Abstract
Background:
The presence of bone metastases in patients with metastatic renal cell carcinoma treated with oral tyrosine kinase inhibitors (TKIs) is associated with poorer outcome as compared with patients without bone involvement. Concomitant bisphosphonates could probably improve outcomes but also induce osteonecrosis of the jaw (ONJ).
Methods:
Retrospective study on all the renal cell carcinoma patients with bone metastases treated with sunitinib or sorafenib between November 2005 and June 2012 at the University Hospitals Leuven and AZ Groeninge in Kortrijk.
Results:
Seventy-six patients were included in the outcome analysis: 49 treated with concomitant bisphosphonates, 27 with TKI alone. Both groups were well balanced in terms of prognostic and predictive markers. Response rate (38% vs 16% partial responses, P=0.028), median progression-free survival (7.0 vs 4.0 months, P=0.0011) and median overall survival (17.0 vs 7.0 months, P=0.022) were significantly better in patients receiving bisphosphonates. The incidence of ONJ was 10% in patients treated with TKI and bisphosphonates.
Conclusion:
Concomitant use of bisphosphonates and TKI in renal cell carcinoma patients with bone involvement probably improves treatment efficacy, to be confirmed by prospective studies, but is associated with a high incidence of ONJ.
Keywords: bisphosphonates, bone metastases, renal cell carcinoma, osteonecrosis of the jaw, outcome, targeted therapy
Renal cell carcinoma (RCC) accounts for about 2% of all the cancers worldwide (Parkin et al, 2005). At initial diagnosis, up to one-third of patients present with metastatic disease and 40% of primary non-metastatic patients, who underwent a nephrectomy with curative intent, will ultimately relapse or develop metastases (Lam et al, 2005; Jemal et al, 2006; US NIH, 2006). New therapies targeting the vascular endothelial growth factor (VEGF) pathway, such as the tyrosine kinase inhibitors (TKIs) sunitinib, sorafenib, pazopanib and axitinib, and the monoclonal antibody bevacizumab, or the mammalian target of rapamycin pathway, such as everolimus and temsirolimus, (Escudier et al, 2007a, 2007b; Hudes et al, 2007; Motzer et al, 2007; Motzer et al, 2008) have recently replaced cytokines as the first-line and second-line treatment of advanced or metastatic RCC (mRCC).
About one mRCC patient out of three presents – at some point in the course of disease – with bone metastases, mainly osteolytic and frequently leading to skeletal-related events (SREs) such as pain, pathologic fractures, hypercalcemia and the need for antalgic radiation therapy or surgery. There is growing evidence that bone metastases in mRCC are adversely linked to outcome. In a retrospective analysis on 223 clear cell mRCC patients, we observed a lower response rate (RR) in patients with bone metastases (35% vs 55% P=0.006), a lower median progression-free survival (PFS) (8.2 vs 19.1 months; P<0.0001) and a lower median overall survival (OS) (19.5 vs 38.5 months; P<0.0001) as compared with patients without bone metastases. On multivariate analysis, bone metastasis was the major independent variable associated with a poorer PFS and OS (Beuselinck et al, 2011). Patil et al (2011), when validating the Memorial Sloan-Kettering Cancer Center criteria for OS (time from initial diagnosis to start of systemic therapy, baseline lactate dehydrogenase, baseline corrected calcium, low-baseline haemoglobin and low Eastern Cooperative Oncology Group performance status (Motzer et al, 1999, 2004)) in the era of targeted therapy, added the presence of bone metastases as a new independent prognostic factor for OS (HR 1.706, P<0.001), with a borderline hazard ratio (HR) for PFS (HR 1.263, P=0.075). Accordingly, in a retrospective series of 58 RCC patients treated with sorafenib as the first-line systemic therapy, Riechelmann et al (2008) found a lower median PFS in patients with bone metastases (4.7 vs 11.2 months; P=0.002). Moreover, in the pivotal trial of everolimus conducted by Motzer et al (2010) in anti-VEGF-TKI refractory RCC, the absence of bone metastases was independently linked to better outcome with a HR of 2.30 for PFS (P<0.001) and 1.64 for OS (P<0.001).
Concomitant administration of bone resorption inhibitors could have a favourable impact on outcome, but the possible benefits of bisphosphonates must outweigh the enhanced risk for osteonecrosis of the jaw (ONJ). Although ONJ has rarely been reported in patients with RCC treated with bisphosphonates, it has been recently suggested that the combination of bisphosphonates and anti-VEGF-TKIs may increase the risk for ONJ. Several case reports were published, and in December 2010 the European Medicines Agency issued safety warnings about ONJ risk in patients receiving sunitinib or bevacizumab. Larger series assessing the true incidence of ONJ in RCC patients treated with bisphosphonates and TKIs are lacking. Therefore, we studied the benefits and risks of concomitant bisphosphonates in RCC patients treated with the TKIs sunitinib and sorafenib.
Patients and methods
We retrospectively reviewed the records of all mRCC patients with bone metastases, who started first-line TKIs between November 2005 and May 2012 at the University Hospitals Leuven, Leuven, Belgium and General Hospital Groeninge, Kortrijk, Belgium. The primary objectives were to assess the impact of concomitant bisphosphonates on PFS under the first-line treatment with the TKIs sunitinib and sorafenib, and to quantify the incidence of ONJ. PFS was defined as the lapse of time between the start of first-line targeted therapy and progressive disease under this first-line therapy or death. The secondary objective was to study the impact of treatment with bisphosphonates on OS in such patients. OS was defined as the lapse of time between the start of first-line targeted therapy and death of any cause.
