Abstract
Environmental assessment and exposure reduction are a set of diagnostic and treatment techniques that work in tandem with the traditional medical approach by reducing a patient’s exposure to adverse environmental conditions as part of medical care. Assessment involves identifying the specific exposures to which a patient is sensitive and locating the corresponding contaminants in the patient’s environment. This provides a more complete diagnostic evaluation of a patient’s problem than could be obtained merely by examining the patient alone. Exposure reduction involves reducing the identified triggers to levels that are below thresholds that are associated with increased risk of sensitization and disease morbidity.
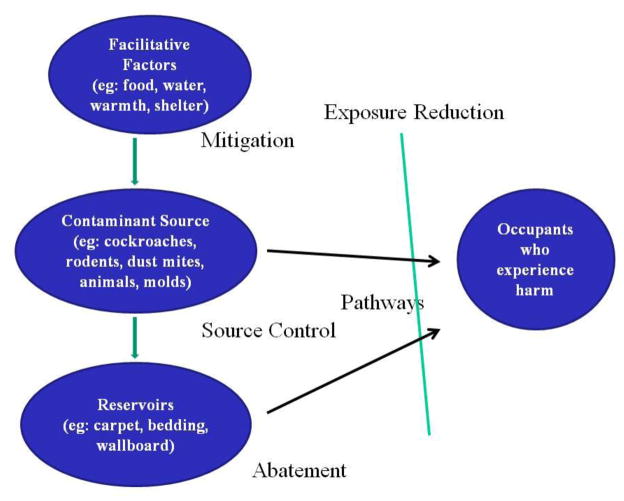
Assessment of an environment for contaminants focuses on a chain of factors that include contaminant sources such as cockroaches, rodents, dust mites and fungi that excrete contaminants into an environment, facilitative factors such as moisture, food, water and shelter that help sources to thrive, and reservoirs where contaminants can accumulate prior to subsequent transport to occupants. By using this model to guide environmental assessments and their corresponding interventions, the root cause of health problems can be addressed, leading to improved quality of life for patients and reduced need for chronic medications.
Keywords: Environmental control, Abatement, Mitigation, Model, Environmental assessment, Exposure, Reduction, Contaminants, Interventions, Reservoirs, Pathways
Introduction
Environmental assessment and exposure reduction have been a mantra of the allergy profession almost since its inception. The idea is straightforward: a patient with a medical problem that is likely to be triggered by adverse environmental exposures is evaluated by an allergist who helps the patient to identify those exposures. Given that information, the patient is instructed to avoid future exposure using a variety of environmental interventions generically termed “avoidance”. As a result of this advice, the illness abates, the patient can reduce his or her intake of medications, and all is well.
While this approach sounds rational, in practice it is not easily achieved (1). The problem is that many patients are sensitive to multiple environmental triggers, many of which have not been fully characterized and for which there are no readily available tests. In addition, since many exposures are ubiquitous, interventions to completely avoid them are not practical and therefore do not work. Finally, many patients are not willing to perform the recommended environmental interventions unless the situation is so extreme that they are forced to do so (2).
Certainly, it is not possible to avoid outdoor allergens unless the patient is willing to stay indoors throughout seasons when they are airborne. Indoor allergens, on the other hand, do have the potential of being controlled and therefore have been the focus of substantial research. Recently, in acknowledgement of the need for standardized approaches to environmental assessment with intervention, the Joint Taskforce on Practice Parameters has started to develop a series of practice guidelines for the management of environmental exposures (3).
This review will describe our current understanding of how adverse indoor environmental exposures are formed, where they are located, and how they travel from reservoirs to building occupants. Interventions including integrated pest management (IPM) are also briefly reviewed with an emphasis on how they integrate into a new model for exposure reduction.
The model
Health problems occur as a result of environmental exposures to substances referred to as contaminants (3). A contaminant is defined generically as any physical, chemical, biological, or radioactive substance that can have an adverse effect on air, water or soil, or on any interior or exterior surface, and that has the potential to cause harm to a building’s occupants. Contaminants can consist of allergens, irritants or other types of substances, including biologically active ones. A mechanism for the production of allergen contaminants usually consists of biologic organisms such as fungi, rodents, dust mites, furry animals and insects. Non-allergen contaminant sources include chemical reactions, combustion by-products, particulates, and microbial organisms that produce substances such as endotoxin and volatile organic compounds.
