Abstract
The benefits of computerized physician order entry have been widely recognized, although few institutions have successfully installed these systems. Obstacles to successful implementation are organizational as well as technical. In the spring of 2000, following a 4-year period of planning and customization, a 9-month pilot project, and a 14-month hiatus for year 2000, the Ohio State University Health System extensively implemented physician order entry across inpatient units. Implementation for specialty and community services is targeted for completion in 2002. On implemented units, all orders are processed through the system, with 80 percent being entered by physicians and the rest by nursing or other licensed care providers. The system is deployable across diverse clinical environments, focused on physicians as the primary users, and accepted by clinicians. These are the three criteria by which the authors measured the success of their implementation. They believe that the availability of specialty-specific order sets, the engagement of physician leadership, and a large-scale system implementation were key strategic factors that enabled physician-users to accept a physician order entry system despite significant changes in workflow.
The benefits of physician order entry (POE) and the barriers to its realization have been well documented.1 To date, the barriers appear to dominate. Less than 2 percent of U.S. hospitals have POE completely or partially available and require its use by physicians.2 There is renewed interest in POE as a result of the Institute of Medicine report To Err is Human.3 For example, the Leapfrog Group, a consortium of Fortune 500 companies and other large health care purchasers, selected POE as the basis for one of its first safety standards. Before such initiatives bear fruit, the health care and information technology industries need to develop and share successful implementation practices.
Ohio State University Health Systems (OSUHS) is a large health care system that includes the Ohio State University (OSU) Hospital, a tertiary medical–surgical care facility; the Arthur G. James Cancer Hospital and Richard J. Solove Research Institute, a National Cancer Institute comprehensive cancer center; Dodd Hall, an acute rehabilitation facility; OSU and Harding Behavioral Health, a neuropsychiatric hospital; and OSU Hospitals East, a recently acquired community hospital; and numerous clinics and physician offices. The system is organized along the traditional clinical services of an academic medical center, including medical and surgical subspecialties, obstetrics and gynecology, burn treatment, bone marrow transplant, physical rehabilitation, and psychiatry. In addition, OSUHS is the primary site for education and training for the College of Medicine and Public Health, the School of Allied Health Professions, and the Colleges of Dentistry, Nursing, Optometry, and Pharmacy. This breadth of services, with budgeted revenues in excess of $600 million, classifies OSUHS as a comprehensive integrated health care delivery system. Table 1 ▶provides an overview of OSUHS patient, staff, service, and inpatient POE implementation statistics.
Table 1 .
Statistics for Ohio State University Health Systems (OSUHS) Inpatient Hospitals, 2000
| OSUH | Dodd Hall Rehabilitation | James Cancer Hospital | OSU East | OSU Harding | |
|---|---|---|---|---|---|
| No. of beds: | |||||
| Total | 483 | 60 | 143 | 148 | 59 |
| With POE | 362 | 60 | 143 | 0 | 0 |
| Areas awaiting POE implementation | Women & Infant | None | None | Community hospital | Psychiatric hospital |
| Percentage of POE implemented | 75% | 100% | 100% | 0 | 0 |
| No. of users: | |||||
| Attending physicians, residents and medical students | ←2,057 (across all hospitals)→ | ||||
| Staff | 5,998 | 3,999 | 873 | 695 | 216 |
| No. of inpatients | 42,930 | 28,671 | 6,149 | 6,740 | 1,370 |
At OSUHS, information technology is viewed as a critical element to support clinical and business initiatives and the growth of the health system. Physician order entry is viewed as a logical extension of the OSUHS strategic plan. Implementation strategies adopted to facilitate achievement of our measures of successes include 1) development of a portable and scalable system that could be implemented across diverse and physically distinct clinical environments; 2) identification of the physician as the primary user, and customization of the system to meet physicians' needs; and 3) clinical acceptance. This paper describes the processes that OSUHS used to plan, customize, and implement a POE system that meets these criteria.