During treatment, all patients underwent chest and abdominal CT-scan every 2–3 months as part of clinical routine practice. Bone metastases were detected by radiographs, CT-scan, MRI and/or bone scintigraphy. Previous immunotherapy or chemotherapy did not exclude cases from this analysis. Patients who underwent complete resection of a single-bone lesion before the start of a TKI were excluded. Patients with bone only disease were excluded because of the difficulty of assess response. Patients who stopped TKIs before completing a first 4 weeks of TKI treatment for toxicity reasons were also excluded. The decision whether to start bisphosphonates was at the discretion of the treating physician.
Once administered, bisphosphonates will remain imbedded in the bone during several years and as such capable of influencing osteoclast activity during a long period. Therefore, patients with concomitant bisphosphonates were defined as patients (A) who started these drugs together with TKIs or (B) who received them before and until the beginning or during the treatment with first-line TKIs. Patients without concomitant bisphosphonates were defined as individuals who did not receive any bisphosphonates before or during the first-line targeted therapy.
Response was defined according to the Response Criteria in Solid Tumours 1.0. Progression-free survival and OS distributions were estimated using the Kaplan–Meier product-limit method and survival curves were compared with the Mantel-Cox log-rank test. Any prognostic parameter related to PFS and OS in univariate analysis (by Kaplan–Meier with a P-value <0.2) was included in the multivariate model (Cox regression). First-line sunitinib vs sorafenib use was also included in the multivariate analysis. A P-value <0.05 was considered statistically significant in the multivariate model. χ2-test was used for the comparison between percentages. Statistical analyses were conducted using GraphPad Prism 5 (GraphPad Software, La Jolla, CA, USA) and XLSTAT software (Addinsoft, Paris, France).
Results
We collected data on 77 mRCC patients with bone metastases, who started TKI treatment between November 2005 and May 2012, and who met the inclusion criteria of this study. All these patients were treated in common clinical practice and not included in clinical trials. One patient was excluded from the efficacy analysis because bisphosphonates were started several months after the start of sunitinib and then administered concomitantly. The characteristics of the 76 included patients, 27 treated with TKIs alone and 49 with TKIs and bisphosphonates, are given in Table 1. All the previously described characteristics linked to PFS and OS were well balanced between both the groups. There were two concerns in our baseline patient characteristics. First, although not at a significant level, the interval between the diagnosis of metastases and the start of TKIs was longer in patients with concomitant therapy (8.5 vs 5.0 months; P=0.23). The longer this interval, the higher the probability that bisphosphonates were started at a certain moment during this interval and thus the higher the possibility of inclusion of slow evolving tumours in the concomitant arm. In order to exclude that this fact would influence the final outcome, an additional parameter ‘time from diagnosis metastases to start TKIs ⩽6 months or >6 months’ was analysed in univariate analysis for PFS and OS, and eventually included in the multivariate analysis for PFS.
Table 1. Patient characteristics.
| Patient characteristics at initial diagnosis | Total | Only TKI | Concomitant TKI and bisphosphonates | χ2 or log-rank |
|---|---|---|---|---|
| Number of patients | 76 | 27 | 49 | |
| Mean age (years) | 59 | 61 | 58 | |
| Male | 71% (54/76) | 70% (19/27) | 71% (35/49) | |
| No nephrectomy | 9% (7/76) | 11% (3/27) | 8% (4/49) | P=0.67 |
| M1 (synchronous metastases) | 55% (42/76) | 48% (13/27) | 59% (29/49) | P=0.35 |
| Interval between diagnosis initial tumour and diagnosis metastases (median) | 5.0 months | 0.0 months | P=0.49 | |
| Interval between diagnosis metastases and start TKI (median) | 5.0 months | 8.5 months | P=0.23 | |
| Interval between diagnosis initial tumour and start TKI (median) | 23.0 months | 17.0 months | P=0.42 | |
| Fuhrman | ||||
| Grade 1–3 | 58% (42/72) | 65% (17/26) | 54% (25/46) | P=0.36 |
| Grade 4 | 42% (30/72) | 35% (9/26) | 46% (21/46) | |
| Histology | ||||
| Clear cell | 88% (67/76) | 85% (23/27) | 90% (44/49) | |
| Non-clear cell | 12% (9/76) | 15% (4/27) | 10% (5/49) | |
| Sarcomatoid features | 20% (15/76) | 11% (3/27) | 24% (12/49) | P=0.16 |
| Patient characteristics at start of TKI | ||||
| ECOG PS>0 | 58% (44/76) | 67% (18/27) | 53% (26/49) | P=0.34 |
| Neutrophils >4500 mm−3 | 58% (44/76) | 52% (14/27) | 61% (30/49) | P=0.43 |
| Platelets >400 000 mm−3 | 17% (13/76) | 15% (4/27) | 18% (9/49) | |
| Haemoglobin <11.5 g dl−1 (women) or <13 g dl−1 (men) | 66% (51/76) | 59% (16/27) | 71% (35/49) | P=0.28 |
| LDH>1.5x ULN | 5% (4/76) | 4% (1/27) | 6% (3/49) | |
| Corrected calcium>10 mg dl−1 | 13% (10/76) | 7% (2/27) | 16% (8/49) | P=0.27 |
| Interval between nephrectomy and systemic treatment <12 months | 54% (41/76) | 41% (11/27) | 61% (30/49) | P=0.086 |
| Immunotherapy before targeted therapy | 43% (33/76) | 44% (12/27) | 43% (21/49) | |
| Site of metastasis | ||||
| Lung | 79% (60/76) | 85% (23/27) | 76% (37/49) | P=0.32 |
| Liver | 21% (16/76) | 30% (8/27) | 16% (8/49) | P=0.17 |
| Bone | 100% (76/76) | 100% (27/27) | 100% (49/49) | |
| Brain | 9% (7/76) | 4% (1/27) | 12% (6/49) | P=0.22 |
| Mean number of sites of metastases | 3.64 | 4.07 | 3.39 | |
| Mean number of bone metastases | 3.20 | 2.29 | 4.04 | |
| Targeted treatment | ||||
| Sunitinib | 75% (57/76) | 63% (17/27) | 82% (40/49) | P=0.072 |
| Sorafenib | 25% (19/76) | 37% (10/27) | 18% (9/49) | |
| MSKCC prognosis | ||||
| Favourable | 8% (6/76) | 7% (2/27) | 8% (4/49) | |
| Intermediate | 57% (43/76) | 59% (16/27) | 55% (27/49) | |
| Poor | 36% (27/76) | 33% (9/27) | 37% (18/49) | |
Abbreviations: ECOG PS=Eastern Cooperative Oncology Group performance status; LDH=lactate dehydrogenase; MSKCC=Memorial Sloan-Kettering Cancer Center; TKI=tyrosine kinase inhibitor; ULN=upper limit of normal.