Production of contaminants by biologic organisms can be facilitated when certain environmental conditions are present. Examples of such conditions include moisture, food, warmth and shelter, which are prerequisites for survival of most biologic organisms. Non-allergen contaminants do not require such conditions but are produced through both normal daily maintenance activity and when home conditions are altered by a significant event (construction, renovation, disaster restoration). This can include use of household products, introduction of new building materials, or more common activities such as burning candles, certain hobbies, and occupational substances.
Once contaminants are produced, they tend to remain in the environment, forming reservoirs until they either decay or dissipate. Common reservoirs for allergens include carpets, bedding, upholstered furniture, settled dust, wall cavities, inside cabinets, air ducts, and crawlspaces (4), While contaminants are present in reservoirs, they have a potential to travel along pathways to the living space of occupants where they can cause adverse health effects. Contaminants can travel via air and water, and on fomites (inanimate objects) or vectors (living animals).
Figure 1 shows this model of environmental exposure, starting with facilitative factors which assist organisms that serve as sources of allergens. Allergens are either transported to occupants along pathways or deposited in reservoirs from which they subsequently travel to the occupants. By understanding how these factors fit together, it is possible to measure the contributions of each and to design a feasible intervention plan that is likely to reduce occupant exposure.
Figure 1.
A model for contaminant production leading to occupant exposure.
Health Effects of Environmental Exposures
The effect that contaminant exposure has on health depends on the amount and duration of the exposure, the intrinsic biologic effect of the exposure, and the sensitivity to it of occupants. The amount of exposure that is associated with sensitization (development of specific IgE), sensitivity (development of symptoms after exposure to the allergen), and morbidity (long-term adverse health effects from ongoing exposure) has been studied extensively. Suggested exposure thresholds for selected allergens that are associated with development of symptoms in sensitized people are shown in Table 1.
Table 1.
Allergen exposure thresholds reported in studies of health effects. (Data from Salo et al. [31].)
| Dust Mmite (Der p 1) | 2 mμcg/gram |
| Dust Mmite (der f 1) | 2 mcμg/gram |
| Cat (fFel d 1) | 8 mcμg/gram |
| Dog (Can f 1) | 10 mcμg/gram |
| German Ccockroach (Bla g 1) | 2 Uunits/gram |
| German Ccockroaoch (Bla g 2) | 0.04 mcμg/gram |
| Mouse (Mus m 1) | 1.6 mcμg/gram |
For each of these allergens, there are data demonstrating that patients with exposure below each threshold experience fewer symptoms and less morbidity than those who are exposed to levels above the threshold. Even so, it should not be assumed that exposure to an allergen level below one of these thresholds is safe and above these thresholds is inevitably harmful. The shape of the dose response curve for most allergens is not known. It is just as likely that a sigmoidal curve is a more accurate representation of the health effects of a given exposure, suggesting that reduction of exposure to levels significantly below the suggested threshold may be necessary to achieve health benefits.
It is important to note that the relationship between exposure and health effects is not necessarily causal. The studies supporting this relationship are usually population studies that are either cross-sectional or observational, providing correlations between exposure and symptoms. The reason for this is that it would not be feasible to perform a randomized study in which selected subjects are exposed to increased allergen levels from birth while controls are not. Interventional studies in which exposure reduction leads to reduced symptoms supports the use of exposure reduction, but it does not prove that living in an intrinsically more allergenic environment causes the health effects.
Interventions
The goal of environmental interventions is to reduce occupant exposure to contaminants to concentrations that are below the threshold that causes adverse health effects. Interventions designed to prevent development of specific IgE antibodies using exposure reduction are referred to as primary prevention (5,6). What is interesting is that exposure to increased amounts of furry animal allergens in the first few months of life seems to provide a protective effect by reducing the risk of sensitization (7). This same effect is not found for cockroach (8) or mold, and the data are unclear for rodents.
Once a patient develops specific IgE antibodies, exposure reduction is necessary to prevent future development of a disease such as asthma. This is referred to as secondary prevention (9). Tertiary prevention, otherwise known as treatment, is necessary once a sensitized individual has developed asthma to prevent morbidity that would be caused by the exposure (10).
