Abstract
Atrioventricular nodal reentrant tachycardia (AVNRT), caused by a reentry circuit involving fast and slow atrioventricular nodal pathways, is one of the most common types of paroxysmal supraventricular tachycardias. While familial Wolff-Parkinson-White syndrome has been well recognized, familial AVNRT has been rarely reported. We report a familial occurrence of AVNRT in a mother and her son, who were symptomatic and successfully treated with radiofrequency catheter ablation of slow pathway.
Keywords: Tachycardia, atrioventricular nodal reentrant
Introduction
Atrioventricular nodal reentrant tachycardia (AVNRT) is one of the most common forms of supraventricular tachycardias. Its mechanism is associated with a form of reentry involving two functional dual pathways in the atrioventricular (AV) node, including fast and slow pathways. Radiofrequency catheter ablation of slow pathway has become the definitive treatment of choice for most symptomatic AVNRT patients. The familial tendency of cardiac arrhythmias has gained great interest and advances in molecular genetics have demonstrated the exact genetic basis of familial arrhythmias. Familial Wolff-Parkinson-White (WPW) syndrome with autosomal dominant inheritance has long been recognized. The prevalence of pre-excitation among first-degree relatives of WPW syndrome patients is 3.4%.1) In addition, familial lone atrial fibrillation belongs to the family of "channelopathies" and is characterized by autosomal dominant inheritance, corresponding to a locus on chromosome 10.2) However, whether a genetic mechanism also contributes to the development of AVNRT has not been well known. Thus, we report a case of familial AVNRT clustering in a mother and her son.
Case
A 49-year-old woman and her 21-year-old son visited our outpatient department due to intermittent sudden palpitations. The mother had a history of intermittent disabling palpitation for over 20 years, but she had not been treated with any management. Her palpitation was provoked by coughing, sneezing or bending over and usually lasted about one to two hours. It did not terminate spontaneously until she put herself in a supine position. Her son also had a similar history of palpitation for over 7 years. Their palpations developed and terminated suddenly.
Physical examinations of both patients revealed no abnormal findings. Twelve-lead electrocardiographys (ECGs) showed a normal sinus rhythm and no delta wave, and 2-dimensional echocardiography findings were normal. Several ECGs failed to document any arrhythmia. However, paroxysmal supraventricular tachycardia was clinically suspected.
Electrophysiological studies of both patients were performed on the same day. Under local anesthesia and using a sterile technique, two quadripolar electrode catheters were positioned to record the activity of the His-bundle and right ventricular apex. A 7-Fr deflectable duodecapolar electrode catheter (Daig Corp., Minnetonka, MN, USA) was placed at the coronary sinus (CS) and the right atrium (RA) simultaneously via the right femoral vein. In our laboratory, we prefer to use a 7-Fr deflectable duodecapolar electrode catheter rather than a decapolar catheter since the duodecapolar electrode catheter has several advantages of simultaneous mapping of RA and CS, easier mapping of RA, and avoiding a discomfortable subclavian or jugular venous puncture in the patient. The duodecapolar catheters were not fully engaged into the distal CS in both patients, probably due to a small-sized CS or complicating Thebesian valve anatomy, such as semilunar, fenestrated or band shaped (Fig. 1A-D).
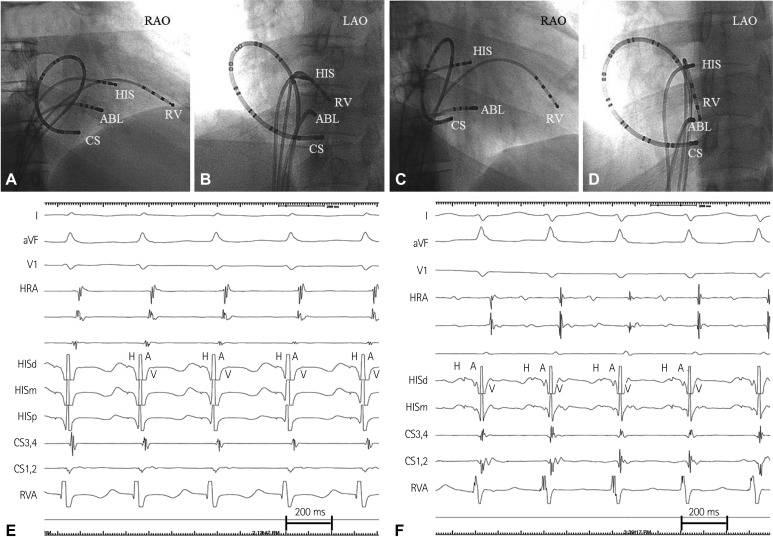
Fig. 1.