Note: When differences in frequency of markers were found, a statistical comparison was performed with a χ2-test for percentages or a log-rank for comparison of time-to-events.
Note: The Memorial Sloan-Kettering Cancer Center criteria stratify patients receiving immunotherapy into three risk groups (favourable, intermediate and poor prognosis) according to five factors adversely associated with OS: time from initial diagnosis to start of systemic therapy, elevated baseline lactate dehydrogenase (LDH) and corrected calcium, low-baseline haemoglobin, and low Eastern Cooperative Oncology Group performance status.
Secondly, compared with the concomitant group, in the TKI alone group, more patients received sorafenib. Nevertheless, in both univariate and multivariate analysis, in our series, the outcomes on sorafenib were the same as the outcomes on sunitinib.
Zoledronic acid (ZA) was the most commonly used bisphosphonate, but one patient received pamidronate and one ibandronate. In most patients bisphosphonates were administered at the usual recommended dose every 4 weeks and were continued after progression on first-line therapy. Bisphosphonates were stopped in case of occurrence of ONJ, renal insufficiency and in some cases when the clinician estimated that the patient did not benefit anymore from their administration. Among the 27 patients without concomitant bisphosphonates during their first-line TKI, two patients received bisphosphonates during their second-line therapy and five in the palliative setting for hypercalcemia (13 administrations in total, range 1–4 per patient). The global incidence of SREs was 78%: 72% of patients required radiation therapy, 39% required bone surgery, 20% had spinal cord compression, 21% presented with pathologic fractures and 11% with hypercalcemia.
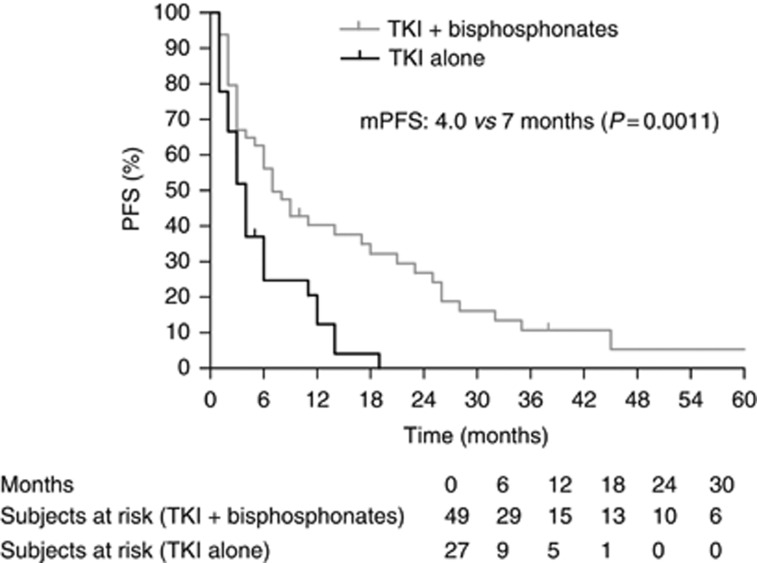
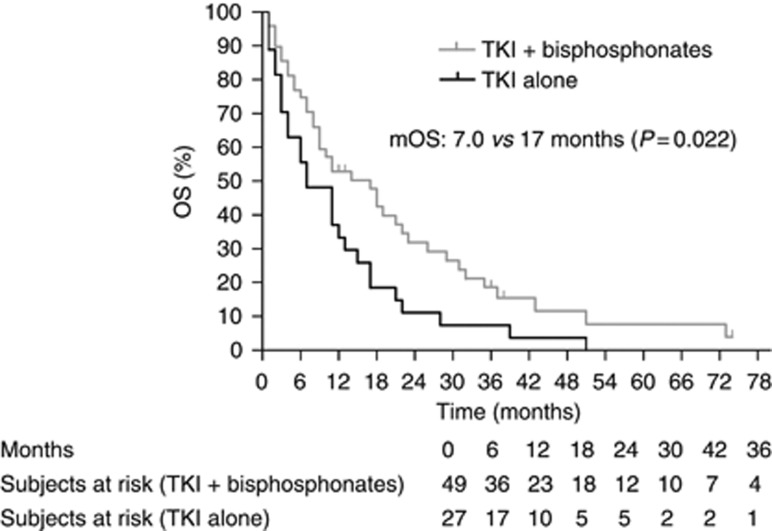
Global median PFS was 6.0 months and global median OS 11.0 months. As shown in Table 2 and Figures 1 and 2, RR (38% vs 16% of partial responses), median PFS (7.0 vs 4.0 months) and median OS (17.0 vs 7.0 months) were significantly better in patients receiving bisphosphonates.
