Abstract
Objectives
We evaluated whether implementation of Treatment on Demand (TOD) policy in San Francisco was associated with improved access to drug abuse treatment.
Methods
Data came from San Francisco’s treatment program waiting list over 4 years spanning the implementation of TOD policy. Access measures were monthly applicants waiting and days waited by treatment admissions. Quantitative analyses with 69 treatment facilities contrasted those receiving vs. not receiving TOD funds. Qualitative data came from interviews with facility administrators.
Results
There was a small statistically significant decline in monthly waiting lists in the number of people waiting for treatment during the study period. The days waited by those admitted to treatment, however, significantly increased in TOD-funded facilities. Facilities used varied criteria for completing the access measures, which limit the utility of the measures.
Conclusions
Access to treatment improved slightly with implementation of TOD policy.
Keywords: Access, drug abuse treatment, policy, waiting lists
INTRODUCTION
The term drug abuse “treatment on demand” (TOD) refers to a policy that supports immediate entry into drug treatment for all requesting it. Timely access to treatment contrasts with policies that emphasize punishment or interdiction. TOD has been endorsed in several metropolitan areas including Baltimore, Maryland (1), and Sacramento, California (2).
San Francisco, CA adopted TOD as policy in late 1996 and began implementing the program mid-1997 (3–5). Implementation of TOD was gradual: San Francisco increased its drug treatment budget from $31.9 million in FY 1995–1996 to $45.2 million in FY 1999–2000. Admissions to drug treatment programs increased 15% during that time (6), and TOD was associated with an increase in the utilization of comprehensive treatments, particularly day treatment, with a decrease in the utilization of front-end treatments, such as drop-in services (7).
A primary goal of TOD was to improve access to treatment. “Treatment access” has long been defined as the ease of reaching a program and obtaining its services (8). Treatment access includes several dimensions—temporal, geographical, financial, psychological, and cultural. In a study of multiple stakeholders, all groups cited lack of treatment slots and long waiting periods as significant barriers to treatment enrollment (9). The current study examined temporal access, namely, treatment waiting lists, yet other dimensions are important, for example, distance to treatment programs (10), financial cutbacks (11), and psychological and cultural barriers (12). The lack of accessible drug treatment is a significant barrier to individuals needing care (13, 14).
This research asked whether waiting lists at drug treatment programs improved with the implementation of TOD. The problematic nature of waiting lists is widely documented (15–18). For example, many potential patients may not bother to apply to treatment, and many who do apply will give up rather than wait. Applicants on waiting lists use more drugs than those who enter treatment (19). In many communities drug users who want treatment need to wait for months. Although implementation of TOD might decrease waiting lists, it is also possible that waiting lists will increase as many individuals who had not attempted to get into treatment decide that the effort is worth their while. Surprisingly, little is understood about the relationship between the demand for treatment and waiting lists (20).
The federal Office of National Drug Control Policy is responsible for monitoring access to drug treatment. Improving treatment access is an objective of the national drug control plan (21). Every U.S. state reports information about patients waiting for drug treatment. In California, the Drug and Alcohol Treatment Access Reporting (DATAR) system gathers information from drug treatment programs. Each month, programs respond to questions that describe their capacity to admit patients.
This study used DATAR information to assess whether implementation of TOD policy was associated with improved access to drug treatment. We tested the hypotheses that 1) the number of applicants on waiting lists would decrease and 2) the waiting time to get into treatment would decrease. We interviewed program administrators to gain program perspectives and to understand limitations in the data.
METHODS
The DATAR Reporting System
We downloaded DATAR information from the San Francisco County’s drug treatment administration from July 1995 through June 1999. A total of 33 programs in San Francisco reported to DATAR during this time, representing 69 treatment facilities. The reports of applicants on the waiting list did not contain individual identifiers; consequently, DATAR could not detect an individual who applied to multiple programs.