Methods
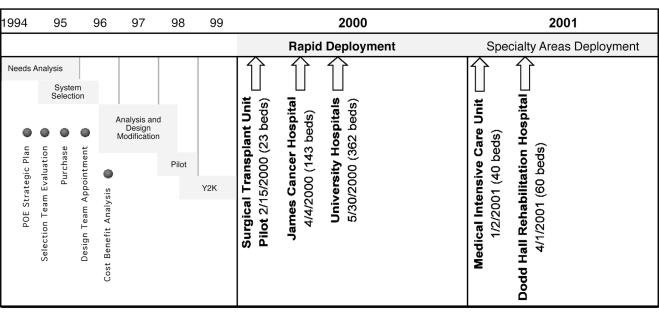
Physician order entry implementation at OSUHS encompassed five phases: needs analysis and clinical system selection, system analysis and design, system modification, initial system implementation, and complete system deployment. The first four phases, from needs analysis through initial system pilot implementation, spanned four years, from 1994 to early 1998 (Figure 1▶). This process was interrupted for 14 months because of the replacement of nearly every clinical and business system, which was necessary for compliance with year 2000 (Y2K) initiatives. The final phase of implementation of POE across the health system began in early 2000 and is targeted for completion in 2002.
Figure 1 .
Time frame for physician order entry implementation.
Needs Analysis
In the early 1990s, a strategic vision for a computerized patient record (CPR) was established at the OSUHS executive level, including the Chief Medical Officer, the Chief Executive Officer and other administrative staff. In addition, the Hospital Board of Trustees and the Medical Staff Administrative Committee approved proceeding with the realization of this vision and provided subsequent funding. Implementation of POE was seen as a key element of the CPR.
In 1995, a selection committee was established and given the charge of recommending the information systems technologies that were needed to support POE. Key physicians, clinical and administrative personnel, and information systems staff served on the committee. Their first step was to analyze the needs of the OSUHS and establish selection criteria for the information system technologies. After conducting clinician surveys and interviews and performing a workflow analysis, the committee assembled a list of POE system requirements that were important to OSUHS clinicians (Table 2▶).
Table 2 .
Physician Order Entry System Requirements
| Can be easily maintained |
| Supports advancing technologies and migration paths |
| Meets all order requirements for the patients' medical record |
| Is stable, and its use is intuitive |
| Provides interfaces to business, clinical, and ancillary systems |
| Supports implementation of best practice and clinical practice guidelines |
| Can be easily expanded for a variety of clinical users and environments |
Following the needs assessment, a recommendation was made to move forward with the selection of a vendor-based solution for physician order communication. The committee recommended a vendor system over an internally developed system because the cost of purchasing and maintaining a vendor-based system was lower than the cost of internally developing a system. In addition, the committee felt it would be easier to stay current with industry standards by using a vendor-based system. Siemens (formerly SMS) PhysicianView provided the framework and tools necessary to develop a product that would meet the needs of the clinically diverse hospitals within the health care system.
Recommendations were also made for future phases of the project. The committee recommended that physicians be the primary users of POE. This proved to be a key decision, and all subsequent decisions were driven by this premise and paradigm.
Design and Analysis
Once a system selection was made, design teams were quickly established. Various clinical personnel were assigned to the project full time. These reallocated staff consisted of a laboratory technician, a pharmacist, a nurse, a respiratory therapist, and a radiology technician. These persons combined with traditional information system personnel to form the core of the POE development team, reporting up through the information systems department.
Hospital administration realized the importance of having physicians take an active and meaningful role in system design.4 To this end, a formalized physician consultant team was established. The ten physician participants were required to sign a contract that outlined their responsibilities (Appendix A). The physicians were empowered by medical and administrative leadership to approve system design and operational policy relative to POE implementation. Clinical expertise included emergency medicine, oncology, gynecology, pulmonary, cardiology, surgical oncology, surgical transplant, pathology, radiology, and general medicine. Representation included both junior and senior attending staff and fellows. Since the commitment was extensive, the physicians' departments were paid release-time fees to compensate for the time spent outside other clinical and administrative responsibilities.
The physician consultant team provided the vehicle for validation of design elements, policies, implementation plans, and training methodologies. An important milestone of POE design was approval of a working prototype by the physician consultant team. Additional validation for the working model was sought from other OSU physicians. Of particular importance was the involvement of physician house staff, since they enter most of the orders at an academic medical center. The end result of this process was a system designed and validated by a wide group of physician users. Physician involvement at this phase seems to have had a positive effect on physician satisfaction and system success following implementation.
The general philosophy of the design team was to create a system that served the needs of the various clinical specialties as well as those of the ancillary areas. Therefore, consistency was essential for both system design and workflow modification. Efforts to reach consensus were made to standardize processes and practices during all phases of the design of automated ordering. With strong backing from physician leadership and administration, numerous efforts to standardize practices and policies across the enterprise became an integral part of the POE project.