Table 2. Outcome analysis.
| Results | Total | Only TKI | Concomitant TKI and bisphosphonates | |
|---|---|---|---|---|
| Median PFS (months) | 6 | 4 | 7 | P=0.0011a HR for progression 0.3528 95% CI of ratio 0.1889 to 0.6588 |
| Progression reached | 91% (69/76) | 100% (27/27) | 86% (42/49) | P=0.039b |
| Median OS (months) | 11 | 7 | 17 | P=0.022a HR for survival 0.5229 95% CI of ratio 0.3004 to 0.9101 |
| Death reached | 87% (66/76) | 100% (27/27) | 80% (39/49) | P=0.0118b |
| Partial response | 31% (22/72) | 16% (4/25) | 38% (18/47) | P=0.028c Relative risk: 1.505 95% CI of relative risk 1.082 to 2.094 |
| Stable disease | 38% (27/72) | 40% (10/25) | 36% (17/47) | |
| Progressive disease | 32% (24/72) | 44% (12/25) | 26% (12/47) | |
| Proportion of patients who received second-line targeted therapy after progression on first line | 42% (29/69) | 37% (10/27) | 46% (19/41) |
Abbreviations: CI=confidence interval; HR=hazard ratio; OS=overall survival; PFS, progression-free survival; TKI=tyrosine kinase inhibitor
Kaplan–Meier analysis and log-rank for comparison of curves.
Fisher exact test.
Fisher exact test partial response vs stable disease vs progressive disease.
Figure 1.
PFS according to concomitant bisphosphonate use.
Figure 2.
OS according to concomitant bisphosphonates use.
Table 3 gives an overview of all previously described prognostic criteria assessed in univariate analysis. On multivariate analysis (Table 4), concomitant bisphosphonate administration was independently linked to PFS (P<0.0001) and OS (P=0.014). Baseline platelet count and baseline neutrophil count were also associated with median PFS. Non-clear cell histology and baseline platelet count were linked to median OS.
Table 3. The impact of formerly described parameters linked to outcome in our series.
| Parameter (number of patients) | Median PFS (months) | P | Median OS (months) | P |
|---|---|---|---|---|
| Neutrophils >4500 mm−3 (47) | 4 | 0.018 | 9 | 0.05 |
| Neutrophils ⩽4500 mm−3 (29) | 9 | 14 | ||
| Platelets >400 000 mm−3 (13) | 2 | 0.0001 | 5 | 0.0003 |
| Platelets ⩽400 000 mm−3 (63) | 7 | 14 | ||
| ECOG PS>0 (48) | 3 | 0.27 | 8 | 0.16 |
| ECOG PS 0 (28) | 11 | 17 | ||
| LDH >1.5ULN (4) | 1.5 | <0.0001 | 2 | 0.0003 |
| LDH ⩽1.5ULN (72) | 6 | 14 | ||
| Hb low (<11.5 g dl−1 (women) or <13 g dl−1 (men)) (51) | 6 | 0.64 | 11 | 0.62 |
| Hb normal (25) | 7 | 13 | ||
| Corrected Calcium >10 mg dl−1 (10) | 5 | 0.60 | 13.5 | 0.57 |
| Corrected Calcium ⩽10 mg dl−1 (66) | 6 | 11 | ||
| Time from nephrectomy to systemic treatment <12 months (41) | 4 | 0.92 | 11 | 0.92 |
| Time from nephrectomy to systemic treatment >12 months (35) | 6 | 11 | ||
| Time from diagnosis metastases to start TKIs ⩽6 months (35) | 3 | 0.20 | 8 | 0.46 |
| Time from diagnosis metastases to start TKIs >6 months (41) | 8 | 17 | ||
| Liver metastases (16) | 3 | 0.074 | 7 | 0.019 |
| No liver metastases (60) | 6 | 13 | ||
| No nephrectomy (8) | 1.5 | 0.019 | 11 | 0.15 |
| Nephrectomy (68) | 6 | 11 | ||
| Sorafenib (19) | 6 | 0.70 | 10 | 0.46 |
| Sunitinib (57) | 6 | 11 | ||
| Non-clear cell (9) | 3 | 0.28 | 7 | 0.13 |
| Clear cell (67) | 6 | 12 | ||
| Sarcomatoid features (15) | 3 | 0.21 | 7 | 0.29 |
| No sarcomatoid features (61) | 6 | 12 |
Abbreviations: ECOG PS=Eastern Cooperative Oncology Group performance status; LDH=lactate dehydrogenase; OS=overall survival; PFS=progression-free survival; TKI=tyrosine kinase inhibitor.