While a variety of individual interventions have been evaluated, none have proven to be effective for avoiding any of the allergens listed in Table 1 by itself. It appears to be necessary to combine interventions for this type of reduction to be achieved. For allergen sources such as cockroaches and rodents, strategies such as integrated pest management (IPM) are essential (11). Other exposures such as dust mites and fungi require similar strategies without the behavior components, since such organisms do not learn to thwart interventions the way that rats and cockroaches do. Furry animals have their own set of challenges since homeowners often prefer to keep a pet in the house regardless of their allergy status.
This model of exposure reduction provides a framework for designing interventions. To reduce exposure, it is necessary to provide interventions that address each component of the model including facilitative factors, sources, reservoirs, and pathways. If any of these are left unmanaged, it is likely that the exposure reduction will be unsuccessful. For example, a combination of education, use of insecticides, professional cleaning, and habitat alteration appears to be necessary for cockroach control because it addresses facilitative factors, causative organisms, and reservoirs in combination. Application of insecticides alone can reduce the number of cockroaches in a house, but this does not necessarily lead to improved health (12).
Facilitative Factors
Facilitative factors for cockroaches and rodents include a means of ingress, appropriate temperature, food, water, and shelter. For that reason, IPM, which focuses on these pests, first emphasizes identification of facilitative factors. Once identified, interventions include sealing of openings that permit pests to enter a building, removal of food and water from areas where the pests can get to them, and elimination of clutter and other places where pests can find shelter. Elimination of facilitative factors reduces the carrying capacity of the environment for the pests (11). As a result, rodents and cockroaches either have to migrate somewhere else or die due to lack of resources needed to survive. Fungi and dust mites also require moisture and food to survive; however, they can thrive on sources that are not necessarily apparent. Moisture resulting from external sources (intrusion) or internal sources (condensation, leakage) may be sufficient to support growth of these microscopic sources. Food in the form of cellulose for fungi and skin cells for dust mites may be difficult to remove and result from a recurring water problem, which is why an emphasis is placed on moisture control (13).
Interventions that eliminate facilitative factors, therefore, include use of dehumidifiers to reduce humidity below 50%, elimination of sources of moisture, sealing of food and water containers, and elimination of clutter. In general, patients are moderately willing to reduce humidity; however, their willingness to perform other interventions less clear. The more difficult the intervention, the less likely it is to be done (2).
Sources
Sources of allergens consist of the organisms that produce them. Furry animals produce dog and cat allergens merely by their presence in the environment. To date, there are no proven non-allergenic dogs or cats despite advertisements to the contrary. Since most animal allergens are released in their sebaceous secretions, washing the animals regularly has been shown to reduce dissemination into the environment (14, 15). Denaturation with tannic acid or bleach can also reduce cat allergen exposure (16). In general, most patients are not willing to eliminate a pet though they are willing to wash pets regularly and to keep them out of bedrooms (2).
Cockroaches continue to produce allergens, irritants such as chitin, and other inflammatory substances as long as they are present. Though reduction of the carrying capacity of the environment for cockroaches will eventually lead to decreased numbers, it may also be necessary to exterminate them to achieve a rapid reduction where an infestation exists. Glue boards can be used to monitor the extent of an infestation and its duration. If all captured cockroaches are from a single generation, the infestation is short-term. Representation from a variety of stages on a glue board suggests a longer-term problem. Extermination can be done using a variety of insecticides, though it is important that as part of an IPM plan they are applied through targeted deployment using baits and gels according to the manufacturer’s instructions to avoid adverse health effects on the building occupants. Ideally, a licensed, professional pest control contractor should apply insecticides (17).
Rodents produce significant allergens in their urine which they distribute as they move about. While elimination of rodents begins by eliminating facilitative factors, they can also be removed using snap traps, live traps, and glue boards. Predators such as cats can also reduce rodent populations, though there is a risk that the occupant could become sensitized to the cat (18). Rodenticides usually consisting of anticoagulants can also be used, though, as with insecticides, it is essential that these be applied properly using bait stations to avoid unintentional harm to other nontargeted animals (19).
