Abstract
We experienced a case of acute myocarditis as the initial presentation of Crohn's disease. A 19-year-old woman was admitted with impaired consciousness, shock, and respiratory failure. She had suffered from frequent diarrhea and abdominal pain for several years. Cardiac troponin I and creatine kinase-MB fraction levels were elevated to 5.32 and 16.66 ng/mL, respectively. A 12-lead electrocardiogram showed sinus tachycardia, and a chest radiograph revealed interstitial pulmonary edema. An echocardiogram showed dilated ventricles with akinesia of the basal to apical inferoseptal, anteroseptal, anterior, and inferior left ventricular walls and severely impaired systolic function. Intensive care with inotropic support was effective, and her clinical condition gradually improved. Two weeks later, a colonoscopy revealed ulceration with stenosis in the terminal ileum and multiple aphthous ulcers in the rectum. A biopsy of the rectum revealed non-caseating granulomatous inflammation. She was diagnosed with Crohn's disease presenting with acute myocarditis.
Keywords: Crohn disease, Myocarditis
INTRODUCTION
Crohn's disease, an idiopathic inflammatory bowel disease (IBD), can affect any part of the gastrointestinal (GI) tract from the mouth to the anus, and can show extraintestinal manifestations.1 Myocarditis is a rare extraintestinal complication of IBD that can occur as an initial manifestation of Crohn's disease and also independently of bowel disease activity.2,3 We report here on a case of acute myocarditis as the initial presentation of Crohn's disease and review the literature.
CASE REPORT
A 19-year-old woman was admitted with impaired consciousness. She was a university student and social drinker of less than 50 g per week. She had no specific medication and travel history. Other past medical history was unremarkable. She suffered from frequent diarrhea and abdominal pain for several years. Her diarrheal symptom had progressively worsened for 2 months before admission. Three days prior to admission, she presented with high fever, headache, and myalgia.
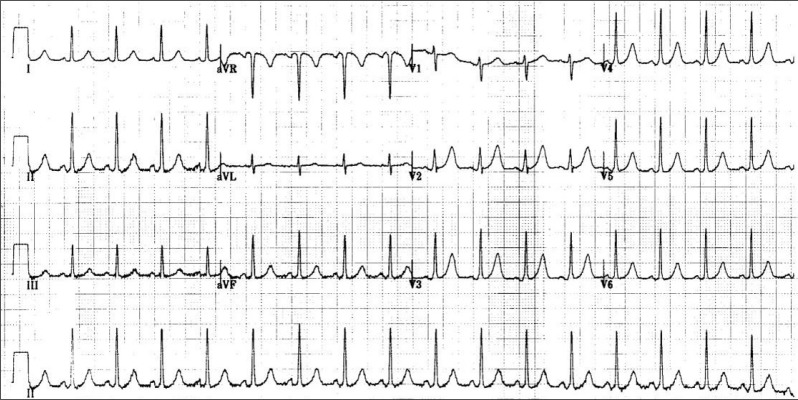
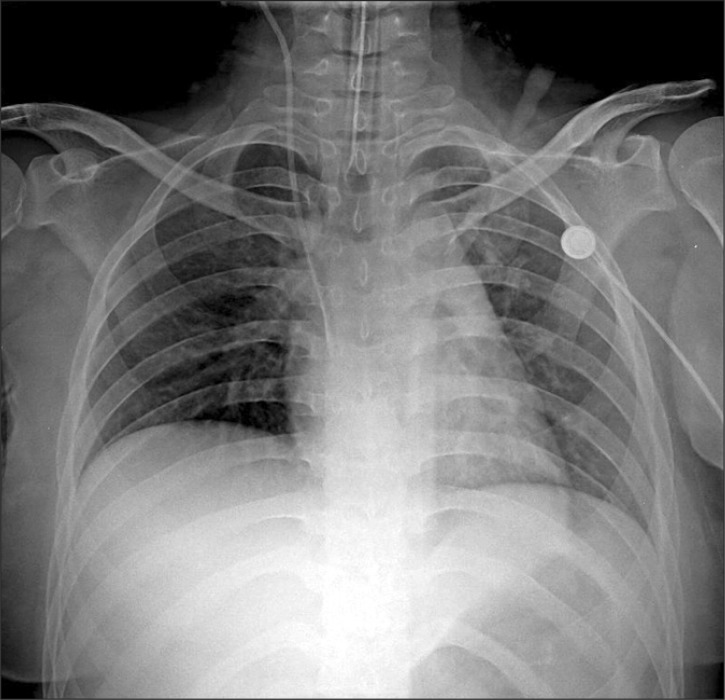
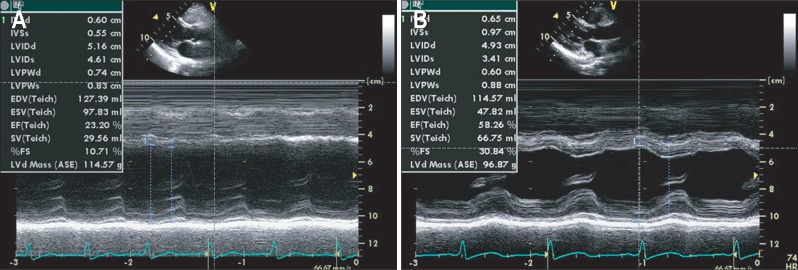
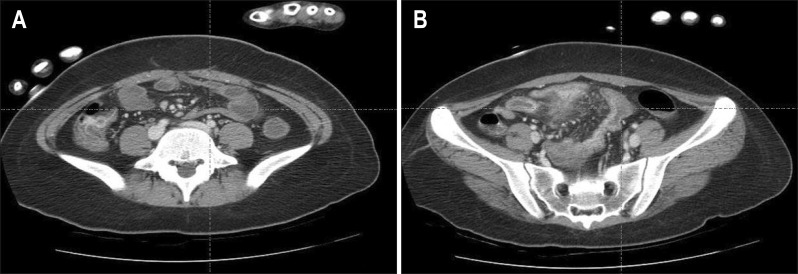