Table 4. Multivariate analysis.
| P -value | Hazard ratio | 95% CI | |
|---|---|---|---|
| For PFS | |||
| Concomitant bisphosphonates vs not | <0.0001 | 3.226 | 1.749–5.950 |
| Baseline platelets <400 000 mm−3 vs >400 000 mm−3 | 0.001 | 3.381 | 1.620–7.055 |
| Baseline neutrophils >4500 mm−3 vs <4500 mm−3 | 0.027 | 0.512 | 0.284–0.925 |
| For OS | |||
| Concomitant bisphosphonates vs not | 0.014 | 1.977 | 1.147–3.408 |
| Clear cell histology vs other histology | 0.040 | 2.431 | 1.041–5.681 |
| Baseline platelets <400 000 mm−3vs >400 000 mm−3 | 0.047 | 2.340 | 1.011–5.415 |
| Baseline ECOG PS >0 vs 0 | 0.065 | 0.589 | 0.336–1.034 |
Abbreviations: ECOG PS=Eastern Cooperative Oncology Group performance status; OS=overall survival; PFS=progression-free survival.
The factors that were included for multivariate analysis for PFS were: baseline neutrophil count; baseline platelet count; time from diagnosis metastases to start TKIs; presence of liver metastases; prior nephrectomy vs no prior nephrectomy; sunitinib vs sorafenib; administration of bisphosphonates.
The factors that were included for multivariate analysis for OS were: baseline neutrophil count; baseline platelet count; baseline Eastern Cooperative Oncology Group performance status; presence of liver metastases; prior nephrectomy vs no prior nephrectomy; sunitinib vs sorafenib; clear cell histology vs other histology; administration of bisphosphonates.
Baseline lactate dehydrogenase was not taken into account because few patients presented with elevated values.
Note: On multivariate analysis for PFS, the P-value for the parameter ‘time from diagnosis metastases to start TKIs ⩽6 months or >6 months’ was 0.38. The P-value for the parameter ‘sunitinib vs sorafenib’ was 0.22. On multivariate analysis for OS, the P-value for the parameter ‘sunitinib vs sorafenib’ was 0.51.
For the ONJ-incidence analysis, 52 patients were evaluable: the 49 patients of the concomitant bisphosphonates group, one patient who started bisphosphonates during first-line TKIs and two patients who received bisphosphonates together with second-line TKI. The mean duration of bisphosphonate administration was 14.3 months (Table 5). Five patients out of 52 (10%) developed ONJ after 4, 12, 18, 27 and 60 months of bisphosphonates (mean 24.2 months) and 2, 5, 6, 27 and 39 months of TKIs. This incidence might underestimate the risk for ONJ in concomitant anti-VEGF-TKI and bisphosphonates because most of the patients had a short survival and short administration of bisphosphonates. The incidence of ONJ in patients with bisphosphonates administration for >12 months was 17%. In one of these patients ONJ developed after dental extractions performed before the start of the bisphosphonates. Three patients did not have a dental check-up before starting bisphosphonates as they started bisphosphonates at a moment at which there was no awareness of the higher incidence of ONJ with bisphosphonates.
Table 5. Incidence of ONJ.
| Bisphosphonate exposure (months) | Number of patients | Mean duration of bisphosphonates (months) | Mean duration of TKI use (months) | Incidence ONJ |
|---|---|---|---|---|
| 1–6 | 24 | 2.4 | 5.0 | 1/24 (4%) |
| 7–12 | 10 | 9.7 | 10.8 | 1/10 (10%) |
| 13–24 | 6 | 17.3 | 10.0 | 1/6 (17%) |
| 25–36 | 6 | 30.2 | 32.0 | 1/6 (17%) |
| 37–84 | 6 | 50.8 | 26.0 | 1/6 (17%) |
| Cumulative exposure of bisphosphonates (months) | Number of patients | Mean duration of bisphosphonates (months) | Mean duration of TKI use (months) | Incidence ONJ |
| 1–12 | 34 | 4.6 | 7.0 | 2/34 (6%) |
| 1–24 | 40 | 6.5 | 7.0 | 3/40 (8%) |
| 1–36 | 46 | 9.6 | 10.0 | 4/46 (9%) |
| 1–84 | 52 | 14.3 | 12.3 | 5/52 (10%) |
| >12 | 18 | 32.8 | 23.0 | 3/18 (17%) |
| >24 | 12 | 40.5 | 29.0 | 2/12 (17%) |
Abbreviations: ONJ=osteonecrosis of the jaw; TKI=tyrosine kinase inhibitor.
Note: One patient received bisphosphonates for 84 months.
Discussion
Our retrospective data suggest that the concomitant use of bisphosphonates has a positive impact on survival outcomes in RCC patients treated with TKIs.
As bone metastases in RCC are mainly osteolytic, the vicious circle of mutual stimulation between metastatic tumour cells and osteoclasts, the so called ‘seed and soil’ phenomenon, probably has an important role in RCC. Osteolysis mediated by osteoclasts liberates several bone-embedded growth factors such as transforming growth factor-beta, bone morphogenic proteins and platelet-derived growth factor, which not only stimulate the local growth of malignant mRCC cells, but probably also circulate and stimulate remote metastatic growth. In that case, concomitant administration of bone resorption inhibitors might have a favourable impact on outcome (Clezardin and Teti, 2007). Additionally, bisphosphonates have been shown to have a broad anti-tumoral potency (anti-migration, anti-angiogenic and immunostimulation), at least in vitro.
Our study, owing to its retrospective nature and small number of patients, can have some biases. A randomized placebo-controlled trial could give more convincing data, but patients in the placebo arm would be exposed to high rates of SREs. According to the literature, up to 75% of patients with mRCC who do not receive bone-targeting agents develop an SRE (Saad and Lipton, 2005) and in patients with mRCC, the first year skeletal morbidity rate can be as high as 2.5–4 SREs per year (Zekri et al, 2001).