Dust mites produce allergens in their fecal pellets. They generally live in bedding, carpets, and upholstered furniture and dine on skin cells, fungi, and each other. While acaricides such as benzoic acid have been used to eliminate dust mites, it is usually more feasible to eliminate the facilitative factors including moisture to reduce dust mite populations. The mites themselves are difficult to eliminate though they can be killed with washing in hot water and/or drying in high heat (20).
Fungi produce numerous allergens, irritants, and proinflammatory substances including volatile organic compounds. Molds can be removed from surfaces using detergent and water and killed using a dilute bleach solution as well as a variety of fungicides, but these need to be applied regularly to prevent regrowth (21). As long as the facilitative factors are present, fungi will grow. For that reason, an emphasis is placed on removal of moisture which is the main facilitative factor. If the substrate on which a fungus is growing is desiccated, the organism will not grow (13).
Reservoirs
Once elimination of facilitative factors and removal of the sources of allergen production has been accomplished, it is also necessary to remove reservoirs of allergens. Such reservoirs can remain for long periods of time before the allergens either decay into nonallergenic fragments or are removed. As long as the reservoirs are present, exposure of occupants will continue. The specific type of reservoir that needs mitigation depends on the source and type of allergen. Furry animals, dust mites, and fungi often leave allergens in carpeting and upholstered furniture. Cockroaches and rodents leave allergens in walls, along baseboards and in contaminated clutter.
Carpeting and upholstered furniture can be cleaned with a HEPA or high efficiency vacuum or with a central vac. Vacuums with low-efficiency bags tend to redistribute allergens and can make the reservoir worse. Mattresses can be covered with allergen-impermeable covers that separate allergens and dust mites from where the occupant sleeps. Fungus-contaminated wallboard and other materials may be cleaned with soap and water or with a dilute bleach solution if the degree of contamination is small. More extensively affected areas need to be removed and replaced.
The use of HEPA cleaners either in the HVAC or stand-alone units has been reviewed (22). The authors in this extensive review concluded that portable room air cleaners with HEPA filters appear to reduce occupant exposure. This is particularly true if the filter clears the breathing zone during sleep. In addition, the use of high-efficiency disposable filters is useful with forced-air HVAC systems along with regular maintenance (23).
Pathways
While ideally sources and reservoirs should be abated, it is also important to prevent residual allergens from traveling from remaining locations to occupants. Transport of contaminants can occur in air if the particles are small enough to become airborne and to remain airborne long enough to travel from sources and reservoirs to occupants. Pathways can occur when air ducts are leaky or when air circulates from contaminated areas to clean ones. Volatile compounds require ventilation for their removal. For these reasons, differential building pressures and differential pressure between rooms becomes an important consideration in both assessing exposure and in recommending effective interventions.
Implications
A number of studies have examined the efficacy of cockroach and rodent removal with subsequent reduction in allergen exposure, as a way to improve asthma symptoms. Researchers from the Inner City Asthma Study (ICAS) were the first to demonstrate that environmental interventions reduced asthma symptoms. They demonstrated that one year of interventions, which included professional cleaning, bait traps, insecticides, and HEPA filters, was sufficient to reduce cockroach allergen levels, and that these improvements were significantly correlated with decreased wheeze, decreased nighttime asthma symptoms, and fewer missed school days. In addition, clinical improvement persisted for at least one year after the environmental intervention had ceased (24). In a similar study, Eggleston et al. used environmental interventions to reduce cockroach allergen and, subsequently, daytime asthma symptoms (25).
On the other hand, the National Inner City Asthma Study demonstrated a decrease in cockroach allergen that persisted for 6 months after interventions, but levels had returned to baseline by 12 months (26). As noted previously, Sever et al. found significant reduction in cockroach allergen 12 months after interventions performed by professional entomologists, but no reduction at 12 months after intervention by a commercial pest removal company (17). This demonstrates that continuous efforts (professionally or family directed) to eliminate these allergens may be necessary for sustained cockroach allergen reduction. Similar long-term studies are needed on the reduction of rodent allergen.
The efficacy of IPM for rodents had some success in the ICAS where Mus m 1 levels were reduced by a small but significant 27 % (27). A subset of children whose homes had at least a 50 % reduction in Mus m 1 had fewer missed school days, reduced sleep disruption, and reduced caretaker burden, suggesting that an intervention that can achieve at least a 50 % reduction in allergen levels may improve asthma (28).