To ensure patient safety and prevent user confusion, we decided not to permit both manual and electronic ordering for a single unit or patient. We decided that, if electronic entry was the exclusive means for order processing, physicians and other licensed care providers would be less likely to revert to manual ordering. This key decision was an important rationale for large and rapid system deployment.
Order sets were necessary to facilitate physician utilization and promote clinical standardization of care. We divided our order sets into two major types. The first type consisted of orders that were generally included for a defined patient condition or diagnosis. The second type consisted of a selection of pre-defined orders (pick lists). Order sets were further categorized and named by phase of care, such as admission, pre-operative, postoperative, post-transfer, post-procedure, comorbidities, and chemotherapy. The pick lists commonly included medication groups as well as some selected laboratory tests. We developed a process for the clinicians and technical staff to work together to develop the order set content. Disease-specific order sets were an automated derivative of evidenced-based clinical practice guidelines that were reviewed and approved by clinicians. Each order set was reviewed for cost effectiveness, best practice, and order clarity. Physician-specific order sets were not permitted.
The challenges associated with this approach included significant time commitment and support by expert staff. The responsibility of developing the order sets was clearly vested with the clinical leaders. Once the content of the order sets was established, the technical staff of the information technology department achieved the translation of the content into a computerized order entry system format. A manually written dietary order for a postsurgical patient, for instance, might be “nothing by mouth (NPO) for dinner, advance to clear liquids, then regular diet as tolerated.” This order needed to be translated with respect to time if it was to truly become an order that could be electronically communicated to other ancillary care providers. This translation was done by creating three separate orders with different start and stop times. Without the time element, dietary staff would not know when to begin a regular diet.
System Adaptation and Customization
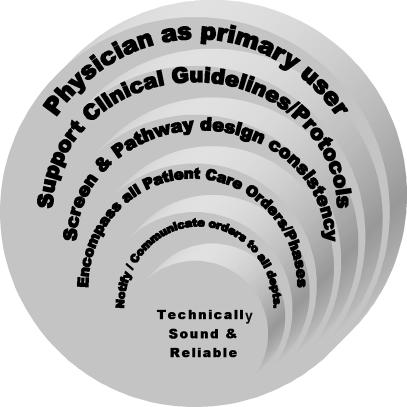
Although the vendor-based application provided a foundation architecture, significant customization and adaptation were required to meet the needs of the physician-user. The vendor's architecture enabled the information systems department to integrate the design specifications recommended by the physician consultant team. Using rapid application development principles, prototypes were developed in the system prior to final design approval by the physicians. A prerequisite for approval of system design was an alpha-level online prototype. Physician consultant team review and approval were required for every order flow and screen design. Pathway design was partitioned into logical groupings to facilitate review, as described in Figure 2▶. Foundation order elements, such as standardized frequencies, order duration, census displays, patient information, and allergy history, were approved first. This was followed by the development of order screens and order flow.
Figure 2 .
Methodology for system customization and implementation.
Maintenance of user interface consistency was an ongoing focus of POE development. Once the general layouts and order flows were established, department-specific designs were addressed. All department order screens needed to comply with the generic screen template. For the unique needs of specialized departments, portions of the screen were adjusted. For example, in Respiratory Therapy, the ventilator management screen required many unique order elements, although their positioning and functionality remained consistent with more general order screens.
After completion of the POE prototype, we were positioned to incorporate decision support tools, such as order defaults, best-practice order sets, and clinical rules. These elements of decision support were added to the prototype in a step-wise fashion, beginning with clinically determined areas of focus. Patient data, such as admission diagnoses, allergy history, height/weight, and selected laboratory results were added to provide alerts and reminders to help physicians in ordering. To meet OSUHS needs, the vendor product was modified to include weight-based chemotherapy order dosing, limited ordering of nonformulary medications, drug interaction checking, and duplicate order checking. Best ordering practices, such as default dose, frequency, and duration, were extensively incorporated into pharmacy ordering. These patient-safety-focused strategies supported the physician as the primary user of POE and were felt to positively influence physician acceptance. Use of decision support tools to provide more discrete clinical results and medication dose checking is being expanded as a strategy to further reduce medication errors.