The longer the time between the diagnosis of bone metastases and the start of TKIs, the higher the probability that at a certain moment bisphosphonates were started. Therefore, in the group with concomitant TKIs and bisphosphonates, there might be more patients with a more indolent tumour, although this is not reflected by the distribution of the baseline patient characteristics and although in the concomitant group there were more patients with synchronous metastases (59% vs 48%), more patients with a lapse between the initial diagnosis and the start of TKI shorter than 12 months (61% vs 41%) and a shorter median interval between initial diagnosis at the start of TKIs (17.0 vs 23.0 months). On the other hand, the interval between the diagnosis of metastases and the start of TKIs was longer in patients with concomitant therapy (8.5 vs 5.0 months). Nevertheless, none of these findings was significant. Therefore, an additional parameter was analysed in univariate and multivariate analysis: the interval between the diagnosis of metastases and the start of TKIs ⩽6 months or >6 months. We could not retain this parameter as an independent factor linked to PFS or OS.
Our findings are in accordance with the findings of Keizman et al (2012), who published a series of 76 RCC patients with bone metastases treated with sunitinib. Thirty-five patients received concomitant bisphosphonates, whereas 41 patients did not. Median PFS was 15 vs 5 months (P<0.0001) and median OS not reached vs 14 months (P=0.029).
The survival outcome in our retrospective study, with well balanced groups in terms of all known and possible factors linked to outcome, is also confirmed by the ‘posthoc’-analysis of the RCC-cohort in the large randomized phase III trial of ZA vs placebo in solid tumours (Rosen et al, 2003). This analysis was set up in the pre-targeted therapy era. In the RCC subset of 46 patients treated with either ZA (n=27) or placebo (n=19), ZA significantly extended time to disease progression (19.5 vs 3.0 months; P=0.014) and demonstrated a trend towards prolonged OS (11.6 vs 7.2 months; P=0.104) (Saad and Eastham, 2010).
There is other evidence of survival benefit in some malignancies with predominantly lytic tumour bone disease. Results from the prospective placebo-controlled trial in 40 patients with bone metastases from bladder cancer demonstrated that ZA (4 mg monthly for 6 months) significantly increased the 1-year OS rate (36% vs 0% P=0.004) and improved SRE-free survival (P=0.001) compared with placebo (Zaghloul et al, 2010). Zarogoulidis observed a clinically and statistically significant difference in OS in a series of 144 stage IV NSCLC patients with bone metastases. All were treated with combination chemotherapy with carboplatin and docetaxel. Eighty-seven of these patients experienced bone pain and were treated with bisphosphonates, meanwhile the other 57, who did not experience bone pain, did not receive bisphosphonates. Median time to progression was 8.8 vs 5 months (P<0.001), and median OS 19 vs 12.8 months (P<0.001). In patients treated with concomitant bisphosphonates, partial RR was 28.7% vs 15.7% in the group treated with chemotherapy alone (Zarogoulidis et al, 2009). Finally, in multiple myeloma, ZA extended median OS by 5.5 months (P=0.04) vs clodronic acid and increased median PFS by 2 months (P=0.0179) (Morgan et al, 2010).
ONJ, an aseptic necrosis of either mandibula or maxilla with painful ulceration in the mouth is regarded as a specific adverse event associated with the use of bisphosphonates or denosumab. It occurs in 1.5–10% of cancer patients treated with intravenous bisphosphonates. The incidence of ONJ is related to the time of exposure: in a series of 252 patients, Bamias et al (2005) observed an ONJ incidence of 1.5% after 1–12 months, 4.3% after 13–24 months and 7.7% after 24–48 months of exposure. ONJ is much less common in patients treated with bisphosphonates for osteoporosis (in whom bisphosphonates are used at lower doses or longer intervals). Negative predictive factors for the development of ONJ are poor mouth hygiene and poor dental state, concomitant therapies like thalidomide with anti-angiogenic properties and dexamethasone, concomitant radiotherapy and dental interventions like extractions. Nitrogen-containing bisphosphonates are more linked to ONJ than the less potent non-nitrogen-containing bisphosphonates.
We noticed a high incidence of ONJ in patients treated concomitantly with anti-VEGF-targeted TKIs and bisphosphonates. This incidence might underestimate the risk for ONJ in concomitant anti-VEGF-TKI and bisphosphonates because most of the patients had a short survival and short administration of bisphosphonates. Moreover, as this was a retrospective study, there was no prospective screening for ONJ by a dentist, but ONJ was only diagnosed when patients developed symptoms.
Several case reports of ONJ in patients treated with TKIs and bisphosphonates have been published (Ayllon et al, 2009), as well as some retrospective series. In two large retrospective series of 223 and 425 patients with locally recurrent or metastatic breast cancer receiving a bevacizumab-containing regimen and concomitant bisphosphonates, Guarneri et al (2010) found an ONJ incidence of 0.9% and 2.4%. Probably patients receiving anti-VEGF-TKIs are at higher risk than patients receiving anti-VEGF-monoclonal antibodies. Concerning TKIs only small series are available. Christodoulou et al (2009) reports an ONJ-incidence of 16% in 25 patients with bone metastatic colon, breast and mRCC patients treated with sunitinib- or a bevacizumab-containing regimen and bisphosphonates. In a series of 21 mRCC patients treated concomitantly with ZA and sunitinib, five patients (24%) developed ONJ after a mean duration of exposure of 18.5 months of ZA and 5.4 months of sunitinib (Bozas et al, 2011). Keizman et al (2012) did not report any case of ONJ in their series of 35 patients receiving concomitantly sunitinib and bisphosphonates. As this is a retrospective study, precise data on dental hygiene are lacking and as several patients started bisphosphonates before the time of awareness of the higher risk for ONJ, they did not all undergo a dental check-up.