On admission, her vital signs were unstable: blood pressure of 70/40 mm Hg, pulse rate 130 beats/min, body temperature 41.0℃, and respiratory rate 35/min. Her mental status was stuporous. The abdomen was diffusely tender and distended without palpable mass. Laboratory findings showed a white blood cell count of 21,440/mm3 with 92% neutrophil, hemoglobin 13.4 g/dL, platelet 332,000/µL, urea 10 mg/dL, creatinine 1.1 mg/dL, and C-reactive protein 92.9 mg/L. Cardiac troponin I and creatine kinase-MB were elevated to 5.32 and 16.66 ng/mL, respectively. Human immunodeficiency virus antibody, hepatitis B surface antigen antigen, hepatitis C virus antibody, and anti-nuclear antibody were negative. The blood and urine cultures and stool examinations were not remarkable. A 12-lead electrocardiogram showed sinus tachycardia (Fig. 1) and a chest radiograph revealed a normal-shaped heart but interstitial pulmonary edema (Fig. 2). A Doppler echocardiogram showed dilated ventricles with akinesia of the basal to apical inferoseptal, anteroseptal, anterior, and inferior left ventricular (LV) wall and severely impaired systolic function: the estimated ejection fraction was 38% (Fig. 3A and B). Fulminant myocarditis with acute LV failure was diagnosed. An abdominal-pelvic computed tomography scan showed active inflammatory wall thickening in the distal ileum and sigmoid colon, associated mesenteric hyperemia and intervening normal segments of the ileum (Fig. 4). She was admitted to the intensive care unit with intubation and received ventilator care. Intravenous hydration and inotropic support with dopamine, noradrenaline, and dobutamine were performed.
Fig. 1.
Sinus tachycardia was noted in 12-lead electrocardiogram.
Fig. 2.
Initial chest X-ray revealed interstitial pulmonary edema.
Fig. 3.
(A) At admission, Doppler echocardiography showed dilated ventricles with akinesia of the basal to apical inferoseptal, anteroseptal, anterior and inferior left ventricular (LV) wall, and severe LV dysfunction (ejection fraction, 38%). (B) LV wall motion was markedly improved on follow-up echocardiography 8 days later (ejection fraction, 62%).
Fig. 4.
(A, B) Abdominal-pelvic computed tomography scan demonstrated active inflammatory wall thickening in the distal ileum and sigmoid-colon, associated mesenteric hyperemia, and intervening normal segments of the ileum.