For furry animals, a multiple intervention study demonstrated that 11 months of biweekly cat washing, use of mattress and pillow encasings, weekly washing of encasings at 60°C, excluding the cat from the bedroom, and application of tannic acid led to reductions of Fel d 1 concentration in house dust by 91.4 % in an active intervention group but not in a control group (29). While a combination of environmental interventions does seem to be effective in the reducing the cat allergen load in homes, they also appear to lead to reduced symptoms. Such intervention combinations, involving both mechanical methods for allergen reduction and educational efforts of asthmatic children and their parents, appear to be necessary to reduce exposure to asthma triggers and improved health outcomes for asthmatic children (30).
Conclusions
The traditional medical approach involves diagnosing what is wrong with the patient and fixing it, usually with medications. Since respiratory and many other illnesses are, at least in part, exacerbated by adverse environmental exposures, it seems only reasonable that diagnosis and treatment aimed at a patient’s environment should be part of routine care.
Environmental assessment and exposure reduction has the potential to reduce exposure to adverse environmental conditions. If such exposures can be decreased to levels that are below thresholds associated with increased risk of sensitization and disease morbidity, patients may experience improved health while taking less medication. By focusing on facilitative factors, contaminant sources, and reservoirs, environmental assessment and its corresponding set of interventions can be incorporated into routine medical care. The challenge will be to make this transition in an era of tightening healthcare resources.
Footnotes
Disclosure Dr. Portnoy has served as a consultant for, received honoraria from, and had travel/accommodations expenses covered/reimbursed by Thermofisher.
Drs. Ciaccio and Kennedy reported no potential conflicts of interest relevant to this article.
References
- 1.Schatz M, Zeiger RS. Ineffectiveness of telephone-based environmental control intervention to improve asthma outcomes. J Allergy Clin Immunol. 2010;126(4):873–5. doi: 10.1016/j.jaci.2010.07.035. Epub 2010/10/06. [DOI] [PubMed] [Google Scholar]
- 2**.Schatz M, Zeiger RS. Telephone-based environmental control interventions in asthmatic patients: what are patients willing to do? Ann Allergy Asthma Immunol. 2012 doi: 10.1016/j.anai.2012.03.001. In press. Of major importance. This study and the earlier one (reference 1) determined what patients are actually willing to do about environmental control. This is important because if patients are not willing to modify their enviornment, the interventions described in this review will not be effective. [DOI] [PubMed] [Google Scholar]
- 3**.Portnoy J, Kennedy K, Sublett J. Environmental assessment and exposure control: a practice parameter-furry animals. Ann Allergy Asthma Immunol. 2012;108(4):223 e1–e15. doi: 10.1016/j.anai.2012.02.015. Epub 2012/04/04. Of major importance. This is the first in a series of practice parameters that address the issue of environmental assessment and source reduction. The basics of the new model are described and practical, evidence-based recommendations are provided. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis RD, Breysse PN, Lees PS, Diener-West M, Hamilton RG, Eggleston P. Factors affecting the retention of dust mite allergen on carpet. Am Ind Hyg Assoc J. 1998;59(9):606–13. doi: 10.1080/15428119891010776. Epub 1998/10/21. [DOI] [PubMed] [Google Scholar]
- 5.Ciaccio CE, Portnoy JM. Strategies for primary prevention of atopy in children. Curr Allergy Asthma Rep. 2008;8(6):493–9. doi: 10.1007/s11882-008-0090-y. Epub 2008/10/23. [DOI] [PubMed] [Google Scholar]