Conclusion
The concomitant use of bisphosphonates with TKIs targeting angiogenic pathways in RCC patients with bone metastasis is possibly associated with a better outcome in terms of RR, PFS and OS as compared with patients treated with TKIs alone, but increases the incidence of ONJ. Careful dental protective measures, limitation of the duration of bisphosphonate use and immediate interruption in case of the first signs of ONJ are indicated. Larger prospective series should better define the benefits and risks of concomitant bisphosphonates and TKIs.
Acknowledgments
Benoit Beuselinck received a grant from the Fonds voor Wetenschappelijk Onderzoek Vlaanderen ‘Klinische doctoraatsbeurs’ (Belgium) (2011–2013). Alexandra Karadimou received a grant from the Hellenic Society of Medical Oncology (Athens, Greece) (2010–2011).
Footnotes
The authors declare no conflict of interest.
References
- Ayllon J, Launay-Vacher V, Medioni J, Cros C, Spano JP, Oudard S (2009) Osteonecrosis of the jaw under bisphosphonate and antiangiogenic therapies: cumulative toxicity profile? Ann Oncol 20(3): 600–601 [DOI] [PubMed] [Google Scholar]
- Bamias A, Kastritis E, Bamia C, Moulopoulos LA, Melakopoulos I, Bozas G, Koutsoukou V, Gika D, Anagnostopoulos A, Papadimitriou C, Terpos E, Dimopoulos MA (2005) Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol 23(34): 8580–8587 [DOI] [PubMed] [Google Scholar]
- Beuselinck B, Oudard S, Rixe O, Wolter P, Blesius A, Ayllon J, Elaidi R, Schöffski P, Barrascout E, Morel A, Escudier B, Lang H, Zucman-Rossi J, Medioni J (2011) ‘Negative impact of bone metastasis on outcome in clear cell renal cell carcinoma treated with sunitinib’. Ann Oncol 22(4): 794–800 [DOI] [PubMed] [Google Scholar]
- Bozas G, Allgar V, Greenwood G, Maraveyas A (2011) Osteonecrosis of the jaw in patients treated with sunitinib and zoledronic acid. J Clin Oncol 29(Suppl): abstract e15116 [Google Scholar]
- Christodoulou C, Pervena A, Klouvas G, Galani E, Falagas ME, Tsakalos G, Visvikis A, Nikolakopoulou A, Acholos V, Karapanagiotidis G, Batziou E, Skarlos DV (2009) Combination of bisphosphonates and antiangiogenic factors induces osteonecrosis of the jaw more frequently than bisphosphonates alone. Oncology 76(3): 209–211 [DOI] [PubMed] [Google Scholar]
- Clezardin P, Teti A (2007) Bone metastasis: pathogenesis and therapeutic implications. Clin Exp Metastasis 24(8): 599–608 [DOI] [PubMed] [Google Scholar]
- Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Siebels M, Negrier S, Chevreau C, Solska E, Desai AA, Rolland F, Demkow T, Hutson TE, Gore M, Freeman S, Schwartz B, Shan M, Simantov R, Bukowski RM, TARGET Study Group (2007a) TARGET Study Group. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med 356(2): 125–134 [DOI] [PubMed] [Google Scholar]
- Escudier B, Pluzanska A, Koralewski P, Ravaud A, Bracarda S, Szczylik C, Chevreau C, Filipek M, Melichar B, Bajetta E, Gorbunova V, Bay JO, Bodrogi I, Jagiello-Gruszfeld A, Moore N, AVOREN Trial investigators (2007b) Bevacizumab plus interferon alfa-2a for treatment of metastatic renal cell carcinoma: a randomised, double-blind phase III trial. Lancet 370(9605): 2103–2111 [DOI] [PubMed] [Google Scholar]
- Guarneri V, Miles D, Robert N, Diéras V, Glaspy J, Smith I, Thomssen C, Biganzoli L, Taran T, Conte P (2010) Bevacizumab and osteonecrosis of the jaw: incidence and association with bisphosphonate therapy in three large prospective trials in advanced breast cancer. Breast Cancer Res Treat 122(1): 181–188 [DOI] [PubMed] [Google Scholar]
- Hudes G, Carducci M, Tomczak P, Dutcher J, Figlin R, Kapoor A, Staroslawska E, Sosman J, McDermott D, Bodrogi I, Kovacevic Z, Lesovoy V, Schmidt-Wolf IG, Barbarash O, Gokmen E, O'Toole T, Lustgarten S, Moore L, Motzer RJ, Global ARCC Trial (2007) Global ARCC Trial. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med 356(22): 2271–2281 [DOI] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, Thun MJ (2006) Cancer statistics, 2006. CA Cancer J Clin 2006: 106–130 [DOI] [PubMed] [Google Scholar]
- Keizman D, Ish-Shalom M, Pili R, Hammers H, Eisenberger M, Sinibaldi V, Boursi B, Maimon N, Gottfried M, Hayat H, Peer A, Kovel S, Sella A, Berger R, Carducci MA (2012) Bisphosphonates combined with sunitinib may improve the response rate, progression free survival and overall survival of patients with bone metastases from renal cell carcinoma. Eur J Cancer 48(7): 1031–1037 [DOI] [PubMed] [Google Scholar]