On the next day, her clinical condition gradually improved and the intubation tube could be removed. Cardiac troponin I were decreased to 0.857 ng/mL. To identify the cause of myocarditis, viral antibody titers, such as coxsackie virus, adenovirus, rubella virus, mumps virus, cytomegalovirus, and human herpes virus, were checked. Among them, coxsackie virus A4, A16, B1, and B3, and adenovirus antibody titers were low positive (<1:16 dilution), and coxsackie virus B4 antibody titer was high positive (1:256 dilution). In the follow-up echocardiogram 1 week later, LV systolic function was markedly improved and the estimated ejection fraction was 62%. She was getting better and was discharged on the 10th hospital day. She has taken angiotensin-converting enzyme inhibitors to prevent cardiac decompensation.
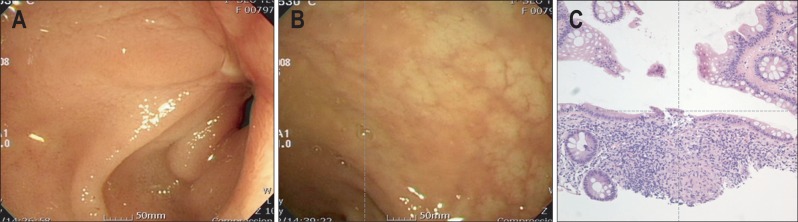
Four weeks later, a colonoscopy was performed. Colonoscopy showed ulceration with stenosis in the terminal ileum and multiple aphthous ulcers in the rectum (Fig. 5A and B). Rectal biopsy revealed a non-caseating granulomatous inflammation consistent with Crohn's disease (Fig. 5C). The Crohn's disease activity index was 177. We started treatment with oral steroids and mesalazine and her symptoms of abdominal pain and diarrhea improved. The disease has been well controlled with maintenance therapy using mesalazine and azathioprine.
Fig. 5.
(A, B) Initial endoscopic findings revealed ulceration with stenosis in the terminal ileum and multiple aphthous ulcers in the rectum. (C) A biopsy specimen showed non-caseating granulomatous inflammation (H&E stain, ×200).
Six months later, the antibody titer for coxsackie virus B4 was not changed (1:256 dilution), indicating that myocarditis was not caused by coxsackie virus infection.
DISCUSSION
Crohn's disease can affect the GI tract as well as cause extraintestinal complications.1 Extraintestinal manifestations of IBD occur in 42% of patients with colonic disease and 23% of patients with small bowel involvement.4 The main sites of extraintestinal manifestation are the joints (14% to 39% of patients), the skin (15%), the eye (4%), and the oral cavity (aphthous stomatitis, 4%).1,5 Rarely, cardiac problems such as pericarditis, pericardial effusion, myocarditis, endocarditis, and arrythmias can occur, but these can be fatal.6 These cardiac manifestations may also develop due to treatment side effects.7,8
Myocarditis may be more common at the beginning of IBD exacerbation and there is usually more than one extraintestinal manifestation present, but there is no direct relationship of the cardiac symptoms to disease activity.5 We found a case of acute myocarditis presenting as the initial complication of mildly active Crohn's disease. Viral and post-viral myocarditis remain major causes of acute and chronic dilated cardiomyopathy.9 To date, diagnosis of viral myocarditis has generally been based on the isolation of virus from another site, and the demonstration of a fourfold or greater rise in antibody titer from acute to convalescent sera.10 But the viral antibody titer of our case was not changed from acute to convalescent phase. Moreover, the sero-prevalence of coxsackie virus B4 in general population was not low (range, 9.3% to 19.1%).11 So, we assumed that her myocarditis was not associated with coxsackie B virus, but with Crohn's disease. In addition, there was no evidence of other possible cause for her myocarditis, such as infection, allergy, autoimmune diseases, and drugs. Similar case was reported in our country, but the patient experienced myocarditis during the treatment period with immunomodulator, steroid, and 5-aminosalicylic acid, and he was expired due to the myocarditis. In our case, myocarditis was developed in the patient who had not received treatment of Crohn's disease, and her cardiac symptoms were fully recovered.12 In a Danish cohort study, the risk ratio of myocarditis compared with the background population was 8.3 for Crohn's disease and 2.6 for ulcerative colitis.13