Implementation
As we prepared for pilot use of the system, we decided that all orders for the pilot patient population would be placed electronically. For this reason, we made the decision not to introduce POE piecemeal but to wait until it could be introduced with integration in all ancillary areas. Instead of implementation on a single patient-care unit, we chose to implement an entire hospital. The James Cancer Hospital (143 beds), including the bone marrow transplant unit, implemented POE on Apr 4, 2000. The University Hospital (483 beds), including surgical and medical intensive care units but excluding women and infant units, implemented POE on May 30, 2000. The Dodd Hall Rehabilitation Hospital (60 beds) implemented POE on Apr 1, 2001. This methodology was different from that of other institutions. At one institution, for instance, the installation began with basic administrative functions, then radiology and dietary; a year later, pharmacy order entry followed.5
An initial pilot study to validate POE system functionality ran from Feb 1, 1998, to Oct 29, 1998 (see Figure 1▶). During 1999, information systems staff resources were assigned to complete year 2000 compliance conversion and complete POE design specifications. As shown in Figure 1, a second pilot implementation on Feb 15, 2000, preceded the subsequent full deployment of POE. The medical intensive care unit attempted implementation with the OSU Hospitals Live. Because of needs related to support, order set development, and workflow redesign, its full implementation was rescheduled for Jan 2, 2001. In areas of POE implementation, the computerized system has replaced the written record completely (dual ordering process is nonexistent).
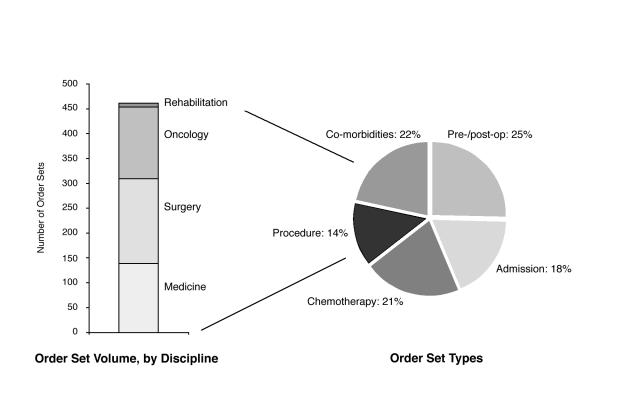
Each physician specialty identified the order sets they would need to care for the majority of patients admitted to their clinical area. Until the necessary order sets were created, it was determined that a POE live date could not be established. Prior to implementation, more than 450 order sets were approved and available for physician use. The bar graph in Figure 3 ▶shows the volume and distribution of order sets by specialty. The pie chart shows the percentage of order set types across all specialties.
Figure 3 .
Order set availability.
An implementation as complex as POE requires extensive support and training to achieve user acceptance. A formalized training program for all clinicians and physicians preceded implementation by 2 to 4 weeks. In addition, extensive on-site training occurred during the implementation period. We quickly realized that the traditional help-desk phone call was inadequate for user support. We needed around-the-clock support dedicated to POE, which could be immediately dispatched to the user when a problem arose. Beginning with the live date and continuing for 1 month, information system development staff provided 24-hour support. In addition, key clinicians were released from their clinical duties to focus on issue resolution. After the live date, hospital administration supported the implementation by creating permanent POE support positions with an on-site schedule of 6 a.m. to 11 p.m. 7 days a week. To fill these positions, we hired clinical staff and gave them extensive training in the use of the POE system. They also took classes in conflict resolution. The new support staff, known as “red coats” for their distinctive tunics, have been well received and have played a key role in system success.
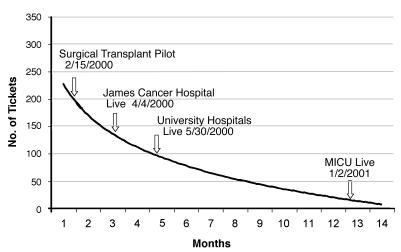
The normalized user request log shown in Figure 4 ▶indicates a decline in user modification and enhancement requests since implementation. System requests and feedback were solicited from users in a variety of ways. These included help-desk phone calls, conversation with red coats, e-mail, intranet forms, communication with information system staff through the POE application, and multiple meetings. Requests ranged from order set modifications and correction of system bugs to changes in order flow. The majority of comments were requests to fine-tune the system to adapt it to specific clinical environments. None of the requests required significant changes to the system.
Figure 4 .
User requests for enhancements and modifications.