- Lam JS, Leppert JT, Belldegrun AS, Figlin RA (2005) Novel approaches in the therapy of metastatic renal cell carcinoma. World J Urol 23(3): 202–212 [DOI] [PubMed] [Google Scholar]
- Morgan GJ, Davies FE, Gregory WM, Cocks K, Bell SE, Szubert AJ, Drayson MT, Owen RG, Feyler S, Ashcroft AJ, Ross F, Byrne J, Roddie H, Rudin C, Cook G, Jackson GH, Child JA, National Cancer Research Institute Haematological Oncology Clinical Study Group (2010) First-line treatment with zoledronic acid as compared with clodronic acid in multiple myeloma (MRC Myeloma IX): a randomised controlled trial. Lancet 376(9757): 1989–1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motzer R, Bacik J, Mazumbar M (2004) Prognostic factors for survival of patients with stage IV renal cell carcinoma: Memorial Sloan Kettering Cancer Center experience. Clin Cancer Res 10(18 Part 2): 6202S–6203S [DOI] [PubMed] [Google Scholar]
- Motzer R, Mazumdar M, Bacik J, Berg W, Amsterdam A, Ferrara J (1999) Survival and prognostic stratification of 670 patients with advanced renal cell carcinoma. J Clin Oncol 17(8): 2530–2540 [DOI] [PubMed] [Google Scholar]
- Motzer RJ, Escudier B, Oudard S, Hutson TE, Porta C, Bracarda S, Grünwald V, Thompson JA, Figlin RA, Hollaender N, Kay A, Ravaud A, RECORD-1 Study Group (2010) Phase 3 trial of everolimus for metastatic renal cell carcinoma: final results and analysis of prognostic factors. Cancer 116(18): 4256–4265 [DOI] [PubMed] [Google Scholar]
- Motzer RJ, Escudier B, Oudard S, Hutson TE, Porta C, Bracarda S, Grünwald V, Thompson JA, Figlin RA, Hollaender N, Urbanowitz G, Berg WJ, Kay A, Lebwohl D, Ravaud A, RECORD-1 Study Group (2008) Efficacy of everolimus in advanced renal cell carcinoma: a double-blind, randomised, placebo-controlled phase III trial. Lancet 372(9637): 449–456 [DOI] [PubMed] [Google Scholar]
- Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, Oudard S, Negrier S, Szczylik C, Kim ST, Chen I, Bycott PW, Baum CM, Figlin RA (2007) Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med 356(2): 115–124 [DOI] [PubMed] [Google Scholar]
- Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55(2): 74–108 [DOI] [PubMed] [Google Scholar]
- Patil S, Figlin R, Hutson T, Michaelson M, Négrier S, Kim T, Huang X, Motzer R (2011) Prognostic factors for progression free survival and overall survival with sunitinib targeted therapy and with cytokine as first-line therapy in patients with metastatic renal cell carcinoma. Ann Oncol 22(2): 295–300 [DOI] [PubMed] [Google Scholar]
- Riechelmann R, Chin S, Wang L, Tannock IF, Berthold DR, Moore MJ, Knox JJ (2008) Sorafenib for metastatic renal cancer: the Princess Margaret experience. Am J Clin Oncol 31(2): 182–187 [DOI] [PubMed] [Google Scholar]
- Rosen LS, Gordon D, Tchekmedyian S, Yanagihara R, Hirsh V, Krzakowski M, Pawlicki M, de Souza P, Zheng M, Urbanowitz G, Reitsma D, Seaman JJ (2003) Zoledronic acid versus placebo in the treatment of skeletal metastases in patients with lung cancer and other solid tumors: a phase III, double-blind, randomized trial-the Zoledronic Acid Lung Cancer and Other Solid Tumors Study Group. J Clin Oncol 21(16): 3150–3157 [DOI] [PubMed] [Google Scholar]
- Saad F, Eastham JA (2010) Zoledronic acid use in patients with bone metastases from renal cell carcinoma or bladder cancer. Semin Oncol 37(Suppl 1): S38–S44 [DOI] [PubMed] [Google Scholar]
- Saad F, Lipton A (2005) Zoledronic acid is effective in preventing and delaying skeletal events in patients with bone metastases secondary to genitourinary cancers. BJU Int 96: 964–969 [DOI] [PubMed] [Google Scholar]
- US National Institutes of Health (2006) Surveillance, epidemiology and end results (SEER) cancer statistics review. Kidney and Renal Pelvis Cancer 5-year Relative Survival Rates, 1996–2002; http://seer.cancer.gov/cgi-bin/csr/1975_2003/search.pl#results (September 2006)
- Zaghloul MS, Boutrus R, El-Hossieny H, Kader YA, El-Attar I, Nazmy M (2010) A prospective, randomized, placebo-controlled trial of zoledronic acid in bony metastatic bladder cancer. Int J Clin Oncol 15(4): 382–389 [DOI] [PubMed] [Google Scholar]
- Zarogoulidis K, Boutsikou E, Zarogoulidis P, Eleftheriadou E, Kontakiotis T, Lithoxopoulou H, Tzanakakis G, Kanakis I, Karamanos NK (2009) The impact of zoledronic acid therapy in survival of lung cancer patients with bone metastasis. Int J Cancer 125(7): 1705–1709 [DOI] [PubMed] [Google Scholar]
- Zekri J, Ahmed N, Coleman RE, Hancock BW (2001) The skeletal metastatic complications of renal cell carcinoma. Int J Oncol 19: 379–382 [DOI] [PubMed] [Google Scholar]