Measures and Time Periods
Two measures evaluated whether TOD improved patient access to treatment: 1) number of applicants on the waiting list at the end of the month; 2) mean days waited by those admitted to treatment before entering treatment. We studied the 4-year period from 2 years prior to beginning TOD funding, to 2 years after. July 1997 marked the beginning of TOD funding, which has been used in other analyses (22). TOD support infused into the system gradually, starting in the final 3 months of the 1996–1997 fiscal year (April–June 1997). To assess whether or not a treatment facility received support to implement TOD we consulted county staff, as well as the TOD Planning Council to reconstruct program funding line items with treatment facilities. We further clarified facility funding during an interview described below.
Interviews with TOD Program Administrators
To augment the DATAR information we conducted semi-structured, qualitative interviews with administrators who provided consent from TOD-funded programs. The UCSF Institutional Review Board approved all procedures. Interviews were audio taped and transcribed. Interviews were intended to clarify: 1) accuracy of the waiting list reports, and 2) how well reports reflected access to treatment. Additional questions were asked about the “mechanics” of the waiting list, experience, training, institutional feedback, and understanding of DATAR. Programs were recruited for interviews if they: 1) reported to DATAR; 2) received TOD funding; and 3) allocated the TOD funding to treatment (not just prevention). Fourteen programs were recruited, representing 23 treatment facilities. One program declined and 13 programs were interviewed.
Aggregation of Data
DATAR reports were analyzed for accuracy. Unusual variances were flagged and investigated, automated cleaning eliminated duplicate entries, and facilities that reported < 5 months of data over the 4-year period were dropped. Graphs showing facility-specific data were created to illustrate irregularities, which were discussed in the interview with TOD programs to learn whether unusual variances were accurate or errors.
Data Analysis Approach
The primary goal was to test the hypothesis that implementation of TOD policy was associated with improved access to drug treatment. We first examined the characteristics of the treatment programs and facilities and summarized the access measures system-wide. We then examined changes access as a function of time. Standard linear regression analyses were inappropriate for this time series data, because preliminary analysis of 2-dimensional plots—outcome measure (Y) by time (X)—indicated nonconvergent sinusoidal distributions in time. To avoid violating the linear regression assumption of independent errors, we employed the SAS® AUTOREG procedure (23). Analysis of interviews with TOD program administrators used both quantitative and qualitative techniques.
RESULTS
Descriptive Analyses
The 69 treatment facilities included: Outpatient Drug Free (25, 9 TOD funded); Residential Drug Free (21, 6 TOD funded); Day Treatment (9, 3 TOD funded); Residential Detoxification (7, none TOD funded); Outpatient Methadone Detoxification (3, 2 TOD funded); Outpatient Methadone Maintenance (3, all TOD funded); and one Outpatient Detoxification Non-Methadone (not TOD funded). Figure 1 shows applicants on the waiting list system-wide. The waiting list was substantial throughout the 4 years of the study, ranging from a low of 889 applicants in March 1999 to a high of 1,883 in December 1995. Mean days waiting for treatment ranged from 12 in July 1997 to 44 in January 1999.
Figure 1.
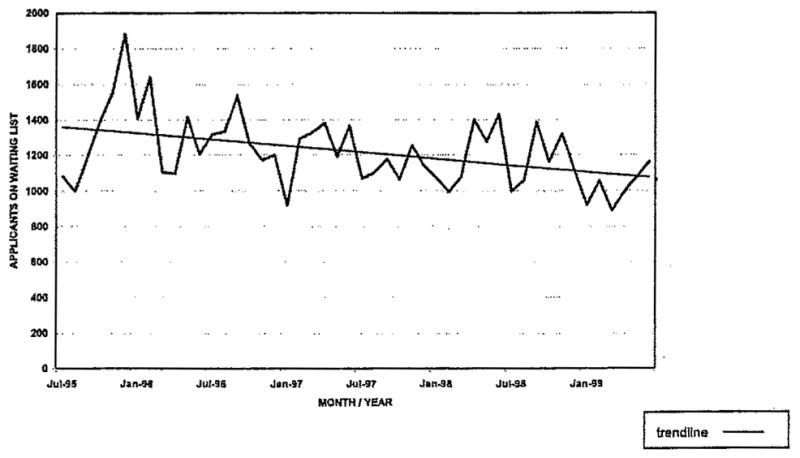
Number of applicants on the waiting list at the end of the month all facilities.