Status
Physician order entry is deployed in all the clinical areas of the James Cancer Hospital, including the bone marrow transplant intensive care unit. At the OSU Hospitals and Dodd Hall Acute Rehabilitation Facility, POE is deployed in all clinical areas except the maternal-fetal area. Implementation for this area is currently in progress. Plans are also under way to extend implementation of POE into the community and outpatient settings (see Figure 1▶).
In the areas of deployment, 100 percent of patient care orders are entered through the computerized system. Table 3 ▶shows various breakdowns of these computerized orders. Of the approximately 6,000 orders entered daily, physicians consistently enter 80 percent. The remaining orders are entered by clinical care providers, including nurses, pharmacists, physician assistants, and medical students. These orders are subsequently countersigned electronically by a physician.
Table 3 .
System Availability and Average Daily Volume of Patient Orders
| No. | % | |
|---|---|---|
| Orders entered by physician | 5,233 | 82.03 |
| Orders requiring physician's countersignature: | 1,147 | 17.97 |
| Traditional unit staff | 1,053 | 16.50 |
| Physician assistant | 24 | 0.37 |
| Medical student | 63 | 0.99 |
| Types of order: | ||
| Pharmacy | 2,129 | 33.37 |
| Laboratory | 1,689 | 26.47 |
| Nursing | 1,441 | 22.58 |
| Radiology | 243 | 3.81 |
| Physician and ancillary consultant | 154 | 2.41 |
Notes: The figures reflect physician order entry use in the Ohio State University Health System (OSUHS) on May 6, 2000. On that day, the total number of orders was 6,380, and the average system availability was 99.7%. Summary figures for hospitals in the system were as follows: James—15 admissions, 14 order sets; University and Dodd—93 admissions, 60 order sets; OSUHS (total)—108 admissions, 74 order sets.
Physician order entry has been live for more than a year through much of the institution, as shown in Figure 1▶. With the exception of the medical intensive care unit, once an area has fully implemented POE, there has been no return to manual order entry. Our maternal-fetal area is scheduled for POE implementation in early 2002. The remaining community areas are actively petitioning to become the next in line for POE implementation.
Discussion
Physician order entry systems have been touted as one of the primary vehicles to enhance patient safety and to control the rising costs of managed care.3 Physician order entry is still largely a vision for all but a few pioneering institutions. The present turbulence in the health care industry has forced freestanding hospitals to merge with other institutions to streamline the business of health care.
The formidable task facing these new, integrated health care delivery systems is the challenge of developing clinical systems to meet the needs of diverse specialties and environments. The OSUHS, an academic integrated health system, accomplished this by successfully implementing a POE system that is integrated with its comprehensive business and clinical systems and serves the needs of the current health care system. Our three measurement criteria for a successful POE implementation included broad system deployment across diverse clinical environments, physicians as primary users, and clinician acceptance of the system.
Several key factors and methods influenced our success. These included continuous executive support and physician empowerment, an effective implementation team, a consistent user-friendly interface, ongoing user support, breadth of order sets, and elimination of dual ordering processes.
Identification of the physician as the primary user of POE has enhanced our ability to introduce clinical decision support tools to address institutional goals of quality, efficiency, and cost. Order set development was one area in which we were able to influence clinical decisions.
Throughout implementation, some clinicians wanted to return to manual order entry. The resolve of the clinical leaders and administrative support staff were crucial to the success of POE implementation, particularly the avoidance of “user revolt” and a subsequent return to paper ordering. Physician acceptance and ongoing use of the POE system were measured in terms of length of uptime since implementation and volume of enhancement requests.
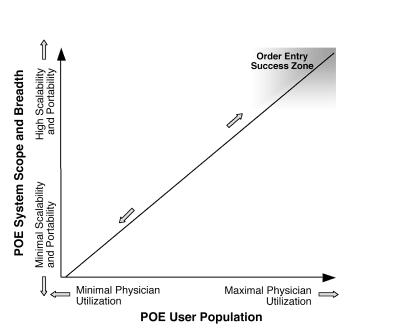
The large-scale implementation enabled us to meet the three criteria necessary for a successful POE implementation, as shown in Figure 5▶. Any other approach might have limited the success in terms of any one of these criteria. The methods applied throughout our POE implementation were important to ensure the potential for large-scale institutional impact. Partially meeting any of the three criteria would have resulted in an installation falling short of success, which may explain the relatively small number of large-scale POE implementations.