The mother's (A and B) and her son's (C and D) fluoroscopic images of endocardial mapping catheters in the right anterior oblique view (RAO) and the left anterior oblique view (LAO). The duodecapolar catheter was not fully engaged into the distal coronary sinus in both patients. The mother's (E) and her son's (F) intracardiac electrogram of typical atrioventricular nodal reentrant tachycardia (slow-fast type). During tachycardia, atrial activation is earliest at the HIS region and simultaneous with the ventricular activation. The VA interval (measured from the onset of ventricular activation on the surface electrocardiography to the earliest deflection of the atrial activation in the HIS electrogram) of both patients was <70 msec. HIS: His bundle, RV: right ventricle, HRA: high right atrium, CS: coronary sinus, ABL: ablation, VA: ventriculo-atrial, HISd: HIS distal, HISm: HIS middle, HISd: HIS distal.
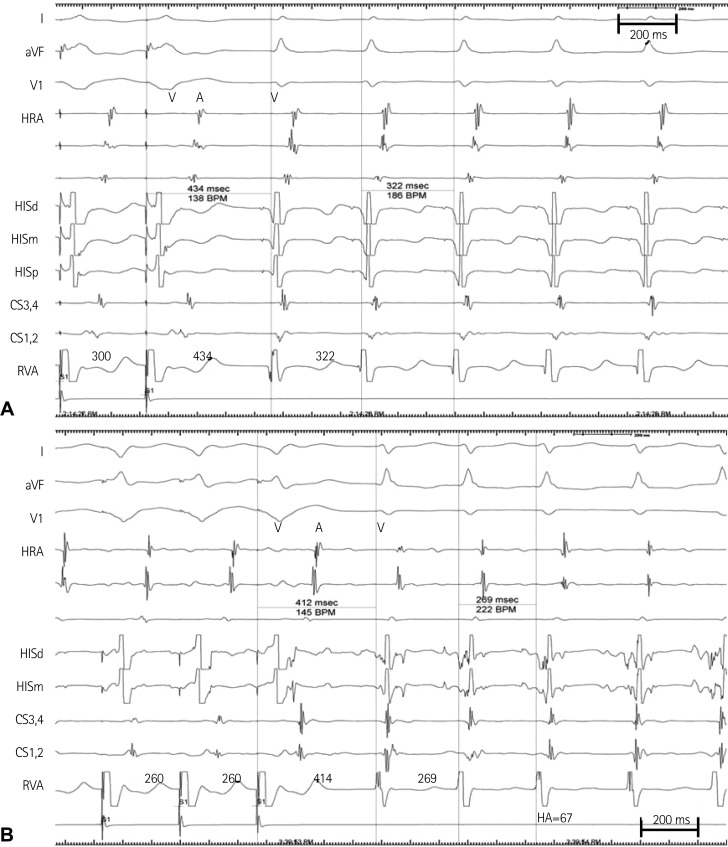
Programmed stimulation of the RA of both patients demonstrated dual AV nodal physiology, and a sustained narrow QRS complex tachycardia was reproducibly induced (cycle lengths of 307 msec in the mother and 292 msec in her son) during isoproterenol infusion (Fig. 1E and F). The short septal ventriculoatrial time of <50 ms and a V-A-V response to entrainment of the tachycardia from the ventricle confirmed the mechanism as typical AVNRT (slow/fast type) in both patients (Fig. 2).
Fig. 2.
The mother's (A) and her son's electrogram (B) during typical atrioventricular nodal reentrant tachycardia. Following cessation of ventricular entrainment pacing the tachycardia resumes with a V-A-V response and the values of the post-pacing interval minus the tachycardia cycle length were greater than 115 msec in both patients. HISd: HIS distal, HISm: HIS middle, HISd: HIS distal, HA: HIS-atrial interval.
A 7-Fr, 4-mm-tip deflectable ablation catheter (Boston Scientific, San Jose, CA, USA) was positioned at the roof of the CS ostium, and slow pathway was ablated in the inferior region of the Koch's triangle where the local A/V was <0.5. Junctional beats appeared during radiofrequency energy delivery. Thereafter, programmed atrial stimulation demonstrated the elimination of slow pathway conduction, and it did not induce any other supraventricular tachycardias despite isoproterenol infusion. The ablation procedures for both patients were successfully performed without any complications.
Discussion
Atrioventricular nodal reentrant tachycardia is a common arrhythmia that occurs in patients with two functionally distinct conduction pathways through the AV node, referred to as the fast and slow pathways. The slow pathway has a shorter refractory period than the fast pathway. Both pathways are necessary to maintain AVNRT. The common form of AVNRT is typically initiated when an atrial premature beat blocks in the fast pathway, conducts down the slow pathway, and returns by the fast pathway to depolarize the atrium. This is usually cured by radiofrequency catheter ablation of slow pathway.