- 6.Arshad SH, Bateman B, Matthews SM. Primary prevention of asthma and atopy during childhood by allergen avoidance in infancy: a randomised controlled study. Thorax. 2003;58(6):489–93. doi: 10.1136/thorax.58.6.489. Epub 2003/05/31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7*.Wegienka G, Johnson CC, Havstad S, Ownby DR, Zoratti EM. Indoor pet exposure and the outcomes of total IgE and sensitization at age 18 years. J Allergy Clin Immunol. 2010;126(2):274–9. 9 e1–5. doi: 10.1016/j.jaci.2010.05.001. Epub 2010/06/29. Of importance. This article demonstrated that indoor exposure to pet allergens has an important impact on sensitization 18 years later. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arruda LK, Vailes LD, Ferriani VP, Santos AB, Pomes A, Chapman MD. Cockroach allergens and asthma. J Allergy Clin Immunol. 2001;107(3):419–28. doi: 10.1067/mai.2001.112854. Epub 2001/03/10. [DOI] [PubMed] [Google Scholar]
- 9.Prevention strategies for asthma--secondary prevention. CMAJ. 2005;173(6 Suppl):S25–7. Epub 2005/09/15. [PMC free article] [PubMed] [Google Scholar]
- 10.Sheikh A, Hurwitz B, Nurmatov U, van Schayck CP. House dust mite avoidance measures for perennial allergic rhinitis. Cochrane Database Syst Rev. 2010;(7):CD001563. doi: 10.1002/14651858.CD001563.pub3. Epub 2010/07/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11**.Sheehan WJ, Rangsithienchai PA, Wood RA, Rivard D, Chinratanapisit S, Perzanowski MS, et al. Pest and allergen exposure and abatement in inner-city asthma: a work group report of the American Academy of Allergy, Asthma & Immunology Indoor Allergy/Air Pollution Committee. J Allergy Clin Immunol. 2010;125(3):575–81. doi: 10.1016/j.jaci.2010.01.023. Epub 2010/03/17.Of major importance. This report reviews the data demonstrating that IPM is effective and which interventions are necessary to result in improved health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arbes SJ, Jr, Sever M, Mehta J, Gore JC, Schal C, Vaughn B, et al. Abatement of cockroach allergens (Bla g 1 and Bla g 2) in low-income, urban housing: month 12 continuation results. J Allergy Clin Immunol. 2004;113(1):109–14. doi: 10.1016/j.jaci.2003.10.042. Epub 2004/01/10. [DOI] [PubMed] [Google Scholar]
- 13.WHO guidelines for indoor air quality :dampness and mould. Copenhagen, Denmark: World Health Organization; 2009. [PubMed] [Google Scholar]
- 14.Avner DB, Perzanowski MS, Platts-Mills TA, Woodfolk JA. Evaluation of different techniques for washing cats: quantitation of allergen removed from the cat and the effect on airborne Fel d 1. J Allergy Clin Immunol. 1997;100(3):307–12. doi: 10.1016/s0091-6749(97)70242-2. Epub 1997/10/06. [DOI] [PubMed] [Google Scholar]
- 15.Hodson T, Custovic A, Simpson A, Chapman M, Woodcock A, Green R. Washing the dog reduces dog allergen levels, but the dog needs to be washed twice a week. J Allergy Clin Immunol. 1999;103(4):581–5. doi: 10.1016/s0091-6749(99)70227-7. Epub 1999/04/13. [DOI] [PubMed] [Google Scholar]
- 16.Matsui E, Kagey-Sobotka A, Chichester K, Eggleston PA. Allergic potency of recombinant Fel d 1 is reduced by low concentrations of chlorine bleach. J Allergy Clin Immunol. 2003;111(2):396–401. doi: 10.1067/mai.2003.11. Epub 2003/02/18. [DOI] [PubMed] [Google Scholar]
- 17.Sever ML, Arbes SJ, Jr, Gore JC, Santangelo RG, Vaughn B, Mitchell H, et al. Cockroach allergen reduction by cockroach control alone in low-income urban homes: a randomized control trial. J Allergy Clin Immunol. 2007;120(4):849–55. doi: 10.1016/j.jaci.2007.07.003. Epub 2007/09/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Curtin-Brosnan J, Saams J, Breysse P, diette G, Bradley H, Matsui E. Relationship between Cat and Mouse Allergen Levels in the Homes of Inner City Children with Asthma. J Allergy Clin Immunol. 2009:S64. [Google Scholar]