Inferential Analyses
As Figure 1 and Table 1 illustrate, the monthly number of applicants on San Francisco’s treatment waiting list decreased (regression coefficient = −6.690, CI = (−9.007, −4.371), p < .001). As Table 1 illustrates, the mean number of days waited by those admitted to treatment from the waiting list did not change over the study period (regression coefficient=.078, CI = (−.136, .291), and p = .482).
Table 1.
Time series analysis of time effects on monthly waiting list data: Comparison of treatment on demand (TOD) funded with non-TOD funded facilities
| Dependent variable | All facilities (n = 69)
|
TOD facilities (n = 23)
|
Non-TOD facilities (n = 46)
|
Comparison of TOD and non-TOD slopes
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Regression coefficient | CI | R2 | p-value | Regression coefficient | CI | R2 | p-value | Regression coefficient | CI | R2 | p-value | T-value | p-value | |
| Number of applicants on waiting list at end of month | −6.690 | −9.007, −4.371 | .397 | < .0001 | −2.372 | −7.79, 3.047 | .377 | .396 | −2.991 | −7.382, 1.4 | .230 | .189 | .174 | .863 |
| Mean number of days waited by those admitted to treatment | .078 | −0.136, .291 | .248 | .482 | .553 | .084, 1.022 | .267 | .025 | −.095 | −.279, .089 | .244 | .318 | 2.522 | .015 |
The total R squared statistic, computed from the autoregressive model residuals, reflects the improved fit from the use of past residuals to help predict the next Y value (23).
Table 1 summarizes the AUTO-regression results comparing TOD and non-TOD funded facilities. In applicants on the waiting list, there was no significant difference in the rate of change between TOD and non-TOD funded facilities. However, on days waited by those admitted to treatment, the slopes were significantly different (t = 2.522, p = .015), indicating slower entry into treatment among clients admitted to TOD-funded facilities. Days waited for treatment admission significantly increased in TOD funded facilities (regression coefficient = .553, CI = (.084, 1.022), p = .025), but did not significantly change in non-TOD funded facilities (regression coefficient = − .095, CI = (−.279, .089), p = .318).
Interviews with TOD program administrators asked two questions with quantitative responses to tap how well DATAR reflected the number of people on the waiting list and how well the waiting list reflected accessibility of program services. Program responses were varied but did not provide much support for the DATAR measures. Only one response indicated that DATAR reflected “very well” the number of people on the waiting list, and 5 interviewees indicated that the waiting list reflected accessibility of program services “very well.”
Qualitative responses revealed wide discrepancy in how programs reported to DATAR. For example, in one program if applicants telephoned they would be entered on the waiting list, and in another program they would not. Within-program policy changes also affected the DATAR reports. For example, one program eliminated its waiting list by creating an “orientation group” so that patients could obtain some service while awaiting, more intensive treatment. Another program diverted applicants to any treatment that was not full, so applicants received services, even if not the services for which they applied.
All program administrators expressed a desire for feedback about DATAR, and half requested updated training. Although reporting had been a monthly requirement since 1992, programs had not been informed about what use was being made of the data. One administrator commented: “I just wish (it) was truly a tool, that since you’re collecting the data, that it could be translated into new knowledge that could then be kicked back to the people that are at the front lines doing the work, to learn from each other.”
DISCUSSION
We examined whether the implementation of TOD policy in San Francisco was associated with enhanced access to drug treatment and found that TOD was associated with limited improvement. Citywide the number of applicants on the waiting list improved significantly. The length of time waiting for treatment did not change; however, among facilities that received TOD funding, waiting time significantly increased.
The decrease in applicants on the waiting list is congruent with other research. Earlier our group documented that admissions increased when TOD was implemented (6, 22). The finding of increased waiting time to enter treatment among TOD-funded facilities was unexpected. One possibility is that programs retained people in treatment longer, hence increasing the wait time for those seeking treatment. A study of admissions (7) indicated TOD involved a shift away from short-term services, and increased access into longer-term care. Alternatively, facilities may have used TOD funds to launch new programs, starting wait lists before accepting patients. Our data cannot test these hypothesized explanations.
