsy in postmenopausal women: a randomised placebo-controlled double-blind study. British journal of obstetrics and gynaecology. 1997 Mar;104(3):316–9. doi: 10.1111/j.1471-0528.1997.tb11460.x. [DOI] [PubMed] [Google Scholar]
- 26.Gupta N, Gupta B, Dadhwal V, Mittal S. Efficacy of intrauterine lignocaine plus vaginal misoprostol for pain relief in premenopausal women undergoing endometrial aspiration and ambulatory hysteroscopy. Acta obstetricia et gynecologica Scandinavica. 2010 Aug;89(8):1066–70. doi: 10.3109/00016349.2010.499444. [DOI] [PubMed] [Google Scholar]
- 27.Lau WC, Tam WH, Lo WK, Yuen PM. A randomised double-blind placebo-controlled trial of transcervical intrauterine local anaesthesia in outpatient hysteroscopy. BJOG : an international journal of obstetrics and gynaecology. 2000 May;107(5):610–3. doi: 10.1111/j.1471-0528.2000.tb13301.x. [DOI] [PubMed] [Google Scholar]
- 28.Guney M, Oral B, Bayhan G, Mungan T. Intrauterine lidocaine infusion for pain relief during saline solution infusion sonohysterography: a randomized, controlled trial. Journal of minimally invasive gynecology. 2007 May-Jun;14(3):304–10. doi: 10.1016/j.jmig.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 29.Costello MF, Horrowitz S, Steigrad S, Saif N, Bennett M, Ekangaki A. Transcervical intrauterine topical local anesthetic at hysterosalpingography: a prospective, randomized, double-blind, placebo-controlled trial. Fertil Steril. 2002 Nov;78(5):1116–22. doi: 10.1016/s0015-0282(02)03362-9. [DOI] [PubMed] [Google Scholar]
- 30.Frishman GN, Spencer PK, Weitzen S, Plosker S, Shafi F. The use of intrauterine lidocaine to minimize pain during hysterosalpingography: a randomized trial. Obstetrics and gynecology. 2004 Jun;103(6):1261–6. doi: 10.1097/01.AOG.0000127370.66704.f5. [DOI] [PubMed] [Google Scholar]
- 31.Gupta N, Ghosh B, Mittal S. Comparison of oral naproxen and intrauterine lignocaine instillation for pain relief during hysterosalpingography. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2008 Sep;102(3):284–6. doi: 10.1016/j.ijgo.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 32.Kafali H, Cengiz M, Demir N. Intrauterine lidocaine gel application for pain relief during and after hysterosalpingography. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2003 Oct;83(1):65–7. doi: 10.1016/s0020-7292(03)00154-1. [DOI] [PubMed] [Google Scholar]
- 33.Edelman A, Nichols MD, Leclair C, Astley S, Shy K, Jensen JT. Intrauterine lidocaine infusion for pain management in first-trimester abortions. Obstetrics and gynecology. 2004 Jun;103(6):1267–72. doi: 10.1097/01.AOG.0000127981.53911.0e. [DOI] [PubMed] [Google Scholar]
- 34.Edelman A, Nichols MD, Leclair C, Jensen JT. Four percent intrauterine lidocaine infusion for pain management in first-trimester abortions. Obstet Gynecol. 2006 Feb;107(2 Pt 1):269–75. doi: 10.1097/01.AOG.0000194204.71925.4a. [DOI] [PubMed] [Google Scholar]
- 35.Oloto EJ, Bromham DR, Murty JA. Pain and discomfort perception at IUD insertion - Effect of short-duration, low-volume, intracervical application of two per cent lignocaine gel (Instillagel(TM)) - A preliminary study. Br J Fam Plan. 1997 Jan;22(4):177–80. [Google Scholar]
- 36.Guney M, Oral B, Mungan T. Efficacy of intrauterine lidocaine for removal of a “lost” intrauterine device: a randomized, controlled trial. Obstetrics and gynecology. 2006 Jul;108(1):119–23. doi: 10.1097/01.AOG.0000223201.42144.80. [DOI] [PubMed] [Google Scholar]
- 37.Isley MM, Jensen JT, Nichols MD, Lehman A, Bednarek P, Edelman A. Intrauterine lidocaine infusion for pain management during outpatient transcervical tubal sterilization: a randomized controlled trial. Contraception. 2012 Mar;85(3):275–81. doi: 10.1016/j.contraception.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 38.Katz VL, GM, Lobo RA, Gershenon DM. Comprehensive Gynecology. 5. Philadelphia PA: Mosby Elsevier; 2007. [Google Scholar]
- 39.Quinn MJ, Kirk N. Differences in uterine innervation at hysterectomy. American journal of obstetrics and gynecology. 2002;187(6):1515–9. doi: 10.1067/mob.2002.130007. [DOI] [PubMed] [Google Scholar]
- 40.Tokushige N, Markham R, Russell P, Fraser IS. High density of small nerve fibres in the functional layer of the endometrium in women with endometriosis. Hum Reprod. 2006;21(3):782–7. doi: 10.1093/humrep/dei368. [DOI] [PubMed] [Google Scholar]
- 41.Rousseau GF, Oram M, Barrington J, Priston M, Swart M. Plasma lidocaine concentrations following insertion of 2% lidocaine gel into the uterine cavity after uterine balloon thermal ablation. Br J Anaesth. 2002 Dec;89(6):846–8. doi: 10.1093/bja/aef267. [DOI] [PubMed] [Google Scholar]
- 42.Ash-Bernal R, Wise R, Wright SM. Acquired methemoglobinemia: a retrospective series of 138 cases at 2 teaching hospitals. Medicine. 2004 Sep;83(5):265–73. doi: 10.1097/01.md.0000141096.00377.3f. [DOI] [PubMed] [Google Scholar]