- 19.Dodds W, Frantz S, Story K. The Professional’s Guide to Managing Poisoning by Anticoagulant Rodenticides. New York: Chempa Products Div., Lipha Chemicals, Inc; 1986. [Google Scholar]
- 20.Arlian LG, Vyszenski-Moher DL, Morgan MS. Mite and mite allergen removal during machine washing of laundry. J Allergy Clin Immunol. 2003;111(6):1269–73. doi: 10.1067/mai.2003.1547. Epub 2003/06/06. [DOI] [PubMed] [Google Scholar]
- 21.Barnes CS, Kennedy K, Johnson L, Forrest E, Gard L, Pacheco F, et al. Use of dilute sodium hypochlorite spray and home cleaning to reduce indoor allergen levels and improve asthma health parameters. Ann Allergy Asthma Immunol. 2008;101(5):551–2. doi: 10.1016/S1081-1206(10)60297-9. Epub 2008/12/06. [DOI] [PubMed] [Google Scholar]
- 22*.Sublett JL, Seltzer J, Burkhead R, Williams PB, Wedner HJ, Phipatanakul W. Air filters and air cleaners: rostrum by the American Academy of Allergy, Asthma & Immunology Indoor Allergen Committee. J Allergy Clin Immunol. 2010;125(1):32–8. doi: 10.1016/j.jaci.2009.08.036. Epub 2009/11/17.Of importance. The definitive review of evidence for the use of air filtration. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson L, Ciaccio C, Barnes CS, Kennedy K, Forrest E, Gard LC, et al. Low-cost interventions improve indoor air quality and children’s health. Allergy Asthma Proc. 2009;30(4):377–85. doi: 10.2500/aap.2009.30.3257. Epub 2009/09/24. [DOI] [PubMed] [Google Scholar]
- 24.Morgan WJ, Crain EF, Gruchalla RS, O’Connor GT, Kattan M, Evans R, 3rd, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351(11):1068–80. doi: 10.1056/NEJMoa032097. Epub 2004/09/10. [DOI] [PubMed] [Google Scholar]
- 25.Eggleston PA, Butz A, Rand C, Curtin-Brosnan J, Kanchanaraksa S, Swartz L, et al. Home environmental intervention in inner-city asthma: a randomized controlled clinical trial. Ann Allergy Asthma Immunol. 2005;95(6):518–24. doi: 10.1016/S1081-1206(10)61012-5. Epub 2006/01/13. [DOI] [PubMed] [Google Scholar]
- 26.Gergen PJ, Mortimer KM, Eggleston PA, Rosenstreich D, Mitchell H, Ownby D, et al. Results of the National Cooperative Inner-City Asthma Study (NCICAS) environmental intervention to reduce cockroach allergen exposure in inner-city homes. J Allergy Clin Immunol. 1999;103(3 Pt 1):501–6. doi: 10.1016/s0091-6749(99)70477-x. Epub 1999/03/09. [DOI] [PubMed] [Google Scholar]
- 27.Krieger J, Jacobs DE, Ashley PJ, Baeder A, Chew GL, Dearborn D, et al. Housing interventions and control of asthma-related indoor biologic agents: a review of the evidence. J Public Health Manag Pract. 2010;16(5 Suppl):S11–20. doi: 10.1097/PHH.0b013e3181ddcbd9. Epub 2010/08/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pongracic JA, Visness CM, Gruchalla RS, Evans R, 3rd, Mitchell HE. Effect of mouse allergen and rodent environmental intervention on asthma in inner-city children. Ann Allergy Asthma Immunol. 2008;101(1):35–41. doi: 10.1016/S1081-1206(10)60832-0. Epub 2008/08/07. [DOI] [PubMed] [Google Scholar]
- 29.Juliusson S, Jakobinudottir S, Runarsdottir V, Blondal T, Gislason D. Environmental control (EC) can effectively reduce cat allergen (Fel d 1) in house dust samples without removal of the cat [abstract] J Allergy Clin Immunol. 1997;99:S388. [Google Scholar]
- 30.Wu F, Takaro TK. Childhood asthma and environmental interventions. Environ Health Perspect. 2007;115(6):971–5. doi: 10.1289/ehp.8989. Epub 2007/06/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salo PM, Arbes SJ, Jr, Crockett PW, Thorne PS, Cohn RD, Zeldin DC. Exposure to multiple indoor allergens in US homes and its relationship to asthma. J Allergy Clin Immunol. 2008;121(3):678–84. e2. doi: 10.1016/j.jaci.2007.12.1164. Epub 2008/02/08. [DOI] [PMC free article] [PubMed] [Google Scholar]