The study has limitations that can be explored in future research. Foremost is the quality of treatment access measurement. DATAR was developed as an administrative tool, not a research instrument. Interviews revealed inconsistencies in the way data were gathered. More frequent training and monitoring could improve the system. In addition, the access measure, as practiced in San Francisco, did not include individual client identifiers, so it is not possible to determine whether more people applied for treatment under the TOD policy. Also we emphasize that access is a broader topic than the number of patients in line for treatment or their waiting time. Equally important issues may include geographic, financial, and cultural access to services, which were not measured.
Finally, the 23-facility sample in the TOD analysis is small and could affect the stability of slope estimates related to the access measures. Because this was a community initiative, the sample size was fixed. However, the stability of the estimate is affected not only by the number of facilities, but also by the data points per facility, which involved multiple months of observation. The confidence interval for the finding of decreased mean number of days waited by those admitted to treatment, although based on data from only 23 facilities, does not encompass zero, reflecting good stability of the estimate derived.
Future research should develop more specific and reliable measures of treatment access, and program staff would benefit from continued training in these data systems. Progress in this area could improve federal efforts to monitor national waiting lists for drug abuse treatment. In community-based service systems, policy decisions seldom wait for research findings to guide them. As budgetary shortfalls mounted in San Francisco, and throughout the country during the early 2000s, San Francisco remained committed to TOD, and overall substance abuse treatment funding continued to increase during the years 2000–2001 and 2001–2002. Fiscal year 2002–2003 marked the first actual decrease in treatment funding in San Francisco. The TOD Planning Council still exists, yet the task has become managing budget reductions rather than planning to increase services. The concept of “Treatment on Demand” remains an ideal, which was partially implemented in San Francisco. Results of the current study indicate that TOD had a detectable, though not dramatic, impact on the accessibility of services.
Acknowledgments
Supported in part by National Institutes of Health grants R01DA12221 and P50DA09253, and by the Center for Substance Abuse Treatment task order 282-98-0026. The authors appreciate the assistance of Sarah Yoo, Christine Lin, and TeChieh Chen. A preliminary report of the study was presented at the meeting of the American Public Health Association.
References
- 1.Johnson JL, Ahmed A, Plemons B, Powell W, Carrington H, Graham J, Hill R, Schwartz RP, Brooner RK. Steps to Success: The Baltimore Drug and Alcohol Treatment Outcomes Study. Baltimore, MD: Baltimore Substance Abuse Services; 2002. [Last accessed May 20, 2005]. Available at http://www.soros.org/baltimore/Executive%20Summary%20doc.pdf. [Google Scholar]
- 2.Moore T. Sacramento County’s Alcohol and Other Drug Treatment Initiative. [Last accessed May 20, 2005];CSAT TIE Communique, Fall’98 1997. Available at http://www.treatment.org/communique/comm98W/Sacramento.html.
- 3.Carlsen W. San Francisco Chronicle. May 17, 1997. SF proposes on-demand drug treatment: It’s aimed at poor, youth; p. 1. Section A. [Google Scholar]
- 4.Gordon R. San Francisco Examiner. Jan 18, 1997. Mayor promises drug treatment on demand; p. 1. Section A. [Google Scholar]
- 5.Stein L. San Francisco pioneers plan to treat all drug users—Program will test whether treatment can reduce drug abuse—and save city money. The Christian Science Monitor. 1997 Jan 29;89(44):4. [Google Scholar]