In the past, sepsis was the most common cause of death in patients with Crohn's disease, but GI cancer has become the leading cause of mortality. Moreover, pulmonary embolism, amyloidosis, steroid side effects, short bowel syndrome, protein losing enteropathy, and extraintestinal manifestations, such as ischemic heart diseases, cerebral vascular diseases, and congestive heart failure have increased in importance.1,14
In summary, we experienced a case of acute myocarditis as the initial complicated presentation of Crohn's disease and report this case with a review of the literature. Since the cardiac manifestations of Crohn's disease can be fatal, further work should explore the pathophysiology, natural history, and prognosis of these interactions.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Sands BE, Siegel CA. Crohn's disease. In: Sleisenger MH, Feldman M, Friedman LS, Brandt LJ, editors. Sleisenger and Fordtran's gastrointestinal and liver disease: pathophysiology, diagnosis, management. 9th ed. Volume 2. Philadelphia: Saunders; 2010. pp. 1941–1973. [Google Scholar]
- 2.Jackson JF, Sitaraman SV. Pericarditis as the presenting sign of Crohn's disease. Inflamm Bowel Dis. 2005;11:81–82. doi: 10.1097/00054725-200501000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Hyttinen L, Kaipiainen-Seppänen O, Halinen M. Recurrent myopericarditis in association with Crohn's disease. J Intern Med. 2003;253:386–388. doi: 10.1046/j.1365-2796.2003.01082.x. [DOI] [PubMed] [Google Scholar]
- 4.Greenstein AJ, Janowitz HD, Sachar DB. The extra-intestinal complications of Crohn's disease and ulcerative colitis: a study of 700 patients. Medicine (Baltimore) 1976;55:401–412. doi: 10.1097/00005792-197609000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Weiss N, Rademacher A, Zoller WG, Schlöndorff D. Myocarditis and subcutaneous granulomas in a patient with Crohn's disease of the colon. Am J Med. 1995;99:434–436. doi: 10.1016/s0002-9343(99)80194-6. [DOI] [PubMed] [Google Scholar]
- 6.Iizuka B, Yamagishi N, Honma N, Hayashi N. Cardio vascular disease associated with ulcerative colitis. Nihon Rinsho. 1999;57:2540–2545. [PubMed] [Google Scholar]
- 7.Kupferschmidt H, Langenegger T, Krähenbühl S. Pericarditis in chronic inflammatory bowel disease: underlying disease or side effects of therapy? Clinical problem solving. Schweiz Med Wochenschr. 1996;126:2184–2190. [PubMed] [Google Scholar]
- 8.Gujral N, Friedenberg F, Friedenberg J, Gabriel G, Kotler M, Levine G. Pleuropericarditis related to the use of mesalamine. Dig Dis Sci. 1996;41:624–626. doi: 10.1007/BF02282352. [DOI] [PubMed] [Google Scholar]
- 9.Cooper LT., Jr Myocarditis. N Engl J Med. 2009;360:1526–1538. doi: 10.1056/NEJMra0800028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Savoia MC, Oxman MN. Myocarditis and pericarditis. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 6th ed. Edinburgh: Elsevier Churchill Livingstone; 2004. pp. 1053–1058. [Google Scholar]
- 11.Mavrouli MD, Spanakis N, Levidiotou S, et al. Serologic prevalence of coxsackievirus group B in Greece. Viral Immunol. 2007;20:11–18. doi: 10.1089/vim.2006.0085. [DOI] [PubMed] [Google Scholar]
- 12.Kwon CI, Hong SP, Choi YJ, et al. A case of acute dilated cardiomyopathy caused by coxsackie virus B in a patient with Crohn's disease. Korean J Gastroenterol. 1999;34:125–130. [Google Scholar]
- 13.Sorensen HT, Fonager KM. Myocarditis and inflammatory bowel disease. A 16-year Danish nationwide cohort study. Dan Med Bull. 1997;44:442–444. [PubMed] [Google Scholar]
- 14.Andrews HA, Lewis P, Allan RN. Mortality in Crohn's disease: a clinical analysis. Q J Med. 1989;71:399–405. [PubMed] [Google Scholar]