For WPW syndrome, the second most common cause of supraventricular arrhythmias in the western world and the most common cause in China,3) several responsible mutations in the PRKAG2 gene have been identified in the familial form of WPW syndrome with an autosomal dominant trait of inhereitance.4),5) In contrast, much less is known about a potential hereditary contribution to the development of AVNRT. A familial clustering of AVNRT has been reported in several families, suggesting a hereditary contribution to the development of AVNRT in some patients.6)
In an earlier report, variable familial clusterings were observed in six families. The most common clustering was mother and daughter relationship which was present in three families. In the other three families, AVNRT was present in the father, son and daughter in one family, three siblings (two sisters and a brother) in another family, and two sisters in the other family. However, in one family with three relatives with proven dual AV nodal pathways and AVNRT, all patients/family members also had prolapsed mitral valve on echocardiography. Other than mitral valve prolapse, there were no unique clinical or electrophysiological features that distinguished the familial case from the vast majority of presumable sporadic cases. This is in distinction to familial WPW syndrome, in which a higher frequency of multiple accessory pathways and an increased risk of sudden death have already been well established.1) Another case report involved a familial AVNRT in two siblings of brother and sister who had an autosomal recessive Wolfram syndrome.7)
This is the first familial AVNRT of a mother-son relationship. The patients had no structural cardiac abnormalities on echocardiography. Another interesting feature in both patients was difficulty in the cannulation of a duodecapolar catheter into their CS. The catheters were not fully engaged into the distal CS. Cannulation of the CS during an interventional procedure may be hindered by obstruction due to Thebesian valves. The valves may cover the CS ostium from 0 to 100% and may be semilunar, fenestrated, or band shaped.8) However, it is uncertain whether our case was complicated by obstruction due to Thebesian valves.
It remains unclear whether familial AVNRT is secondary to multifactorial inheritance or is determined by a single gene defect. The findings from previous reports and our cases suggest that, in some family cases, the inheritance pattern of dual AV nodal physiology and AVNRT is likely to be autosomal rather than X-linked. Our cases imply that the familial AVNRT can occur in any kind of relationship.
The limitation of the current study is that a confirmatory gene analysis was not performed. Therefore, we could not ascertain that a genetic mechanism was responsible for our familial AVNRT cases rather than a clustering by chance. However, it is unlikely that the familial clustering of dual AVN physiology and AVNRT is simply a fortuitous event.
We present a familial occurrence of AVNRT that was cured by radiofrequency catheter ablation of slow pathway, which provides evidence for a genetic role in AVNRT.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Vidaillet HJ, Jr, Pressley JC, Henke E, Harrell FE, Jr, German LD. Familial occurrence of accessory atrioventricular pathways (preexcitation syndrome) N Engl J Med. 1987;317:65–69. doi: 10.1056/NEJM198707093170201. [DOI] [PubMed] [Google Scholar]
- 2.Brugada R, Tapscott T, Czernuszewicz GZ, et al. Identification of a genetic locus for familial atrial fibrillation. N Engl J Med. 1997;336:905–911. doi: 10.1056/NEJM199703273361302. [DOI] [PubMed] [Google Scholar]
- 3.Wan Q, Wu N, Fan W, Tang YY, Jin L, Fang Q. Clinical manifestations and prevalence of different types of supraventricular tachycardia among Chinese. Chin Med J (Engl) 1992;105:284–288. [PubMed] [Google Scholar]
- 4.Gollob MH, Green MS, Tang AS, et al. Identification of a gene responsible for familial Wolff-Parkinson-White syndrome. N Engl J Med. 2001;344:1823–1831. doi: 10.1056/NEJM200106143442403. [DOI] [PubMed] [Google Scholar]
- 5.Kang BH, Kim HJ, Namgung J, et al. Wolff-Parkinson-White syndrome treated with radiofrequency ablation in father and his son. Korean Circ J. 2002;32:715–719. [Google Scholar]
- 6.Hayes JJ, Sharma PP, Smith PN, Vidaillet HJ. Familial atrioventricular nodal reentry tachycardia. Pacing Clin Electrophysiol. 2004;27:73–76. doi: 10.1111/j.1540-8159.2004.00388.x. [DOI] [PubMed] [Google Scholar]
- 7.Frisch DR, Kwaku KF, Allocco DJ, Zimetbaum PJ. Atrioventricular nodal reentrant tachycardia in two siblings with Wolfram syndrome. J Cardiovasc Electrophysiol. 2006;17:1029–1031. doi: 10.1111/j.1540-8167.2006.00522.x. [DOI] [PubMed] [Google Scholar]
- 8.Gerber TC, Sheedy PF, Bell MR, et al. Evaluation of the coronary venous system using electron beam computed tomography. Int J Cardiovasc Imaging. 2001;17:65–75. doi: 10.1023/a:1010692103831. [DOI] [PubMed] [Google Scholar]