- 6.Guydish J, Moore L, Gleghorn A, Davis T, Sears C, Harcourt J. Drug abuse treatment on demand in San Francisco: Preliminary findings. J Psychoactive Drugs. 2000;32:363–370. doi: 10.1080/02791072.2000.10400237. [DOI] [PubMed] [Google Scholar]
- 7.Sears C. Investigating the Effects of San Francisco’s Treatment on Demand Initiative on a Publicly-Funded Substance Abuse Treatment System: A Time Series Analysis. San Francisco, CA: UCSF Institute of Health Policy Studies; 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Landsberg G, Neigher WD, Hammer RJ, Windle C, Woy JR, editors. Evaluation in Practice: A Sourcebook of Program Evaluation Studies from Mental Health Care Systems in the United States. Washington, DC: U.S. Government Printing Office; 1979. [Google Scholar]
- 9.Appel PW, Wllison AE, Jansky HK, Oldak R. Barriers to enrollment in drug abuse treatment and suggestions for reducing them: Opinions of drug injecting street outreach clients and other system stakeholders. Am J Drug Alcohol Abuse. 2004;30:129–153. doi: 10.1081/ada-120029870. [DOI] [PubMed] [Google Scholar]
- 10.Beardsley K, Wish E, Fitzelle D, O’Grady K, Arria A. Distance traveled to outpatient drug treatment and client retention. J Substance Abuse Treatment. 2003;25:279–285. doi: 10.1016/s0740-5472(03)00188-0. [DOI] [PubMed] [Google Scholar]
- 11.Galanter M, Keller DS, Dermatis H, Egelko S. The impact of managed care on substance abuse treatment: A report of the American Society of Addiction Medicine. J Addictive Behaviors. 2000;19:13–34. doi: 10.1300/J069v19n03_02. [DOI] [PubMed] [Google Scholar]
- 12.Kail B, Elberth M. Moving the Latina substance abuser toward treatment: The role of gender and culture. J Ethnicity Substance Abuse. 2002;3:3–16. [Google Scholar]
- 13.Farabee D, Leukefeld CG, Hays L. Accessing drug-abuse treatment: perceptions of out-of-treatment injectors. J Drug Issues. 1998;28(2):381–394. [Google Scholar]
- 14.Knight KR, Rosenbaum M, Kelley MS, Irwin J, Washburn A, Wenger L. Defunding the poor: The impact of lost access to subsidized methadone maintenance treatment on women injection drug users. J Drug Issues. 1996;26(4):923–942. [Google Scholar]
- 15.Festinger DS, Lamb RJ, Kountz MR, Kirby KC, Marlowe D. Pretreatment dropout as a function of treatment delay and client variables. Addictive Behaviors. 1995;20:111–115. doi: 10.1016/0306-4603(94)00052-z. [DOI] [PubMed] [Google Scholar]
- 16.Fountain J, Strang J, Griffiths P, Powis B, Gossop M. Measuring met and unmet need of drug misusers: Integration of quantitative and qualitative data. European Addiction Research. 2000;6:97–103. doi: 10.1159/000019017. [DOI] [PubMed] [Google Scholar]
- 17.French MT, Dunlap LJ, Galinis DN, Rachal JV, Zarkin GA. Health care reforms and managed care for substance abuse services: Findings from eleven case studies. J Public Health Policy. 1996;17:181–203. [PubMed] [Google Scholar]
- 18.Wenger LD, Rosenbaum M. Drug treatment on demand—not. J Psychoactive Drugs. 1994;26(1):1–11. doi: 10.1080/02791072.1994.10472597. [DOI] [PubMed] [Google Scholar]
- 19.Yancovitz SR, Des Jarlais DC, Peyser NP, Drew E, Friedmann P, Trigg HL, Robinson JW. A randomized trial of an interim methadone maintenance clinic. Am J Public Health. 1991;81:1185–1191. doi: 10.2105/ajph.81.9.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alterman AI, Bedrick J, Howden D, Maany I. Reducing waiting time for substance abuse treatment does not reduce attrition. J Substance Abuse. 1994;6:325–332. doi: 10.1016/s0899-3289(94)90513-4. [DOI] [PubMed] [Google Scholar]
- 21.Office of National Drug Control Policy. [Last accessed May 20, 2005];National Drug Control Strategy. 2002 Available at http://www.whitehousedrugpolicy.gov/publications/policy/03ndcs/2priorities.html.
- 22.Kahn JG, Stump D, Davis T, McConnel CE, Gleghorn A, Stillwell J, Guydish J. Substance Abuse Treatment On Demand: The Effect of Increased Funding on Treatment Capacity in San Francisco, 1995–1999. San Francisco, CA: UCSF Institute of Health Policy Studies; 2004. [Google Scholar]
- 23.SAS Institute Inc. SAS/ETS® User’s Guide, Version 6. 2. Cary, NC: SAS Institute; 1993. p. 1.p. 22. [Google Scholar]