Figure 5 .
Order entry success zone.
As described, our overall implementation timeline was lengthy. The first two years of our implementation were focused on system programming to meet comprehensive physician workflow requirements. This time was necessary to develop a product that was acceptable for physician use. As POE remains a national focus, entities like the Institute of Medicine and the Leapfrog Group will influence hospital and vendor knowledge and expertise in this area. This increase in knowledge, coupled with improved technologies and vendor platforms, should enable other institutions to implement POE in a much shorter time.
Acknowledgments
The authors thank Kamilla Sigafoos, Judy Gilliam, Suzanne Martin, Joyce Miller Evans, and the OSUHS Information Systems staff for the development and support of the POE system. They also thank Liz Marshall for editorial contributions.
Appendix
Physician Consultant Information Systems Contract
_____________________________ has agreed to act as a physician consultant to the Department of Information Systems. Their role consists of the following:
Promotion
Promotes and provides leadership of medical staff participation in various groups and task forces to assist in the design, review, and evaluation of the clinical information systems, hardware, and communication components at OSUHS.
Represents medical staff in medical center discussions relating to the application and use of computerization in clinical practice.
Policy
Participates in the development of and coordinates policy recommendations required for the implementation and augmentation of the clinical information systems.
Project Management
Provides consultation and input to the clinical departments on the responsibilities and use of the Clinical Information systems in patient care, assessment, teaching, and research at OSUHS.
Provides assistance in establishing opportunities, priorities, specifications, and policies for the use of the Clinical Information Systems by non-hospital based physicians and physician groups, individual groups, practices, and individual physicians.
Supports individual departmental and house staff systems committees established to provide communication and guidance concerning the use of the Physician Order Entry System. In addition, committee structures will be used to coordinate recommendations for future clinical system modifications and developments.
Provides physician based interface with other medical center computer system developments to increase efficiency, limit duplication and costs, and assure the secure and appropriate use of clinical data.
Advises the Assistant VP Health Services, Medical Director and Associate Dean for Clinical Affairs on physician issues concerning computer applications in patient care, management, and evaluation.
Participates as a member of the Clinical Information System project management teams.
Acts a chairperson or member for the POE Implementation committees.
System Development
Assists in the design, development, review, implementation, and evaluation of all clinical applications.
Assists OSUHS in establishing priorities and coordinating efforts for modifications and additions to the Clinical Information Systems for physicians, including current and future developments such as bedside systems, video functionality, voice interface, office practice access, electronic medical record, and others.
Is responsible for providing long range planning input to the information systems steering committee in the area of Clinical Information Systems.
Training
Assists in the development, delivery, and evaluation of training materials for physicians in order to facilitate a smooth and successful implementation of the Clinical Information Systems and subsequent modifications.
Provides the development and coordination for the annual orientation and training program for new physicians in the use of the Clinical Applications.
The appointment is temporary and may be terminated by either party at any time.
I have read to above and understand the role and responsibilities of the Physician Consultant and agree to serve 8 hours per week.
Physician Consultant________________ Date________ Chief Medical Officer____________________________
Reprint requests: Dr. Hagop S. Mekhjian, MD, Assoc. Vice President for Health Sciences, Chief Medical Officer, Vice Dean for Clinical Affairs, 130 Doan Hall, 410 West 10th Avenue, Columbus, OH 43210; e-mail: <Mekhjian-1@medctr.osu.edu>.
References
- 1.Sittig, DF, Stead, WW. Computer-based physician order entry: the state of the art. J Am Med Inform Assoc. 1994;1:108–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ash JS, Gorman PN, Hersh WR. Physician order entry in U.S. hospitals. Proc AMIA Annu Symp. 1998:235–9. [PMC free article] [PubMed]
- 3.Kohn LT, Corrigan JM, Donaldson MS (eds), for the Institute of Medicine Committee on Quality of Healthcare in America. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press, 2000. [PubMed]
- 4.Ashmos DP, Duchon D, McDaniel RR. Physicians and decisions: a simple rule for increasing connections in hospitals. Health Care Manage Rev. 2000;25(1),109–15. [DOI] [PubMed] [Google Scholar]
- 5.McDonald CJ, Overhage JM, Abernathy G, et al. The Regenstrief Medical Record System: cross-institutional usage, note writing, and mosaic/html. Proc Annu Symp Comput Appl Med Care. 1995:1029.